Abstract
Teratomas are neoplasm composed of three germinal layers of the embryo that form tissues not normally found in the organ in which they arise. These are most common in the sacrococcygeal region and are rare in the head and neck, which account for less than 6%. An unusual case of facial teratoma in a new born, managed successfully is described here with postoperative follow up of 2 years without any recurrence.
Keywords: Teratoma, Mature teratoma, Facial teratoma, Zygomatic bone
Introduction
Teratomas of facial region are interesting because of their obscure origin, bizarre microscopic features, different morphology, location and often dramatic clinical presentation. They are true neoplasm, composed of mixture of tissues, which are not native to the area where the tumor occurs. These are benign tumors composed of tissue elements of bidermal or tridermal origin.
Teratomas are most commonly located in the sacrococcygeal region, followed by the ovaries, testes, anterior mediastinum, retroperitoneum, and finally the head and neck. Teratomas in the face are extremely rare, which account for less than 6% [1].
Teratomas in head and neck region usually were discovered during neonatal period, where as teratomas in other anatomic regions usually were discovered in the second decade of life 2. These tumors are frequently associated with other congenital anomalies with in head and neck such as cleft palate, bifid tongue and bifid uvula [2, 3].
This report describes a rare case of teratoma with different morphology and location.
Case Report
A 1 day old full term male baby was referred to our Oral Maxillofacial Surgery unit with finger like projections over upper right cheek. On clinical examination of the growth, it was soft to hard in consistency, non collapsible, fixed at the base and movable at tip measuring about 30 mm in length and 20 mm in diameter. Below the projection, two small skin tags measuring 15 and 10 mm, which was soft in consistency, mobile and connected with stalk were also present. (Figs. 1, 2)
Fig. 1.

Showing finger like projection on right zygomatic region
Fig. 2.
CT scan of face showing an osseous growth arising from right lateral wall of the orbit
Baby was investigated to rule out other congenital anomalies like cleft palate, bifid tongue and bifid uvula. The routine hematological investigations were preformed, the results of which were within normal limits.
Computed tomography (CT) scan of face revealed an osseous growth arising from right lateral wall of the orbit with soft tissue component surrounding it measuring 35 × 20 mm without any abnormal intra cranial or intra orbital communication.
Based on the clinical examination and imaging study, a working diagnosis of teratoma was made. After obtaining the informed consent, the patient was taken up for planned surgical excision of the lesion under general anesthesia. After standard painting and draping of the surgical area, incision was placed at the base of the tumor projection and deep complete excision of tumor was carried out with careful dissection in a circumferential manner. The adjacent skin tags were removed separately at the base of the stalk. After achieving proper haemostasis, tension-free closure was done in layers by using ‘Z plasty’ technique with 4-0 vicryl and 6-0 ethilon sutures. Postoperative course of baby was uneventful. The patient is on a regular follow up since last 2 years and showed no signs of recurrence and morbidity accept a small linear scar.
Histopathological report of excised large lesion showed skin with adenexal structure (sebaceous glands), bundles of smooth muscle fibers, mature adipose tissue, nerve bundles, mature bone and cartilage tissue, suggestive of mature teratoma. And two skin tags showed fibro-epithelial polyp.(Figs. 3, 4, 5)
Fig. 3.
