Abstract
Background
We sought to identify early risk factors for work disability compensation prior to and after carpal tunnel syndrome (CTS) surgery, and to determine whether pre-surgery disability compensation is associated with long-term disability.
Methods
Washington State workers’ compensation administrative data and data from interviews with workers 18 days (median) after submitting new workers’ compensation claims for CTS were examined. Baseline risk factors for pre-surgery disability compensation and for long-term disability (≥365 days of work disability compensation prior to two years after claim filing) were evaluated for workers who underwent CTS surgery and had at least one day of disability compensation (N=670).
Results
After adjustment for baseline long-term disability risk factors, workers with pre-surgery disability compensation had over five times the odds of long-term disability. Baseline factors in multiple domains, including job, psychosocial, clinical, and worker pain and function, were associated with both pre-surgery disability compensation and long-term disability.
Conclusions
Risk factors for work disability prior to and after CTS surgery are similar, and early work disability is a risk factor for long-term CTS-related disability. An integrated approach to CTS-related disability prevention could include identifying and addressing combined risk factors soon after claim filing, more efficient use of conservative treatments and appropriate work modifications to minimize early work loss, and, when indicated, timely surgical intervention.
Keywords: carpal tunnel syndrome (CTS), workers’ compensation, surgery, disability compensation, disability, work, occupational diseases
INTRODUCTION
Carpal tunnel syndrome (CTS) in workers’ compensation settings is associated with substantial work productivity loss and costs [Silverstein and Adams, 2007; Foley et al., 2007; Silverstein et al., 2010; Cheadle et al., 1994]. Previous studies have sought to identify risk factors for CTS-related work disability, with the aim of reducing disability by targeting interventions toward workers at highest risk. These studies have identified risk factors in multiple domains, including job physical demands, other workplace factors, worker psychosocial characteristics, and worker clinical characteristics [Turner et al., 2007]. Similar results have been reported in community-based CTS studies [Katz et al., 1997; Katz et al., 1998; Katz et al., 2005].
Carpal tunnel release surgery may be indicated for individuals with clinical and electro-diagnostic evidence of CTS whose symptoms have not improved with conservative treatment [Maggard et al., 2010; WA DLI IIMAC, 2009]. There is increasing evidence that surgery in these patients may be more effective than continued conservative management in alleviating symptoms and improving work disability outcomes [Gerritsen et al., 2002; Shin et al., 2000; Jarvik et al., 2009; Hui et al., 2005]. The timing of CTS surgery may be important; delay in surgery may lead to an increased duration of lost-work compensation [Daniell et al., 2009].
Missed work after CTS surgery as part of the immediate recovery phase may be expected [WA DLI IIMAC, 2009], but the significance of missed work before CTS surgery is unclear. Early missed work has been identified as a risk factor for self-reported absence from work at six and 18 months in community-based CTS studies, which included CTS surgery patients [Katz et al., 1997; Katz et al., 1998]. Katz et al. found that commonly reported reasons for early missed work included symptom interference with work and no employer offer of job accommodations [Katz et al., 1998]. However, little is known about why some workers who undergo CTS surgery have work disability prior to surgery while others do not. Furthermore, little is known about the extent to which disability compensation for missed work prior to CTS surgery is associated with long-term work disability.
To help fill these gaps in knowledge, we used data from a population-based, longitudinal cohort study of workers with new workers’ compensation claims for CTS [Turner et al., 2004]. We examined the subset of workers who underwent CTS surgery within one year after claim filing and received work disability compensation in the first two years after claim filing. Our objectives were to: (1) identify factors early in the claim that are associated with pre-surgery disability compensation; (2) identify factors early in the claim that are associated with long-term disability; and (3) determine whether pre-surgery disability compensation is associated with long-term disability. We expected that early risk factors for pre-surgery disability compensation would be similar to those for long-term disability, and we hypothesized that pre-surgery disability compensation would be associated with long-term disability, even after adjusting for other important risk factors for long-term disability.
MATERIALS AND METHODS
Study Participants and Procedures
The sample for this study was a subset of participants in the Washington State Workers’ Compensation Disability Risk Identification Study Cohort (D-RISC), a prospective, population-based study designed to identify risk factors for long-term work disability due to musculoskeletal disorders [Turner et al., 2004]. In D-RISC, the Washington State Department of Labor and Industries (DLI) State Fund workers’ compensation claims database was reviewed weekly from July 2002 through May 2004 to identify workers aged 18 years and older who had submitted a new CTS claim. The State Fund insures about two thirds of non-federal Washington State workers. The other one third of workers, who are covered by larger self-insured companies, was excluded from the study due to insufficient administrative data. Trained interviewers telephoned potentially eligible workers; confirmed eligibility (age 18 years or older, recent submission of workers’ compensation claim for hand/wrist symptoms, ability to complete telephone interview in English or Spanish); obtained informed consent from eligible workers; and conducted computer-assisted telephone interviews in English or Spanish. Study participants’ medical records were reviewed by a study nurse, who verified that the participant had CTS. The study was approved by the University of Washington institutional review board, and all participants provided informed consent. Workers were paid $10 for completing the interview.
For the current study, we applied further exclusion criteria in order to obtain the analysis sample. We excluded D-RISC CTS participants who had a workers’ compensation claim that was ultimately not accepted, who had CTS surgery before the baseline interview, who did not have CTS surgery within the first year after claim filing, who had no disability compensation days up to two years after claim filing, and who had missing data on variables analyzed for this study. Figure 1 shows the number of participants excluded for each reason.
Figure 1.
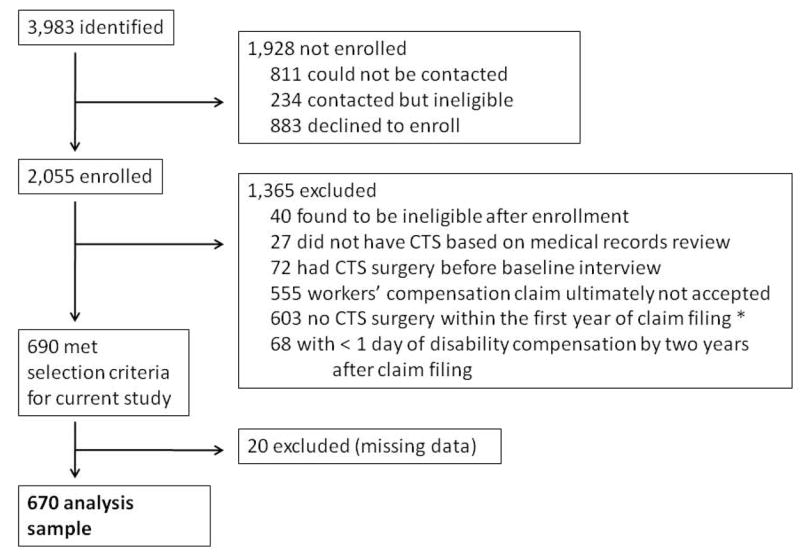
Study Profile
* 97% of participants who had surgery after claim filing had surgery within the first year.
As reported previously [Turner et al., 2007], comparisons of D-RISC CTS participants (those who were enrolled, whose claims were accepted for CTS, and who had at least one day of work disability compensation) and nonparticipants (those who could not be contacted or declined to participate but whose claims were accepted for CTS and who had at least one day of work disability compensation) indicated that participants were slightly older on average and had a larger proportion of females. However, participants did not differ from non-participants in the proportion with 180 or more days of work disability compensation in the year after claim filing, an outcome examined in secondary analyses in the present study.
Measures
Potential risk factors for pre-surgery and long-term CTS-related work disability compensation were assessed through the baseline worker interviews and by examination of data obtained from DLI databases. The interview was translated into Spanish by an accredited translator, and this version was used with Spanish-speaking participants. In the absence of any prior reports of risk factors for pre-surgery disability compensation, previously reported risk factors for long-term CTS-related disability [Adams et al., 1994; Daniell et al., 2009; Katz et al., 1997; Katz et al., 1998; Katz et al., 2005] were selected for evaluation as potential risk factors for both pre-surgery and long-term disability compensation. In addition, factors that we previously found to be associated with ≥180 CTS-related work disability days in the year after claim filing in the study sample from which the subsample for the current study was drawn [Turner et al., 2007] were examined. Baseline factors were grouped into five domains, as indicated in the following sections.
Baseline socio-demographic characteristics
During the baseline interview, workers provided information about socio-demographic characteristics. For the present study, age, gender, race, ethnicity, and education level were examined.
Baseline job factors
We examined worker-reported information on various job-related characteristics. This information included whether their employer had offered them some type of job accommodation (e.g., light duty, part-time work, special equipment) to allow them to work. Job physical demands questions were adapted from a checklist developed to assess ergonomic risk factors for upper extremity disorders [Keyserling et al., 1993; Silverstein et al., 1997] and included a question asking the worker to characterize his/her job as sedentary (sitting most of the time, occasionally moving up to a 10-pound load); light (walking or standing more than one-third of the time, often moving up to 10 pounds); medium (often moving up to 25 pounds, sometimes up to 50 pounds); heavy (often moving up to 50 pounds, sometimes up to 100 pounds); or very heavy (often moving over 50 pounds, sometimes over 100 pounds). Job psychosocial condition questions were adapted from the Psychosocial Job Demands and Supervisor Social Support scales of the Job Content Questionnaire [Karasek et al., 1998]. Workers were read several statements (that their job is very hectic, requires working very fast, they are asked to do an excessive amount of work, they can take a break when they want to, they have enough time to get the job done, and their supervisor is willing to listen to their work-related problems) and asked whether they disagreed strongly, disagreed, agreed, or agreed strongly with each. Workers were also asked how satisfied they were overall with their job (not at all, not too satisfied, somewhat, or very satisfied). Information on industry (Standard Industry Classification system) and occupation (Standard Occupational Classification system) was obtained from a Washington State DLI administrative database.
