Abstract
AIM: To investigate the clinical features and in-hospital outcomes of young adults with acute myocardial infarction (AMI) in Singapore.
METHODS: Between January 2005 to September 2010, 333 consecutive patients aged ≤ 45 years old were diagnosed to have AMI at our institution. As Singapore is a multi-ethnic society, we also analysed whether ethnic differences exist between the three dominant ethnic groups, Malay, Chinese and Indian with regards to the clinical features. Clinical data was collected retrospectively on demographic characteristics, presenting signs and symptoms, blood investigation, angiographic findings and in-hospital clinical outcomes.
RESULTS: The mean age at presentation was 40.2 ± 4.0 years with male predominance (94%). The majority of patients were Chinese (51%) followed by Indians (31%) and Malays (18%). The most common risk factor was smoking (74%) followed by hypertension (28.5%) and hyperlipidemia (20.0%). 37% of patients were obese. The majority of patients had single vessel disease (46%) on coronary angiography. The mean total cholesterol, low-density lipoprotein and high-density lipoprotein levels were 5.6 ± 1.2 mmol/L, 3.8 ± 1.1 mmol/L and 0.93 ± 0.25 mmol/L respectively. The mean left ventricular function was 44% ± 10% with the incidence of heart failure 3% and cardiogenic shock 4.5%. Overall in-hospital mortality was low with 4 deaths (1.2%). For ethnic subgroup analysis, Indians have a 3-fold risk of developing premature AMI when compared to other ethnic groups.
CONCLUSION: Young AMI patients in Singapore are characterized by male predominance, high incidence of smoking and obesity. Overall in-hospital clinical outcomes are favourable. Among the 3 ethnic groups, Indians have the highest risk of developing premature AMI.
Keywords: Clinical features, Myocardial infarction, Outcomes, Southeast asia, Young
INTRODUCTION
Acute myocardial infarction (AMI) is a major cause of morbidity and mortality worldwide. The burden of AMI can be substantial if the individual is relatively young as they are commonly breadwinners of the family and in the prime of their working life with significant contributions to the society. Several studies[1-12] have described the clinical profiles and outcomes of young adults with AMI and its incidence ranged between 2% and 10%. In general, young patients are more likely to be male, have a history of smoking and hyperlipidemia but less likely to have other co-morbidities and demonstrate less extensive coronary artery disease (CAD) on coronary angiogram. There is limited data[11,12] on the clinical features of young adults with AMI in the Southeast Asian region. We therefore sought to investigate the clinical characteristics, angiographic findings and clinical outcomes (in-hospital) of young adults with AMI in Singapore. As Singapore is a multi-ethnic society, we also analysed whether ethnic differences exist between the three dominant ethnic groups i.e., Malay, Chinese and Indian with regards to the clinical features.
MATERIALS AND METHODS
Study population
Between January 2005 to September 2010, 333 consecutive patients aged ≤ 45 years old were diagnosed to have AMI at our institution, a tertiary referral centre in Singapore. Clinical data was collected retrospectively from the medical records on demographic characteristics, presenting signs and symptoms, blood investigation, angiographic findings and in-hospital clinical outcomes.
The diagnosis of AMI was defined as the presence of chest pain and/or electrocardiographic changes suggestive of infarction or ischaemia, associated with increased level of cardiac troponins or cardiac enzymes to at least twice the upper limit of the normal value. All the study patients underwent coronary angiography during the index hospitalisation. Angiographic stenosis was defined as diameter reduction of ≥ 50%. The culprit artery for AMI was identified based on morphology including complete occlusion, thrombus and ulcerative stenosis or assumed to be the tightest stenosis if these features were absent. The classification of body weight by body mass index (BMI) was according to the World Health Organization recommendation for an Asian population[13]. A BMI of more than 27 kg/m2 was defined as obese. The major clinical outcomes (in-hospital) analysed in our study include all-cause mortality, congestive heart failure (New York Heart Association class III-IV), major arrhythmia events (complete heart block, ventricular tachycardia/fibrillation) and cardiogenic shock.
Subgroup analysis by ethnicity
Singapore is a Southeast Asian city-state which has a multi-ethnic population of 5.1 million. There are 3 dominant ethnic groups namely, Malays, Chinese and Indians with the rest being a mixture of minority ethnic group/foreigners. Based on the government census report, the racial composition of Malays, Chinese and Indians in the general population were 13.4%, 74.2% and 9.2%, respectively.
