Abstract
Background
We determined the expression of forkhead box Q1 (FoxQ1), E-cadherin (E-cad), Mucin 1 (MUC1), vimentin (VIM) and S100 calcium binding protein A4 (S100A4), all epithelial-mesenchymal transition (EMT) indicator proteins in non-small cell lung cancer (NSCLC) tissue samples. We also investigated the relationship between these five proteins expression and other clinicopathologic factors in NSCLC. Finally, we assessed the potential value of these markers as prognostic indicators of survival in NSCLC's patients.
Methods
Quantitative real-time PCR and immunohistochemistry were used to characterize the expression of the FoxQ1 mRNA and protein in NSCLC. Expression of transcripts and translated products for the other four EMT indicator proteins was assessed by immunohistochemistry in the same clinical NSCLC samples.
Results
FoxQ1 mRNA and protein were up-regulated in NSCLC compared with normal tissues (P = 0.015 and P<0.001, respectively). Expression of FoxQ1 in adenocarcinoma was higher than in squamous cell carcinoma (P = 0.005), and high expression of FoxQ1 correlated with loss of E-cad expression (P = 0.012), and anomalous positivity of VIM (P = 0.024) and S100A4 (P = 0.004). Additional survival analysis showed that high expression of FoxQ1 (P = 0.047) and E-cad (P = 0.021) were independent prognostic factors.
Conclusion
FoxQ1 maybe plays a specific role in the EMT of NSCLC, and could be used as a prognostic factor for NSCLC.
Introduction
Lung cancer is the most frequently occurring cancer type, and the leading cause of cancer death globally, with greater mortality than breast, prostate, and colorectal cancer combined [1], [2]. Over the past three decades in China, lung cancer mortality has increased by 465%, with these malignancies becoming the second leading cause of death after liver cancer [3]. Despite great advance in the treatment of cancers in recent years, the prognosis for patients with lung cancer remains poor, with 5-year survival rates less than 15% [4], [5]. Most patients with lung cancer are at an advanced period of the disease at the time of diagnosis, and approximately 85% of these cancers are non-small cell lung cancer (NSCLC) [1], [6].
Many recent studies have noted that the epithelial-mesenchymal transition (EMT) is a critical event in tumour invasion and metastasis in epithelial-derived cancers [7]–[10], including NSCLC [11]–[14]. The awareness of the EMT phenomena dates back as early as 1908. During the 1990s, EMT gained more recognition as a possibly important mechanism in chronic diseases, such as organ fibrosis and cancer [15]. EMT is characterized by down-regulation of epithelial differentiation markers E-cadherin (E-cad) [16]–[20] and Mucin 1 (MUC1) [21], and the up-regulation of mesenchymal markers such as vimentin (VIM) [17]–[20], [22], [23], fibronectin [17], [20], [24] and S100 calcium-binding protein A4 (S100A4) [25]–[28]. Previous studies have described a key role for forkhead box Q1 (FoxQ1) in regulating EMT and aggressiveness in human cancer [29]–[32].
FOXQ1, formerly known as HNF-3/forkhead homolog 1 (HFH1), belongs to a member of the forkhead transcription factor family [32]–[34], which are expressed in different tissues and play important roles in development, metabolism, cancer and aging [30], [34]. As one of the first forkhead genes studied, FOXQ1 has been implicated to repress smooth muscle-specific genes, such as Sm22α and telokin in A10 cells [35]. FOXQ1 has been shown to be a downstream mediator of Hoxa1 in embryonic stem cells [36]. Human FOXQ1, located on chromosome 6p23-25, has been isolated and characterized [33] and plays an essential part in the aetiology of human cancer [31], [32].
Recent studies have described that FOXQ1 has been found to be overexpressed in colorectal cancer [29], [31] and breast cancer [31], [32], in which patients have poor clinical outcomes [31], [32]. Although the overexpression of FOXQ1 in cancer cell lines confirmed that the gene might play a role in the development of lung cancer [29], [33], the correlation between FOXQ1 expression and EMT factors to determine its clinical significance in NSCLC has not been previously reported.
We analysed expression of the FoxQ1 gene using quantitative reverse transcription polymerase chain reactions (RT-PCRs) in small, freshly frozen NSCLC tissue samples. Expression of the FoxQ1 protein and four common EMT indicator proteins (E-cad, MUC1, VIM and S100A4) was assessed by immunohistochemistry using the same tissue microarray (TMA) sections. Additionally, we investigated the relationship between the expressions of the five genes encoding these proteins and other clinicopathological factors in NSCLC. Finally, we assessed the potential value of these markers as prognostic indicators of survival in patients with NSCLC.