Baseline worker psychosocial characteristics
Worker mental health was assessed using the Mental Health scale of the Short Form-36 version 2 (SF-36v2) [Ware et al., 2000], a valid and reliable quality of life measure that is scored based on general US population norms (lower scores indicate psychological distress). For Spanish-speaking participants, the U.S. Spanish SF-36v2 Mental Health scale was used [Ware et al., 2000]. Catastrophizing was assessed using three questions, scored on 0-4 scales, from the Pain Catastrophizing Scale [Sullivan et al., 1995]. Ratings from questions about thoughts that pain can no longer be tolerated, that it is awful and overwhelming, and the desire to make pain stop were averaged (higher scores indicate greater catastrophizing). Questions from the Vermont Disability Prediction Questionnaire [Hazard et al., 1996] were used to assess workers’ recovery expectations [certainty that they would be working in 6 months (0–10 scale from ‘not at all certain’ to ‘extremely certain’)] and relations with co-workers (0–10 scale from ‘don’t get along well at all’ to ‘get along extremely well’). Work fear-avoidance was assessed using two items from the Fear Avoidance Beliefs Questionnaire (FABQ) work scale [Waddell et al., 1993]. Workers rated on a scale from 0 to 6 their agreement with statements that their work might be harmful to their condition and that their work makes or might make their pain worse. The two ratings were averaged (higher scores indicate higher work fear-avoidance).
Baseline pain and function
At the baseline interview, workers rated their average pain intensity in the past week on a scale of 0 to 10, where 0 is “no pain” and 10 is “pain as bad as could be.” In separate questions, workers rated the extent to which pain interfered with their ability to work on a scale of 0 (“no interference”) to 10 (“unable to carry on any activities”) and reported the number of work days missed for wrist symptoms in the year prior to submitting the workers’ compensation claim. Workers completed the Carpal Tunnel Syndrome Assessment Questionnaire (CTSAQ) Functional Status (FS) scale, which has been shown to be valid, reliable, and responsive to clinical change [Levine et al., 1993]. CTSAQ FS scores were categorized into quartiles based on the distribution in the analysis sample, with higher quartiles indicating worse symptoms and function. Workers also completed the CTSAQ Symptom Severity scale [Levine et al., 1993], which was not analyzed in this study due to its known high correlation with the CTSAQ FS scale [Turner et al., 2007].
Baseline clinical and healthcare characteristics
During the baseline interview, workers provided information about the date of current CTS symptom onset, whether symptoms were unilateral or bilateral, prior episodes involving similar (CTS-like) symptoms, long-term medical conditions, and height and weight. Body mass index (BMI) was calculated by dividing workers’ self-reported weight in kilograms by the square of their self-reported height in meters. BMI was categorized as underweight/normal/overweight (BMI < 30) and obese (BMI ≥ 30). Workers completed the Alcohol Use Disorders Identification Test-C (AUDIT-C), a validated screening instrument for alcohol problems [Bush et al., 1998]. Scores on the AUDIT-C range from 0 to 12 and were categorized as less than four (moderate alcohol use or less) or four and higher (heavy alcohol use). Workers were also asked about current use of tobacco products (cigarettes, cigars, pipes, or chewing tobacco) and responses were categorized as never or occasionally/frequently/daily. Information on the medical specialty of the first provider seen for the current CTS claim was obtained from a Washington State DLI administrative database.
CTS surgery
CTS surgery was defined using current procedural terminology (CPT) codes for carpal tunnel release surgery (29848, 64721) obtained from administrative records of medical bills.
Outcomes: pre-surgery disability compensation and long-term disability
Information about disability compensation payments was obtained from DLI databases. In Washington State, workers receive temporary total disability compensation after missing at least four days of work due to the work-related injury or condition. Disability compensation payments are stopped when the worker returns to work or is judged to be medically stable. For this study, we defined pre-surgery disability compensation (a dichotomous variable) as any disability compensation payments beginning prior to 7 days before the date of the first CTS surgery. We defined long-term disability as 365 or more disability compensation days prior to two years after claim filing.
Statistical analysis
Descriptive statistics were used to summarize job and worker characteristics. Logistic regression models were used to examine bivariate associations between baseline variables and pre-surgery disability compensation. Next, separate multivariable logistic regression models were constructed for each domain of variables (socio-demographic, job, worker psychosocial, pain and function, and clinical and healthcare) in order to identify the baseline risk factors within each domain that independently predicted pre-surgery disability compensation. Variables that had a P-value ≤ 0.20 in these models were entered together into a single multi-domain logistic regression model. P-values < 0.05 in the multi-domain logistic regression model were considered statistically significant. This procedure was repeated for the long-term disability outcome. In addition, pre-surgery disability compensation was added to the final multi-domain model of long-term disability to determine whether pre-surgery disability compensation is an independent risk factor for long-term disability.
Several planned sensitivity analyses were performed. First, regression analyses were repeated with the inclusion of more specific variables describing job physical demands and job psychosocial conditions, which were available from the baseline interview. Overall job physical demands and job satisfaction were examined in primary analyses, and more specific job physical demands (pinching fingers, wrist bending, and forearm twisting) and psychosocial conditions (hectic job, fast work, excessive work, supervisor who listens, able to take breaks) were examined in sensitivity analyses. Second, analyses were repeated with pre-surgery disability compensation defined as first disability compensation occurring up to one day and up to three days, rather than up to one week, before the date of the first CTS surgery. Third, pre-surgery and long-term disability analyses were repeated with the addition of a variable reflecting time from claim filing to surgery. Fourth, long-term disability analyses were repeated using 180 or more disability compensation days instead of 365 or more days up to two years after claim filing. Finally, long-term disability analyses were repeated using only disability compensation days between surgery and two years after claim filing (i.e., excluding disability compensation days before surgery). All analyses were performed using STATA 10 (StataCorp. College Station, TX).
RESULTS
Sample Characteristics
Among the 670 study participants in the analysis sample, the mean age was 44.9 years [standard deviation (SD) 9.6 years], 38% were male, 47% had some education beyond high school, and 81% described their race/ethnicity as white non-Hispanic. Seventeen interviews were conducted in Spanish. The largest proportion of participants (29%) worked in the Services industry, followed by 18% in Retail Trade, 12% in Construction, and 12% in Manufacturing. Common occupations included Office and Administrative Support (16%), Production (12%), and Construction and Extraction (10%). Eighty-three percent of study participants reported bilateral CTS symptoms, and 73% reported having no other major medical conditions. The median symptom duration prior to claim filing for those with complete data on the month and year of symptom onset (n=560) was 5.2 [interquartile range (IQR), 2.0-14.3] months. The median number of days between claim filing and the baseline interview was 18 (IQR, 15-24).
Thirty percent of the study sample (n=204) had pre-surgery disability compensation. There was no significant difference in the number of months between workers’ compensation claim filing and surgery for workers with pre-surgery disability compensation (median 4.1; IQR, 2.6-6.0) versus those without pre-surgery disability compensation (median 3.8; IQR, 2.6-5.9). Among those with pre-surgery disability compensation, the median number of disability compensation days prior to surgery was 78 (IQR, 35-134), and only 11 of these workers had fewer than seven days of disability compensation prior to surgery. The great majority (n = 420, 90%) of the 466 workers without pre-surgery disability compensation began their disability compensation on the day of surgery.
The median number of disability compensation days up to two years was 242 (IQR, 138-413) for workers with pre-surgery disability compensation but only 48 (IQR, 26-87) for workers without pre-surgery disability compensation. A significantly larger proportion of workers with pre-surgery compensation, as compared to workers without pre-surgery disability compensation, was receiving disability compensation at two years after claim filing (19.1% versus 5.6%; χ2 = 29.69, P < 0.001). Similarly, a larger proportion of workers with pre-surgery disability compensation met our definition of long-term disability at two years (29.9% versus 5.2%; χ2 78.47, P < 0.001).
Risk factors for pre-surgery disability compensation
Table I shows baseline sample characteristics and their unadjusted associations with pre-surgery disability compensation. In domain-specific multivariable models, several variables were independently associated with pre-surgery disability compensation (P ≤ 0.20 level). Workers who reported having less education, a shorter job duration prior to symptom onset, greater job physical demands, low or uncertain recovery expectations, a higher number of work days missed for wrist symptoms in the past year, current tobacco use, a higher BMI, higher fear-avoidance and pain interference scores, and lower SF-36 Mental Health and AUDIT-C scores had higher odds of pre-surgery disability compensation. Older workers, workers initially seen by occupational medicine specialists and orthopedic or hand surgeons, and workers with longer symptom durations prior to claim filing had lower odds of pre-surgery disability compensation.
Table I.