Statistical analysis
Continuous variables were expressed as mean ± SE of mean. Dichotomous variables were expressed as counts and percentages. Statistical comparisons were performed using analysis of variance (ANOVA) and chi square test for trend, as appropriate. A statistically significant effect in ANOVA is followed up by Tukey’s range test. Calculations were performed using SPSS software (version 16.0; SPSS, Inc., Chicago, Illinois). All P values were 2-sided and P values < 0.05 were considered statistically significant. All investigations were carried out in accordance with the Declaration of Helsinki and the study was approved by the local ethics committee.
RESULTS
Table 1 shows the baseline clinical characteristics of our patients. For the overall study group, the mean age at presentation was 40.2 ± 4.0 years (range 25 to 45 years) with male predominance (94%). The most common risk factor was smoking (74%) followed by antecedent hypertension (28.5%), hyperlipidemia (20%) and diabetes mellitus (16.5%). The mean BMI was 26.1 ± 3.8 kg/m2 with 37% of young adults considered obese by Asian BMI criteria. The most common risk factor newly identified at presentation was hyperlipidemia (28%) followed by diabetes mellitus (13%) and hypertension (3%). The mean total cholesterol, low-density lipoprotein and high-density lipoprotein levels were 5.6 ± 1.2 mmol/L, 3.8 ± 1.1 mmol/L and 0.93 ± 0.25 mmol/L respectively. For those with pre-existing diabetes mellitus, the mean HBa1c level was 7.7 ± 2.3 mmol/L. The mean left ventricular function was 44% ± 10%. The mean peak creatine kinase was 2227 ± 2389 IU/L and Troponin-I level was 36.0 ± 33.7 µg/L.
Table 1.
Baseline clinical characteristics of patients
| Overall (n = 333) | Malay (n = 59) | Chinese (n = 171) | Indian (n = 103) | P value | |
| Mean age at presentation (yr) | 40.2 ± 4.0 (25-45) | 40.3 ± 4.8 (25-45) | 40.4 ± 3.6 (30-45) | 39.9 ± 4.2 (26-45) | 0.62 |
| Male:female | 329:23 (93.5:6.5) | 53:6 (89.8:10.2) | 160:11 (93.6:6.4) | 100:3 (97.1:2.9) | 0.06 |
| Ever smoker | 246 (73.8) | 48 (81.4) | 127 (74.3) | 71 (68.9) | 0.08 |
| Hypertension | 95 (28.5) | 15 (25.4) | 54 (31.6) | 26 (25.2) | 0.78 |
| Hyperlipidemia | 66 (19.8) | 10 (16.9) | 32 (18.7) | 24 (23.3) | 0.28 |
| Diabetes | 55 (16.5) | 10 (16.9) | 23 (13.5) | 22 (21.4) | 0.31 |
| Mean BMI (kg/m2) | 26.1 ± 3.8 | 26.2 ± 4.7 | 25.8 ± 3.6 | 26.7 ± 3.7 | 0.15 |
| Newly diagnosed hyperlipidemia | 93 (27.9) | 19 (32.3) | 49 (28.7) | 25 (24.3) | 0.26 |
| Newly diagnosed diabetes | 43 (12.9) | 3 (5.1) | 23 (13.5) | 17 (16.5) | 0.047a |
| Newly diagnosed hypertension | 9 (2.7) | 5 (8.5) | 2 (1.2) | 2 (1.9) | 0.04a |
| Mean total cholesterol (mmol/L) | 5.6 ± 1.2 | 5.9 ± 1.1 | 5.6 ± 1.2 | 5.5 ± 1.3 | 0.16 |
| Mean LDL (mmol/L) | 3.8 ± 1.1 | 4.1 ± 1.1 | 3.7 ± 1.0 | 3.8 ± 1.1 | 0.08 |
| Mean HDL (mmol/L) | 0.93 ± 0.25 | 0.92 ± 0.22 | 0.95 ± 0.27 | 0.89 ± 0.22 | 0.14 |
| Mean HBa1c (mmol/L) | 7.7 ± 2.3 | 7.7 ± 2.3 | 7.4 ± 2.3 | 8.15 ± 2.4 | 0.04a |
| LVEF (%) | 44 ± 10 | 41 ± 10 | 45 ± 9 | 43 ± 11 | 0.008a |
| Creatine kinase (IU/L) | 2227 ± 2389 | 1870 ± 2064 | 2350 ± 2656 | 2220 ± 2055 | 0.41 |
| Troponin (ng/mL) | 36 ± 34 | 32 ± 34 | 36 ± 34 | 38 ± 33 | 0.55 |
P < 0.05. BMI: Body mass index; LDL: Low density lipoprotein; HDL: High density lipoprotein; HBa1c: Glycosylated hemoglobin; LVEF: Left ventricular ejection fraction.
