Abstract
Objectives
To characterize emergency admissions for patients with sickle cell crisis in NHS Brent and to determine which patients and practices may benefit most from primary care intervention.
Design
Observational study
Setting
Emergency departments attended by residents of the London borough of Brent
Participants
Patients with sickle cell disease registered with a general practitioner (GP) in the borough of Brent
Main outcome measures
Analysis of admissions between January 2008 and July 2010 that included length of stay (average and <2 days versus ≥2 days) by age group and registered GP practice.
Results
Thirty six percent of sickle cell disease admission spells resulted in a length of stay of less than two days. Seventy four percent of total bed days are associated with patients with more than one admission during the period of analysis, i.e. multiple admissions. Two general practices in Brent were identified as having the highest number of patients admitted to the emergency department for sickle cell crisis and may benefit most from primary care intervention.
Discussion
Patients with short length of stay and multiple admissions may be potentially amenable to primary care intervention. The practices which have the highest numbers of sickle cell disease patients who frequently seek emergency care will be earmarked for an education intervention designed to help further engage general practitioners in the care and management of their sickle cell patients.
Introduction
Sickle cell disease (SCD) is the most common genetic disorder worldwide, predominantly affecting Black and ethnic minorities (BME) groups. Incidence and prevalence in England has increased significantly in recent decades, particularly in urban areas.1 The growth in affected populations and the associated rising costs have attracted the attention of the healthcare community to SCD as an important public health issue. While just twenty years ago, infants born with SCD often did not survive childhood, a better understanding of the disease and improvements in medical technology and drug therapy have all contributed to patients with SCD surviving well into adulthood. However, positive health and life-expectancy outcomes are dependent on disease management and continuity of care throughout childhood, adolescence and adulthood.2
SCD is a genetic blood disorder characterized by abnormal, crescent-moon shaped red blood cells. These so called ‘sickled’ cells become lodged inside blood vessels, thereby obstructing blood flow and impeding efficient oxygen delivery to tissues throughout the body. Severe blockages cause episodes of acute pain, referred to as ‘crisis,’ which may be triggered by a range of physical and psychological stresses, including but not limited to infection, pregnancy, surgery, anxiety, or depression. If not treated promptly, crises can result in internal organ and tissue damage, particularly to the lungs, kidneys, liver and bones. The frequent recurrence of crisis can lead to chronic complications such as leg ulcers, blindness, and stroke. Acute chest syndrome, or chest crisis, is a common and particularly dangerous complication that is currently the leading cause of death among SCD patients.3 Ambulatory care strategies such as nutritional counselling, folic acid supplementation, pain medication protocols, vaccinations and antibiotics for the prevention and treatment of infection, are essential to SCD management.4
In England, approximately three quarters of all SCD admissions to hospitals are by London residents. SCD is also one of the most common reasons to be admitted to hospital and has one of the highest rate of multiple admissions for individual patients. The distribution of SCD in London also shows 80% of all admissions are in people living in the most deprived areas.5,6
The London Borough of Brent is one high prevalence area for SCD.7,8 A pre-study focus group held at the Sickle Cell Society in Brent revealed low patient confidence in general practitioner (GP) knowledge of management strategies for SCD. The perception that GPs lack the skills to properly treat and control SCD may help to explain why SCD patients and their caregivers expressed a preference for attending the hospital emergency department (ED) during a crisis.9,10
The rising cost of healthcare places the health system in England under increasing pressure to reduce such inappropriate hospital admissions.11,12 The national confidential enquiry into patient outcome and death reports that a multidisciplinary and multi-agency approach is needed in the ongoing pain management of patients with sickle cell disease, and that this should largely be taking place outside of hospitals.6 The purpose of our analysis of emergency admissions of residents in Brent with SCD aims to provide a picture of admissions presenting at the ED and to identify areas for improving primary care intervention to improve the care of patients with SCD and reduce such admissions.
