Abstract
The lingering numbness that can last anywhere from 3 to 5 h after a routine dental procedure is often an unnecessary, inconvenient hassle. Patients may find that their ability to speak, smile, eat and drink is impaired, and may even have uncontrollable drooling. The effects of local dental anesthetics can now be reversed. That’s because OraVerse, an anesthetic reversal agent, can return the patient to normal sensation and function in about half the time. OraVerse which is U.S. Food and Drug Administration approved is a safe and effective form of phentolamine mesylate, a vasodilator that has been used in several other medical applications since 1952. OraVerse injection – the first and only proven safe and effective product of its kind can quickly reverse the effects of local dental anesthetics, so patient can carry on without impairment of talk, smile and drink after dental procedures. Studies also have shown that there are no known drug interactions and no evident toxicity or contraindications for using OraVerse.
Keywords: OraVerse, Submucosal injection, Anaesthesia, Periodontal maintenance, Reverses numbness
Introduction
Patients can have their dental work performed in a pain-free fashion. Of course, the problem with dental anesthetics is that for some people, it takes hours for their mouths to recover from the numbing effect. This issue often translates into a problem for busy working people who can’t afford to spend half a day feeling numb in the face. Instead of a quick morning filling appointment being a simple affair, it can negatively impact a person’s work performance by impairing speech and impeding a person’s ability to present them publicly without humiliation. Fortunately, mouth-related numbness doesn’t have to be an all-day affair thanks to a new anesthetic reversal agent called OraVerse.
So what is this magic drug and how does it work? OraVerse is the first and only local dental anesthesia reversal agent in the market proven to accelerate the reversal of anaesthetic effect (numbness) after dental procedures. To administer OraVerse, dentist will inject it into the area of the patient’s mouth that has been worked on and is therefore already numb. Since the oral injection site will already be numb by the time the OraVerse is given, patients won’t feel any additional discomfort during this process. After OraVerse is given, patients can expect their numbness recovery period to be virtually reduced to half the duration of total anaesthesia.
OraVerse is recommended for adults, adolescents, and children who are aged six and older and who weigh a minimum of 33 pound.
Description
OraVerse is a formulation of phentolamine mesylate that accelerates the return to normal sensation and function for patients after routine dental procedures. OraVerse is dispensed in a standard dental cartridge marked with a green label for ease of identification. It is administered by injection with a standard dental syringe in the same injection site as that used for the local anesthetic. OraVerse is used in a 1:1 ratio to local anesthetic. Each package includes 10, 1.7 ml cartridges and prescribing information [1]. The maximum recommended dose of OraVerse is two cartridges in patients’ age 12 or greater, one cartridge in children age 6–11 years and weighing over 66 lbs, and one half cartridge in children 6–11 years and weighing 33–66 lbs. OraVerse is not indicated in children less than 6 years of age or weighing less than 33 lbs. It is not recommended to use after invasive procedures such as endodontic treatment or surgery, where post-operative discomfort is anticipated [1].
Oraverse increases the diameter of blood vessels in the area. The increase in blood flow removes the extra drug and takes it to the liver and the kidneys to be broken down. Microscopic picture is shown in Fig. [1] [2].
Fig. 1.
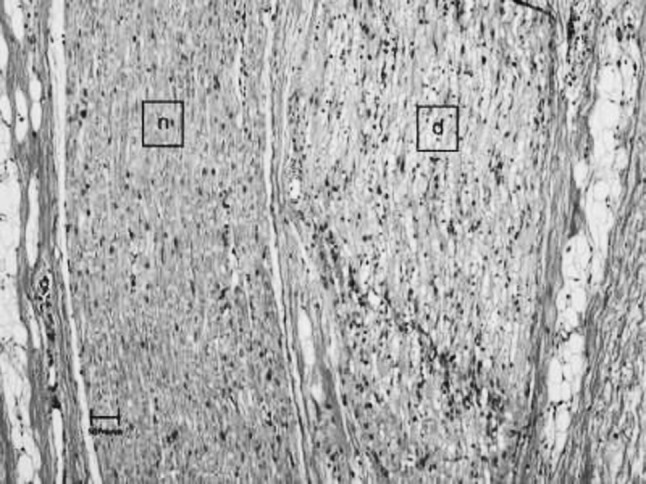
Photomicrograph of normal (n) and degenerated nerve (d) adjacent in the gingival biopsy from an animal 24 hours after it received 27 μg/kg phentolamine mesylate in the right maxilla adjacent to the first premolar
Full Prescribing Information
Indications and Usage: [3, 4]
(1). OraVerse is indicated for reversal of the soft-tissue anesthesia (STA), i.e., anesthesia of the lip and tongue, and the associated functional deficits resulting from an intraoral submucosal injection of a local anesthetic containing a vasoconstrictor. (2). Prevention or control of hypertensive episodes in patients with pheochromocytoma. (3). Pharmacologic test for pheochromocytoma (not method of choice). (4). Prevention and treatment of dermal necrosis and sloughing following IV administration or extravasation of norepinephrine.