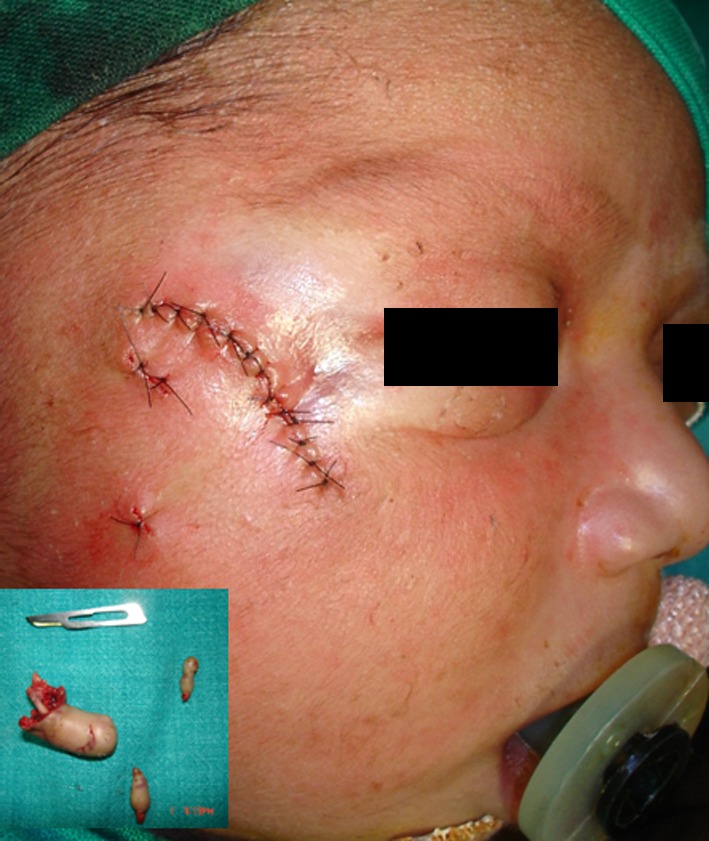
Closure with 6-0 ethilon suture and excised specimen of the tumor in inner box
Fig. 4.
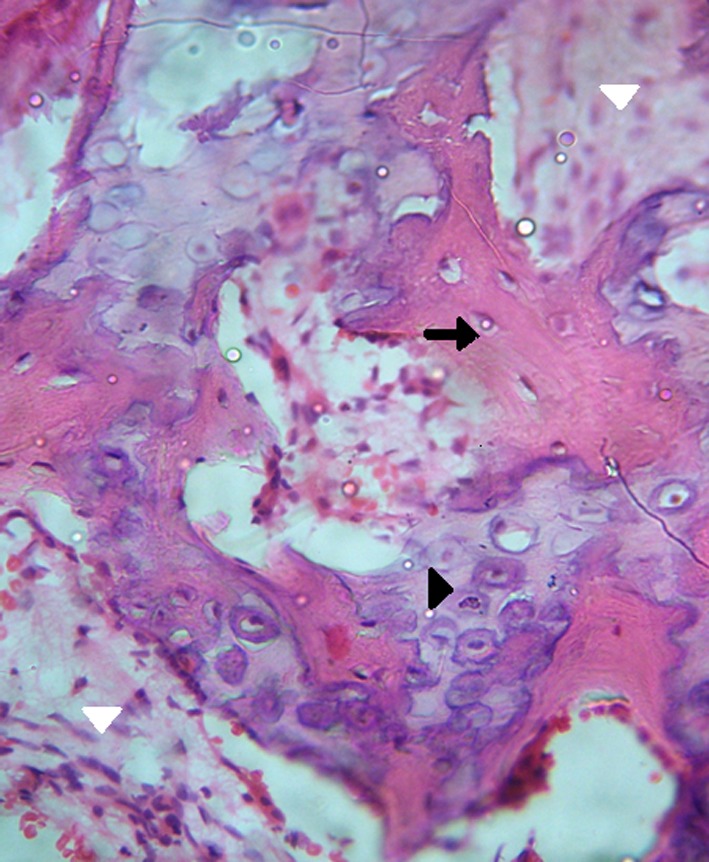
Shows fragments of mature bone tissue (black arrow) with areas of mature cartilage (black arrow head) and stromal connective tissue (white arrow head) (H & E stain, original magnification ×10)
Fig. 5.

Two-year postoperative follow-up with no recurrence (frontal view)
Discussion
Teratoma in head and neck region are very rare, with the incidence 2–9% of all teratomas [2]. They are true neoplasm composed of an assemblage of tissue often alien to the site in which it arises. Head and neck teratomas reportedly occur in 1 of 40,000 births [4].
The term teratoma is often used to describe any of the four types of tumor that constitute tissue foreign to the area in which it is located. These include dermoids (hairy polyps), teratoid, true teratomas, and epignathi. In 1992, Tharrington and Bussen proposed following histologic classification for the congenital tumors [4].
Dermoids are neoplasm composed of only of ectodermal and mesodermal elements.
Teratoids contain ectodermal, mesodermal, and endodermal elements. These elements are however not well differentiated and lack clear organization.
True teratomas contain tissue derivatives from 3 germ layers. Cell layers demonstrate more organization.