Table 2 shows the clinical presentation, angiographic findings, procedural variables and clinical outcomes of our patients. The majority of patients presented with ST-elevation MI (66.3%) with a slightly higher rate of inferior-posterior MI than anterior MI. By angiographic analysis, the majority of patients (46%) had single vessel disease followed by double vessel disease (26%) and triple vessel disease (23.4%). Occlusive left main disease was present in 11 patients (3.3%) and 14 patients (4.2%) had normal coronary vessels. Two hundred and forty two patients (73%) were treated with percutaneous coronary intervention (PCI) with the rest receiving medical therapy (thrombolysis/anti-thrombotic therapy). The mean number of stents per patient was 1.32 ± 0.65, mean stent diameter was 3.05 ± 0.64 mm and the average length of stents was 21.7 ± 6.9 mm. The majority of patients (67%) had bare metal stent implantation during PCI.
Table 2.
Clinical presentation, angiographic findings, procedural variables and clinical outcomes (in-hospital) of patients
| Overall (n = 333) | Malay (n = 59) | Chinese (n = 171) | Indian (n = 103) | P value | |
| Presentation | |||||
| Anterior STEMI | 109 (32.7) | 19 (32.2) | 59 (34.5) | 31 (30.1) | 0.68 |
| Inferior/posterior STEMI | 112 (33.6) | 14 (23.7) | 59 (34.5) | 39 (37.9) | 0.08 |
| NSTEMI | 112 (33.6) | 26 (44.1) | 53 (31.0) | 33 (32.0) | 0.18 |
| Number of diseased vessels on angiography | |||||
| 0 | 14 (4.2) | 1 (1.7) | 10 (5.8) | 3 (2.9) | 0.95 |
| 1 | 153 (45.9) | 23 (39) | 78 (45.6) | 52 (50.5) | 0.15 |
| 2 | 88 (26) | 18 (30.5) | 45 (26.3) | 25 (24.3) | 0.40 |
| 3 | 78 (23.4) | 17 (28.8) | 38 (22.2) | 23 (22.3) | 0.40 |
| Left main | 11 (3.3) | 2 (3.4) | 8 (4.7) | 1 (1.0) | 0.27 |
| Procedural variables | |||||
| DES:BMS | 80:162 (33:67) | 11:26 (29.7:70.3) | 45:79 (36.3:63.7) | 24:57 (29.6:70.4) | 0.75 |
| Mean number of stents | 1.32 ± 0.65 | 1.41 ± 0.72 | 1.37 ± 0.69 | 1.21 ± 0.52 | 0.14 |
| Mean stent diameter,mm | 3.05 ± 0.64 | 3.03 ± 0.72 | 3.13 ± 0.57 | 2.94 ± 0.69 | 0.11 |
| Stent length,mm | 21.7 ± 6.9 | 21.4 ± 7.3 | 22.4 ± 7.1 | 20.8 ± 6.4 | 0.25 |
| Clinical outcomes | |||||
| All-cause mortality | 4 (1.2) | 0 (0) | 2 (1.2) | 2 (1.9) | 0.27 |
| Congestive heart failure | 10 (3.0) | 2 (3.4) | 3 (1.8) | 5 (4.9) | 0.43 |
| Major arrhythmic event | 24 (7.2) | 1 (1.7) | 17 (9.9) | 6 (5.8) | 0.32 |
| Cardiogenic shock | 15 (4.5) | 0 (0) | 9 (5.3) | 6 (5.8) | 0.12 |
STEMI: ST-elevation myocardial infarction; NSTEMI: Non ST-elevation myocardial infarction; DES: Drug eluting stent; BMS: Bare metal stent.