Contraindications
(1). OraVerse is not recommended for use in children less than 6 years of age or weighing less than 15 kg. (2). Hypersensitivity to phentolamine or related compounds. (3). History of myocardial infarction, coronary insufficiency, angina, or other evidence suggestive of coronary artery disease
Dosage and Administration
General Dosing Information: [5]
The recommended dose of OraVerse is based on the number of cartridges of local anesthetic with vasoconstrictor administered:
| Amount of local anesthesia administered | Dose of Oraversa (mg) | Dose of Oraversa (Cartridge) |
|---|---|---|
| ½ cartridge | 0.2 | 1/2 |
| 1 cartridge | 0.4 | 1 |
| 2 cartridge | 0.8 | 2 |
OraVerse should be administered following the dental procedure using the same location(s) and technique(s) (infiltration or block injection) employed for the administration of the local anesthetic.
Note: Do not administer OraVerse if the product is discolored or contains particulate matter.
If dose is effective, normal skin color should return to the blanched area within 1 h
Vasoconstrictor (alpha-adrenergic agonist) extravasation: Infiltrate the area of extravasation with multiple small injections using only 27 or 30 gauge needles and changing the needle between each skin entry. Be careful not to cause so much swelling of the extremity or digit that a compartment syndrome occurs. If infiltration is severe, may also need to consult vascular surgeon.
Dosing in Special Populations
In pediatric patients weighing 15–30 kg, the maximum dose of OraVerse recommended is 1/2 cartridge (0.2 mg).
(Note: Use in pediatric patients under 6 years of age or weighing less than 15 kg (33 lbs) is not recommended. A dose of more than 1 cartridge [0.4 mg] of OraVerse has not been studied in children less than 12 years of age).
Dosage Forms and Strengths
0.4 mg/1.7 ml solution per cartridge.
Warnings and Precautions
Cardiovascular Events
Myocardial infarction, cerebrovascular spasm, and cerebrovascular occlusion have been reported to occur following the parenteral administration of phentolamine. These events usually occurred in association with marked hypotensive episodes producing shock-like states. Tachycardia and cardiac arrhythmias may occur with the use of phentolamine or other alpha-adrenergic blocking agents. Although such effects are uncommon after administration of OraVerse, clinicians should be alert to the signs and symptoms of these events, particularly in patients with a prior history of cardiovascular disease [6].
Adverse Reactions
Cardiovascular
Tachycardia (6%); bradycardia (4%); acute and prolonged hypotensive episodes, cardiac arrhythmias, orthostatic hypotension (post marketing).
Miscellaneous
Post procedural pain (10%); injection-site pain (6%).
In clinical trials, the most common adverse reaction with OraVerse was injection site pain that was greater than the control group.
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Dental patients were administered a dose of 0.2, 0.4 or 0.8 mg of OraVerse. The majority of adverse reactions were mild and resolved within 48 h. There were no serious adverse reactions and no discontinuations due to adverse reactions [7].
Table 1 lists adverse reactions where the frequency was greater than or equal to 3% in any OraVerse dose group and was equal to or exceeded that of the control group [3].
Table 1.
