Abstract
This study involves mandibular and midface fractures recorded in the trauma reports of OMFS department, SCB dental college, Cuttack, Odisha. The reports were studied between December 2004 and November 2009. The 503 patients had 539 mandibular fractures and 117 midface fractures. Males accounted for 442 (87.87%) and females accounted for 61 (12.12%). Male to female ratio was 7.25:1. The most common cause of fracture was road traffic accident and accounted for 404 (80.31%). The most common site of fracture mandible was parasymphysis where as in middle third fracture it was zygomatic complex fracture. The most common age groups involved in fracture were 21–30 years and the incidence of head injury was 97(19.28%). Many of these variations may be related to socioeconomic, cultural and environmental conditions.
Keywords: Maxillofacial Injuries, Analysis, Pattern, Odisha
Introduction
Various studies on the incidence of maxillofacial fractures in different countries have been previously reported. Mandibular fractures are twice as common as fractures of the bones of midface and comprise most of the traumatic injuries treated by an oral and maxillofacial surgeon. The incidence is about 38% of all facial bone fractures. The main causes worldwide are assaults and traffic accidents, but the most frequent cause varies from one country to another. Some studies have shown that assault is most common in developing countries, whereas, traffic accidents are more common in developed countries.
The aim of the present study is to analyze retrospectively the age and sex distribution, aetiology and location of mandibular and midface fractures in a sample of patients from SCB Dental College, Cuttack, Odisha.
The causes of mandibular fractures were classified as road traffic accidents, assaults, falls and sport related injuries. Anatomically, the fractures of the mandibles were classified into seven regions namely condyle, coronoid, ramus, angle, body, parasymphysis, symphysis & dentoalveolar regions. The midface fractures are classified into Le forte-I, Le forte-II, Le forte-III, nasal bone, zygomatic complex and maxilla fracture. The above mentioned samples were taken from the trauma form, filled for every patient on their first visit to the department, before the patient underwent treatment. Age of the patients ranging from 6 years to above 76 years and for ease of description they are classified into different age groups such as 0–10 years, 11–20 years, 21–30 years, 31–40 years, 41–50 years, 51–60 years and above 60 years.
Patients and Methods
The data for this study were obtained from the medical records of 503 cases treated at SCB Dental College, Cuttack, Odisha, during the period from December 2004 to November 2009. Data were collected regarding gender, age, date of trauma, date of surgery, addictions, dentition, oral hygiene condition, etiology, signs and symptoms, fracture area, treatment performed, date of hospital discharge, and drug therapy. Complications such as malocclusion, infection, mal-union, nonunion, fibrous union and presence of scars recorded.
All patients were treated by the same oral and maxillofacial surgeon. When each patient arrived at hospital for the first medical appointment, a trauma form was filled and depending on the fracture pattern the appropriate treatment was given. In most of the cases maxillo-mandibular fixation (MMF) were performed with Erich arch bar and 26 gauge stainless steel wire. The rigid internal fixation (RIF) was used in all surgical treatments and MMF was not necessary beyond the intra-operative period. RIF was performed using 1.5, 2, 2.5 mm screws and titanium plates.
Antero-posterior, lateral-oblique, submento-vertex, towne radiographs, occlusal view, occipitomental view, and lateral skull view were carried out to determine fracture diagnosis.
Results
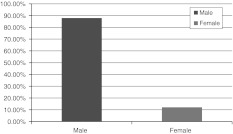
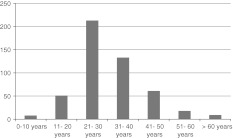
In this study we found that, the total number of patients were 503, among them 539 mandibular fractures and 117 midface fractures were reported. The maxillofacial fractures occurred in 61 females having mean age group 34.19 years (range 10–70 years) and 442 males with mean age group 31.85 years (range 6–76 years). Sex distribution is shown in pie diagram in Fig. 1. The average ages of women were older than the average age of men. The ages of the patient were ranged from 6 to 76 years. Most common age groups involved were of 21–30 years. Least common fracture occurred in the age group of 0–10 years. Numbers of fractures in different age groups are shown in Fig. 2. Males greatly outnumbered female patients in this data as was studied in various other studies. Males accounted for 442 (87.87%) and females accounted for 61 (12.12%), resulting in a male: female ratio of 7.25:1. In males, numbers of mandible fracture were 454 and midface fractures were 102 and in females the numbers of mandible fractures were 49 and midface fractures were 15.