Baseline job and worker characteristics, and crude associations with disability compensation before surgery and long-term work disability (N=670)
| Characteristic | No disability compensation before surgery | Disability compensation before surgery | Crude ORa (95% CI) | No long-term work disability | Long-term work disability | Crude ORa (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||||
| Total | 466 | 69.6% | 204 | 30.4% | 585 | 87.3% | 85 | 12.7% | |||
| Socio-demographic | |||||||||||
| Age (years)b | Age (years)d | ||||||||||
| ≤44 | 187 | 40.0% | 124 | 60.8% | 1.00 | 260 | 44.4% | 51 | 60.0% | 1.00 | |
| 45-55 | 183 | 39.3% | 58 | 28.4% | 0.48 (0.33,0.69) | 216 | 36.9% | 25 | 29.4% | 0.59(0.35,0.98) | |
| ≥55 | 96 | 20.6% | 22 | 10.8% | 0.35 (0.21,0.58) | 109 | 18.6% | 9 | 10.6% | 0.42(0.20,0.88) | |
| Genderc | Gender | ||||||||||
| Female | 301 | 64.6% | 116 | 56.9% | 1.00 | 364 | 62.2% | 53 | 62.4% | 1.00 | |
| Male | 165 | 35.4% | 88 | 43.1% | 1.38 (0.99,1.94) | 221 | 37.8% | 32 | 37.6% | 0.99(0.62,1.59) | |
| Race | Race | ||||||||||
| White Non-Hispanic | 378 | 81.1% | 167 | 81.9% | 1.00 | 474 | 81.0% | 71 | 83.5% | 1.00 | |
| Hispanic | 34 | 7.3% | 11 | 5.4% | 0.73 (0.36,1.48) | 41 | 7.0% | 4 | 4.7% | 0.65(0.23,1.87) | |
| Other | 54 | 11.6% | 26 | 12.7% | 1.09 (0.66,1.80) | 70 | 12.0% | 10 | 11.8% | 0.95(0.47,1.94) | |
| Educationd | Education | ||||||||||
| > HS | 234 | 50.2% | 82 | 40.2% | 1.00 | 279 | 47.7% | 37 | 43.5% | 1.00 | |
| ≤ HS | 232 | 49.8% | 122 | 59.8% | 1.50 (1.07,2.09) | 306 | 52.3% | 48 | 56.5% | 1.18(0.75,1.87) | |
| Job factors | |||||||||||
| Job duration (months)b | Job durationb | ||||||||||
| > 6 months | 428 | 91.8% | 151 | 74.0% | 1.00 | 514 | 87.9% | 65 | 76.5% | 1.00 | |
| ≤ 6 months | 38 | 8.2% | 53 | 26.0% | 3.95 (2.51,6.24) | 71 | 12.1% | 20 | 23.5% | 2.23(1.27,3.90) | |
| Employer offered job accommodations | Employer offered job accommodationsb | ||||||||||
| No/unsure | 303 | 65.0% | 141 | 69.1% | 1.00 | 373 | 63.8% | 71 | 83.5% | 1.00 | |
| Yes | 163 | 35.0% | 63 | 30.9% | 0.83 (0.58,1.18) | 212 | 36.2% | 14 | 16.5% | 0.35(0.19,0.63) | |
| Physical demandsb | Physical demandsc | ||||||||||
| Sedentary/unsure | 123 | 26.4% | 38 | 18.6% | 1.00 | 150 | 25.6% | 11 | 12.9% | 1.00 | |
| Light | 125 | 26.8% | 39 | 19.1% | 1.01 (0.61,1.68) | 144 | 24.6% | 20 | 23.5% | 1.89(0.88,4.09) | |
| Medium | 120 | 25.8% | 57 | 27.9% | 1.54 (0.95,2.49) | 150 | 25.6% | 27 | 31.8% | 2.45(1.17,5.13) | |
| Heavy | 65 | 13.9% | 34 | 16.7% | 1.69 (0.98,2.94) | 86 | 14.7% | 13 | 15.3% | 2.06(0.88,4.80) | |
| Very heavy | 33 | 7.1% | 36 | 17.6% | 3.53 (1.95,6.41) | 55 | 9.4% | 14 | 16.5% | 3.47(1.49,8.10) | |
| Overall satisfaction with jobc | Overall satisfaction with jobb | ||||||||||
| Very/somewhat satisfied | 407 | 87.3% | 167 | 81.9% | 1.00 | 510 | 87.2% | 64 | 75.3% | 1.00 | |
| Unsatisfied/unsure | 59 | 12.7% | 37 | 18.1% | 1.53 (0.98,2.39) | 75 | 12.8% | 21 | 24.7% | 2.23(1.29,3.86) | |
| Worker psychosocial | |||||||||||
| Relations with co-workers | Relations with co-workersd | ||||||||||
| Excellent | 354 | 76.0% | 150 | 73.5% | 1.00 | 449 | 76.8% | 55 | 64.7% | 1.00 | |
| Poor-medium/unsure | 112 | 24.0% | 54 | 26.5% | 1.14 (0.78,1.66) | 136 | 23.2% | 30 | 35.3% | 1.80(1.11,2.92) | |
| Catastrophizingb | Catastrophizingb | ||||||||||
| <1 | 107 | 23.0% | 24 | 12.3% | 1.00 | 122 | 20.9% | 10 | 11.8% | 100 | |
| 1-1.9 | 115 | 24.7% | 43 | 21.1% | 1.60 (0.92,2.80) | 144 | 24.6% | 14 | 16.5% | 1.19(0.51,2.77) | |
| 2-2.9 | 140 | 30.0% | 70 | 34.3% | 2.14 (1.27,3.60) | 186 | 31.8% | 24 | 28.2% | 1.57(0.73,3.41) | |
| ≥3 | 104 | 22.3% | 66 | 32.4% | 2.72 (1.59,4.63) | 133 | 22.7% | 37 | 43.5% | 3.39(1.62,7.12) | |
| Work fear-avoidanceb | Work fear-avoidanceb | ||||||||||
| Very low-moderate (< 5) | 176 | 37.8% | 41 | 20.1% | 1.00 | 203 | 34.7% | 14 | 16.5% | 1.00 | |
| High-very high (5-6) | 290 | 62.2% | 163 | 79.9% | 2.41 (1.63,3.56) | 382 | 65.3% | 71 | 83.5% | 2.70(1.48,4.90) | |
| Recovery expectationsb | Recovery expectationsb | ||||||||||
| Very high-high | 381 | 81.8% | 128 | 62.7% | 1.00 | 472 | 80.7% | 37 | 43.5% | 1.00 | |
| Low or unsure | 85 | 18.2% | 76 | 37.3% | 2.66 (1.84,3.85) | 113 | 19.3% | 48 | 56.5% | 5.42(3.37,8.72) | |
| SF-36v2 (1 week) mental healthb | SF-36v2 (1 week) mental healthb | ||||||||||
| >50 | 247 | 53.0% | 70 | 34.3% | 1.00 | 289 | 49.4% | 28 | 32.9% | 1.00 | |
| 41-50 | 121 | 26.0% | 49 | 24.0% | 1.43 (0.93,2.19) | 155 | 26.5% | 15 | 17.6% | 1.00(0.52,1.93) | |
| 31-40 | 70 | 15.0% | 52 | 25.5% | 2.62 (1.68,4.10) | 94 | 16.1% | 28 | 32.9% | 3.07(1.73,5.45) | |
| ≤30 | 28 | 6.0% | 33 | 16.2% | 4.16 (2.35,7.35) | 47 | 8.0% | 14 | 16.5% | 3.07(1.51,6.26) | |
| Pain and function | |||||||||||
| Pain intensity (past week)b | Pain intensity (past week)b | ||||||||||
| 0-4 | 104 | 22.3% | 19 | 9.3% | 1.00 | 117 | 20.0% | 6 | 7.1% | 1.00 | |
| 5-7 | 243 | 52.1% | 106 | 52.0% | 2.39 (1.39,4.10) | 314 | 53.7% | 35 | 41.2% | 2.17(0.89,5.30) | |
| 8-10 | 119 | 25.5% | 79 | 38.7% | 3.63 (2.06,6.40) | 154 | 26.3% | 44 | 51.8% | 5.57(2.30,13.52) | |
| Pain interference with work (past week)b | Pain interference with work (past week)b | ||||||||||
| 0-4 | 202 | 43.3% | 31 | 15.2% | 1.00 | 223 | 38.2% | 10 | 11.8% | 1.00 | |
| 5-10 | 264 | 56.7% | 173 | 84.8% | 4.27 (2.79,6.52) | 362 | 61.9% | 75 | 88.2% | 4.62 (2.34,9.13) | |
| Work days missed for wrist (past year)b | Work days missed for wrist (past year)b | ||||||||||
| 0 | 393 | 84.3% | 131 | 64.2% | 1.00 | 472 | 80.7% | 52 | 61.2% | 1.00 | |
| 1-29 | 53 | 11.4% | 44 | 21.6% | 2.49 (1.59,3.89) | 82 | 14.0% | 15 | 17.6% | 1.66(0.89,3.09) | |
| ≥ 30 | 20 | 4.3% | 29 | 14.2% | 4.35 (2.38,7.95) | 31 | 5.3% | 18 | 21.2% | 5.27(2.76,10.07) | |
| CTSAQ FS (score range)b | CTSAQ FS (score range)b | ||||||||||
| ≤ 25th percentile (1.0-2.3) | 143 | 30.7% | 28 | 13.7% | 1.00 | 166 | 28.4% | 5 | 5.9% | 1.00 | |
| 25-50th percentile (2.3-3.0) | 152 | 32.6% | 58 | 28.4% | 1.95 (1.18,3.23) | 189 | 32.3% | 21 | 24.7% | 3.69(1.36,10.00) | |
| 50-75th percentile (3.0-3.4) | 82 | 17.6% | 53 | 26.0% | 3.30 (1.94,5.62) | 116 | 19.8% | 19 | 22.4% | 5.44(1.97,14.98) | |
| >75th percentile (3.4-5.0) | 89 | 19.1% | 65 | 31.9% | 3.73 (2.23,6.25) | 114 | 19.5% | 40 | 47.1% | 11.65(4.46,30.42) | |
| Clinical and healthcare | |||||||||||
| Symptom duration prior to claim filingb | Symptom duration prior to claim filing | ||||||||||
| < 6 months | 177 | 38.0% | 117 | 57.4% | 1.00 | 250 | 42.7% | 44 | 51.8% | 1.00 | |
| 6-11 months | 72 | 15.5% | 30 | 14.7% | 0.63 (0.39,1.02) | 91 | 15.6% | 11 | 12.9% | 0.69(0.34,1.39) | |
| ≥ 12 months | 189 | 40.6% | 51 | 25.0% | 0.41 (0.28,0.60) | 214 | 36.6% | 26 | 30.6% | 0.69(0.41,1.16) | |
| Missing | 28 | 6.0% | 6 | 2.9% | 0.32 (0.13,0.81) | 30 | 5.1% | 4 | 4.7% | 0.76(0.25,2.26) | |