Adverse reaction with frequency greater than or equal to 3% and equal to or exceeding control [3]
| Adverse Event | OraVerse | Control | |||
|---|---|---|---|---|---|
| 0.2 mg (N = 83) | 0.4 mg (N = 284) | 0.8 mg (N = 51) | Total (N = 418) | Total (N = 359) | |
| N (%) | N (%) | N (%) | N (%) | N (%) | |
| Patients with AEx | 15 (18) | 82 (29) | 20 (39) | 117 (28) | 96 (27) |
| Tachycardia | 0 (0) | 17 (6) | 2 (4) | 19 (5) | 20 (6) |
| Bradycardia | 0 (0) | 5 (2) | 2 (4) | 7 (2) | 1 (0.3) |
| Injection site pain | 5 (6) | 15 (5) | 2 (4) | 22 (5) | 14 (4) |
| Post procedural pain | 3 (4) | 17 (6) | 5 (10) | 25 (6) | 23 (6) |
| Headache | 0 (0) | 10 (4) | 3 (6) | 13 (3) | 14 (41) |
An examination of population subgroups did not reveal a differential adverse reaction incidence on the basis of age, gender, or race.
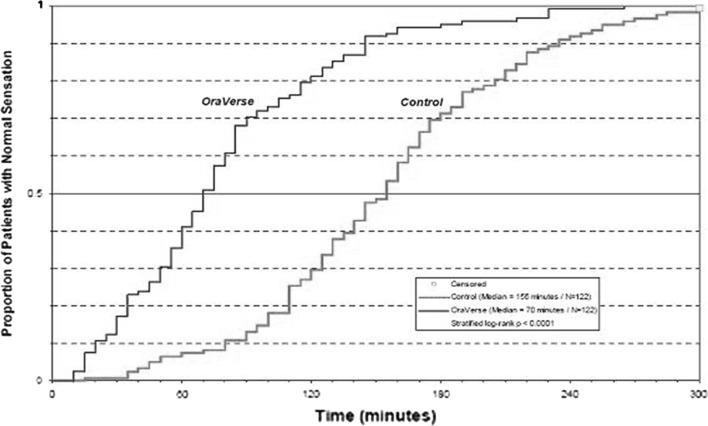
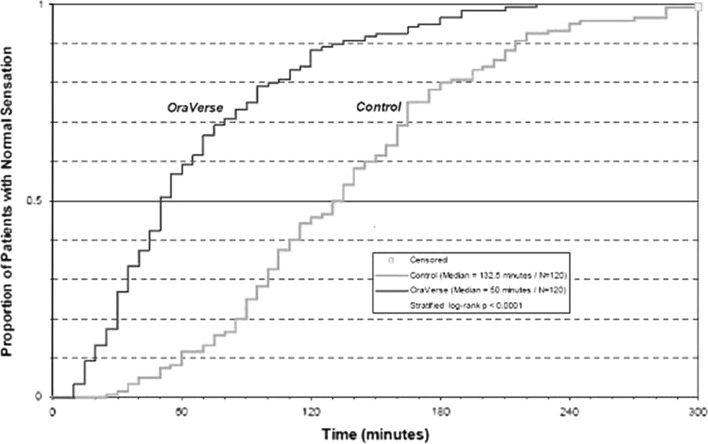
Results from the pain assessments in study 1 and study 2, involving mandibular and maxillary procedures, respectively, indicated that the majority of dental patients in both OraVerse and control groups experienced no or mild oral pain, with less than 10% of patients in each group reporting moderate oral pain with a similar distribution between the OraVerse and control groups. No patient experienced severe pain in these studies [Fig. 2, 3].
Fig. 2.
Kaplan-Meier plot of time to recovery of normal sensation in the lower lip (ITT analysis data set)
Fig. 3.
Kaplan-Meier plot of time to recovery of normal sensation in the upper lip (ITT analysis data set)
Adverse Reactions in Clinical Trials
Adverse reactions reported by less than 3% but at least two dental patients receiving OraVerse and occurring at a greater incidence than those receiving control, included diarrhea, facial swelling, increased blood pressure/hypertension, injection site reactions, jaw pain, oral pain, paresthesia, pruritis, tenderness, upper abdominal pain and vomiting. The majority of these adverse reactions were mild and resolved within 48 h. The few reports of paresthesia were mild and transient and resolved during the same time period [8].
Post Marketing Adverse Reaction Reports from Literature and Other Sources
The following adverse reactions have been identified during post approval parenteral use of phentolamine mesylate. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Acute and prolonged hypotensive episodes and cardiac arrhythmias have been reported with the use of phentolamine. In addition, weakness, dizziness, flushing, orthostatic hypotension, and nasal stuffiness have occurred [9].
Drug Interactions
Antihypertensive Agents
Withhold prior to test for diagnosis of pheochromocytoma; do not perform this test on normotensive patients [4].
