Abstract
Benign and malignant tumors of the temporomandibular joint are rare. An aneurysmal bone cyst (ABC) of the condyle is even more unusual and usually presents as a slowly enlarging firm swelling which occasionally may be associated with pain and tenderness. Surgical curettage or excision is the treatment of choice, in an attempt to reduce the potential problem of recurrence; we undertook surgical resection of the affected bone. Immediate mandibular reconstruction using autologous bone was deferred though it is generally recommended in such type of cases.
Keywords: Aneurysmal bone cyst (ABC), Mandibular condyle, Mandibular reconstruction
Introduction
The aneurysmal bone cyst is a type of pseudocysts of the jaw. It is a non-neoplastic lesion of the bone, characterized by replacement with fibro-osseous tissue containing blood-filled sinusoidal or cavernous spaces. The lesion remains a relatively uncommon finding in the facial bones and the etiology and pathogenesis have yet to be elucidated [1].
Fifty percent of ABCs arise in the long bones, and 20% occur in the vertebral column. ABC accounts for 1.5% of the nonodontogenic, nonepithelial cysts of the mandible [2, 3].
It is reported among children and adults with no gender predilection. It generally affects young persons predominantly under 20 years of age [1]. In patients with this lesion, 50–70% may recall a history of trauma although the relationship between trauma and ABCs has yet to be ascertained [4].
Diagnosis is made considering the patient’s history, physical and radiographic examinations, histopathology and intra-operative findings. This is a case report of a patient treated for ABC of the mandibular condyle in our unit.
Report of a Case
In Oct 2007, an 18 year old female patient was referred to our unit with a chief complaint of swelling in the left preauricular region associated with pain which has progressively increased over a period of 5 months. Initially she developed pain on chewing in the left temporomandibular joint, following which she noticed a small lump in the left preauricular region, which gradually increased in size. There was no history of trauma. On physical examination a solitary swelling was noticed which was smooth, oval and measuring about 3 × 2 cm in the left preauricular region (Figs. 1, 2). The swelling moved in conjunction with the mandibular movement. On palpation the swelling was bony hard in consistency with a smooth surface, tender and no pulsations were felt. The patient had a maximal interincisal opening of 20 mm, with cranial nerves V and VII being intact. There were no clinically palpable lymph nodes. Patient reported no history of weight loss or cachexia and no significant medical or dental history. Aspiration of the left preauricular swelling was done and a bright red colored fluid was obtained.
Fig. 1.

Pre-op
Fig. 2.

Pre-op (lateral)
Panoramic radiographs revealed, large expansile radiolucent lesion involving the condyle and the upper half of the ramus (Fig. 3). There was marked thinning of the both the cortices. Inferior expansion of the radiolucency was almost up to the level of the occlusal plain. Coronal and axial CT scans revealed near symmetrical expansion of the medial and lateral cortices of the left condyle and also that of the ramus (Fig. 4). No temporal bone involvement was seen. Routine hematology and specific blood chemistry were normal. Aspiration report revealed that there were only red blood cells with few leukocytes. The tissue biopsy of the lesion showed fibrocollagenous cyst wall with woven bone trabeculae with scattered multinucleated giant cells amongst fibroblasts. Focal blood filled spaces were also seen. No pleomorphism or mitosis was seen.
Fig. 3.