Methods
Data source
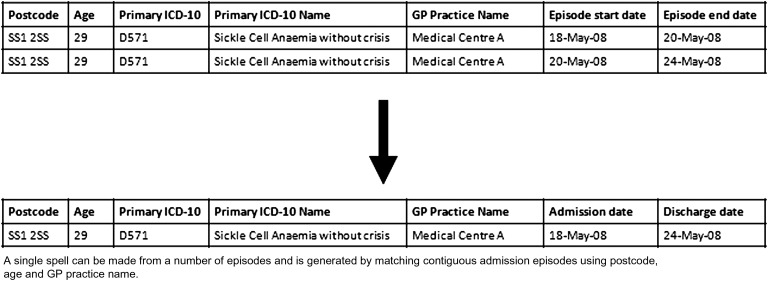
SUS (Secondary Uses Service) data were provided by NHS Brent for all admissions through the Emergency Department using temporal, admission and diagnostic parameters for the period January 2008 and July 2010 (Figure 1). Before analysis, data quality was checked by ensuring that episodes were commensurate with the admission and discharge dates of spells. Whilst in hospital patients may be under the care of a number of different consultants, each known as a finished consultant episode (FCE) and a spell is comprised of one or more continuous FCE. The FCE data was converted to spells by combining contiguous FCEs through cross-referencing a combination of postcode, age and registered practice. (Figure 2).
Figure 1.
Conversion of full consultant episode (FCE) data to admission spell
Figure 2.
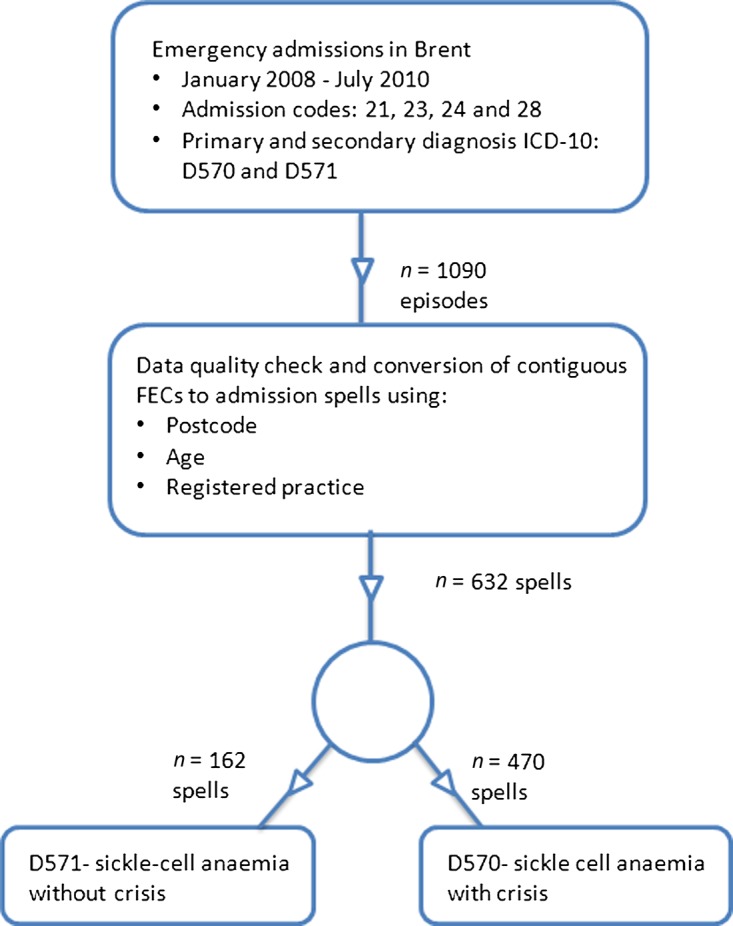
Schematic demonstrating the extraction, filtering, conversion and analysis of emergency admission data from NHS Brent
Analysis and outcome measures
Analysis was undertaken to compare admissions across the three diagnostic groups: sickle cell anaemia with crisis, sickle cell anaemia without crisis and sickle cell trait. Descriptive analysis of patients admitted with a diagnosis of sickle cell anaemia with crisis (D570) was undertaken; the main outcome measure was length of stay (average and <2 days versus ≥2 days) by age group and registered GP practice. Additional analysis of the frequency of individual patient admission was completed by linking patient spells over the period of analysis.