Overall in-hospital mortality was low with 4 deaths (1.2%). Three patients died due to complications of AMI whereas the 4th patient died of in-hospital sepsis. The incidence of heart failure was 3% and cardiogenic shock was 4.5%. Only 10 patients (3%) required intraaortic balloon counterpulsation for hemodynamic support. The incidence of major arrhythmia events was 7.2%.
Subgroup analysis by ethnicity
Figure 1 shows the relative risk of each ethnic group for developing AMI in relation to racial composition in the general population. Indians have a 3-fold risk of developing AMI before age of 46 compared to Malays (1.25-fold risk) and Chinese (0.7-fold risk) respectively. As shown in Table 1, there was no significant difference between the 3 ethnic groups with regards to antecedent cardiovascular risk factors. Indians were however more likely to be diagnosed with new-onset diabetes mellitus at presentation and also, have the highest Hba1c values in pre-existing diabetics when compared with the other ethnic groups. On the other hand, Malays were more likely to be diagnosed with new-onset hypertension at presentation when compared to the rest. As shown in Table 2, there was no significant difference among the 3 ethnic groups in terms of clinical presentation and severity of CAD by coronary angiography. The incidence of in-hospital major complications and in-hospital mortality also did not differ between the 3 ethnic groups. Although there were ethnic differences in the mean left ventricular function (Table 1), this did not translate to any significant difference in the clinical outcomes.
Figure 1.
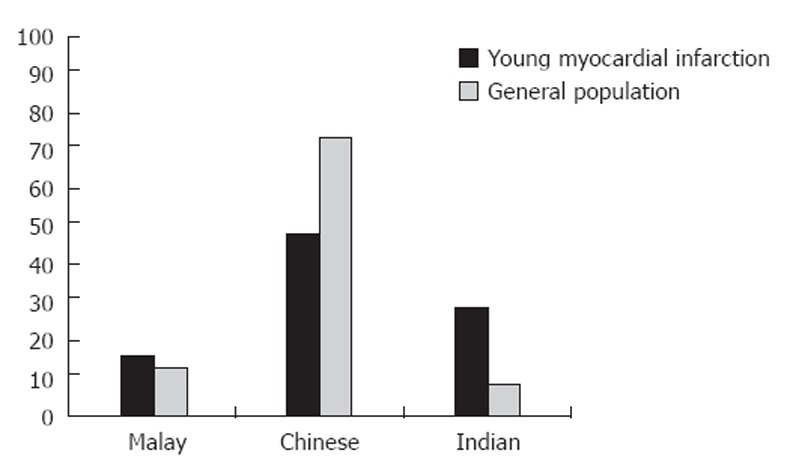
Relative risk of premature acute myocardial infarction of different ethnic groups in relation to racial composition in the general population.
DISCUSSION
To our knowledge, this is the largest cross-sectional study looking at the clinical profile of young adults with AMI in the Southeast Asian region. Young adults represented 8%-12% of all AMIs during the 5-year study period. Our study demonstrated that young adults with AMI in Singapore are characterized by male predominance, high incidence of smoking and obesity. This is consistent with findings of prior studies[1-12] in which young patients are more likely to be male, have a history of smoking and hyperlipidemia but less likely to have other co-morbidities. Smoking remains the single most important modifiable risk factor in causing premature MI in all the reported studies[1-12,14]. This is also confirmed in our study as 74% of our patients had history of tobacco use. The other common risk factors are antecedent hyperlipidemia and hypertension with varying rates of prevalence reported in different studies. In our study, 28.5% of patients had antecedent hypertension and 20% had antecedent hyperlipidemia. On the other hand, 16.5% of patients had antecedent diabetes mellitus and this rate is relatively high (> 10%) when compared to other studies. Obesity is also a common risk factor in our patients as 37% were found to be obese at presentation. Both these risk factors are likely a reflection of the rising rate of metabolic syndrome[15,16] in Asia which is increasingly recognised as a growing public health problem.
Previous studies[1-11] have shown that young patients demonstrated less extensive CAD on coronary angiogram ie the majority of patients had single vessel disease. This was also true for our cohort of patients, however, the percentage of single vessel disease was < 50% in our study. On the other hand, the percentages of two vessel disease and triple vessel disease were relatively higher, 26% and 23.4% respectively. These angiographic features suggest that our overall cohort of patients have relatively “extensive” CAD at presentation when compared to patients described in prior studies. This finding have potential implications as it suggests our patients might be at higher risk for future major adverse cardiac events if risks factors are not optimally controlled. They also would have a higher likelihood of needing multi-vessel PCI or coronary artery bypass surgery if the CAD progressed.