| Specialty (first provider seen)d | Specialty (first provider seen) | ||||||||||
| Primary care | 213 | 45.7% | 102 | 50.0% | 1.00 | 274 | 46.8% | 41 | 48.2% | 1.00 | |
| Orthopedic or hand Surgery | 132 | 28.3% | 40 | 19.6% | 0.63 (0.41,0.97) | 151 | 25.8% | 21 | 24.7% | 0.93(0.53,1.63) | |
| Occupational medicine | 30 | 6.4% | 12 | 5.9% | 0.84 (0.41,1.70) | 37 | 6.3% | 5 | 5.9% | 0.90(0.34,2.43) | |
| Emergency room | 8 | 1.7% | 10 | 4.9% | 2.61 (1.00,6.81) | 15 | 2.6% | 3 | 3.5% | 1.34(0.37,4.82) | |
| Other | 83 | 17.8% | 40 | 19.6% | 1.01 (0.64,1.57) | 108 | 18.5% | 15 | 17.6% | 0.93(0.49,1.75) | |
| Bilateral symptoms | Bilateral symptomsc | ||||||||||
| Yes | 387 | 83.0% | 167 | 81.9% | 1.00 | 479 | 81.9% | 75 | 88.2% | 1.00 | |
| No | 79 | 17.0% | 37 | 18.1% | 1.09 (0.71,1.67) | 106 | 18.1% | 10 | 11.8% | 0.60(0.30,1.20) | |
| Previous similar wrist problems | Previous similar wrist problems | ||||||||||
| No/unsure | 330 | 70.8% | 144 | 70.6% | 1.00 | 412 | 70.4% | 62 | 72.9% | 1.00 | |
| Yes | 136 | 29.2% | 60 | 29.4% | 1.01 (0.70,1.45) | 173 | 29.6% | 23 | 27.1% | 0.88(0.53,1.47) | |
| Number of co-morbid medical conditionsc | Number of co-morbid medical conditions | ||||||||||
| 0 | 331 | 71.0% | 156 | 76.5% | 1.00 | 429 | 73.3% | 58 | 68.2% | 1.00 | |
| ≥ 1 | 135 | 29.0% | 48 | 23.5% | 0.75 (0.52,1.10) | 156 | 26.7% | 27 | 31.8% | 1.28(0.78,2.09) | |
| Tobacco useb | Tobacco useb | ||||||||||
| Never | 322 | 69.1% | 101 | 49.5% | 1.00 | 385 | 65.8% | 38 | 44.7% | 1.00 | |
| Occasionally/frequently/daily | 144 | 30.9% | 103 | 50.5% | 2.28 (1.63,3.20) | 200 | 34.2% | 47 | 55.3% | 2.38(1.50,3.77) | |
| AUDIT-C | AUDIT-C | ||||||||||
| Moderate or less | 363 | 77.9% | 162 | 79.4% | 1.00 | 456 | 77.9% | 69 | 81.2% | 1.00 | |
| Heavy or more | 103 | 22.1% | 42 | 20.6% | 0.91 (0.61,1.37) | 129 | 22.1% | 16 | 18.8% | 0.82(0.46,1.46) | |
| BMI | BMI | ||||||||||
| ≤ 30 (underweight/normal/overweight) | 252 | 54.1% | 114 | 55.9% | 1.00 | 317 | 54.2% | 49 | 57.6% | 1.00 | |
| > 30 (obese) | 192 | 41.2% | 86 | 42.2% | 0.99 (0.71,1.39) | 246 | 42.1% | 32 | 37.6% | 0.84(0.52,1.35) | |
| Missing | 22 | 4.7% | 4 | 2.0% | 0.40 (0.14,1.19) | 22 | 3.8% | 4 | 4.7% | 1.18(0.39,3.56) | |
| Disability compensation | Disability compensationb | ||||||||||
| After surgery only | ---- | ---- | ---- | 442 | 75.6% | 24 | 28.2% | 1.00 | |||
| Pre-surgery | ---- | ---- | ---- | 143 | 24.4% | 61 | 71.8% | 7.86 (4.72, 13.06) | |||
AUDIT-C, Alcohol Use Disorders Identification Test-C; BMI, body mass index; CI, confidence interval; CTS, carpal tunnel syndrome; CTSAQ, Carpal Tunnel Syndrome Assessment Questionnaire; FS, functional status scale; HS, high school; OR, odds ratio; SF-36v2, Short Form-36 version 2.
Odds ratios and 95% confidence intervals obtained from logistic regression predicting disability compensation before surgery or long-term disability. Statistically significant effect estimates (p<0.05) are bolded.
P < 0.01,
P < 0.20, and
P < 0.05 in crude logistic regression analyses predicting disability compensation before surgery or long-term disability
Because data were missing for > 3% of participants for BMI (n=26 with missing data) and for date of symptom onset (n=34 with missing data), BMI and symptom duration categories include a “missing” category.
Five study participants were unsure of or declined to provide information on race; nine participants were unsure whether their employer offered job accommodations; five participants were unsure about job physical demands; four participants were unsure about job satisfaction; two participants were unsure about relations with co-workers; and four participants were unsure about previous wrist symptoms.
In order to identify characteristics independently associated with pre-surgery disability compensation across all domains, variables found to have a P-value ≤ 0.20 in the domain-specific models were entered into a single multi-domain logistic regression model. Seven baseline variables were statistically significant in the multi-domain model (Table II). Workers with a shorter job duration prior to claim filing, greater work fear-avoidance, greater pain interference with work, a greater number of work days missed because of wrist symptoms in the past year, and current tobacco use had higher odds of pre-surgery disability. Older workers and those with longer symptom duration prior to claim filing had lower odds of pre-surgery disability.
Table II.
Baseline risk factors in multi-domain model of pre-surgery disability compensation (N=670)
| Characteristic | OR (95% CI) | P-value |
|---|---|---|
| Socio-demographic | ||
| Age (ref. ≤44) | 0.01 | |
| 45-54 | 0.54 (0.35, 0.84) | |
| ≥55 | 0.53 (0.29, 0.98) | |
| Education (ref. >HS) | 0.99 | |
| <HS | 1.00 (0.67,1.51) | |
| Job factors | ||
| Job duration (ref. > 6 months) | <0.001 | |
| ≤ 6 months | 2.80 (1.59, 4.92) | |
| Job physical demands (ref. sedentary/unsure) | 0.09 | |
| Light | 1.16 (0.62,2.17) | |
| Medium | 1.35 (0.74,2.47) | |
| Heavy | 1.70 (0.86,3.36) | |
| Very heavy | 2.71 (1.26,5.86) | |
| Worker psychosocial | ||
| Work fear-avoidance (ref. Very low-moderate) | 0.03 | |
| High-very high | 1.66 (1.05, 2.64) | |
| Recovery expectations (ref. Very high-high) | 0.06 | |
| Low-unsure | 1.55 (0.98, 2.45) | |
| SF-36v2 (1 week) mental health (ref. >50) | 0.09 | |
| 41-50 | 1.22 (0.74,2.01) | |
| 31-40 | 1.75 (1.01,3.02) | |
| ≤30 | 2.04 (1.04, 4.00) | |
| Pain and function | ||
| Pain interference with work (past week) (ref 0-4) | 0.002 | |
| 5-10 | 2.19 (1.33, 3.60) | |
| Work days missed for wrist, past year (ref. 0) | 0.001 | |
| 1-29 | 1.97 (1.16, 3.37) | |
| ≥ 30 | 2.99 (1.48, 6.07) | |
| Clinical and healthcare | ||
| Symptom duration prior to claim filing (ref. <6 months) | 0.002 | |
| 6-11 months | 0.56 (0.32,0.99) | |
| ≥12 months | 0.40 (0.25,0.64) | |
| Missing | 0.65 (0.24,1.79) | |
| Specialty (first provider seen) (ref. primary care) | 0.21 | |
| Orthopedic or hand surgery | 0.60 (0.36, 1.00) | |
| Occupational medicine | 0.57 (0.24, 1.33) | |
| Emergency room | 1.63 (0.47, 5.62) | |
| Other | 0.86 (0.51, 1.47) | |
| Tobacco use (ref. Never) | 0.01 | |
| Occasionally/frequently/daily | 1.73 (1.13, 2.66) | |
| AUDIT-C (ref. Moderate or less) | 0.08 | |
| Heavy or more | 0.63 (0.38, 1.06) | |
| BMI (ref. ≤ 30) | 0.12 | |
| >30 | 0.62 (0.36,1.06) | |
| Missing | 0.96 (0.57,1.61) |
AUDIT-C, Alcohol Use Disorders Identification Test-C; BMI, Body Mass Index; CI, confidence interval; HS, high school; OR, odds ratio; SF-36v2, Short Form-36 version 2.
Because data were missing for > 3% of participants for BMI (n=26 with missing data) and for date of symptom onset (n=34 with missing data), BMI and symptom duration categories include a “missing” category.
Statistically significant effect estimates (p<0.05) are bolded.