Results
Hospital emergency admissions
A total of 1090 episodes were identified, during the period January 2008 and July 2010, as emergency admissions, with either a primary or secondary diagnosis of sickle cell anaemia with crisis (D570), sickle-cell anaemia without crisis (D571) or sickle cell trait (D573). The conversion of episode data to admissions spells resulted in 632 unique spells, of which 470 spells included a diagnostic code for sickle cell anaemia with crisis (74.4 percent), 97 spells with sickle-cell anaemia without crisis (15.4 percent) and 65 spells with sickle cell trait (10.2 percent) (Figure 3). Only patients admitted with a primary or secondary diagnosis of sickle cell anaemia with crisis were included in subsequent analysis.
Figure 3.
Emergency admissions of patients registered at practices in the London borough of Brent
Length of stay and age
The most frequently admitted age group were patients between 21–25 years (85/470 spells). Thirty six percent of admissions resulted in a length of stay of less than two days (163/470 spells) (Figure 4).
Figure 4.
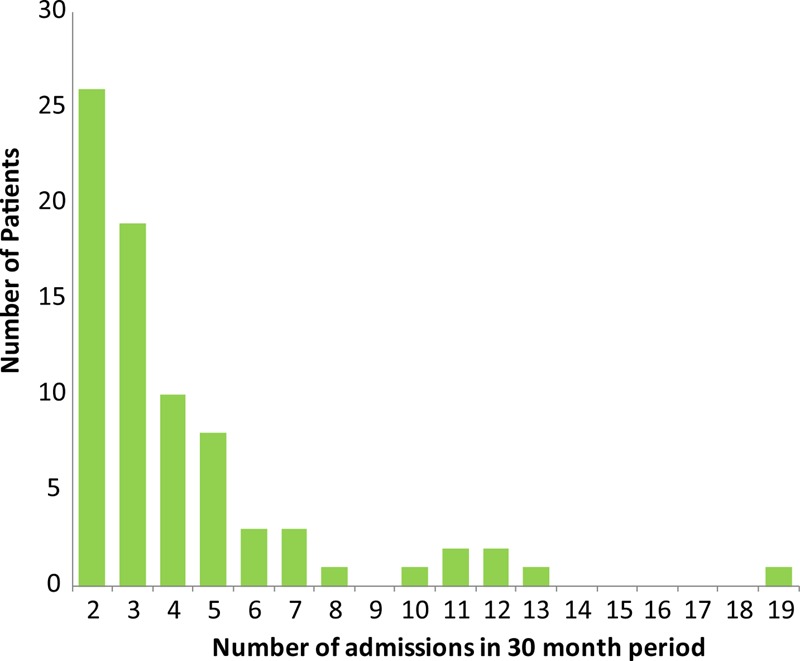
Emergency admissions between January 2008 and July 2010 for sickle cell crisis in NHS Brent by frequency of spells for individual patients admitted (total number of patients 77)
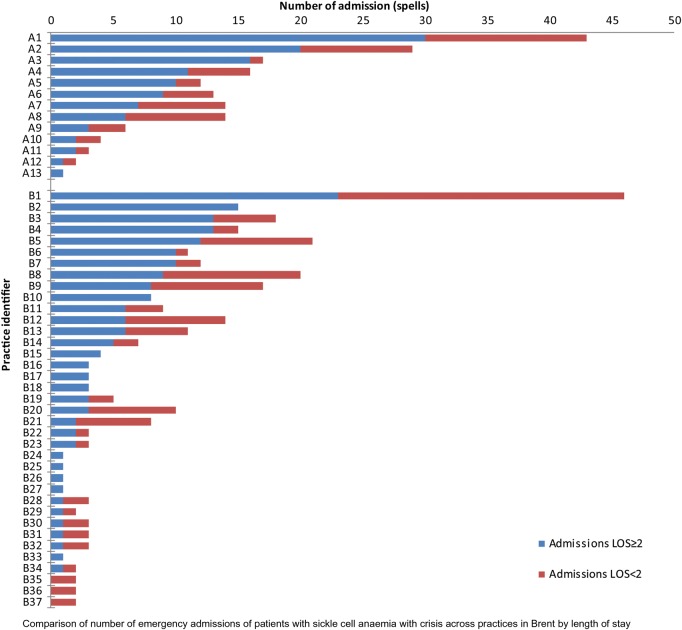
Practice level analysis
The practice level analysis included all practices in NHS Brent where registered patients were admitted over the 30 month study period. Practices were split into two groups, those involved in a current Sickle Cell Disease educational programme (Group A) and those not involved (Group B). The educational programme started after the current study end date (July 2010). Group A comprised of 15 GP practices plus one GP access centre with approximately 20 full-time and 9 part-time GPs and an estimated 50 registered patients with SCD. Group B is comprised of 55 practices with approximately 122 full-time and 61 part-time GPs, and an estimated 155 registered patients with SCD. Two practices were identified in Group A with the highest numbers of admissions A7 (43 spells) and A6 (29 spells), and have some of the highest rates of emergency admissions for Sickle Cell crisis. Within Group B, practice B3 had the highest number (47 spells) (Table 1).