Methods
Patients and TMA of NSCLC samples
After a full pathological review according to the 7th Edition of TNM in Lung Cancer [37], a panel of formalin-fixed paraffin-embedded NSCLC tissues with corresponding tumour-adjacent tissues undergoing surgical therapy were obtained from the Affiliated Hospital of Nantong University between January 2005 and December 2006. Clinical data (including gender, age, histological type, grade, stage, tumour size, differentiation, lymph node metastasis status) were obtained from each patient's medical records.
Among the archival material, 103 tissue blocks from NSCLC patients with 5 years' follow-up survival records were available and used for constructing the TMA. A representative area of each tumour was selected and 2.0 mm tissue cores were used to construct a TMA by Shanghai Outdo Biotech (China). The quality of TMA sections was confirmed using haematoxylin-eosin staining (H&E). The average age of the group was 62.5 years (range: 35–81 years). Survival was calculated from the date of surgery until the date of death or last follow-up. Furthermore, a panel of 20 freshly frozen NSCLC tissues and matching peritumour tissues from the same hospital mentioned above were used in this study. Before surgical therapy, none of the patients had received neoadjuvant chemotherapy, radiation therapy or immunotherapy. Ethics approval to perform this study was obtained from the local Human Research Ethics Committee.
Quantitative RT-PCR (qRT-PCR)
Total RNA was extracted and purified from 40 freshly frozen NSCLC tissue samples, including 20 NSCLC tissues and 20 corresponding non-cancerous tissues. Total RNA extraction, quality control and one-step qRT-PCR were performed as previously reported [38]. FOXQ1-specific oligonucleotide primers (forward, 5′-ACG CTG GCG GAG ATC AAC GAG-3′; reverse, 5′-AGG TTG TGG CGC ACG GAG TT-3′) were designed to yield a 92-bp PCR product. The data were normalized using glyceraldehyde-3-phosphate dehydrogenase (GAPDH) as a reference gene (forward primer, 5′-TCG GAG TCA ACG GAT TTG GTC GT-3′; reverse primer, 5′-TGC CAT GGG TGG AAT CAT ATT GGA-3′).
Immunohistochemistry (IHC)
IHC was performed as described previously [39]. Deparaffinized sections (4-μm thick) from array blocks were separately stained on an Autostainer Universal Staining System (LabVision, USA) using the following primary antibodies: mouse anti-FOXQ1 (1∶300 dilution; Abcam, UK), mouse anti-E-cad (1∶120; Invitrogen, USA), monoclonal mouse anti-MUC1 (1∶200; Novocastra, UK), monoclonal mouse anti-VIM (1:100; Invitrogen, USA), and polyclonal rabbit anti-S100A4 (1∶100; Newmarker, USA). Secondary antibodies used were: Envision goat anti-mouse HRP (DAKO, USA), Envision goat anti-rabbit HRP (DAKO, USA). The evaluation of immunostaining of these sections was made blind to two trained pathologists who were unaware of the clinical background of the samples.
The percentages of FoxQ1-positive cells were scored and placed into four categories according to staining: 0 for 0%; 1 for 1–33%; 2 for 34–66%; and 3 for 67–100%. The FoxQ1 staining intensities were also scored as: 0, 1, 2, or 3. The sum of the percentages and intensity scores was used as the final FoxQ1 staining score, which we have outlined previously [39] and has been defined as follows: 0–2, low expression; and 3–6, high expression. However, for the positivity of the selected EMT makers (E-cad, MUC1, VIM and S100A4), no detectable or <10% positive staining of tumour cells was deemed as negative, whereas ≥10% positive staining of tumour cells was considered positive [40]. All samples were evaluated at 4 × and 10× magnification.
Statistical methods
The FoxQ1 mRNA level in freshly frozen NSCLC tissues and corresponding non-cancerous tissues was normalized to GAPDH and analysed using the Wilcoxon signed rank test for Nonparametric Tests. Associations between clinicopathologic variables and FoxQ1 protein expression were examined by χ2 tests. The chi-squared were used to confirm the correlation between expression of FoxQ1 and EMT indicator proteins. Survival curves were calculated using the method of Kaplan-Meier and compared using the log-rank test. Factors shown to be of prognostic significance in the univariate models were evaluated using a multivariate Cox regression model. A P-value less than 0.05 was considered to be statistically significant. Data were analysed using STATA 9.0 software (Stata Corporation).
Results
FoxQ1 mRNA expression in NSCLC and peritumoural tissues
Total RNA was extracted from the freshly frozen NSCLC tissues and subjected to one-step qRT-PCR to investigate FoxQ1 mRNA expression. We also investigated samples from adjacent matched tumour tissues. When normalized to GAPDH, the mean expression levels of FoxQ1 mRNA in NSCLC and corresponding non-cancerous tissue were 0.15±0.02 and 0.04±0.02 (P = 0.015), respectively. FoxQ1 expression was 3.75-fold higher on average in the cancer samples than in non-malignant tissues (Fig. 1).
