Abstract
Background
Prior annualized estimates of pediatric ischemic stroke incidence have ranged from 0.54 to 1.2 per 100,000 U.S. children, but relied purely on diagnostic code searches to identify cases. We sought to obtain a new estimate using both diagnostic code searches and searches of radiology reports, and to assess the relative value of these two strategies.
Methods
Using the population of 2.3 million children (<20 years old) enrolled in a Northern Californian managed care plan (1993–2003), we performed electronic searches of (1) in-patient and out-patient diagnoses for ICD-9 codes suggestive of stroke and cerebral palsy (CP) and (2) radiology reports for keywords suggestive of infarction. Cases were confirmed through chart review. We calculated sensitivities and positive predictive values (PPV) for the two search strategies.
Results
We identified 1,307 potential cases from the ICD-9 code search, and 510 from the radiology search. A total of 205 ischemic stroke cases were confirmed, yielding an ischemic stroke incidence of 2.4 per 100,000 person-years. The radiology search had a higher sensitivity (83%) than the ICD-9 code search (39%), although both had low PPV’s. For perinatal stroke, the sensitivity of the stroke ICD-9 codes alone was 12%, versus 57% for stroke and CP codes combined; the radiology search was again the most sensitive (87%).
Conclusions
Our incidence estimate doubles that of prior U.S. reports, a difference at least partially explained by our use of radiology searches for case identification. Studies relying purely on ICD-9 code searches may underestimate childhood ischemic stroke rates, particularly for neonates.
Keywords: Stroke, ischemic, Child, Neonatal, Incidence
INTRODUCTION
Pediatric stroke has been increasingly recognized as an important cause of childhood disability. Prior annualized incidence estimates in the U.S. range from 0.54–1.2 ischemic strokes per 100,000 children.1–5 However, these studies have typically relied on International Classification of Diseases, 9th Revision (ICD-9) codes for the identification of cases. Several reports have documented the limited and variable accuracy of stroke ICD-9 codes when applied to adults,6, 7 and a single pediatric study has shown the same for the use of these codes in children.8 These data demonstrate the importance of case confirmation through chart review in the generation of stroke incidence estimates. However, because these reports did not address the sensitivity of ICD-9 code searches, they provide no insight into how many stroke cases are missed by epidemiologic studies relying solely on this search strategy.
Kaiser Permanente Medical Care Program (KPMCP) is a large comprehensive health care plan in Northern California that maintains extensive electronic medical records, including radiology data, on all of its members. Using KPMCP as our setting, we sought to (1) obtain a more accurate estimate of the incidence of pediatric ischemic stroke in the U.S. by using both ICD-9 code searches of diagnosis databases and text-string searches of radiology reports for case identification; and (2) to assess the relative value of these two search strategies.
METHODS
We addressed these questions using the Kaiser Pediatric Stroke Study (KPSS), a retrospective cohort study that attempted to identify all stroke cases within the population of children (0 to 19 years of age) enrolled in KPMCP from 1/1993 through 12/2003; its methods have been partially described in prior reports using KPSS data.9, 10 The institutional review boards at KPMCP and the University of California, San Francisco approved this study.
Setting
KPMCP, the largest nonprofit managed-care organization in the country, has 16 hospitals and 36 outpatient clinics that provide care to approximately 30% of the population of Northern California. During the 11 year study period, 2.3 million children were members and made up our cohort. The demographics of KPMCP are similar to those of California as a whole except for underrepresentation of socioeconomic extremes.11 KPMCP maintains extensive electronic databases that include demographics, all in-patient and out-patient diagnoses (comprehensive since 1993), and all radiology reports (comprehensive since 1997). In-patient diagnoses are coded by a trained medical records abstracter, while out-patient diagnoses are coded by the medical provider: the physician, for medical visits, or the therapist, for rehabilitation visits. All care received at outside hospitals is captured within the electronic databases. The rare exception could occur if a child has dual forms of insurance and only the alternate insurance pays for the stroke hospitalization. However, because such children would likely return to KPMCP for follow-up, they might still be identified through an out-patient stroke diagnosis or follow-up brain imaging. Discharge summaries, and other records from outside hospitalizations, are placed in the traditional KPMCP medical charts.