Fig. 1.
Sex distribution
Fig. 2.
Age distribution
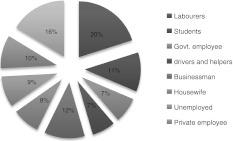
Data on occupation are presented in Fig. 3. Among 61 females, 40 were housewife, 8 were students, 4 were labourers and other 9 females were govt. tailors, electrician, private employee, engineers and shopkeeper etc.
Fig. 3.
Occupation wise distribution
From the 442 males, 101 were labourers, 59 were businessman, 57 were students, 37 were govt. employee, 34 were drivers and helpers, 46 males were unemployed, 48 males were private employee and other 82 males were carpenter, contractor, doctor, advocate, tailor, policemen, shopkeeper, politician, goldsmith, etc.
From the trauma report, it was found that the mean time of reporting of the patients to OMFS OPD after trauma was 5.3 days (range 1–23 days), mean time between reporting and surgery was 3.7 days (range 1–10 days), and mean time between surgery and discharge was 1.6 days (range 1–7 days).
At least one social risk factor at the time of maxillofacial trauma was found in 157 patients (31.21%). Alcohol abuse was observed in 74 patients i.e., on every seventh patient one was an alcoholic, smoking was observed in 85 patients; both alcohol and smoking were observed in 112 patients. One case of intravenous drug abuse case was reported.
The most common sign was pain at fracture site, facial swelling, followed by limitation of mouth opening, and malocclusion. Mental nerve paraesthesias were reported in 53 cases of mandibular body fractures and 5 cases of angle fractures. Infra-orbital nerve paraesthesias were reported in 37 cases of Leforte-II and zygomatic complex fractures. Otorrhoea and rhinorrhoea cases were not noted in this study.
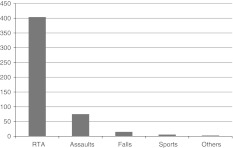
Most common cause of fracture was RTA 404 (80.31%) followed by assault 75 (13.91%), falls 15 (2.98%), sports 6 (1.19%) and least commonly by others 3 (0.59%). Data on etiology of fractures are shown in Fig. 4. In females 53 were involved in RTA and 4 cases each were of assault and fall. Among the males 351 were of RTA, 71 were assault injuries, 11 were of fall from height and 6 of sport injuries and 3 of other injuries. Both in males and females RTA was the main cause of fracture. Most of the females involved in RTA were fall from back seat of bike either at a speed breaker or due to wearing of saris which can entangle to the wheels of a speeding motor vehicle. In RTA, motor cycles were commonly involved contributing to 307 (75.99%) followed by car and other four wheelers of about 69 (17.07%), bicycle injury 17 (4.2%), pedestrian 11 (2.7%). RTA is the most common cause because of increasing number of vehicles now-a-days. Among 307 motor cycles accident victims only 112 (36.48%) persons were used helmets at the time of accident and other 195 (63.52%) persons were without helmets. Information regarding seat belt application was missing in the trauma form so we could not document the data.
Fig. 4.
Trauma etiologies
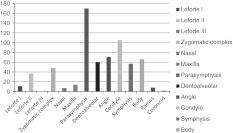
The most common site of mandibular fracture was the parasymphysial region. The parasymphysial fracture was commonly associated with a subcondylar fracture. The order of fracture site from most common to least common were parasymphysis 170 (33%), condyle 105 (20.87%), angle 71 (14.11%), body fracture 66 (13.12%), dentoalveolar fracture 60 (11.92%), symphysis fracture 57 (11.33%), ramus 8 (1.5%) and lastly the coronoid process 2 (0.39%). The data on different fracture sites are presented in Fig. 5. The order of mid face fracture are zygomatic complex 48 (9.5%), Le forte-II 37 (7.3%), Maxilla fracture 14 (2.7%), Le forte-I 11 (2.1%), & nasal fracture 7 (1.3%). Le forte-III cases were not reported in this study.