Table 1.
Parameters for data extraction
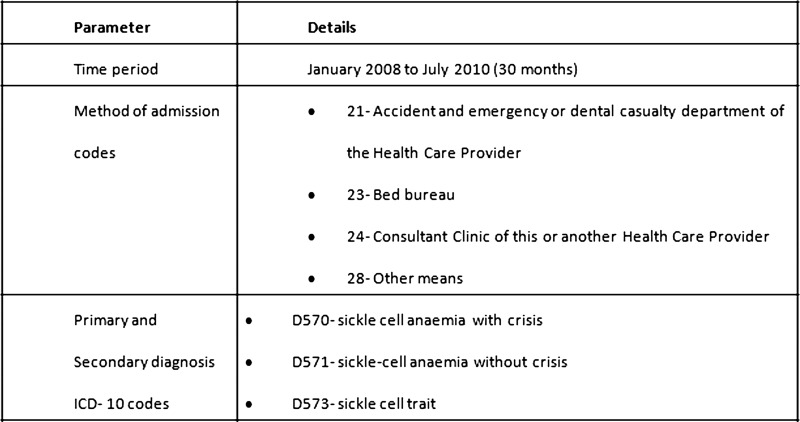 |
SUS data were provided by NHS Brent for all emergency hospital admissions of patients living in the London borough of Brent with one of three ICD-10 codes for the period January 2008 until July 2010
Multiple admissions
Seventy-seven patients accounted for multiple admissions (327 spells) and 143 patients were single admissions (143 spells). Multiple admissions accounted for 1530 bed days and 74% of the total number of admissions (Table 2).
Table 2.
Comparison of patients admitted with sickle cell crisis by length of stay (LoS) for various age groups (0–75 years)
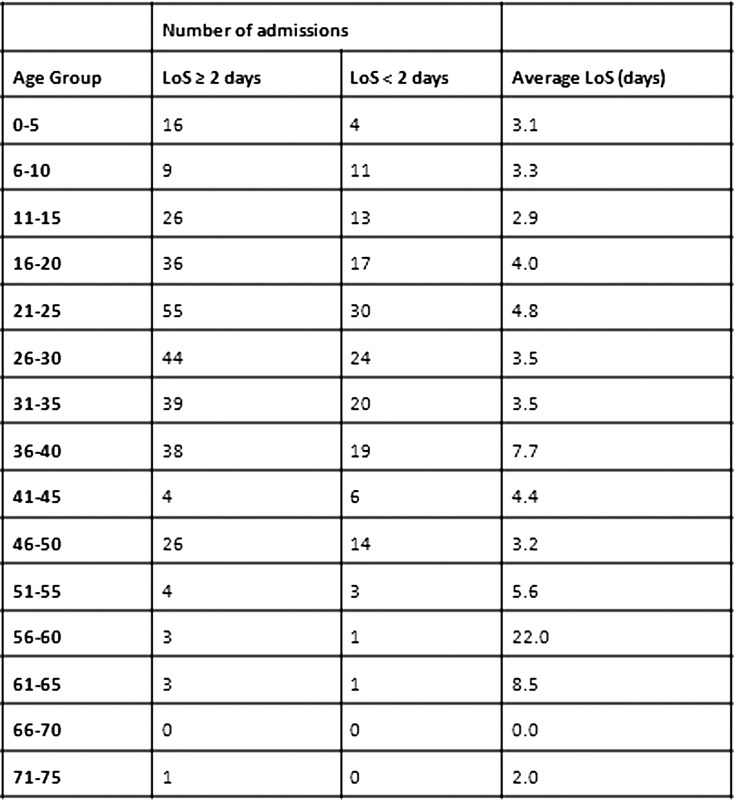 |
Most patients admitted were between the ages of 21-25 years and admissions with a length of stay less than 2 days form a significant proportion of all admissions.