Epinephrine, Ephedrine
Vasoconstrictive and hypertensive effects of epinephrine and ephedrine are antagonized by phentolamine [10].
Lidocaine and Epinephrine
When OraVerse was administered as an intraoral submucosal injection 30 min after injection of a local anesthetic, 2% lidocaine HCl with 1:100,000 epinephrine, the lidocaine concentration increased immediately after OraVerse intraoral injection. Lidocaine, Area under the concentration Curve (AUC) and Cmax (maximum drug concentration achieved in systemic circulation following drug administration) values were not affected by administration of OraVerse. OraVerse administration did not affect the Pharmaco Kinetics (PK) of epinephrine [11].
Laboratory Test Interactions
There are no known drug interactions with OraVerse.
Uses in Specific Populations
Pregnancy
Pregnancy Category C
There are no adequate and well-controlled studies in pregnant women. OraVerse should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Oral administration of phentolamine to pregnant rats and mice at doses at least 24 times the recommended dose (based on a 60 kg human) resulted in slightly decreased growth and slight skeletal immaturity of the fetuses. Immaturity was manifested by increased incidence of incomplete or unossified calcaneal and phalangeal nuclei of the hind limb and of incompletely ossifiedsternebrae. At oral phentolamine doses at least 60 times the recommended dose (based on a 60 kg human), a slightly lower rate of implantation was found in the rat. Phentolamine did not affect embryonic or fetal development in the rabbit at oral doses at least 20 times the recommended dose (based on a 60 kg human). No teratogenic or embryotoxic effects were observed in the rat, mouse, or rabbit studies [12].
Nursing Mothers
It is not known whether OraVerse is secreted in human milk. Because many drugs are secreted in human milk, caution should be exercised when OraVerse is administered to a nursing woman. The unknown risks of limited infant exposure to phentolamine through breast milk following a single maternal dose should be weighed against the known benefits of breastfeeding.
Pediatric Use
In clinical studies, pediatric patients between the ages of 3 and 17 years received OraVerse. The safety and effectiveness of OraVerse have been established in the age group 6–17 years. Effectiveness in pediatric patients below the age of 6 years has not been established. Use of OraVerse in patients between the ages of 6 and 17 years old is supported by evidence from adequate and well-controlled studies of OraVerse in adults, with additional adequate and well-controlled studies of OraVerse in pediatric patients aged 12–17 years old [studies 1 (mandibular procedures) and 2 (maxillary procedures)] and ages 6–11 years old [study 3 (mandibular and maxillary procedures)]. The safety, but not the efficacy, of OraVerse has been evaluated in pediatric patients under the age of 6 years old. Dosages in pediatric patients may need to be limited based on body weight [13].
Geriatric Use
Of the total number of patients in clinical studies of OraVerse, 55 were 65 and over, while 21 were 75 and over. No overall differences in safety or effectiveness were observed between these patients and younger patients, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Overdosage
No deaths due to acute poisoning with phentolamine have been reported [14].
Overdosage with parenterally administered phentolamine is characterized chiefly by cardiovascular disturbances, such as arrhythmias, tachycardia, hypotension, and possibly shock. In addition, the following might occur: excitation, headache, sweating, pupillary constriction, visual disturbances, nausea, vomiting, diarrhea, or hypoglycemia.
There is no specific antidote; treatment consists of appropriate monitoring and supportive care. Substantial decreases in blood pressure or other evidence of shock-like conditions should be treated vigorously and promptly [15].
Chemical Structure
Phentolamine mesylate is phenol, 3-[[(4, 5-dihydro-1 H-imidazol-2-yl) methyl] (4-methyl-phenyl)amino]-, methanesulfonate (salt), a non-specific alpha adrenergic blocker.
Phentolamine mesylate United States Pharmacopenia (USP) is a white to off-white, odorless crystalline powder with a molecular weight of 377.46. It is sparingly soluble in water, soluble in alcohol, and slightly soluble in chloroform. The empirical formulation is C 17H19N3O·CH4O3S and the chemical structure is [3].  OraVerse (phentolamine mesylate) injection is a clear, colorless, sterile, non pyrogenic, isotonic, preservative free solution. Each 1.7 ml cartridge contains 0.4 mg phentolamine mesylate, D-mannitol, edetate disodium, and sodium acetate. Either acetic acid or sodium hydroxide is used as necessary to adjust the pH [3].