Fig. 5.
Site distribution
Classification of fractures revealed that 135 (26.83%) were close and 368 (73.16%) were open fractures. Patients having single fracture on their face were 217 (43.14%), multiple fractures were 250 (49.7%), comminuted fractures were 31 (6.16%) and incomplete fractures were reported only in five cases. In single fracture, the parasymphysis was commonly involved, whereas, in multiple fractures the parasymphysis and subcondylar region were commonly involved. Comminuted and incomplete fractures were commonly involving the body region. Out of 105 condylar fractures, only 12 were treated by open reduction and 93 patients were treated conservatively. There were no significant differences between open and close reduction. So we preferred close reduction by MMF for 2 weeks followed by release of MMF and jaw exercise leading to normal jaw opening and function.
Most of the fractures were treated by the MMF (89.06%) and RIF were performed in only 34 (6.75%) cases (6 mid face and 28 mandible fractures) and 21 (4.17%) patients were treated conservatively.MMF were done by using Erich arch bar, 26 gauge stainless steel wire and elastics. RIF were done by 1.5, 2, 2.5 mm diameter titanium plates and plate size were four-hole and six-hole plate with gap using screws of length 8, 10, 12 mm. Fractures of the symphysis and parasymphysis were always stabilized using two plates through an intraoral approach. The same pattern of treatment was used for body fractures; but the extra-oral approach was used in few cases. In midface fractures four-hole L-plate and six-hole orbital plate were used and all approaches were made intraorally.
Of all trauma patients, head injury were reported in 19.28% cases (97 patients) and associated other injuries were reported in 22.46% cases (113 patients). Soft tissue injuries were accounted for 14.91% (75 patients), skeletal injuries were of 7.15% (36 patients) and visceral injuries were of only 0.39% (2 cases). Complications after treatment were noted in 28 cases, among them malocclusion in 14 cases, mal-union in 9 cases, infection in 4 cases, fibrous union in only one case and nonunion was not found.
Discussion
Epidemiologic surveys of mandibular fractures are consistently influenced by geographic area, population density, socioeconomic status of the cohort, regional government, cultural differences and the period of investigation [1, 4, 8, 12]. The epidemiology of mandibular fractures has changed dramatically with the advent of lower speed limits, new seatbelt and helmet laws, and increased urban violence [12]. The gender predilection found in this study was more towards the male subjects. Also, as generally reported, most of these were in the second and third decades of life. Such persons are more commonly involved in high speed driving, altercations, sports and other outdoor activities than older patients and this is confirmed by the predominant causes of their mandibular fractures. Children below 10 years suffered less number of injuries though during this period children are under constant supervision.
Most frequent cause of fracture mandible in this study was RTA. This was due to increasing number of vehicles, high speed driving, less use of seat belts and absence of airbags in most of the vehicles and alcohol abuse during driving. Most RTAs were with two wheelers than four wheelers because numbers of two wheelers were more than four wheelers and also younger adults usually drive two wheelers. Two types of motor cycle helmets, closed and open are usually used [2]. The open type does not protect the entire face and exposes the mandible to trauma. Helmets are available in specific sizes for each motorcyclist’s head, but this is disregarded by some motorcyclist’s, resulting in inadequate protection. Some motorcyclists refuse to fasten their chin straps and others wear closed helmets ‘half off’, just sitting on their heads, giving them a false sense of safety. Among those who suffered a traffic accident, 80% were wearing a seatbelt during the car accident. 36.48% motor cycle accident patients were wearing helmets, but only 12% of these helmets were closed. None of the car accident victims were driving cars equipped with air bags. Most cars do not have air bags in this part of the world. Recent research has concluded that drivers sustain fewer facial fractures when airbags are deployed, either alone or in combination with a seatbelt. Among passengers, airbags provide significant protection from lacerations but have no impact on the incidence of facial fractures. The use of any protective device decreases the incidence of facial trauma sustained in motor vehicle accidents; airbags provide the best protection of all currently available devices [15].