Case ascertainment
KPSS employed two search strategies to identify cases of pediatric stroke (ischemic and hemorrhagic) within the study cohort: (1) diagnostic (ICD-9) code searches and (2) radiology text string searches. For the first, we searched the electronic medical records of all 2.3 million children for hospital discharge and outpatient diagnoses suggestive of a stroke. This included the following ICD-9 codes: 430 (subarachnoid hemorrhage), 431 (intracerebral hemorrhage), 433.xx (occlusion/stenosis of precerebral arteries), 434.xx (occlusion of cerebral arteries), 435.xx (transient cerebral ischemia), 436 (acute cerebrovascular disease), 437.x (“other and ill-defined cerebrovascular disease” including 437.4, cerebral arteritis; 437.5, moyamoya disease; and 437.6, nonpyogenic thrombosis of intracranial venous sinus), and 438.x (late effects of cerebrovascular disease). Because some children with perinatal stroke might only receive a diagnosis of “hemiplegic CP,” we cross-referenced with a prior study that utilized a KPMCP birth cohort (all births from 1/1991 through 12/2002), and identified pediatric stroke cases through searches of the following CP codes: 342.x (hemiplegia), 343.x (infantile CP), and 344.xx (other paralytic syndromes).12, 13
For the radiology search, we performed electronic text string searches of the formal reports of all head imaging, including CT, CT angiogram (CTA), MRI, MR angiogram (MRA), and conventional angiogram. Text strings included: stroke, infarct# (includes infarction, infarcted), thromb# (includes thrombus, thromboembolic, thromboembolism, thrombotic, thrombosis), ischemi# (includes ischemia, ischemic), lacun# (includes lacune, lacunar), vascular event, and porencephal# (includes porencephaly, porencephalic). We could not electronically distinguish between those reports affirming the presence of infarction and those negating it. Hence, the full imaging reports were then reviewed by a pediatric neurologist (H.J.F.) to exclude those not consistent with stroke, such as reports identified in the search because they stated, “no evidence of ischemia.”
Cases of hemorrhagic stroke were sought through the ICD-9 code search alone. Because of the large number of imaging reports negating the presence of blood, and our inability to electronically distinguish these from reports affirming hemorrhage, it was not feasible to search for hemorrhagic strokes through the radiology database. Hence, our comparisons of the two search strategies were limited to ischemic stroke alone. However, hemorrhagic strokes incidentally identified through the radiology search for infarction were included in KPSS. We chose to include hemorrhagic stroke in this report as we could assess the accuracy of its ICD-9 codes (430, 431).
Case confirmation
Cases identified through either the ICD-9 code search or radiology search were then subjected to chart review. Two neurologists (H.J.F., Y.W.W.) independently confirmed cases of childhood stroke; a third (S.C.J.) arbitrated disputes. The criteria for stroke were: (1) documented clinical presentation consistent with stroke, such as a sudden onset focal neurological deficit, headache, loss of consciousness, or seizure; and (2) CT or MRI showing a focal ischemic infarct, or intracerebral, subarachnoid, and/or intraventricular hemorrhage, in a location and of a maturity consistent with the neurological signs and symptoms. Ischemic stroke included both arterial ischemic stroke and venous sinus thrombosis; hemorrhagic stroke included intracerebral, subarachnoid, or intraventricular hemorrhage, but excluded extra-axial hemorrhages. We also ascertained cases of transient ischemic attack (TIA), defined as a focal neurological deficit of acute onset lasting <24 hours, with no radiographic evidence of an infarct, and clinical suspicion of a TIA by a physician.
Cases were excluded if the stroke occurred prior to enrollment in Kaiser or outside of the study period. We also excluded cases of neonatal intraventricular hemorrhage (occurring in the first 28 days of life) as these are typically considered a distinct entity related to immaturity of the germinal matrix or choroid plexus. All other perinatal strokes, defined as those occurring between 28 weeks gestation and 28 days of life, were included.12, 14 This included the so-called “presumed perinatal strokes” that present in a delayed fashion, but are presumed to happen around the time of birth.15 Strokes occurring from 29 days through 19 years of age were called “later childhood strokes.”
Data abstraction
A single pediatric RN trained medical records analyst reviewed all available electronic and traditional medical records from all KPMCP facilities, and abstracted data on each confirmed case using a standardized protocol. All relevant records were reviewed by a single pediatric vascular neurologist (H.J.F.) to classify the stroke type and determine the underlying etiology; strokes without an apparent etiology were defined as idiopathic.
Data analysis
Stroke incidence rates were calculated for the study period when radiology records were complete (1/1997–12/2003) as the number of strokes occurring during that study period divided by the total number of person-years at risk. We compared the utility of our two search strategies for the identification of pediatric ischemic stroke cases by calculating both sensitivities and positive predictive values (PPV).16 Sensitivity of a search strategy was defined as the number of confirmed ischemic stroke cases identified through that particular search strategy divided by the total number of confirmed ischemic stroke cases. (The “gold standard” was therefore the combination of all search strategies employed in the study.) Sensitivities were calculated using only cases that occurred during the study period when radiology records were complete (1997–2003). Because prior studies have typically relied on ICD-9 code searches of in-patient diagnoses only, we performed stratified analyses to determine the sensitivity of such an in-patient search and the added benefit of an out-patient search. We similarly assessed the added benefit of searching CP ICD-9 codes to identify ischemic stroke cases. We performed additional stratified analyses by age-group, stroke sub-type, and whether or not the stroke was idiopathic.
PPV was defined as the proportion of confirmed cases to potential cases for a particular search strategy. PPV’s were calculated for the two search strategies. In addition, because the accuracy of a stroke code could differ when applied to an in-patient versus an out-patient, we calculated PPV’s of stroke ICD-9 codes in the in-patient and out-patient setting. PPV’s were also calculated for individual ICD-9 codes (including hemorrhagic stroke codes) to assess the accuracy of each code.
We used chi-square tests (or Fisher’s exact, when appropriate) to compare proportions. Alpha was set at 0.05. All statistical comparisons were performed using Stata 9.0 (College Station, TX).