Sensitivity analyses, in which models were adjusted for more specific job physical demands (pinching fingers, wrist bending, and forearm twisting) and other job psychosocial conditions (hectic job, fast work, excessive work, supervisor who listens, able to take breaks), yielded similar results. Variables significantly associated with pre-surgery disability compensation in the main analysis were also significantly associated with pre-surgery disability compensation in sensitivity analyses using one and three instead of seven days prior to surgery as the upper-bound cut-off time for pre-surgery disability compensation. About 25 workers initiated disability compensation in the week preceding surgery, of which 17 initiated compensation in the three days and 14 initiated compensation in the day prior to surgery. Timing of surgery relative to claim filing was not significantly associated with pre-surgery disability compensation when included in the final multi-domain model.
In a post hoc analysis, we explored the impact of removing conceptually and statistically related variables on the final multi-domain regression model. The most highly correlated independent variables in our analyses were pain intensity and catastrophizing (Spearman’s ρ = 0.49, P<0.01), and pain interference with work and CTSAQ FS (Spearman’s ρ = 0.48, P<0.01). Removal of the catastrophizing variable from the analyses did not have a significant impact on the final multi-domain model. However, removal of the pain interference with work variable resulted in a significant and positive association between CTSAQ FS scores and pre-surgery disability compensation in the final multi-domain model.
Risk factors for long-term disability
Crude associations of baseline sample characteristics and long-term disability are shown in Table I. Several variables were associated with long-term disability (P ≤ 0.20 level) in domain-specific multivariable models of long-term disability. Workers who reported a shorter job duration prior to symptom onset, lack of or uncertain job satisfaction, low or uncertain recovery expectations, worse relations with co-workers, a higher number of work days missed for wrist symptoms in the past year, current tobacco use, and co-morbid medical conditions, and workers who had higher catastrophizing, fear-avoidance, pain intensity, pain interference with work, and CTSAQ FS scores and lower SF-36 Mental Health scores had higher odds of long-term disability. Older workers, workers without bilateral symptoms, and workers with an offer of job accommodation from their employer by the time of the baseline interview had lower odds of long-term disability.
Five baseline variables were statistically significant in the final multi-domain model of long-term disability (Table III). Workers who reported worse relations with co-workers, had low or uncertain recovery expectations, had higher CTSAQ FS scores, and who currently used tobacco had higher odds of long-term disability. Workers with an offer of job accommodation had lower odds of long-term disability. Addition of disability compensation category (before versus only after surgery) to the final multi-domain model did not result in substantial differences in associations of baseline risk factors with long-term disability (Table III).
Table III.
Baseline risk factors for long-term disability, with and without adjustment for disability compensation category, multi-domain model (N=670)
| Characteristic | Multivariable model without adjustment for disability compensation category (pre-surgery versus only after surgery) | Multivariable model with adjustment for disability compensation category (pre-surgery versus only after surgery) | ||
|---|---|---|---|---|
|
| ||||
| OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Disability compensation (ref. after surgery only) | ||||
| Pre-surgery disability compensation | ---- | ---- | 5.38 (2.89, 10.01) | <0.001 |
| Socio-demographic | ||||
| Age (ref. ≤44) | 0.14 | 0.54 | ||
| 45-54 | 0.61 (0.33, 1.13) | 0.78 (0.41, 1.48) | ||
| ≥55 | 0.48 (0.20, 1.16) | 0.62 (0.25, 1.58) | ||
| Job factors | ||||
| Job duration (ref. > 6 months) | 0.36 | 0.74 | ||
| ≤ 6 months | 1.39 (0.69, 2.83) | 0.88 (0.42, 1.86) | ||
| Employer offered job accommodations (ref. No/unsure) | 0.002 | 0.003 | ||
| Yes | 0.35 (0.17, 0.68) | 0.34 (0.17, 0.69) | ||
| Overall satisfaction with job (ref. Very/somewhat satisfied) | 0.05 | 0.04 | ||
| Unsatisfied/unsure | 1.93 (0.99, 3.77) | 2.08 (1.03, 4.22) | ||
| Worker psychosocial | ||||
| Relations with co-workers (ref. Excellent) | 0.03 | 0.02 | ||
| Poor-medium/unsure | 1.90 (1.05, 3.44) | 2.09 (1.12, 3.89) | ||
| Catastrophizing (ref. <1) | 0.52 | 0.67 | ||
| 1-1.9 | 0.74 (0.28, 1.99) | 0.74 (0.26, 2.09) | ||
| 2-2.9 | 0.50 (0.19, 1.35) | 0.63 (0.23, 1.76) | ||
| ≥3 | 0.71 (0.25, 1.99) | 0.93 (0.31, 2.74) | ||
| Work fear-avoidance (ref. Very low-moderate) | 0.17 | 0.41 | ||
| High-very high | 1.62 (0.82, 3.21) | 1.35 (0.66, 2.74) | ||
| Recovery expectations (ref. Very high-high) | <0.001 | 0.002 | ||
| Low-unsure | 2.68 (1.52, 4.72) | 2.51 (1.39, 4.54) | ||
| SF-36v2 (1 week) mental health (ref. >50) | 0.36 | 0.16 | ||
| 41-50 | 0.56 (0.26, 1.21) | 0.48 (0.21, 1.09) | ||
| 31-40 | 0.99 (0.48, 2.04) | 0.83 (0.39, 1.77) | ||
| ≤30 | 0.66 (0.27, 1.60) | 0.42 (0.16, 1.10) | ||
| Pain and function | ||||
| Pain intensity (ref. 0-4) | 0.06 | 0.08 | ||
| 5-7 | 0.99 (0.34, 2.83) | 0.87 (0.29, 2.61) | ||
| 8-10 | 2.09 (0.67, 6.52) | 1.87 (0.57, 6.09) | ||
| Pain interference with work (past week) (ref 0-4) | 0.29 | 0.66 | ||
| 5-10 | 1.61 (0.67,3.87) | 1.23 (0.50,3.05) | ||
| Work days missed for wrist, past year (ref. 0) | 0.16 | 0.36 | ||
| 1-29 | 1.19 (0.56, 2.53) | 0.88 (0.40, 1.95) | ||
| ≥ 30 | 2.16 (0.99, 4.72) | 1.69 (0.76, 3.80) | ||
| CTSAQ FS (ref. ≤25th percentile) | 0.03 | 0.04 | ||
| 25-50th percentile (2.3-3.0) | 2.54 (0.86, 7.56) | 2.23 (0.73, 6.78) | ||
| 50-75th percentile (3.0-3.4) | 3.45 (1.09, 10.88) | 2.89 (0.89, 9.33) | ||
| >75th percentile (3.4-5.0) | 5.28 (1.70, 16.40) | 4.87 (1.53, 15.47) | ||
| Clinical and healthcare | ||||
| Bilateral symptoms (ref. Yes) | 0.46 | 0.30 | ||
| No | 0.74 (0.34, 1.63) | 0.65 (0.29, 1.47) | ||
| Number of comorbid medical conditions (ref. 0) | 0.06 | 0.15 | ||
| ≥ 1 | 1.81 (0.97, 3.36) | 1.61 (0.84, 3.07) | ||
| Tobacco use (ref. Never) | 0.03 | 0.09 | ||
| Occasionally/frequently/daily | 1.87 (1.08, 3.26) | 1.64 (0.92, 2.94) | ||
CI, confidence interval; CTSAQ, Carpal Tunnel Syndrome Assessment Questionnaire; FS, functional status scale; OR, odds ratio; SF-36v2, Short Form-36 version 2.
Statistically significant effect estimates (p<0.05) are bolded.
Sensitivity analyses in which models were adjusted for more specific job physical demands and additional job psychosocial conditions yielded similar results. Although the timing of surgery relative to claim filing was significantly associated with long-term disability (longer time to surgery associated with an increased odds of long-term disability), risk factors for long-term disability were otherwise not substantially changed with the addition of timing of surgery to the final multi-domain model. Removal of the catastrophizing variable and the pain interference with work variable from the analyses did not substantially alter associations of other covariates with long-term disability in the final multi-domain model. When long-term disability analyses were repeated using ≥ 180 instead of ≥ 365 disability compensation days within the first two years, lack of employer offer of job accommodation, worse relations with co-workers, low or uncertain recovery expectations, and tobacco use remained significantly associated with long-term disability in the final multi-domain model. In addition, higher pain intensity, shorter symptom duration, and greater number of work days missed for wrist symptoms in the past year were significantly associated with long-term disability.
In sensitivity analyses excluding disability days before surgery from the definition of long-term disability, four baseline variables were statistically significant in the final multi-domain model of long-term disability (Table IV). Workers who reported worse relations with co-workers, had low or uncertain recovery expectations, and who rated their pain intensity as greater had higher odds of long-term disability. Workers with an offer of job accommodation from their employer by the time of the baseline interview had lower odds of long-term disability. Compared to analyses in which disability days prior to surgery were included in the definition of long-term disability, tobacco use and CTSAQ FS scores were no longer significantly associated with long-term disability, but greater pain intensity was. Addition of disability compensation category (before versus only after surgery) did not result in substantial differences in associations of baseline risk factors with long-term disability.
Table IV.