As for in-hospital clinical outcomes, only 4 patients (1.2%) died during the index hospitalisation. The incidence of heart failure and cardiogenic shock were 3% and 4.5% respectively. Our findings are consistent with results of prior studies[1-11] which had shown favourable clinical outcomes for young adults with AMI. This is possibly due to better cardiac reserve for young patients (who have less co-morbidities) with a better capacity to recover from acute cardiac injury than older patients.
Our study is also one of the few studies[11,12,17] to examine whether there were ethnic differences in clinical features and outcomes in a multi-ethnic population for premature AMI. A local study (inclusive of residents aged 20 to 64 years old) by Mak et al[18] had shown that the MI event rates rate for Indians and Malays were much higher than Chinese with overall rate ratios of 3.1 and 2.1 respectively. We extended this previous observation in a much younger patient population and demonstrated that Indians have a 3-fold risk of developing premature AMI in comparison to the other ethnic groups. Prior studies[18-22] have shown that Indians have at least double the risk of CAD than than of white patients after adjustment of risk factors. The causes of this ethnic predisposition to CAD are likely to be multi-factorial ie interaction between genetic and environmental factors. The role of inherited predisposition to coronary thrombosis is limited to certain genetic factors as shown by a recent study[23] in young north Indian survivors of AMI. More importantly, several studies[19-22] have shown that Indians are prone to developing metabolic abnormalities at a lower BMI and lower waist circumference. They were also found to have high serum levels of apolipoprotein B (which forms low density lipoprotein) and triglycerides and demonstrated low levels of apolipoprotein A1 and high density lipoprotein. All these factors lead to incremental risk of having metabolic syndrome which acts as a “fertile ground” for the development of diabetes mellitus and premature CAD in Indians.
In our study, Indians were more likely to be diagnosed with new-onset diabetes mellitus whereas Malays were more likely to be diagnosed with new-onset hypertension at presentation when compared to other ethnic groups. The former also had poorly controlled diabetes mellitus in those with pre-existing diabetes mellitus. This suggests subtle differences in the risk factor profile for each ethnic group and can help tailor the focus of primary preventive measures.
There were several limitations to our study. Although our sample size was relatively large, our study was a retrospective non-randomised study from a tertiary referral center, hence, selection bias was inevitable and would impact on our findings. Family history do play an important role in contributing to premature CAD but we were not able to evaluate this association adequately in our study due to lack of query/documentation in medical records.
We found that young adults with AMI in Singapore are characterized by male predominance, high incidence of smoking and obesity. Overall in-hospital clinical outcomes are favourable. Among the 3 ethnic groups, Indians have the highest risk of developing premature AMI. Primary preventive measures with special focus on smoking cessation and early screening for modifiable risk factors of CAD remain the best strategy to prevent AMI in young adults in Singapore. Obesity is a growing problem which needs to be tackled aggressively with early intervention programs. Further studies are needed to assess the long term clinical outcomes of this group of patients with possible genetic studies to look into each ethnic predisposition for premature CAD.
COMMENTS
Background
Acute myocardial infarction (AMI) is a major cause of morbidity and mortality worldwide. The burden of AMI can be substantial if the individual is relatively young as they are commonly breadwinners of the family and in the prime of their working life with significant contributions to the society. Several studies have described the clinical profiles and outcomes of young adults with AMI but there is limited data on the clinical features of young adults with AMI in the Southeast Asian region.
Research frontiers
The authors therefore sought to investigate the clinical characteristics, angiographic findings and clinical outcomes (in-hospital) of young adults with AMI in Singapore. As Singapore is a multi-ethnic society, the authors also analysed whether ethnic differences exist between the three dominant ethnic groups, Malay, Chinese and Indian with regards to the clinical features.
Applications
The study results showed that young adults with AMI in Singapore are characterized by male predominance, high incidence of smoking and obesity. Overall in-hospital clinical outcomes are favourable. Among the 3 ethnic groups, Indians have the highest risk of developing premature AMI. Primary preventive measures with special focus on smoking cessation and early screening for modifiable risk factors of coronary artery disease remain the best strategy to prevent AMI in young adults in Singapore. Obesity is a growing problem which needs to be tackled aggressively with early intervention programs. Further studies are needed to assess the long term clinical outcomes of this group of patients with possible genetic studies to look into each ethnic predisposition for premature AMI.