Pre-op (OPG)
Fig. 4.
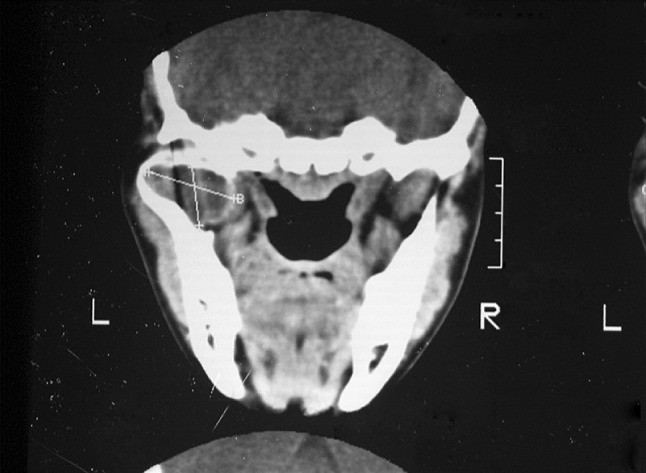
Pre-op CT scan
In December 2007 patient was operated under general anaesthesia. Intraoral incision was placed along the anterior border of the ramus. Ramus and the coronoid process were exposed and a portion of the lesion was removed intraorally (Fig. 6). A horizontal cut was made just above the level of the lingula. Since the access was limited to the condyle through this approach; extraoral retromandibular incision was placed and the remaining cystic lesion in the condylar portion was retrieved (Fig. 5). Thus the lesion enblock was resected and bleeding was controlled using bipolar cautery. Wound closure achieved using layered suture both intraorally and extraorally. Reconstruction at this stage was not done. Postoperative course was uneventful. The excised specimen was sent for microscopic examination (Figs. 7, 8, 9). Subsequently, the diagnosis of ABC was confirmed.
Fig. 6.

Intra-op (intra oral)
Fig. 5.

Intra-op (extra oral)
Fig. 7.