Figure 1. Expression of FoxQ1 mRNA in NSCLC tissues and corresponding non-cancerous tissues.
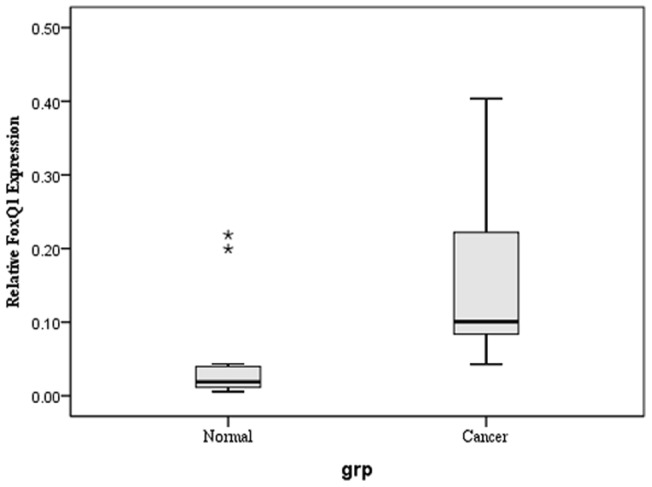
One-step q RT-PCR was performed to confirm the expression of FoxQ1 mRNA in human tissues. Results were normalized to GAPDH mRNA level. The FoxQ1 mRNA level in NSCLC tissues were higher than that in peritumoural tissues with statistical significance using a paired-samples T test. ** P<0.05. Bars indicate standard error (S.E.).
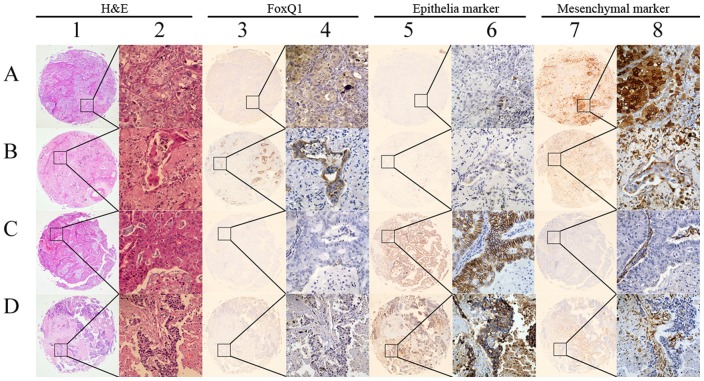
IHC findings for FoxQ1 and EMT indicator proteins in NSCLC tissues
Typical immunohistochemical staining patterns observed for the five genes encoding the FoxQ1 and the other four indicator EMT proteins in NSCLC are shown in Figure 2. Positive staining for FoxQ1 was mainly localized to tumour cells and pneumocytes in the cytoplasm and plasmalemma at different levels. While positive nuclear staining could be seen, FoxQ1 immunolabelling was not observed in the stroma of these tissues. High FoxQ1 expression was detected in 82/103 (50.49%) of NSCLC tissues and was in 38 (20.39%) of the adjacent matched tumour tissues. The data showed statistical significance using χ2 test analysis (χ2 = 38.6450, P<0.001) and was consistent with FoxQ1 mRNA levels in NSCLCs.
Figure 2. Representative IHC images showing expression of FoxQ1 and EMT-related biomarkers in TMA sections of NSCLC.
(A) 1 and 2: lung squamous cell carcinoma tissue pattern with H&E staining; 3 and 4: high expression of FoxQ1; 5 and 6: loss of E-cad expression; 7 and 8: strong VIM-positive staining. (B) 1 and 2: lung adenocarcinoma tissue pattern with H&E staining; 3 and 4: positive staining for FoxQ1; 5 and 6: negative staining for MUC1; 7 and 8: up-regulated expression of S100A4. (C) 1 and 2: lung adenocarcinoma tissue with H&E staining; 3 and 4: negative IHC for FoxQ1; 5 and 6: strong immunological reaction of E-cad; 7 and 8: negative for S100A4. (D) 1 and 2: lung squamous cell carcinoma tissue with H&E staining; 3 and 4: low expression of FoxQ1; 5 and 6: high expression of MUC1; 7 and 8: weak expression of VIM. Original magnification was ×40 for 1, 3, 5 and 7; and ×400 for 2, 4, 6 and 8.
Positive expression of E-cad and MUC1 was localised to the cell membrane, and a combination of the plasmalemma and cytoplasm in NSCLC tumour cells, respectively. Positive immunohistochemical staining for VIM and S100A4 in cancer cells was observed in the cytoplasm, and a combination of the nucleus and cytoplasm. An exception to this was the positive stromal fibroblasts.