Terminology
AMI: Commonly known as a heart attack, results from interruption of blood supply to a part of the heart, causing heart cells to die. This is most commonly due to blockage of a coronary artery which can cause damage or death (infarction) of heart muscle tissue if left untreated for a sufficient period of time; Coronary angiography: A special X-ray evaluation (invasive procedure) of the coronary arteries in which dye is injected down the coronary arteries. The arteries then show up clearly on an X-ray and the exact site and severity of any narrowing of the coronary arteries can be identified; Low density lipoprotein: Commonly known as “bad cholesterol”particles which drive progression of atherosclerosis leading to adverse cardiovascular events and death; High density lipoprotein: Commonly known as “good cholesterol”particles. Higher levels are associated with fewer adverse cardiovascular events and death; Heart failure: The inability of the heart to provide sufficient pump action to distribute blood flow to meet the needs of the body; Cardiogenic shock: Caused by the failure of the heart to pump effectively and is defined by sustained hypotension with tissue hypoperfusion despite adequate left ventricular filling pressure.
Peer review
The authors have performed an interesting descriptive study investigating baseline clinical characteristics and in-hospital outcomes in a total of 333 young AMI patients in Singapore. The authors should be complimented for providing thorough baseline clinical data, angiographic findings and clinical outcomes. The study findings adds important data to the existing literature on premature AMI as data from Southeast Asian region is scarce.
Footnotes
Peer reviewers: Tommaso Gori, MD, PhD, II Medizinische Klinik, Universitätsmedizin der Johannes Gutenberg Universitats Mainz, 55131 Mainz, Germany; Erik Lerkevang Grove, MD, PhD, Department of Cardiology, Aarhus University Hospital, Skejby, Brendstrupgaardsvej 100, DK-8200 Aarhus, Denmark
S- Editor Cheng JX L- Editor A E- Editor Zheng XM
References
- 1.Zimmerman FH, Cameron A, Fisher LD, Ng G. Myocardial infarction in young patients: angiographic characterization, risk factors and prognosis (Coronary Artery Surgery Study Registry) J Am Coll Cardiol. 1995;26:654–661. doi: 10.1016/0735-1097(95)00254-2. [DOI] [PubMed] [Google Scholar]
- 2.Kanitz MG, Giovannucci SJ, Jones JS, Mott M. Myocardial infarction in young adults: risk factors and clinical features. J Emerg Med. 1996;14:139–145. doi: 10.1016/0736-4679(95)02089-6. [DOI] [PubMed] [Google Scholar]
- 3.Moccetti T, Malacrida R, Pasotti E, Sessa F, Genoni M, Barlera S, Turazza F, Maggioni AP. Epidemiologic variables and outcome of 1972 young patients with acute myocardial infarction. Data from the GISSI-2 database. Investigators of the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI-2) Arch Intern Med. 1997;157:865–869. [PubMed] [Google Scholar]
- 4.Doughty M, Mehta R, Bruckman D, Das S, Karavite D, Tsai T, Eagle K. Acute myocardial infarction in the young--The University of Michigan experience. Am Heart J. 2002;143:56–62. doi: 10.1067/mhj.2002.120300. [DOI] [PubMed] [Google Scholar]
- 5.Choudhury L, Marsh JD. Myocardial infarction in young patients. Am J Med. 1999;107:254–261. doi: 10.1016/s0002-9343(99)00218-1. [DOI] [PubMed] [Google Scholar]