Closure
Fig. 8.
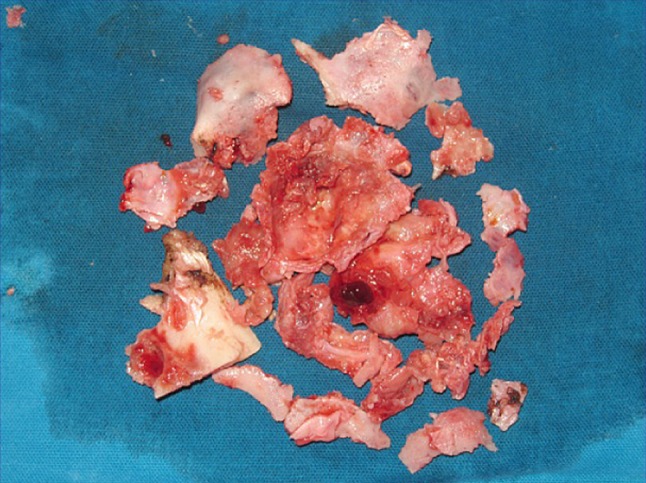
Resected specimen
Fig. 9.
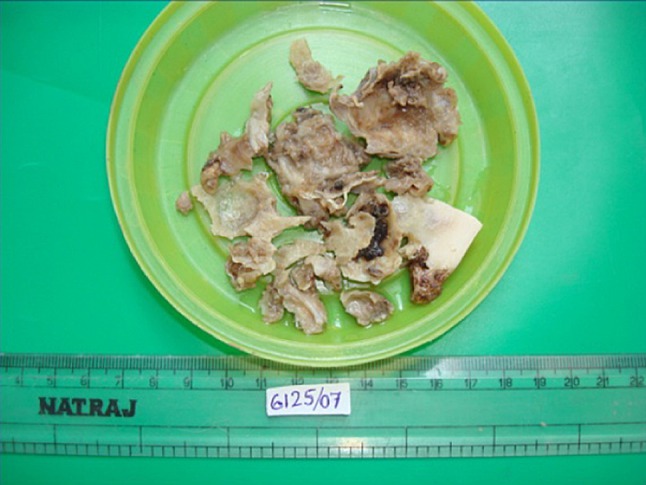
Resected specimen (measured)
Postoperatively patient had mild marginal mandibular nerve weakness and a slight deviation of the mandible to left side on opening the jaw. Patient was discharged on the eighth post-operative day and advised regular follow-up.
Discussion
The ABC was first recognized in 1893 by Van Arsdale [5] and Lichtenstein [6] coined the term “aneurysmal bone cyst” in 1957. In 1983, Sanerkin et al. [7] described the solid type of ABC without vascular and cyst-like cavities as a “typical” ABC. However, the incidence of the solid type of ABC has been reported as 5–7.5% [8].
The cause of these lesions is still controversial. Jaffe and Lichtenstein [9] refer to alterations in local haemodynamics causing increased venous pressures and engorgement of the vascular bed in the tranformed bone, leading to resorption, connective tissue replacement, and osteoid formation. Struthers [10], who found areas similar to the aneurysmal bone cyst in many of the previous lesions, postulated that the lesion occurs due to a microcyst from cellular oedema in the primary lesion such as the central giant cell granuloma, fibrous dysplasia, ossifying and cementifying fibromas. Some pathologists assume the aneurysmal bone cyst is actually a response to an alteration in the vessels of the region causing a proliferative reaction without healing owing to continual effusion of blood from the injured vessels [10].
Clinically, no gender predilection is observed and the mandible is the most common site in the facial bone, which is followed by maxilla [11]. The lesion is a slow growing painless mass that may cause pain and swelling as it increases in size. A bruit may be heard if the arterial component is significant.
The radiographic appearance of ABC is non-specific, variable and may be unilocular or multilocular, soap bubble or moth eaten radiolucency with destruction of the bony cortices and demarcated and irregular margins have been reported [4]. An angiogram, computed tomography scan and MRI help in establishing the diagnosis and is useful in avoiding excessive hemorrhage during biopsy [11].
One pathognomonic component in the microscopic diagnosis of ABC is the presence of well defined blood spaces lined by endothelial not epithelial components [12], (Figs. 10, 11, 12, 13). There are multinuclear giant cells around the foci of hemorrhage. Absence of smooth muscle component is highly suggestive of ABC, while ruling out hemangioma. Presence of haemosiderin is a consistent feature [11].
Fig. 10.
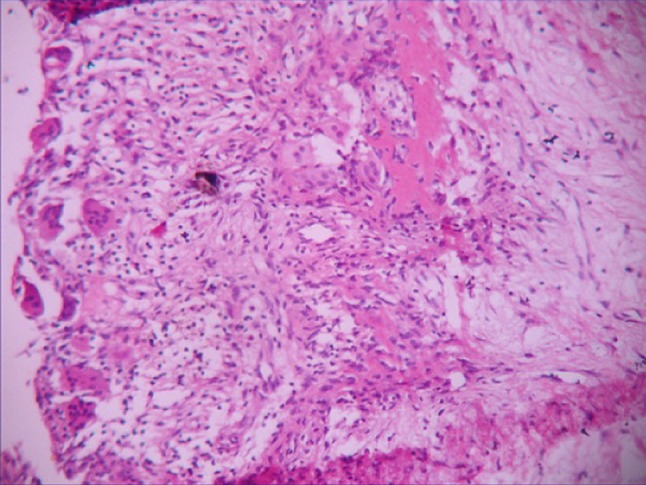
Histopathology
Fig. 11.

Post operative OPG
Fig. 12.

Post operative (lateral)
Fig. 13.