Baseline risk factors for long-term post-surgery disability (365 days or greater, excluding disability days before surgery), with and without adjustment for disability compensation category(N=670)
| Characteristic | Multivariable model without adjustment for disability compensation category (pre-surgery versus only after surgery) | Multivariable model with adjustment for disability compensation category (pre-surgery versus only after surgery) | ||
|---|---|---|---|---|
|
| ||||
| OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Disability compensation (ref. after surgery only) | ||||
| Pre-surgery disability compensation | ---- | ---- | 2.94 (1.57, 5.52) | <0.001 |
| Socio-demographic | ||||
| Age (ref. ≤44) | 0.47 | 0.81 | ||
| 45-54 | 0.68 (0.35, 1.30) | 0.80 (0.41, 1.57) | ||
| ≥55 | 0.74 (0.31, 1.77) | 0.92 (0.38, 2.24) | ||
| Job factors | ||||
| Employer offered job accommodations (ref. No/unsure) | 0.01 | 0.01 | ||
| Yes | 0.38 (0.18, 0.79) | 0.38 (0.18, 0.80) | ||
| Overall satisfaction with job (ref. Very/somewhat satisfied) | 0.12 | 0.12 | ||
| Unsatisfied/unsure | 1.78 (0.86, 3.71) | 1.80 (0.85, 3.82) | ||
| Worker psychosocial | ||||
| Relations with co-workers (ref. Excellent) | 0.03 | 0.01 | ||
| Poor-medium/unsure | 2.02 (1.07, 3.83) | 2.26 (1.17, 4.35) | ||
| Catastrophizing (ref. <1) | 0.66 | 0.78 | ||
| 1-1.9 | 0.74 (0.25, 2.14) | 0.75 (0.25, 2.26) | ||
| 2-2.9 | 0.52 (0.18, 1.51) | 0.61 (0.21, 1.80) | ||
| ≥3 | 0.69 (0.23, 2.07) | 0.81 (0.26, 2.49) | ||
| Work fear-avoidance (ref. Very low-moderate) | 0.19 | 0.37 | ||
| High-very high | 1.65 (0.79, 3.45) | 1.41 (0.66, 3.00) | ||
| Recovery expectations (ref. Very high-high) | 0.005 | 0.02 | ||
| Low-unsure | 2.41 (1.31, 4.42) | 2.15 (1.15, 3.99) | ||
| SF-36v2 (1 week) mental health (ref. >50) | 0.10 | 0.06 | ||
| 41-50 | 0.44 (0.18, 1.05) | 0.41 (0.17, 1.01) | ||
| 31-40 | 1.13 (0.53, 2.41) | 0.98 (0.45, 2.13) | ||
| ≤30 | 0.52 (0.19, 1.42) | 0.38 (0.14, 1.08) | ||
| Pain and function | ||||
| Pain intensity (ref. 0-4) | 0.04 | 0.04 | ||
| 5-7 | 1.45 (0.45, 4.64) | 1.28 (0.39, 4.21) | ||
| 8-10 | 3.28 (0.94, 11.44) | 3.02 (0.85, 10.73) | ||
| Work days missed for wrist, past year (ref. 0) | 0.15 | 0.26 | ||
| 1-29 | 1.25 (0.57, 2.77) | 1.05 (0.46, 2.39) | ||
| ≥ 30 | 2.27 (0.99, 5.17) | 1.97 (0.86, 4.50) | ||
| CTSAQ FS (ref. ≤25th percentile) | 0.07 | 0.10 | ||
| 25-50th percentile (2.3-3.0) | 2.35 (0.72, 7.67) | 2.12 (0.64, 6.95) | ||
| 50-75th percentile (3.0-3.4) | 3.31 (0.96, 11.44) | 2.82 (0.81, 9.82) | ||
| >75th percentile (3.4-5.0) | 4.79 (1.41, 16.33) | 4.31 (1.26, 14.72) | ||
| Clinical and healthcare | ||||
| Tobacco use (ref. Never) | 0.05 | 0.11 | ||
| Occasionally/frequently/daily | 1.83 (1.00, 3.35) | 1.66 (0.89, 3.08) | ||
| AUDIT-C (ref. Moderate or less) | 0.14 | 0.17 | ||
| Heavy or more | 0.54 (0.24, 1.23) | 0.55 (0.24, 1.28) | ||
AUDIT-C, Alcohol Use Disorders Identification Test-C; CI, confidence interval; CTSAQ, Carpal Tunnel Syndrome Assessment Questionnaire; FS, functional status scale; OR, odds ratio; SF-36v2, Short Form-36 version 2.
Statistically significant effect estimates (p<0.05) are bolded.
Risk factors for both pre-surgery disability compensation and long-term disability
Baseline characteristics associated with higher odds of both pre-surgery disability compensation and long-term disability (P-value ≤ 0.20) in domain-specific multivariable models included younger age, shorter job duration prior to symptom onset, low or uncertain recovery expectations, higher fear-avoidance scores, lower (worse) SF-36 Mental Health scores, and tobacco use. Although the specific risk factors differed, baseline factors in job, psychosocial, clinical, and worker pain and function domains were significantly (P-value ≤ 0.05) associated with both pre-surgery disability compensation and long-term disability in multi-domain models (Tables II & III). Tobacco use was significantly associated with both pre-surgery disability compensation and long-term disability in multi-domain models, after adjustment for other baseline risk factors.
Pre-surgery disability compensation as a risk factor for long-term disability
Workers with pre-surgery disability compensation had over five times the odds of long-term disability (odds ratio 5.38; 95% confidence interval 2.89-10.01), after adjustment for baseline risk factors for long-term disability. In sensitivity analyses excluding disability compensation days before surgery from the definition of long-term disability, pre-surgery disability compensation remained significantly associated with long-term disability, although the association was attenuated (odds ratio 2.94, 95% confidence interval 1.57-5.52).
DISCUSSION
In this population-based sample of Washington State workers who underwent surgery for CTS and received workers’ compensation benefits for work loss due to CTS, baseline factors in multiple domains, including job, psychosocial, clinical, and pain and function, were associated with both pre-surgery disability compensation and long-term work disability. These results suggest that a range of factors may influence work status both before surgery and over the long-term among workers undergoing CTS surgery and support a multidimensional model of assessment of workers with CTS. After adjustment for baseline long-term disability risk factors, workers with pre-surgery disability compensation had over five times the odds of long-term disability compared to workers with no pre-surgery disability compensation. To our knowledge, this is the first study that has examined risk factors for pre-surgery disability compensation and evaluated pre-surgery disability compensation as a risk factor for long-term disability.
We found several unexpected risk factors for pre-surgery disability compensation. Younger age, shorter job duration prior to symptom onset, and shorter symptom duration prior to claim filing were all associated with pre-surgery disability compensation, even after adjustment for job physical demands, pain and function, and other factors. There have been conflicting reports of the relationship between age and risk of long-term disability in workers with CTS [Turner et al., 2007; Adams et al., 1994; Katz et al., 1997; Katz et al., 1998; Katz et al., 1996], and there is a paucity of information concerning the association of job and symptom duration with risk of long-term disability. It is possible that our findings are due to confounding by factors not captured in our study. For example, workers with newer jobs may have less flexibility in job tasks and a greater likelihood of receiving a prescription for time off work, or they may be less attached to their jobs and more receptive to missing work. Further research is needed to confirm and better understand the relationships between these factors and pre-surgery work disability related to CTS.
Contrary to our expectations, lack of employer offer of job accommodations was not significantly associated with pre-surgery disability compensation in either unadjusted or multivariable models, although the odds of pre-surgery disability compensation were lower among those offered job accommodations. It is possible that this association might have been statistically significant with a larger sample size. Nonetheless, other factors (e.g., worker psychosocial characteristics, symptom severity, and functional disability) may be more important than early employer offer of job accommodation in determining whether a worker receives compensation for work disability because of CTS early in the course of a claim.
Although the study sample comprised workers who had symptoms severe enough to warrant CTS surgery, 70% did not receive disability compensation prior to surgery. The question may be raised as to how these workers were able to remain at work before surgery, especially given that only 35% reported in the baseline interview that they had been offered job accommodations by their employer. There are several possible reasons. First, our sample included workers with a variety of job tasks, and many may have had tasks that they could continue to perform prior to surgery. Second, workers may have been offered job accommodations at some point after the baseline interview but before surgery. One possible scenario is that some workers’ symptoms may have worsened after the baseline interview, leading both to an offer of job accommodations and the decision to operate.
Our results add to the growing literature suggesting that avoidance of early work disability by offering job accommodations and facilitating participation in modified work may be a critical component of interventions to prevent long-term disability [Williams et al., 2007; Whitfill et al., 2010]. Lack of employer offer of job accommodations by the time of the baseline interview was significantly associated with greater odds of long-term disability (when defined as both ≥ 365 and ≥ 180 days of work disability compensation up to two years after claim filing) in unadjusted and multivariable models. This observation is consistent with findings in the larger D-RISC sample [Turner et al., 2007]. Although the evidence is consistent across multiple studies that early offers of job accommodations are associated with lower risks of long-term disability due to work-related back pain [Franche et al. 2005], more research is needed to establish the generalizability of this finding to other disabling work-related conditions such as CTS.
We found that worker psychosocial characteristics, assessed soon after claim submission, predicted long-term disability. Although it is not always apparent early in the course of treatment which workers with CTS will undergo surgery, early screening for psychosocial risk factors for pre-surgery work disability and post-surgery work disability may be important in preventing long-term disability. Certain worker psychosocial factors may predict long-term disability among workers with CTS regardless of whether they undergo CTS surgery [Turner et al., 2007]. Although guidelines generally recommend early screening for psychosocial risk factors in workers with back pain [Chou et al., 2007], recommendations addressing screening for psychosocial risk factors among workers with CTS are sparse. Several studies of interventions addressing fear-avoidance beliefs and recovery expectations in workers with work-related back pain have demonstrated promising effects [Godges et al., 2008; Slater et al., 2009], but the effect of interventions addressing psychosocial risk factors in workers with CTS is currently unknown.