Discussion
Main findings
This analysis showed that 36% of SCD patient admissions resulted in a length of stay of less than two days, and 74% of total bed days are inpatients with multiple admissions. Patients with short length of stay and multiple admissions may be good candidates for primary care interventions to reduce their risk of SCD-related complications and admissions. They may also benefit from more supportive management when they attend emergency departments, sickle cell centres and outpatient clinics, as many aspects of the management of SCD patients are outside the remit of primary care teams. The study also identified two GP practices, currently part of a GP education programme, that have patients who frequently seek emergency care for SCD-related problems. The Group A Practices will be assessed to identify any benefits realized from an educational intervention designed to help further engage GPs in the care and management of their sickle cell patients. Such benefits may include increasing the quality of care for patients with SCD and reducing the inappropriate use of the ED.
Limitations of the analysis
The analysis has certain limitations which could limit its transferability to areas outside of north-west London. The analysis is based on an area with a high prevalence of SCD. GPs in such areas may be more open to the idea of an educational intervention and more committed to its implementation. In addition, the data did not include those patients that attended the ED but were not admitted into hospital. Future studies may need to account for this subset of patients, as they may also have unmet needs and make high use of NHS resources. A planned GP educational intervention may reduce the number of patients admitted for two days or less or with multiple admissions, but we do not yet know that these patients could be managed in primary care.
Comparison with Existing Literature
This analysis is consistent with other studies that have identified potentially inappropriate use of acute inpatient care as a growing concern, and earmarked the important benefits of GP involvement and primary care in limiting this utilization.13–15 Inappropriate ED attendance distracts ED staff attention and resources from severe and acute cases that need urgent hospital care; adds to the waiting times in the ED, compromises the quality of care a patient receives and increases cost.16 While severe crises require the resources of secondary care and tertiary care, the long-term management of uncomplicated sickle cell pain episodes may be more effectively and efficiently managed in a primary care setting.17 Interventions that move management of SCD, particularly uncomplicated sickle cell pain episodes from tertiary towards primary care, have been successfully implemented elsewhere.15,18
One study showed an average annual reduction of 804 bed days over a three year period, with the average daily cost of a specialist haematology inpatient bed estimated at £356.12,19 Another study saw a 40% reduction in sickle cell ED attendance by introducing a local day hospital concept where SCD patients could bypass the ED and seek primary care plus within a hospital setting.18
Implications for future research and clinical practice
This analysis of Sickle Cell crisis admissions provided an opportunity to not only characterize the admissions but to identify practices with higher levels of admissions especially related to multiple admissions or short length of stays. It also establishes a baseline to monitor progress and validate associations in relation to improving primary care support for patients and reducing ED admissions. The strategic engagement of a small number of GPs followed by further rollout across the London Borough of Brent, will ensure that the delivery of the GP education package is targeted where needed. This programme will make use of the joint work that Brent is carrying out with voluntary groups in its locality with the aim of improving patient experience and addressing health inequalities.20 The data analysis can also facilitate discussions between primary and secondary care as part of the multi-disciplinary, multi-professional project team, as well as encourage ongoing work to explore patient satisfaction through the enhanced care delivered by GPs and with the aim of improving the patient experience.
Conclusions
Patients with SCD make relatively high use of urgent care services, including inpatient care. More appropriate management of these patients in the community may limit this demand and contribute to better health outcomes for patients, as well as economic benefits for the local health economy.