OraVerse (phentolamine mesylate) injection is a clear, colorless, sterile, non pyrogenic, isotonic, preservative free solution. Each 1.7 ml cartridge contains 0.4 mg phentolamine mesylate, D-mannitol, edetate disodium, and sodium acetate. Either acetic acid or sodium hydroxide is used as necessary to adjust the pH [3].
Clinical Pharmacology
Mechanism of Action
The mechanism by which OraVerse accelerates reversal of STA and the associated functional deficits is not fully understood. Phentolamine mesylate, the active ingredient in OraVerse, produces an alpha-adrenergic block of relatively short duration resulting in vasodilatation when applied to vascular smooth muscle. In an animal model, OraVerse increased local blood flow in submucosal tissue of the dog when given after an intra oral injection of lidocaine 2% with 1:100,000 epinephrine.
Pharmacokinetics: [16]
Following OraVerse administration, phentolamine is 100% available from the submucosal injection site and peak concentrations are achieved 10–20 min after injection. Phentolamine systemic exposure increased linearly after 0.8 mg compared to 0.4 mg OraVerse intraoral submucosal injection. The terminal elimination half-life of phentolamine in the blood was approximately 2–3 h [16].
Absorption
T max (Time required to achieve maximum drug concentration in systemic circulation) is 10–20 min.
Elimination
Urine (13% as unchanged drug). Half-life is 19 min (IV) and 2–3 h.
Pediatrics
Following OraVerse administration, the phentolamine Cmax(maximum drug concentration achieved in systemic circulation following drug administration) was higher (approximately 3.5-fold) in children who weighed between 15 and 30 kg (33 and 66 lbs) than in children who weighed more than 30 kg. However, phentolamine AUC was similar between the two groups. It is recommended that in children weighing 15–30 kg, the maximum dose of OraVerse should be limited to ½ cartridge (0.2 mg).
The pharmacokinetics of OraVerse in adults and in children who weighed more than 30 kg (66 lbs) is similar after intraoral submucosal injection.
OraVerse has not been studied in children under 3 years of age or weighing less than 15 kg (33 lbs). The pharmacokinetics of OraVerse after administration of more than 1 cartridge (0.4 mg) has not been studied in children [13].
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies with OraVerse have not been conducted.
Phentolamine was not mutagenic in the in vitro bacterial reverse mutation (Ames) assay. In the in vitro chromosomal aberration study in Chinese hamster ovary cells, numerical aberrations were slightly increased after a 4 h exposure to phentolamine without metabolic activation and structural aberrations were slightly increased after a 4 h exposure to phentolamine with metabolic activation only at the highest concentrations tested, but neither numerical nor structural aberrations were increased after a 20 h exposure without metabolic activation. Phentolamine was not clastogenic in two in vivo mouse micronucleus assays. At doses up to 150 mg/kg (143 times human therapeutic exposure levels at the Cmax), phentolamine mesylate was shown to have no adverse effects on male fertility in the rat [17].
Clinical Studies
The safety and efficacy of OraVerse when used for reversal of STA, were evaluated in the following clinical studies. The efficacy of OraVerse on reversal of local anesthesia of the teeth, mandible and maxilla has not been assessed.
Two Phases 3, double-blinded, randomized, multi-center, controlled studies were conducted in dental patients who had mandibular (study 1) or maxillary (study 2) restorative or periodontal maintenance procedures and who had received a local anesthetic that contained a vasoconstrictor. The primary endpoint was time to normal lip sensation as measured by patient reported responses to lip palpation. The secondary endpoints included patients’ perception of altered function, sensation and appearance, and their actual functional deficits in smiling, speaking, drinking and drooling, as assessed by both the patient and an observer blinded to the treatment. In the mandibular study, the time to recovery of tongue sensation was also a secondary endpoint. Patients were stratified by type and amount of anesthetic administered. OraVerse was administered at a cartridge ratio of 1:1 to local anesthetic. The control was a sham injection [12].
OraVerse reduced the median time to recovery of normal sensation in the lower lip by 85 min (55%) compared to control. The median time to recovery of normal sensation in the upper lip was reduced by 83 min (62%). The differences between these times for both studies are depicted in Kaplan–Meier plots for time to normal lip sensation in Figs. 2 and 3. Within 1 h after administration of OraVerse, 41% of patients reported normal lower lip sensation as compared to 7% in the control group, and 59% of patients in the OraVerse group reported normal upper lip sensation as compared to 12% in the control group [12].