Relationship between expression of FoxQ1 proteins and clinicopathological parameters in NSCLC
The associations between FoxQ1 expression and clinicopathological features of NSCLC are shown in Table 1. FoxQ1 protein expression in adenocarcinoma was higher than in squamous cell carcinoma with statistical significance (χ2 = 10.7089, P = 0.005) by χ2 test analysis. In contrast, no significant associations were seen with patient age, gender, tumour diameter, histological grade of the tumour, lymph node metastasis status, and stage grouping with TNM.
Table 1. Correlation of high FoxQ1 expression with clinicopathologic characteristics of NSCLC.
| Clinicopathologic characteristics | n | FoxQ1 | χ2 | P | |
| high expression (n) | % | ||||
| Gender | 0.077 | 0.782 | |||
| Male | 71 | 56 | 78.87 | ||
| Female | 32 | 26 | 81.25 | ||
| Age (years) | 2.507 | 0.113 | |||
| ≤60 | 40 | 35 | 87.50 | ||
| >60 | 63 | 47 | 74.60 | ||
| Tumor diameter (cm) | 0.344 | 0.558 | |||
| ≤3 | 35 | 29 | 82.86 | ||
| >3 | 68 | 53 | 77.94 | ||
| Histological type | 10.709 | 0.005* | |||
| Squamous cell carcinoma | 46 | 30 | 65.22 | ||
| Adenocarcinoma | 55 | 50 | 90.91 | ||
| Others | 2 | 2 | 100.00 | ||
| Differentiation | 2.431 | 0.297 | |||
| Well | 7 | 6 | 85.71 | ||
| Moderate | 66 | 55 | 83.33 | ||
| Poorly | 30 | 21 | 70.00 | ||
| Lymph node metastasis | 1.201 | 0.548 | |||
| No regional lymph node metastasis | 53 | 41 | 77.36 | ||
| Metastasis in ipsilateral peribronchial | 26 | 20 | 76.92 | ||
| Metastasis in mediastinal | 24 | 21 | 87.50 | ||
| Stage Grouping with TNM | 1.712 | 0.425 | |||
| Stage I | 50 | 38 | 76.00 | ||
| Stage II | 27 | 21 | 77.78 | ||
| Stage III and IV | 26 | 23 | 88.46 | ||
P<0.05.
Correlation between expression of FoxQ1 and the EMT indicator proteins
The relationships between expression of FoxQ1 and the four EMT indicator proteins were calculated and have been outlined in Table 2. It was noted that epithelial protein loss frequencies in the 103 NSCLC tissues were 66.02% for E-cad and 18.45% for MUC1. Abnormal mesenchymal protein expression frequencies in the same samples were 23.30% for VIM and 68.93% for S100A4. The result also showed that high expression of FoxQ1 correlated with a loss of E-cad expression (χ2 = 6.308, P = 0.012), and anomalous positivity of VIM (χ2 = 1.396, P = 0.024) and S100A4 (χ2 = 8.374, P = 0.004) in clinical NSCLC samples.
Table 2. Relationship between the expression of FoxQ1 and EMT indicator proteins.
| Regular EMT marker expression | FoxQ1 expression | χ2 | P | |
| Low or none | high (n) | |||
| E-cad | 6.308 | 0.012* | ||
| E-cad + | 12 | 23 | ||
| E-cad − | 9 | 59 | ||
| MUC1 | 1.396 | 0.237 | ||
| MUC1 + | 19 | 65 | ||
| MUC1 − | 2 | 17 | ||
| VIM | 5.073 | 0.024* | ||
| VIM − | 20 | 59 | ||
| VIM + | 1 | 23 | ||
| S100A4 | 8.374 | 0.004* | ||
| S100A4 − | 12 | 20 | ||
| S100A4 + | 9 | 62 | ||
P<0.05.
Survival analysis
Several known predictive factors of poor outcome in NSCLC were assessed to validate the cohort of patients represented by this TMA (Table 3). High expression of FoxQ1 protein (P = 0.023) and low expression of E-cad protein (P = 0.002) showed a statistically significant association with five year survival by Cox regression univariate analysis. In addition to these two genetic markers, other NSCLC clinical prognostic factors, such as differentiation of tumour and TNM stage were included in a multivariate Cox regression model. Our data demonstrated that high FoxQ1 expression (P = 0.047) and a loss of E-cad expression (P = 0.021) were confirmed to be independent prognosticators for low survival of NSCLC.