Epignathi are the least frequent but most striking of teratomas in that well-formed organs and limbs may be found occurring in abnormal locations (e.g., an arm coming out of the oral cavity) [4].
No single histological picture is characteristic although the usual appearance of disorganized neoplastic tissues of various types readily identifies the lesion to the pathologist.
Etiology of teratoma is unknown, but various theories have been proposed to explain their etiology like:
Acquired traumatic implantation of skin or mucous membrane within deeper tissues.
Congenital inclusion of germ layers into deeper tissue at point where developing somatic regions fails to completely fuse during embryogenesis.
Implantation of pluripotential cells, which subsequently grow in a disorganized manner [3].
The case reported here has different morphology, rare location and histologically mature teratoma and composed of all three germ cell layers. However, these cells are differentiated to the level of specific tissue.
Federico Biglioli et al. have reported a case of teratoma on left infraorbital region which resembled a small breast like growth. The lesion was enucleated and showed no recurrence after 18 months [4]. Congenital epignathus teratoma which occurs in approximately 1:35,000–1:200,000 live births, where major concern are airway obstruction and facial distortion are reported in the literature [2–5].
The diagnosis of this case was easily made as teratoma based on clinical findings and CT scan report. The differential diagnosis of facial teratoma should include cystic hygroma, brachial cleft cyst (non calcified and cystic type) and rhabdhomyosarcoma, hemangioma, lymphangioma (are under calcified and mainly solid) [1, 4].
Teratomas are partly undiagnosed at the time of birth. Diagnostic aids like CT scan and MRI shows anatomic relations of the tumor, extension and margins. Proper diagnosis is important before deciding on the operation [6].
The degree of histological differentiation of teratoma is high and they can be classified as mature, immature and with malignant differentiation [1]. Microscopic examination of excised specimen of this case showed a well-defined organoid structures arranged in disorganized manner, suggestive of mature teratoma.
As the extent of this reported tumor is restricted to the site of tumor origin and no intracranial or intraorbital communication, the prognosis was good with less morbidity. Depending on the location, size and histological grade, a teratoma carries a mortality rate of 80–100% in which the tumor mass impinges on the airway [3, 5, 7].
In the literature, recurrence of teratoma has been reported where in the lesion had been excised incompletely at the primary operation [2]. Hence the best treatment includes early and complete surgical excision of the tumor. In this case the 2 year regular follow up has showed no recurrence.
References
- 1.Biglioli F, Gianni AB, Di Francesco A. Congenital teratoma of the cheek: report of case. Int J Oral Maxillofac Surg. 1996;25:208–209. doi: 10.1016/S0901-5027(96)80032-4. [DOI] [PubMed] [Google Scholar]
- 2.Becker S, Schon R, Gutwald R, Otten JE, Maier W, Hentschel R, et al. A congenital teratoma with a cleft palate: report of a case. Br J Oral Maxillofac Surg. 2007;45:326–327. doi: 10.1016/j.bjoms.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 3.Haghighi K, Cleveland D. Epignathus teratoma with bifid tongue and median glossal salivary mass: report of a case. J Oral Maxillofac Surg. 2004;62:379–383. doi: 10.1016/j.joms.2003.05.012. [DOI] [PubMed] [Google Scholar]
- 4.Tolentino MM, Oconer JNN, Almazan Aguilar NA. Large nasopharyngeal true teratoma in a Filipino newborn: a case report. Philippine J Otolaryngol Head Neck Surg. 2005;20:59–65. [Google Scholar]
- 5.Lionel J, Valvoda M, Al-Abdul Hadi KA. Giant Epignathus-a case report. Kuwait Med J. 2004;36:217–220. [Google Scholar]
- 6.Moore KR. Oculomotor nerve teratoma. Am J Neuroradiol. 2001;22:1566–1569. [PMC free article] [PubMed] [Google Scholar]
- 7.Merhi ZO, Heberman S, Roberts JL, Benin GS. Prenatal diagnosis of palatal teratoma by 3-dimensional sonography and color doppler imaging. J Ultrasound Med. 2005;24:1317–1320. doi: 10.7863/jum.2005.24.9.1317. [DOI] [PubMed] [Google Scholar]