Tobacco use was associated with an increased risk of both pre-surgery disability compensation and long-term disability in unadjusted and multi-domain models. Smoking has been reported to be a risk factor for CTS [Nathan et al., 2002; Nathan et al., 1996; Maghsoudipour et al., 2008; Gelfman et al., 2010] and is also associated with poor wound healing [Sorensen et al., 2009], which could impact successful recovery after CTS surgery. In addition, smoking is associated with psychiatric co-morbidities [Jané-Llopis et al., 2006], which may also be associated with poor outcomes. The association of smoking with pre-surgery disability compensation and long-term disability may therefore reflect confounding by these psychiatric co-morbidities. Regardless of the mechanism of this association, it is recommended that all patients be evaluated for smoking cessation counseling [USPSTF, 2010].
Our finding that pre-surgery disability compensation is a risk factor for long-term disability is consistent with previously published reports. In a prospective, community-based cohort of CTS surgery patients, self-reported pre-operative work absence was associated with self-reported work absence six months following surgery [Katz et al., 1997]. Studies of patients with work-related low back pain indicate that early return-to-work efforts are a key component of interventions aimed at reducing disability [Williams et al., 2007], perhaps because avoidance of early missed work increases worker attachment to the job/employer, reduces worker fear that work will be harmful, and confers mental health benefits. Further research is needed to determine whether avoiding pre-surgery work loss in patients with work-related CTS reduces long-term disability.
In addition to any independent effect work disability prior to CTS surgery may have on long-term disability, pre-surgery disability compensation may be an indicator of the presence of other risk factors for long-term disability. For example, in our study, pre-surgery disability compensation was associated with certain baseline worker psychosocial factors and markers of worse functional status, and factors in these domains predicted long-term disability compensation. Although pre-surgery disability compensation remained significantly associated with long-term disability after controlling for multiple other risk factors, such compensation may be a marker for other risk factors not assessed in this study. These risk factors may not be limited to patient characteristics; they may also include provider and environmental variables. Daniell et al reported that workers undergoing CTS surgery may be more likely to end disability compensation if the diagnosing provider and operating surgeon have relatively high experience with CTS claims [Daniell et al., 2009]. It is conceivable that pre-surgery disability compensation is associated with this or other provider characteristics; this should be examined in future studies. It is also plausible that workers who are not required to perform job tasks that aggravate CTS symptoms and/or have a strong attachment to the current job are less likely to miss work both before and after surgery.
The association between pre-surgery disability compensation and long-term disability appears to be independent of the timing of CTS surgery. Previous studies have suggested that a delay in surgery is associated with an increased duration of lost-work in certain CTS patients [Daniell et al., 2009], and we observed increased odds of long-term disability among patients with a longer time to surgery. However, pre-surgery disability compensation remained significantly associated with long-term disability even after adjustment for the timing of CTS surgery relative to claim filing. These findings suggest that efforts to keep workers with CTS at work, in combination with aggressively pursuing a trial of conservative therapy for CTS so that a decision about whether or not to pursue CTS surgery can be made in a timely fashion, may be important in preventing long-term CTS-related disability.
Previous research has suggested that CTS patients with moderately prolonged median nerve distal motor latencies may benefit more from carpal tunnel release surgery than those with mildly prolonged distal motor latencies [Dennerlein et al., 2002]. However, other factors, including better general physical health prior to surgery, may be stronger predictors of favorable post-surgical outcomes [Dennerlein et al., 2002]. Addressing the pre-surgery and long-term disability risk factors, including those in worker psychosocial and function domains, identified in this study as well as optimizing general health early (before surgery) may help optimize post-surgical outcomes in workers for whom surgery is indicated.
Our study has several important limitations. First, we did not include objective measures of clinical severity. However, such measures can be inaccurate and may have poor inter-rater reliability [Dale et al., 2010; Smith et al., 2010], and a lack of correlation between electro-diagnostic findings and symptoms and function has been reported [Chan et al., 2007]. Further, the relationship between electro-diagnostic findings and surgical outcomes is not straight-forward [Kouyoumdjian et al., 2003; Dennerlein et al., 2002]. Second, we did not include type of surgery (endoscopic versus open) in our analyses. Workers who undergo endoscopic CTS surgery may recover more quickly [Scholten et al., 2007]. However, type of surgery is unlikely to meaningfully impact disability outcomes [Wasiak and Pransky, 2007].
Other limitations include the possibility that important predictors of pre-surgery disability compensation and of long-term disability were not captured in our study. We did not analyze information on nonsurgical therapies or providers’ practices. It is possible that providers who remove workers from work before surgery are more likely to extend work removal for long durations when resuming care post-operatively. Finally, the extent to which our findings may generalize to patients with CTS who do not have workers’ compensation claims or those in other states or countries is unknown. Similar studies in other settings are needed. Strengths of our study include a large, population-based sample, worker self-reported measures covering multiple domains, and objective administrative measures of work disability compensation.
Conclusions
Among Washington State workers’ compensation claimants with disability compensation and surgery for CTS, pre-surgery disability compensation was a significant independent risk factor for long-term disability. Baseline factors in job, psychosocial, clinical, and worker pain and function domains were associated with both pre-surgery disability compensation and long-term disability. The results suggest directions for improving early identification of workers at risk for pre-surgery and long-term disability, and for further research investigating effective strategies for prevention of early and long-term CTS-related work disability.
Acknowledgments
Grant Sponsors: This study was funded by the Centers for Disease Control and Prevention National Institute for Occupational Safety and Health (NIOSH). Support for JTS was provided by the National Institute of Environmental Health Sciences (NIEHS).
Grant Numbers: NIOSH grant no. 1 R01 OHO4069 (“Disability Risk in Work-Related Musculoskeletal Injuries”); NIEHS grant no. T32 ES015459.
Support for JTS was provided by the Occupational Physicians Scholarship Fund.
Footnotes
Institution at which work was performed: University of Washington, Seattle, WA
Conflict of interest statement: The authors report no conflicts of interest.
References
- Adams ML, Franklin GM, Barnhart S. Outcome of carpal tunnel surgery in Washington State workers’ compensation. Am J Ind Med. 1994;25(4):527–36. doi: 10.1002/ajim.4700250407. [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Chan L, Turner JA, Comstock BA, Levenson LM, Hollingworth W, Heagerty PJ, Kliot M, Jarvik JG. The relationship between electrodiagnostic findings and patient symptoms and function in carpal tunnel syndrome. Arch Phys Med Rehabil. 2007;88(1):19–24. doi: 10.1016/j.apmr.2006.10.013. [DOI] [PubMed] [Google Scholar]
- Cheadle A, Franklin G, Wolfhagen C, Savarino J, Liu PY, Salley C, Weaver M. Factors influencing the duration of work-related disability: a population-based study of Washington State workers’ compensation. Am J Public Health. 1994;84(2):190–6. doi: 10.2105/ajph.84.2.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou R, Qaseem A, Snow V, Casey D, Cross JT, Jr, Shekelle P, Owens DK. Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478–91. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- Dale AM, Descatha A, Coomes J, Franzblau A, Evanoff B. Physical examination has a low yield in screening for carpal tunnel syndrome. Am J Ind Med. 2010;54(1):1–9. doi: 10.1002/ajim.20915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniell WE, Fulton-Kehoe D, Franklin GM. Work-related carpal tunnel syndrome in Washington State workers’ compensation: utilization of surgery and the duration of lost work. Am J Ind Med. 2009;52(12):931–42. doi: 10.1002/ajim.20765. [DOI] [PubMed] [Google Scholar]
- Dennerlein JT, Soumekh FS, Fossel AH, Amick BC, 3rd, Keller RB, Katz JN. Longer distal motor latency predicts better outcomes of carpal tunnel release. J Occup Environ Med. 2002;44:176–183. doi: 10.1097/00043764-200202000-00013. [DOI] [PubMed] [Google Scholar]
- Foley M, Silverstein B, Polissar N. The economic burden of carpal tunnel syndrome: long-term earnings of CTS claimants in Washington State. Am J Ind Med. 2007;50(3):155–172. doi: 10.1002/ajim.20430. [DOI] [PubMed] [Google Scholar]