Table 3. Univariate and multivariate analysis of prognostic factors in NSCLC for 5 year survival.
| Univariate analysis | Multivariate analysis | ||||
| P>|z| | HR | P>|z| | [95% Conf. Interval] | ||
| FoxQ1 expression | |||||
| High vs Low | 0.023* | 2.091 | 0.047* | 1.009 | 4.332 |
| Gender | |||||
| Male vs Female | 0.318 | ||||
| Age (years) | |||||
| ≤60 and >60 | 0.054 | ||||
| Diameter (cm) | |||||
| ≤3 vs >3 | 0.367 | ||||
| E-cad | 2.036 | 0.021* | 1.111 | 3.730 | |
| E-cad+ vs E-cad- | 0.002* | ||||
| MUC1 | |||||
| MUC1+ vs MUC1- | 0.121 | ||||
| VIM | |||||
| VIM+ vs VIM- | 0.666 | ||||
| S100A4 | |||||
| S100A4+ vs S100A4- | 0.232 | ||||
| Histological type | |||||
| Sq vs Ad | 0.980 | ||||
| Differentiation | |||||
| Well vs Moderate and Poorly | 0.068 | ||||
| Lymph node metastasis | |||||
| No vs Mip vs Mim | 0.174 | ||||
| Stage Grouping with TNM | |||||
| Stage I vs Stage II vs Stage III\IV | 0.050 | ||||
P<0.05.
Sq, squamous cell carcinoma; Ad, adenocarcinoma; No, no regional lymph node metastasis; Mip, metastasis in ipsilateral peribronchial; Mim, metastasis in mediastinal; HR, Haz. Ratio.
Survival was plotted using the Kaplan–Meier method. The results identified that the patients with a high FoxQ1 expression or loss of E-cad expression had a significantly shorter survival time, compared to those with low or preserved expression, respectively (Fig. 3).
Figure 3. Kaplan-Meier survival curves after surgical therapy in NSCLC.
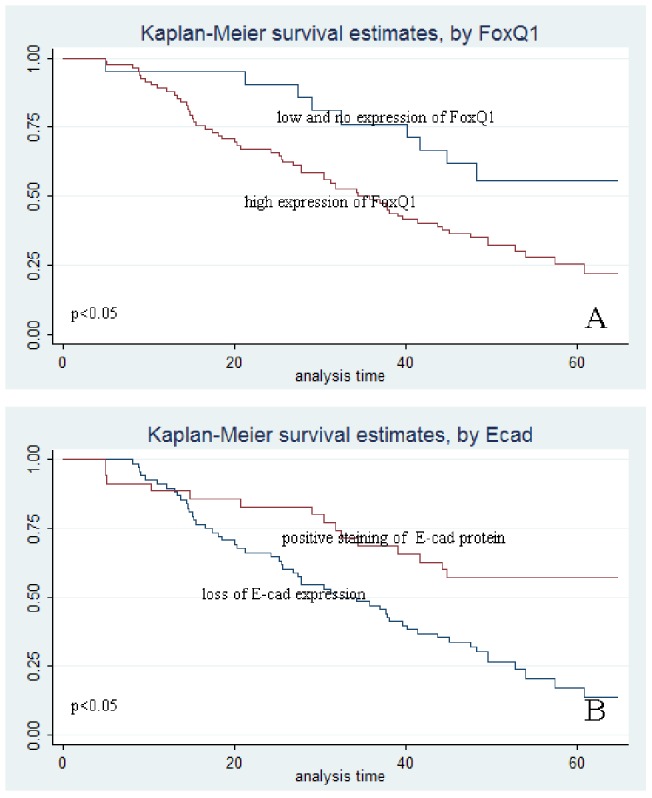
(A) Curves calculated for FoxQ1 expression. High expression in the FoxQ1 group (red line) indicated significantly less survival than low and no expression in the FoxQ1 group (blue line). (B) Curves calculated for E-cad expression. Lifespans of patients with positive E-cad staining are much shorter (red line) than in patients with negative E-cad staining (blue line).
Discussion
In this study, using a TMA, we emphasized the prognostic value of FoxQ1 expression in NSCLC. High expression of FoxQ1 was detectable in TMAs of tumour samples and was significantly correlated with decreased overall survival. Furthermore, the results demonstrated that FoxQ1 expression was significantly associated with EMT in a subgroup of patients. Through multivariate analysis, high expression of FoxQ1 and reduced E-cad expression were shown to be independent prognostic biomarkers for poor overall survival. As far as we know, this is the first report of the clinicopathological significance of FoxQ1 expression related to EMT in clinical NSCLC tissue samples.
Recently, accumulating evidence suggests that human FoxQ1 plays a key role in regulating the EMT of breast cancer [31], [32], and aggressiveness in colon cancer [29], [32]. There is considerable proof that presence of the EMT phenomenon indicates short survival in lung cancer [11]–[14]. To identify the relation between FoxQ1 and EMT in lung carcinoma, four frequent indicator biomarkers were investigated in lung cancer TMA using IHC. Interestingly, our results showed that high levels of expression for the FoxQ1 protein correlated with decreased E-cad protein expression, and increases in VIM and S100A4 protein expression.