DECLARATIONS
Competing interests
None
Funding
NIHR CLAHRC for Northwest London and NHS Brent
Ethical approval
Ethics approval was not required for this work as it is part of a service evaluation and improvement project
Guarantor
SAG
Contributorship
SG, RB and CA conceived of the study; SG performed all analyses, GA wrote the first draft; all authors contributed in the revision of the manuscript
Acknowledgements
The Department of Primary Care & Public Health at Imperial College is grateful for support from the NIHR Biomedical Research Centre scheme and the Imperial Centre for Patient Safety and Service Quality. Disclaimer: This article presents independent research commissioned by the National Institute for Health Research (NIHR) under the Collaborations for Leadership in Applied Health Research and Care (CLAHRC) programme for Northwest London. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Reviewer
Tehmina Bharucha
References
- 1.Streetly A, Clarke M, Downing M, et al. Implementation of the newborn screening programme for sickle cell disease in England: results for 2003–2005. Journal of Medical Screening 2008;15:9–13 [DOI] [PubMed] [Google Scholar]
- 2.Quinn C, Rogers Z, McCavit T, Buchanan G Improved survival of children and adolescents with sickle cell disease. Blood 2010;115:3447–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moore F, Mortimer P, Wooller J Updated Sickle Cell Crisis Guidelines. Joint Royal Colleges Ambulance Liaison Committee. 2009
- 4.Sickle-cell disease and other haemoglobin disorders. Fact sheet N°308. WHO, January 2011. Online http://www.who.int/mediacentre/factsheets/fs308/en/index.html (last accessed 18 August 2011)
- 5.London Health Observatory 2006. Analysis of Frequent Hospital Users, by PCT 2003/4. [Online]. http://www.lho.org.uk/viewResource.aspx?id=10286 (last accessed July 2011)
- 6.Lucas SB, Mason DG, Mason M, Weyman D A Sickle Crisis? National Confidential Enquiry into Patient Outcome and Death. 2008
- 7.Northwest London Sickle Cell & Thalassaemia Managed Clinical Network. Annual Report & Action Plan 2006–7. 2005.
- 8.Hickman M, Modell B, Greengross P, et al. Mapping the Prevalence of Sickle Cell and Beta Thalassaemia in England: estimating and validating ethnic-specific rates. British Journal of Haematology 1999;104:860–7 [DOI] [PubMed] [Google Scholar]
- 9.Okoye O, AlJuburi G Patient Perspective of Primary Care Management of Sickle Cell Disease. The Society for Academic Primary Care: London and South-East Region Annual Scientific Meeting 2011
- 10.Lega F, Mengoni A Why non-urgent patients choose emergency over primary care services? Empirical evidence and managerial implications. Health Policy 2008;88:326–38 [DOI] [PubMed] [Google Scholar]
- 11.Carret ML, Fassa AG, Domingues MR Inappropriate use of emergency services: a systematic review of prevalence and associated factors. Cad. Saúde Pública 2009;25:7–28 [DOI] [PubMed] [Google Scholar]
- 12.Wright J, Bareford D, Wright C, et al. Day case management of sickle pain: 3 years experience in a UK sickle cell unit. British Journal of Haematology 2004;126:878–80 [DOI] [PubMed] [Google Scholar]
- 13.Boeke JP, van Randwijck-Jacobze ME, de Lange-Klerk EMS, Grol SM, Kramer M, van der Horst HE Effectiveness of GPs in accident and Emergency Departments. British Journal of General Practice 2010;60:378–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dale J, Lang H, Roberts JA, Green J, Glucksman E Cost effectiveness of treating primary care patients in accident and emergency: a comparison between general practitioners, senior house officers and registrars. BMJ 1996;312:1340–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coleman P, Irons R, Nicholl J Will alternative immediate care services reduce demands for non-urgent treatment at accident and emergency? Emergency Medical Journal 2001;18:482–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martin A ‘Inappropriate’ attendance at an accident and emergency department by adults registered in local general practices: how is it related to their use of primary care? Journal of Health Service Research and Policy 2002;7:160–5 [DOI] [PubMed] [Google Scholar]
- 17.Lenfant C (ed.). The Management of Sickle Cell. NIH publication No. 02-2117, 4th Edition. [Online] Bethesda: National Institute of Health; 2002. Available from: http://www.nhlbi.nih.gov/health/prof/blood/sickle/sc_mngt.pdf (last accessed July 2011)
- 18.Benjamin LJ, Swinson GI, Nagel RL Sickle cell anemia day hospital: an approach for the management of uncomplicated painful crisis. Blood 2000;95:1130–6 [PubMed] [Google Scholar]
- 19.Netten A, Curtis I Unit Costs of Health and Social Care 2002. Personal Social Services Unit, University of Kent, 2002 [Google Scholar]
- 20.Majeed A, Banarsee R, Molokhia M Health Disparities and Community Participation in England. Journal of Ambulatory Care Management 2009;32:297–301 [DOI] [PubMed] [Google Scholar]