The anatomic distribution and incidence of mandibular fracture are widely variable [11, 18]. Many authors reported the angle as the most frequently affected site [3, 5, 12, 18], whereas, others reported this to be mandibular body [4, 9, 16] and symphysis [3]. In this study, the parasymphysis was the most frequently affected site (33%) and ZMC (9.5%) in mid face region. This may be due to more severe type of injury in RTAs than assaults in this part of the world. According to Rowe and Williams, fracture lines for parasymphysis fractures extend from symphysis to distal line of the canine which is a narrow area. Usually canines are having the larger roots making the mandible anatomically weak in this region leading to most fractures. In assaults commonly symphysis fracture occurs. Commonly parasymphysis fractures are associated with a subcondylar fracture. This is due to transmission of force in that direction and also subcondylar portion is the weak area of the mandible. In midface fracture zygomatic complex is the most common fracture site, as it is the most prominent portion of the face and usually during trauma every person has a tendency to show this portion towards the injuring object. Lefort-III cases were not reported in this study.
31.21% of the patients had at least one social risk factor, including alcohol abuse, smoking, and non-intravenous drug abuse. A relationship between substance abuse and post operative complications has been reported by some authors [7, 13, 14, 17]. Passeri et al. [17] observed a positive association between complications and chronic abuse of alcohol and drugs. 30% of the intravenous drug abusers had complications following mandibular fractures, while non-intravenous drug abusers and chronic alcohol abusers had 19 and 16% complication rates, respectively. HAUG and SCHWIMMER [7] studied the fibrous union of mandibular fractures and found an incidence of 3%. 94% of these patients had at least one medical and social risk factor, which included alcohol abuse (63%), smoking (41%), and intravenous drug abuse (26%). MATHOG et al. [13] observed that out of 25 patients with nonunion, 18 were classified as having alcohol or drug abuse issues. MILES et al. [14] quoted the abuse of tobacco and alcohol as significant factors when determining the risk of postoperative infections in patients with mandibular fractures. The present result did not demonstrate any relationship between social risk factors and complication rates.
Patrocinio et al. analyzed 293 patients with mandibular fractures and observed signs and symptoms such as pain, swelling, hematoma, dental malocclusion, facial contour deficit, cracking, and mobility of bone fragments. In the present study, the most common signs and symptoms were pain and local swelling, with incidences of 91 and 74%, respectively.
The most common etiologies of mandibular fractures in the literature are violence, traffic accidents, gunshot wounds, sporting events, work related accidents, and falls [1, 4, 6, 9, 10, 12, 16] in the present study, the most frequent etiologies were traffic accidents (80.31%), and assaults (13.91%).
In this study, the authors did not find many cases of complex fractures, and appropriate treatments were performed as soon as possible. Treatment was carried out by the same experienced surgeon for all 503 patients, and antibiotic therapy was employed whenever it was indicated. The tooth in the fracture line was removed when the tooth was mobile, had periodontal or periapical pathology, was partially impacted or was carious. The authors think that these precautions are the reason why there was not an excessive rate of complications.
The retrospective study of the distribution, etiology and location of mandibular and mid face fracture revealed that the therapy applied was effective in treating this type of fracture and showed rates of success comparable with published data around the world.
Acknowledgments
Conflict interest
None declared.
Funding
None.