In study 1 (mandibular), OraVerse accelerated: a) the recovery of the perception of normal appearance and function by 60 min (40%), b) the recovery of normal function by 60 (50%) min, and c) the recovery of normal sensation in the tongue by 65 min (52%). In study 2 (maxillary), the recovery of the perception of normal appearance and function was reduced by 60 min (50%) and the recovery of normal function was reduced by 45 min (43%) [Fig. 2, 3] [12].
Another study which was, a pediatric, phase 2, double-blinded, randomized, multi-center, controlled study, conducted in dental patients who had received 2% lidocaine with 1:100,000 epinephrine. Dental patients (n = 152, ages 4–11 years) received 1/2 cartridge of local anesthetic if they weighed ≥ 15 kg but < 30 kg, and one-half or one full cartridge if they weighed ≥ 30 kg at a cartridge ratio of 1:1 to local anesthetic [12].
The median time to normal lip sensation in patients 6–11 years of age who were trainable in the lip-palpation procedures, for mandibular and maxillary procedures combined, was reduced by 75 min (56%). Within 1 h after administration of OraVerse, 44 patients (61%) reported normal lip sensation, while only nine patients (21%) randomized to the control group reported normal lip sensation. In this study, neither the patients’ perception of their appearance or ability to function or their actual ability to function was evaluated [12, 18].
Supplied/Storage and Handling
OraVerse(phentolamine mesylate) injection 0.4 mg/1.7 ml is supplied in a dental cartridge, in cartons of 10 and 50 cartridges. Each cartridge is individually packaged in a separate compartment of a 10 cartridge blister pack.
Store at controlled room temperature, 20–25°C (68–77°F) with brief excursions permitted between 15–30°C (59–86°F). Protect from direct heat and light. Do not permit to freeze [3].
Screening Tests
Urinary assays of catecholamines or other biochemical assays have largely supplanted phentolamine and other pharmacologic tests for pheochromocytoma. Phentolamine is usually used as confirmation. Follow specific guidelines for use of phentolamine.
Patient Counseling Information
Patients should be instructed not to eat or drink until normal sensation return. Instruct patient to avoid sudden position changes to prevent orthostatic hypotension.
Instruct patient to notify health care provider if chest pain develops during infusion.
Advise patient to report the following symptoms to health care provider: dizziness, fainting spells, or weaknesses.
Important Safety Information
Following parenteral use of phentolamine at doses between 5 to 15 times higher than the recommended dose of OraVerse (phentolamine mesylate), myocardial infarction, and cerebrovascular spasm and occlusion have been reported, usually in association with marked hypotensive episodes producing shock-like states. Although such effects are uncommon with OraVerse, clinicians should be alert to the signs and symptoms of tachycardia, bradycardia, and cardiac arrhythmias, particularly in patients with a history of cardiovascular disease; as these symptoms may occur with the use of phentolamine or other alpha-adrenergic blocking agents [7, 19, 20].
OraVerse (solution for injection/dental cartridge) is administered as a submucosal injection and is not to be confused with phentolamine used as an intramuscular or intravenous injection for the treatment of hypertension associated with pheochromocytoma [11].
Conclusion
OraVerse represents a break-through in dentistry that can free patients from the unwanted and unnecessary numb sensation typically experienced after routine dental procedures.
A great benefit that children (and their parents) will experience with OraVerse is that their tendency to chew their tongue, cheeks and/or lips when those areas are numb is greatly reduced, and there is less likely to be a problem because the anesthetized area is more quickly returned to normal.