- 6.Egred M, Viswanathan G, Davis GK. Myocardial infarction in young adults. Postgrad Med J. 2005;81:741–745. doi: 10.1136/pgmj.2004.027532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ismail J, Jafar TH, Jafary FH, White F, Faruqui AM, Chaturvedi N. Risk factors for non-fatal myocardial infarction in young South Asian adults. Heart. 2004;90:259–263. doi: 10.1136/hrt.2003.013631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chua SK, Hung HF, Shyu KG, Cheng JJ, Chiu CZ, Chang CM, Lin SC, Liou JY, Lo HM, Kuan P, et al. Acute ST-elevation myocardial infarction in young patients: 15 years of experience in a single center. Clin Cardiol. 2010;33:140–148. doi: 10.1002/clc.20718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pineda J, Marín F, Roldán V, Valencia J, Marco P, Sogorb F. Premature myocardial infarction: clinical profile and angiographic findings. Int J Cardiol. 2008;126:127–129. doi: 10.1016/j.ijcard.2007.02.038. [DOI] [PubMed] [Google Scholar]
- 10.Colkesen AY, Acil T, Demircan S, Sezgin AT, Muderrisoglu H. Coronary lesion type, location, and characteristics of acute ST elevation myocardial infarction in young adults under 35 years of age. Coron Artery Dis. 2008;19:345–347. doi: 10.1097/MCA.0b013e3283030b3b. [DOI] [PubMed] [Google Scholar]
- 11.Tambyah PA, Lim YT, Choo MH. Premature myocardial infarction in Singapore--risk factor analysis and clinical features. Singapore Med J. 1996;37:31–33. [PubMed] [Google Scholar]
- 12.Chan MY, Woo KS, Wong HB, Chia BL, Sutandar A, Tan HC. Antecedent risk factors and their control in young patients with a first myocardial infarction. Singapore Med J. 2006;47:27–30. [PubMed] [Google Scholar]
- 13.WHO expert consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 14.Barbash GI, White HD, Modan M, Diaz R, Hampton JR, Heikkila J, Kristinsson A, Moulopoulos S, Paolasso EA, Van der Werf T. Acute myocardial infarction in the young--the role of smoking. The Investigators of the International Tissue Plasminogen Activator/Streptokinase Mortality Trial. Eur Heart J. 1995;16:313–316. [PubMed] [Google Scholar]
- 15.Pan WH, Yeh WT, Weng LC. Epidemiology of metabolic syndrome in Asia. Asia Pac J Clin Nutr. 2008;17 Suppl 1:37–42. [PubMed] [Google Scholar]
- 16.Misra A, Khurana L. The metabolic syndrome in South Asians: epidemiology, determinants, and prevention. Metab Syndr Relat Disord. 2009;7:497–514. doi: 10.1089/met.2009.0024. [DOI] [PubMed] [Google Scholar]
- 17.Albarak J, Nijjar AP, Aymong E, Wang H, Quan H, Khan NA. Outcomes in young South Asian Canadians after acute myocardial infarction. Can J Cardiol. 2012;28:178–183. doi: 10.1016/j.cjca.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 18.Mak KH, Chia KS, Kark JD, Chua T, Tan C, Foong BH, Lim YL, Chew SK. Ethnic differences in acute myocardial infarction in Singapore. Eur Heart J. 2003;24:151–160. doi: 10.1016/s0195-668x(02)00423-2. [DOI] [PubMed] [Google Scholar]
- 19.Dhawan J, Bray CL, Warburton R, Ghambhir DS, Morris J. Insulin resistance, high prevalence of diabetes, and cardiovascular risk in immigrant Asians. Genetic or environmental effect? Br Heart J. 1994;72:413–421. doi: 10.1136/hrt.72.5.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McKeigue PM. Metabolic consequences of obesity and body fat pattern: lessons from migrant studies. Ciba Found Symp. 1996;201:54–64; discussion 64-67, 188-193. doi: 10.1002/9780470514962.ch4. [DOI] [PubMed] [Google Scholar]
- 21.Enas EA, Mohan V, Deepa M, Farooq S, Pazhoor S, Chennikkara H. The metabolic syndrome and dyslipidemia among Asian Indians: a population with high rates of diabetes and premature coronary artery disease. J Cardiometab Syndr. 2007;2:267–275. doi: 10.1111/j.1559-4564.2007.07392.x. [DOI] [PubMed] [Google Scholar]
- 22.Ranjith N, Pegoraro RJ, Naidoo DP, Esterhuizen TM. Metabolic syndrome in young Asian Indian patients with myocardial infarction. Cardiovasc J Afr. 2007;18:228–233. [PMC free article] [PubMed] [Google Scholar]
- 23.Dogra RK, Das R, Ahluwalia J, Kumar RM, Talwar KK. Prothrombotic gene polymorphisms and plasma factors in young north Indian survivors of acute myocardial infarction. J Thromb Thrombolysis. 2012:Apr 26; Epub ahead of print. doi: 10.1007/s11239-012-0734-6. [DOI] [PubMed] [Google Scholar]