Post operative OPG
A variety of treatment protocols have been used such as curettage, block resection with reconstruction, therapeutic embolization, and long term follow-up to confirm self healing [12]. Successful results have been obtained through conservative curettages or block resections followed by reconstructions using grafts.
Bernier and Bhasker reported that recurrence is common in the long bones (20–60%), but seldom in the jaw bones [3]. The identification of patients who have ABC-“plus” prior to surgery is quite important since there is a possibility that recurrent ABC may be a manifestation of inadequate treatment of an associated lesion [13].
Block excision or resection though usually reserved for recurrent cases of ABCs as well as ABCs associated with other lesions, we in our case adopted this treatment since the lesion had multiple perforations following extensive expansion of bone and could end up with pathological fracture of the head of the condyle.
Conclusion
The ABC of the jaws is an uncommon benign lesion with an unclear etiology. There are typical radiographic findings, but diagnosis based solely on the radiographic findings may not be possible. Therefore histologically the aneurysmal bone cyst needs to be determined prior to any definitive surgical treatment.
Surgical curettage or excision is the treatment of choice. In an attempt to reduce the potential problem of recurrence, we undertook surgical resection of the affected bone. Immediate mandibular reconstruction using autologous bone was deferred though it is generally recommended in this case.
In conclusion, a policy of long term follow up to confirms the eventual self healing of an aneurysmal bone cyst lesion has been advocated by several authors [12].
Conflict of interest
The authors are the sole proprietary of this material thus stating no other conflicts of interest whatsoever.
References
- 1.Kiattavorncharoen S, Joos U, Brinkschmidt C, Werkmeister R. Aneurysmal bone cyst of the mandible: a case report. Int J Oral Maxillofac Surg. 2003;32:419–422. doi: 10.1054/ijom.2002.0351. [DOI] [PubMed] [Google Scholar]
- 2.Wiatrak BJ, Myer CM, III, Thomas MA. Alternatives in the management of aneurysmal bone cyst of the mandible. Int J Pediatr Otorhinolaryngol. 1995;31:247. doi: 10.1016/0165-5876(94)01082-9. [DOI] [PubMed] [Google Scholar]
- 3.Bemier J, Bhaskar S. Aneurysmal bone cyst of mandible. Oral Surg Oral Med Oral Pathol. 1958;11:1018. doi: 10.1016/0030-4220(58)90142-7. [DOI] [PubMed] [Google Scholar]
- 4.Motamedi MHK. Destructive Aneurysmal bone cyst of the mandibular condyle: report of the case and review of the literature. J Oral Maxillofac Surg. 2002;60:1357–1361. doi: 10.1053/joms.2002.35744. [DOI] [PubMed] [Google Scholar]
- 5.Arsdale WW. Ossifying hematoma. Ann Surg. 1893;18(8):12. doi: 10.1097/00000658-189307000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lichtenstein L. Aneurysmal bone cyst: observations on 50 cases. J Bone Joint Surg Am. 1957;39:837. [PubMed] [Google Scholar]
- 7.Sanerkin NG, Mott MG, Roylance J. An unusual Intraosseous lesion with firbroblastic osteoblastic aneurysmal, fibromyxoid elements: solid variant of aneurysmal bone cyst. Cancer. 1983;51:2278. doi: 10.1002/1097-0142(19830615)51:12<2278::AID-CNCR2820511219>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 8.Vergel De Dios AM, Bond JR, Shives TC. Aneurysmal bone cyst: a clinicopathologic study of 238 cases. Cancer. 1992;69:2921. doi: 10.1002/1097-0142(19920615)69:12<2921::AID-CNCR2820691210>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 9.Jaffe HL, Lichtenstein L. Solitary unicameral bone cyst. With emphasis on the roentgen picture, the pathological appearance and the pathogenesis. Arch Surg. 1942;44:1004–1025. doi: 10.1001/archsurg.1942.01210240043003. [DOI] [Google Scholar]
- 10.Struthers PJ, Shear M. Aneurysmal bone cyst of the jaws (II) pathogenesis. Int J Oral Surg. 1984;13:92–100. doi: 10.1016/S0300-9785(84)80078-2. [DOI] [PubMed] [Google Scholar]
- 11.Gadre KS, Zubairy RA. Aneurysmal bone cyst of the mandibular condyle: report of a case. J Oral Maxillofac Surg. 2000;58:439–443. doi: 10.1016/S0278-2391(00)90932-7. [DOI] [PubMed] [Google Scholar]
- 12.Hernadez GA, Castro A, Castro G, Amdor E, Bogota SF. Aneurysmal bone cyst versus hemangioma of the mandible. Report of long-term follow-up of a self limiting case. Oral Surg Oral Med Oral Pathol. 1993;76:790–796. doi: 10.1016/0030-4220(93)90053-7. [DOI] [PubMed] [Google Scholar]
- 13.Padwa BL, Denhart BC, Kaban LB. Aneurysmal bone cyst—“plus”: a report of three cases. J Oral Maxillofac. 1997;55:1144–1152. doi: 10.1016/S0278-2391(97)90296-2. [DOI] [PubMed] [Google Scholar]