Some authors have shown that E-cad is linked with metastasis of lung cancer [12]. VIM is not believed to be associated with survival in lung cancer [14], although S100A4 has been correlated with prognosis of lung squamous cell carcinoma [41] in clinical research studies. We also determined the prognostic effect of EMT marker expression by univariate and multivariate analysis. Our results revealed that the only marker associated with outcome was E-cad.
Recent studies have confirmed that FoxQ1 to be a valuable prognostic indicator for poor survival in breast cancer [31], [32]. However, high expression of the FoxQ1 gene was also observed in lung cancer, gastric cancer, and colon cancer cell lines [29]. Thus, our present results corroborate previous findings regarding FoxQ1 expression in NSCLC, especially in lung adenocarcinoma.
Although the exact mechanisms of FoxQ1's tumorigenic effects in NSCLC have not been described fully in our present investigation, the molecular basis for the association between FoxQ1 and EMT are well understood in tumor. The results obtained from our data are in accordance with those presented in the emerging literature, which had declared that the repression of FoxQ1 led to an increase in E-cad expression in human carcinoma [31], [32]. Collectively, the findings in our present study corroborated that FoxQ1 could be potentially used as an EMT marker in NSCLC.
In conclusion, we have shown that FoxQ1 was highly expressed in NSCLC and could be used as a direct prognosticator of a negative outcome. Also, our results supported the fact that FoxQ1 has a functional role with respect to EMT-related genes in NSCLC.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This study was supported by grants from the Social Development and Applied Research Projects (S2010041) of Nantong government, China; International Cooperation and Exchanges (2011) from the Department of Health Jiangsu; and the Doctoral Fund (2010) of the Affiliated Hospital of Nantong University, Nantong, China. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Cagle PT, Allen TC, Dacic S, Beasley MB, Borczuk AC, et al. Revolution in lung cancer: new challenges for the surgical pathologist. Arch Pathol Lab Med. 2011;135:110–116. doi: 10.5858/2010-0567-RA.1. [DOI] [PubMed] [Google Scholar]
- 2.Sloan JA. Metrics to assess quality of life after management of early-stage lung cancer. Cancer J. 2011;17:63–67. doi: 10.1097/PPO.0b013e31820e15dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wen C, Dehnel T. China wrestles with lung cancer. Lancet Oncol. 2011;12:15. doi: 10.1016/s1470-2045(10)70303-x. [DOI] [PubMed] [Google Scholar]
- 4.Gao W, Liu L, Lu X, Shu Y. Circulating microRNAs: possible prediction biomarkers for personalized therapy of non-small-cell lung carcinoma. Clin Lung Cancer. 2011;12:14–17. doi: 10.3816/CLC.2011.n.001. [DOI] [PubMed] [Google Scholar]
- 5.Smith CB, Kelley AS, Meier DE. Evidence for new standard of care in non-small cell lung cancer patients. Semin Thorac Cardiovasc Surg. 2010;22:193–194. doi: 10.1053/j.semtcvs.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 6.Ulahannan SV, Brahmer JR. Antiangiogenic agents in combination with chemotherapy in patients with advanced non-small cell lung cancer. Cancer Invest. 2011;29:325–337. doi: 10.3109/07357907.2011.554476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee KW, Kim JH, Han S, Sung CO, Do IG, et al. Twist1 Is an Independent Prognostic Factor of Esophageal Squamous Cell Carcinoma and Associated with Its Epithelial-Mesenchymal Transition. Ann Surg Oncol. 2012;19:326–335. doi: 10.1245/s10434-011-1867-0. [DOI] [PubMed] [Google Scholar]
- 8.Soini Y, Tuhkanen H, Sironen R, Virtanen I, Kataja V, et al. Transcription factors zeb1, twist and snai1 in breast carcinoma. BMC Cancer. 2011;11:73. doi: 10.1186/1471-2407-11-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yi ZY, Feng LJ, Xiang Z, Yao H. Vascular endothelial growth factor receptor-1 activation mediates epithelial to mesenchymal transition in hepatocellular carcinoma cells. J Invest Surg. 2011;24:67–76. doi: 10.3109/08941939.2010.542272. [DOI] [PubMed] [Google Scholar]