References
- 1.Wynn RL. Phentolamine mesylate-An old medical drug becomes a new dental drug. Gen Dent. 2009;57(3):200–202. [PubMed] [Google Scholar]
- 2.Morrow T. OraVerse helps you lose that numbing feeling. Manag Care. 2008;17(90):50–51. [PubMed] [Google Scholar]
- 3.Drugs.com [Internet]. Drug information on line; C 2000-10 Micromedex™ [Updated 2 July 2010], Cerner Multum™ [Updated 24 August 2010], Wolters Kluwer™ [Updated 2 September 2010; Cited 2010 Sept 6]. Available from http://www.drugs.com/pro/oraverse.html
- 4.Myklejord DJ. Undiagnosed pheochromocytoma: the anesthesiologist nightmare. Clin Med Res. 2004;2(1):59–62. doi: 10.3121/cmr.2.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ceatus Media Group LLC [Internet]. Consumer Guide to Dentistry; C 2006-10 [Up dated 2010 May13; Cited 2010 Sep 6]. Available from http://www.yourdentistryguide.com/oraverse/
- 6.Hersh EV, Moore PA, Papas AS, Goodson JM, Navalta LA, Rogy S, et al. Reversal of soft-tissue local anesthesia with phentolamine mesylate in adolescents and adults. J Am Dent Assoc. 2008;139(8):1080–1093. doi: 10.14219/jada.archive.2008.0311. [DOI] [PubMed] [Google Scholar]
- 7.Weaver JM. New drugs on the horizon may improve the quality and safety of anesthesia. Anesth Prog. 2008;55(2):27–28. doi: 10.2344/0003-3006(2008)55[27:NDOTHM]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malamed S. What’s new in local anesthesia? SAAD Dig. 2009;25:4–14. [PubMed] [Google Scholar]
- 9.Gould L, Reddy CV, Chua W. Electrophysiological Properties of Phentolamine in Man. Br Heart J. 1977;39(9):939–944. doi: 10.1136/hrt.39.9.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roberts JR, Krisanda TJ. Accidental Intra-Arterial Injection of Epinephrine Treated With Phentolamine. Ann Emerg Med. 1989;18(4):424–425. doi: 10.1016/S0196-0644(89)80590-6. [DOI] [PubMed] [Google Scholar]
- 11.Rutherford B, Zeller JR, Thake D. Local and systemic toxicity of intraoral submucosal injections of phentolamine mesylate (OraVerse) Anesth Prog. 2009;56(4):123–127. doi: 10.2344/0003-3006-56.4.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laviola M, McGavin SK, Freer GA, Plancich G, Woodbury SC, Marinkovich S, et al. Randomized study of phentolamine mesylate for reversal of local anesthesia. J Dent Res. 2008;87(7):635–639. doi: 10.1177/154405910808700717. [DOI] [PubMed] [Google Scholar]
- 13.Tavares M, Goodson JM, Studen-Pavlovich D, Yagiela JA, Navalta LA, Rogy S, et al. Reversal of soft-tissue local anesthesia with phentolamine mesylate in pediatric patients. J Am Dent Assoc. 2008;139(8):1095–1104. doi: 10.14219/jada.archive.2008.0312. [DOI] [PubMed] [Google Scholar]
- 14.Malamed SF. Local anesthesia reversal. Dent Today. 2010;29(3):65–66. [PubMed] [Google Scholar]
- 15.Hill JM. Phentolamine mesylate: the antidote for vasopressor extravasation. Crit Care Nurse. 1991;11(10):58–61. [PubMed] [Google Scholar]
- 16.Moore PA, Hersh EV, Papas AS, Goodson JM, Yagiela JA, Rutherford B, et al. Pharmaco kinetics of lidocaine with epinephrine following local anesthesia reversal with phentolamine mesylate. Anesth Prog. 2008;55(2):40–48. doi: 10.2344/0003-3006(2008)55[40:POLWEF]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Poulet FM, Berardi MR, Halliwell W, Hartman B, Auletta C, Bolte H. Development of hibernomas in rats dosed with phentolamine mesylate during the 24-month carcinogenicity study. Toxicol Pathol. 2004;32(5):558–566. doi: 10.1080/01926230490505086. [DOI] [PubMed] [Google Scholar]
- 18.Hersh EV, Hermann DG, Lamp CJ, Johnson PD, Mac A, fee KA. Assessing the duration of mandibular soft tissue anesthesia. J Am Dent Assoc. 1995;126(11):1531–1536. doi: 10.14219/jada.archive.1995.0082. [DOI] [PubMed] [Google Scholar]
- 19.Cooper BE. High-dose phentolamine for extravasation of pressors. Clin Pharm. 1989;8(10):689. [PubMed] [Google Scholar]
- 20.Mc Cleane GJ. Oral phentolamine mesylate in the treatment of complex regional pain Syndrome. Ulst Med J. 1996;65(1):87–88. [PMC free article] [PubMed] [Google Scholar]