References
- 1.Brasileiro BF, Passeri LA. Epidemiological analysis of maxillofacial fractures in Brazil: a 5 year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:28–34. doi: 10.1016/j.tripleo.2005.07.023. [DOI] [PubMed] [Google Scholar]
- 2.Chritah A, Lazow SK, Berger JR. Transoral 2.0 mm locking miniplate fixation of mandibular fractures plus 1 week of maxillomandibular fixation: a prospective study. J Oral Maxillofac Surg. 2005;63:1737–1741. doi: 10.1016/j.joms.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 3.Chuong R, Donoff RB, Guralnick WC. A retrospective analysis of 327 mandibular fractures. J Oral Maxillofac Surg. 1983;41:305–309. doi: 10.1016/0278-2391(83)90297-5. [DOI] [PubMed] [Google Scholar]
- 4.Ellis E, III, Moos KF, El-Atar A, Arbor A. Ten years of mandibular fractures: an analysis of 2, 137 cases. Oral Surg Oral Med Oral Pathol. 1985;59:120–129. doi: 10.1016/0030-4220(85)90002-7. [DOI] [PubMed] [Google Scholar]
- 5.Gabrielli MAC, Gabrielli MFR, Marcantonio E, Hochuli-Vieira E. Fixation of mandibular fractures with 2.0 mm miniplates: review of 191 cases. J Oral Maxillofac Surg. 2003;61:430–436. doi: 10.1053/joms.2003.50083. [DOI] [PubMed] [Google Scholar]
- 6.Gassner R, Tuli T, Hachl O, Rudisch A, Ulmer H. Cranio-maxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg. 2003;31:51–61. doi: 10.1016/S1010-5182(02)00168-3. [DOI] [PubMed] [Google Scholar]
- 7.Haug RH, Schwimmer A. Fibrous union of the mandible: a review of 27 patients. J Oral Maxillofac Surg. 1994;52:832–839. doi: 10.1016/0278-2391(94)90230-5. [DOI] [PubMed] [Google Scholar]
- 8.Hogg NJV, Stewart TC, Armstrong JEA, Girotti MJ. Epidemiology of maxillofacial injuries at trauma hospitals in Ontario, Canada, between 1992 and 1997. J Trauma. 2000;49:425–431. doi: 10.1097/00005373-200009000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Horibe KE, Pereira MD, Ferreira LM, Andrade EF. Perfil epidemiologico de fracturas mandibulares tratadas na Universidade Federal de sao Paulo-Escola Paulista de Medicina. Rev Assoc Med Bras. 2004;50:417–421. doi: 10.1590/S0104-42302004000400033. [DOI] [PubMed] [Google Scholar]
- 10.Iida S, Kogo M, Sugiura T, Mima T, Mtsuya T. Retrospective analysis of 1,502 patients with facial fractures. Int J Oral Maxillofac Surg. 2001;30:286–290. doi: 10.1054/ijom.2001.0056. [DOI] [PubMed] [Google Scholar]
- 11.Imazawa T, Komuro Y, Inoue M, Yanai A. Mandibular fracturesw treated with maxillomandibular fixation screws (MMFS method) J Craniofac Surg. 2006;17:544–549. doi: 10.1097/00001665-200605000-00026. [DOI] [PubMed] [Google Scholar]
- 12.James RB, Fredrickson C, Kent JN. Prospective study of mandibular fractures. J Oral Surg. 1981;39:275–281. [PubMed] [Google Scholar]
- 13.Mathog RH, Toma V, Clayman L, Wolf S. Nonunion of the mandible: an analysis of the contributing factors. J Oral Maxillofac Surg. 2000;58:746–752. doi: 10.1053/joms.2000.7258. [DOI] [PubMed] [Google Scholar]
- 14.Miles BA, Potter JK, Ellis E., III The efficacy of postoperative antibiotic regimens in the open treatment of mandibular fractures: a prospective randomized trial. J Oral Maxillofac Surg. 2006;64:576–582. doi: 10.1016/j.joms.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 15.Murphy RX, Jr, Birmingham KL, Okunski WJ, Wasser T. The influence of airbag and restraining devices on the patterns of facial trauma in motor vehicle collisions. Plast Reconstr Surg. 2000;105:516–520. doi: 10.1097/00006534-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Olson RQA, Fonseca RJ, Osbon DB. Fractures of the mandible: a review of 580 cases. J Oral Maxillofac Surg. 1982;40:23–28. doi: 10.1016/S0278-2391(82)80011-6. [DOI] [PubMed] [Google Scholar]
- 17.Passeri LA, Ellis E, III, Sinn DP. Relationship of substance abuse to complications with mandibular fractures. J Oral Maxillofac Surg. 1993;51:22–25. doi: 10.1016/S0278-2391(10)80383-0. [DOI] [PubMed] [Google Scholar]
- 18.Sakr K, Farag IA, Zeitoun IM. Review of 509 mandibular fractures treated at the University Hospital, Alexandria, Egypt. Br J Oral Maxillofac Surg. 2006;44:107–111. doi: 10.1016/j.bjoms.2005.03.014. [DOI] [PubMed] [Google Scholar]