- 10.van Zijl F, Mall S, Machat G, Pirker C, Zeillinger R, et al. A human model of epithelial to mesenchymal transition to monitor drug efficacy in hepatocellular carcinoma progression. Mol Cancer Ther. 2011;10:850–860. doi: 10.1158/1535-7163.MCT-10-0917. [DOI] [PubMed] [Google Scholar]
- 11.Li LP, Lu CH, Chen ZP, Ge F, Wang T, et al. Subcellular proteomics revealed the epithelial-mesenchymal transition phenotype in lung cancer. Proteomics. 2011;11:429–39. doi: 10.1002/pmic.200900819. [DOI] [PubMed] [Google Scholar]
- 12.Wang G, Dong W, Shen H, Mu X, Li Z, et al. A comparison of Twist and E-cadherin protein expression in primary non-small-cell lung carcinoma and corresponding metastases. Eur J Cardiothorac Surg. 2011;39:1028–1032. doi: 10.1016/j.ejcts.2011.01.023. [DOI] [PubMed] [Google Scholar]
- 13.Pirozzi G, Tirino V, Camerlingo R, Franco R, La Rocca A, et al. Epithelial to Mesenchymal Transition by TGFβ-1 Induction Increases Stemness Characteristics in Primary Non Small Cell Lung Cancer Cell Line. PLoS One. 2011;6:e21548. doi: 10.1371/journal.pone.0021548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Soltermann A, Tischler V, Arbogast S, Braun J, Probst-Hensch N, et al. Prognostic significance of epithelial-mesenchymal and mesenchymal-epithelial transition protein expression in non-small cell lung cancer. Clin Cancer Res. 2008;14:7430–7437. doi: 10.1158/1078-0432.CCR-08-0935. [DOI] [PubMed] [Google Scholar]
- 15.Chai JY, Modak C, Mouazzen W, Narvaez R, Pham J. Epithelial or mesenchymal: Where to draw the line? Biosci Trends. 2010;4:130–142. [PubMed] [Google Scholar]
- 16.Soini Y, Tuhkanen H, Sironen R, Virtanen I, Kataja V, et al. Transcription factors zeb1, twist and snai1 in breast carcinoma. BMC Cancer. 2011;11:73. doi: 10.1186/1471-2407-11-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Casas E, Kim J, Bendesky A, Ohno-Machado L, Wolfe CJ, et al. Snail2 is an essential mediator of Twist1-induced epithelial mesenchymal transition and metastasis. Cancer Res. 2011;71:245–254. doi: 10.1158/0008-5472.CAN-10-2330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang XX, Zhu Z, Su D, Lei T, Wu X, et al. Down-regulation of leucine zipper putative tumor suppressor 1 is associated with poor prognosis, increased cell motility and invasion, and epithelial-to-mesenchymal transition characteristics in human breast carcinoma. Hum Pathol. 2011;42:1410–1419. doi: 10.1016/j.humpath.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 19.Liu LK, Jiang XY, Zhou XX, Wang DM, Song XL, et al. Upregulation of vimentin and aberrant expression of E-cadherin/beta-catenin complex in oral squamous cell carcinomas: correlation with the clinicopathological features and patient outcome. Mod Pathol. 2010;23:213–224. doi: 10.1038/modpathol.2009.160. [DOI] [PubMed] [Google Scholar]
- 20.Chen XF, Zhang HJ, Wang HB, Zhu J, Zhou WY, et al. Transforming growth factor-β1 induces epithelial-to-mesenchymal transition in human lung cancer cells via PI3K/Akt and MEK/Erk1/2 signaling pathways. Mol Biol Rep. 2012;39:3549–3556. doi: 10.1007/s11033-011-1128-0. [DOI] [PubMed] [Google Scholar]
- 21.Okamoto S, Okamoto A, Nikaido T, Saito M, Takao M, et al. Mesenchymal to epithelial transition in the human ovarian surface epithelium focusing on inclusion cysts. Oncol Rep. 2009;21:1209–1214. doi: 10.3892/or_00000343. [DOI] [PubMed] [Google Scholar]
- 22.Satelli A, Li S. Vimentin in cancer and its potential as a molecular target for cancer therapy. Cell Mol Life Sci. 2011;68:3033–3046. doi: 10.1007/s00018-011-0735-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roy LD, Sahraei M, Subramani DB, Besmer D, Nath S, et al. MUC1 enhances invasiveness of pancreatic cancer cells by inducing epithelial to mesenchymal transition. Oncogene. 2011;30:1449–1459. doi: 10.1038/onc.2010.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vaid M, Singh T, Katiyar SK. Grape Seed Proanthocyanidins Inhibit Melanoma Cell Invasiveness by Reduction of PGE(2) Synthesis and Reversal of Epithelial-to-Mesenchymal Transition. PLoS One. 2011;6:e21539. doi: 10.1371/journal.pone.0021539. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 25.Sato Y, Harada K, Itatsu K, Ikeda H, Kakuda Y, et al. Epithelial-mesenchymal transition induced by transforming growth factor-{beta}1/Snail activation aggravates invasive growth of cholangiocarcinoma. Am J Pathol. 2010;177:141–152. doi: 10.2353/ajpath.2010.090747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim MA, Lee HS, Lee HE, Kim JH, Yang HK, et al. Prognostic importance of epithelial-mesenchymal transition-related protein expression in gastric carcinoma. Histopathology. 2009;54:442–451. doi: 10.1111/j.1365-2559.2009.03247.x. [DOI] [PubMed] [Google Scholar]