- Franche R-L, Cullen K, Clarke J, Irvin E, Sinclair S, Frank J. Workplace-based return-to-work interventions: a systematic review of the quantitative literature. J Occup Rehab. 2005;15(4):607–31. doi: 10.1007/s10926-005-8038-8. [DOI] [PubMed] [Google Scholar]
- Gelfman R, Beebe TJ, Amadio PC, Larson DR, Basford JR. Correlates of upper extremity disability in medical transcriptionists. J Occup Rehabil. 2010;20(3):340–8. doi: 10.1007/s10926-010-9235-7. [DOI] [PubMed] [Google Scholar]
- Gerritsen AA, de Vet HC, Scholten RJ, Bertelsmann FW, de Krom MC, Bouter LM. Splinting vs surgery in the treatment of carpal tunnel syndrome: a randomized controlled trial. JAMA. 2002;288(10):1245–1251. doi: 10.1001/jama.288.10.1245. [DOI] [PubMed] [Google Scholar]
- Godges JJ, Anger MA, Zimmerman G, Delitto A. Effects of education on return-to-work status for people with fear-avoidance beliefs and acute low back pain. Phys Ther. 2008;88(2):231–9. doi: 10.2522/ptj.20050121. [DOI] [PubMed] [Google Scholar]
- Hazard RG, Haugh LD, Reid S, Preble JB, MacDonald L. Early prediction of long-term disability after occupational low back injury. Spine. 1996;21(8):945–951. doi: 10.1097/00007632-199604150-00008. [DOI] [PubMed] [Google Scholar]
- Hui AC, Wong S, Leung CH, Tong P, Mok V, Poon D, Li-Tsang CW, Wong LK, Boet R. A randomized controlled trial of surgery vs steroid injection for carpal tunnel syndrome. Neurology. 2005;64(12):2074–2078. doi: 10.1212/01.WNL.0000169017.79374.93. [DOI] [PubMed] [Google Scholar]
- Jané-Llopis E, Matytsina I. Mental health and alcohol, drugs and tobacco: a review of the comorbidity between mental disorders and the use of alcohol, tobacco and illicit drugs. Drug Alcohol Rev. 2006;25(6):515–36. doi: 10.1080/09595230600944461. [DOI] [PubMed] [Google Scholar]
- Jarvik JG, Comstock BA, Kliot M, Turner JA, Chan L, Heagerty PJ, Hollingworth W, Kerrigan CL, Deyo RA. Surgery versus non-surgical therapy for carpal tunnel syndrome: a randomised parallel-group trial. The Lancet. 2009;374(9695):1074–81. doi: 10.1016/S0140-6736(09)61517-8. [DOI] [PubMed] [Google Scholar]
- Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- Katz JN, Amick BC, 3rd, Keller R, Fossel AH, Ossman J, Soucie V, Losina E. Determinants of work absence following surgery for carpal tunnel syndrome. Am J Ind Med. 2005;47(2):120–30. doi: 10.1002/ajim.20127. [DOI] [PubMed] [Google Scholar]
- Katz JN, Keller RB, Fossel AH, Punnett L, Bessette L, Simmons BP, Mooney N. Predictors of return to work following carpal tunnel release. Am J Ind Med. 1997;31(1):85–91. doi: 10.1002/(sici)1097-0274(199701)31:1<85::aid-ajim13>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- Katz JN, Lew RA, Bessette L, Punnett L, Fossel AH, Mooney N, Keller RB. Prevalence and predictors of long-term work disability due to carpal tunnel syndrome. Am J Ind Med. 1998;33(6):543–50. doi: 10.1002/(sici)1097-0274(199806)33:6<543::aid-ajim4>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Katz JN, Punnett L, Simmons BP, Fossel AH, Mooney N, Keller RB. Workers’ compensation recipients with carpal tunnel syndrome: the validity of self-reported health measures. Am J Public Health. 1996;86(1):52–6. doi: 10.2105/ajph.86.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyserling WM, Stetson DS, Silverstein BA, Brouwer ML. A checklist for evaluating ergonomic risk factors associated with upper extremity cumulative trauma disorders. Ergonomics. 1993;36(7):807–831. doi: 10.1080/00140139308967945. [DOI] [PubMed] [Google Scholar]
- Kouyoumdjian JA, Morita MP, Molina AF, Zanetta DM, Sato AK, Rocha CE. Long-term outcomes of symptomatic electrodiagnosed carpal tunnel syndrome. Arq Neuropsiquiatr. 2003;61:194–198. doi: 10.1590/s0004-282x2003000200007. [DOI] [PubMed] [Google Scholar]
- Levine DW, Simmons BP, Koris MJ, Daltroy LH, Hohl GG, Fossel AH, Katz JN. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993;75(11):1585–1592. doi: 10.2106/00004623-199311000-00002. [DOI] [PubMed] [Google Scholar]
- Maggard MA, Harness NG, Chang WT, Parikh JA, Asch SM, Nuckols TK Carpal Tunnel Quality Group. Indications for performing carpal tunnel surgery: clinical quality measures. Plast Reconstr Surg. 2010;126(1):169–79. doi: 10.1097/PRS.0b013e3181da8685. [DOI] [PubMed] [Google Scholar]
- Maghsoudipour M, Moghimi S, Dehghaan F, Rahimpanah A. Association of occupational and non-occupational risk factors with the prevalence of work related carpal tunnel syndrome. J Occup Rehabil. 2008;18(2):152–6. doi: 10.1007/s10926-008-9125-4. [DOI] [PubMed] [Google Scholar]
- Nathan PA, Keniston RC, Lockwood RS, Meadows KD. Tobacco, caffeine, alcohol, and carpal tunnel syndrome in American industry. A cross-sectional study of 1464 workers. J Occup Environ Med. 1996;38(3):290–8. doi: 10.1097/00043764-199603000-00015. [DOI] [PubMed] [Google Scholar]
- Nathan PA, Meadows KD, Istvan JA. Predictors of carpal tunnel syndrome: an 11-year study of industrial workers. J Hand Surg Am. 2002;27(4):644–51. doi: 10.1053/jhsu.2002.34003. [DOI] [PubMed] [Google Scholar]
- Scholten RJ, Mink van der Molen A, Uitdehaag BM, Bouter LM, de Vet HC. Surgical treatment options for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007;17(4):CD003905. doi: 10.1002/14651858.CD003905.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin AY, Perlman M, Shin PA, Garay AA. Disability outcomes in a worker’s compensation population: surgical versus nonsurgical treatment of carpal tunnel syndrome. Am J Orthop. 2000;29(3):179–84. [PubMed] [Google Scholar]
- Silverstein B, Adams D. Safety and Health Assessment and Research for Prevention Program. Washington State Department of Labor and Industries; 2007. Work-related musculoskeletal disorders of the neck, back, and upper extremity in Washington State, 1997-2005. Technical Report No. 40-11-2007. [Google Scholar]
- Silverstein BA, Fan ZJ, Bonauto DK, Bao S, Smith CK, Howard N, Viikari-Juntura E. The natural course of carpal tunnel syndrome in a working population. Scand J Work Environ Health. 2010;36(5):384–93. doi: 10.5271/sjweh.2912. [DOI] [PubMed] [Google Scholar]
- Silverstein BA, Stetson DS, Keyserling WM, Fine LJ. Work-related musculoskeletal disorders: comparison of data sources for surveillance. Am J Ind Med. 1997;31(5):600–608. doi: 10.1002/(sici)1097-0274(199705)31:5<600::aid-ajim15>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- Slater MA, Weickgenant AL, Greenberg MA, Wahlgren DR, Williams RA, Carter C, Patterson TL, Grant I, Garfin SR, Webster JS, Atkinson JH. Preventing progression to chronicity in first onset, subacute low back pain: an exploratory study. Arch Phys Med Rehabil. 2009;90(4):545–52. doi: 10.1016/j.apmr.2008.10.032. [DOI] [PubMed] [Google Scholar]
- Smith CK, Bonauto DK, Silverstein BA, Wilcox D. Inter-rater reliability of physical examinations in a prospective study of upper extremity musculoskeletal disorders. J Occup Environ Med. 2010;52(10):1014–8. doi: 10.1097/JOM.0b013e3181f4396b. [DOI] [PubMed] [Google Scholar]
- Sørensen LT, Zillmer R, Agren M, Ladelund S, Karlsmark T, Gottrup F. Effect of smoking, abstention, and nicotine patch on epidermal healing and collagenase in skin transudate. Wound Repair Regen. 2009;17(3):347–53. doi: 10.1111/j.1524-475X.2009.00479.x. [DOI] [PubMed] [Google Scholar]
- Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: Development and validation. Psychol Assess. 1995;7:524–532. [Google Scholar]
- Turner JA, Franklin G, Fulton-Kehoe D, Egan K, Wickizer TM, Lymp JF, Sheppard L, Kaufman JD. Prediction of long-term disability in work-related musculoskeletal disorders: a prospective, population-based study. BMC Musculoskeletal Disorders. 2004;5:14. doi: 10.1186/1471-2474-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner JA, Franklin G, Fulton-Kehoe D, Sheppard L, Wickizer TM, Wu R, Gluck JV, Egan K, Stover B. Early predictors of long-term work disability associated with carpal tunnel syndrome: a longitudinal workers’ compensation cohort study. Am J Ind Med. 2007;50(7):489–500. doi: 10.1002/ajim.20477. [DOI] [PubMed] [Google Scholar]
- United States Preventive Services Task Force (USPSTF) Guide to Clinical Preventive Services. [3/3/11];Agency For Healthcare Research And Quality. http://www.ahrq.gov/clinic/pocketgd.htm.
- Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in long-term low back pain and disability. Pain. 1993;52(2):157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Dewey JE. How to score version two of the SF-36 health survey. Lincoln, RI: QualityMetric Incorporated; 2000. [Google Scholar]
- Washington State Department of Labor and Industries’ (DLI) Industrial Insurance Medical Advisory Committee (IIMAC), Subcommittee On Upper Extremity Entrapment Neuropathies. Work-Related Carpal Tunnel Syndrome Diagnosis and Treatment Guideline. Washington State Department of Labor and Industries; 2009. [3/3/11]. http://www.lni.wa.gov/ClaimsIns/Files/OMD/CarpalTunnel.pdf. [Google Scholar]
- Wasiak R, Pransky G. The impact of procedure type, jurisdiction and other factors in workers’ compensation on work-disability outcomes following carpal tunnel surgery. Work. 2007;28(2):103–10. [PubMed] [Google Scholar]
- Whitfill T, Haggard R, Bierner SM, Pransky G, Hassett RG, Gatchel RJ. Early Intervention Options for Acute Low Back Pain Patients: A Randomized Clinical Trial with One-Year Follow-Up Outcomes. Journal of Occupational Rehabilitation. 2010;20(2):256–63. doi: 10.1007/s10926-010-9238-4. [DOI] [PubMed] [Google Scholar]
- Williams RM, Westmorland MG, Lin CA, Schmuck G, Creen M. Effectiveness of workplace rehabilitation interventions in the treatment of work-related low back pain: a systematic review. Disabil Rehabil. 2007;29(8):607–24. doi: 10.1080/09638280600841513. [DOI] [PubMed] [Google Scholar]