- 27.Ghoul A, Serova M, Astorgues-Xerri L, Bieche I, Bousquet G, et al. Epithelial-to-mesenchymal transition and resistance to ingenol 3-angelate, a novel protein kinase C modulator, in colon cancer cells. Cancer Res. 2009;69:4260–4269. doi: 10.1158/0008-5472.CAN-08-2837. [DOI] [PubMed] [Google Scholar]
- 28.Lo JF, Yu CC, Chiou SH, Huang CY, Jan CI, et al. The epithelial-mesenchymal transition mediator S100A4 maintains cancer-initiating cells in head and neck cancers. Cancer Res. 2011;71:1912–1923. doi: 10.1158/0008-5472.CAN-10-2350. [DOI] [PubMed] [Google Scholar]
- 29.Kaneda H, Arao T, Tanaka K, Tamura D, Aomatsu K, et al. FOXQ1 is overexpressed in colorectal cancer and enhances tumorigenicity and tumor growth. Cancer Res. 2010;70:2053–2063. doi: 10.1158/0008-5472.CAN-09-2161. [DOI] [PubMed] [Google Scholar]
- 30.Feuerborn A, Srivastava PK, Küffer S, Grandy WA, Sijmonsma TP, et al. The Forkhead factor FoxQ1 influences epithelial differentiation. J Cell Physiol. 2011;226:710–719. doi: 10.1002/jcp.22385. [DOI] [PubMed] [Google Scholar]
- 31.Qiao Y, Jiang X, Lee ST, Karuturi RK, Hooi SC, et al. FOXQ1 regulates epithelial-mesenchymal transition in human cancers. Cancer Res. 2011;71:3076–3086. doi: 10.1158/0008-5472.CAN-10-2787. [DOI] [PubMed] [Google Scholar]
- 32.Zhang H, Meng F, Liu G, Zhang B, Zhu J, et al. Forkhead transcription factor foxq1 promotes epithelial-mesenchymal transition and breast cancer metastasis. Cancer Res. 2011;71:1292–1301. doi: 10.1158/0008-5472.CAN-10-2825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bieller A, Pasche B, Frank S, Gläser B, Kunz J, et al. Isolation and characterization of the human forkhead gene FOXQ1. DNA Cell Biol. 2001;20:555–561. doi: 10.1089/104454901317094963. [DOI] [PubMed] [Google Scholar]
- 34.Jonsson H, Peng SL. Forkhead transcription factors in immunology. Cell Mol Life Sci. 2005;62:397–409. doi: 10.1007/s00018-004-4365-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hoggatt AM, Kriegel AM, Smith AF, Herring BP. Hepatocyte nuclear factor-3 homologue 1 (HFH-1) represses transcription of smooth muscle-specific genes. J Biol Chem. 2000;275:31162–31170. doi: 10.1074/jbc.M005595200. [DOI] [PubMed] [Google Scholar]
- 36.Martinez-Ceballos E, Chambon P, Gudas LJ. Differences in gene expression between wild type and Hoxa1 knockout embryonic stem cells after retinoic acid treatment or leukemia inhibitory factor (LIF) removal. J Biol Chem. 2005;280:16484–16498. doi: 10.1074/jbc.M414397200. [DOI] [PubMed] [Google Scholar]
- 37.Goldstraw P. The 7th Edition of TNM in Lung Cancer: what now? J Thorac Oncol. 2009;4:671–673. doi: 10.1097/JTO.0b013e31819e7814. [DOI] [PubMed] [Google Scholar]
- 38.Huang J, Zhu H, Wang X, Tang Q, Huang H, et al. The patterns and expression of KDR in normal tissues of human internal organs. J Mol Histol. 2011;42:597–603. doi: 10.1007/s10735-011-9355-1. [DOI] [PubMed] [Google Scholar]
- 39.Huang J, Zhang X, Tang Q, Zhang F, Li Y, et al. Prognostic significance and potential therapeutic target of VEGFR2 in hepatocellular carcinoma. J Clin Pathol. 2011;64:343–348. doi: 10.1136/jcp.2010.085142. [DOI] [PubMed] [Google Scholar]
- 40.Uchikado Y, Natsugoe S, Okumura H, Setoyama T, Matsumoto M, et al. Slug expression in the E-cadherin preserved tumors is related to prognosis in patients with esophageal squamous cell carcinoma. Clin Cancer Res. 2005;11:1174–1180. [PubMed] [Google Scholar]
- 41.Tsuna M, Kageyama S, Fukuoka J, Kitano H, Doki Y, et al. Significance of S100A4 as a prognostic marker of lung squamous cell carcinoma. Anticancer Res. 2009;29:2547–2554. [PubMed] [Google Scholar]