RESULTS
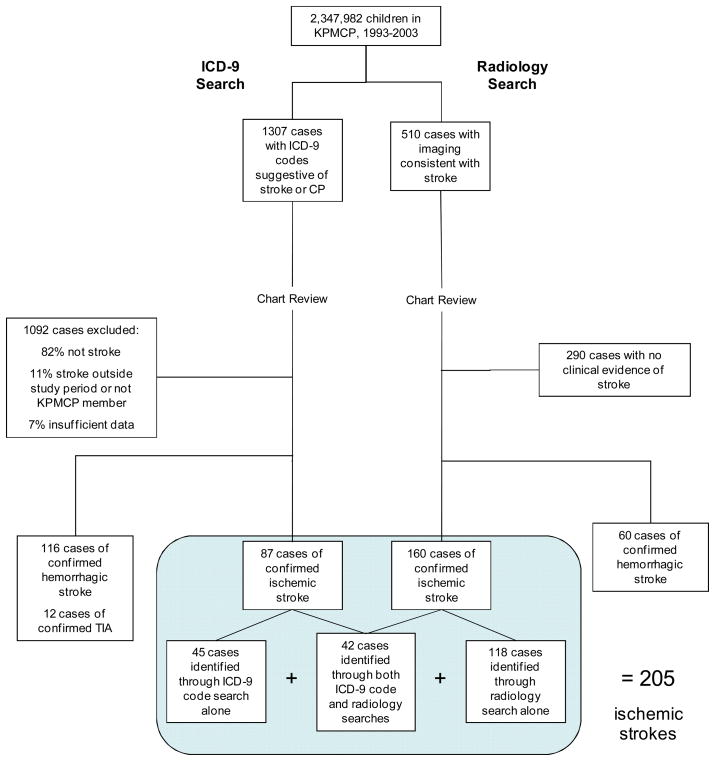
For KPSS, we searched the records of 2,347,982 children enrolled in KPMCP from 1993–2003 (including 1,775,441 enrolled from 1997–2003, when electronic radiology records were complete). The diagnostic code search identified 441 cases with ischemic- or hemorrhagic-stroke-related codes and an additional 866 cases with CP codes (Figure). The radiology search identified 9,599 head imaging reports (regarding 8,658 individual children) with stroke-related text strings; review of these reports yielded 510 cases with imaging consistent with stroke (infarction, intracerebral hemorrhage, or subarachnoid hemorrhage). Through independent chart review, a total of 205 cases of ischemic stroke were confirmed: 84 perinatal and 97 later childhood arterial ischemic strokes; 9 perinatal and 15 later childhood venous sinus thromboses. Of these, only 42 were identified through both search strategies, while 45 were identified through the ICD-9 code search alone, and 118 through the radiology search alone. We identified an additional 12 cases of TIA and 153 cases of hemorrhagic stroke (21 in neonates, 93 in older children); 37 (24%) hemorrhagic strokes were incidentally identified through the radiology search, and had no stroke ICD-9 code.
Figure.
Flow chart demonstrating methods for the ascertainment of stroke cases among 2.3 million children enrolled in KPMCP, 1993–2003. Because electronic radiology reports were not comprehensive until 1997, our incidence rate estimates and sensitivity analyses excluded cases from 1993–1996; totals for those analyses are therefore different than from those in this diagram. CP=cerebral palsy.
Stroke incidence (1997–2003)
Of the 205 ischemic stroke cases, 132 occurred between 1997–2003, yielding an ischemic stroke incidence of 2.4 per 100,000 person-years (95% CI, 2.0–2.9) during that study period. The incidence of later-childhood ischemic stroke (excluding perinatal cases, n=60) was 1.3 per 100,000 person-years (95% CI 1.0–1.7). Addition of hemorrhagic stroke cases (n=114) yielded a combined stroke incidence (all ages) of 4.6 per 100,000 person-years (4.0–5.2); inclusion of TIA cases (n=7) increased the total stroke incidence to 4.7 per 100,000 person-years (95% CI, 4.1–5.3).
From 1997–2003, there were 208,876 live births within KPMCP, and 60 ischemic strokes within that birth cohort. The prevalence of perinatal ischemic stroke was 29 per 100,000 live births (95% CI, 22–37), or 1 per 3500 live births. The overall prevalence of perinatal stroke (including 17 hemorrhagic stroke cases) was 37 per 100,000 live births (95% CI, 29–46), or 1 per 2700 live births.
Comparison of search strategies: sensitivities and PPV’s
While the radiology search was sensitive for ischemic stroke cases, the stroke ICD-9 code search identified only one third (Table 1). Searches limited to in-patient stroke ICD-9 codes identified only one fifth of ischemic stroke cases. The addition of CP ICD-9 codes to the search increased the sensitivity to 59%. The radiology search was the most sensitive strategy regardless of age-group, ischemic stroke sub-type, or etiology (Table 2). The sensitivity of the stroke ICD-9 code search was particularly low for perinatal ischemic strokes: 12%, compared to 50% for later childhood ischemic stroke. Conversely, the added benefit of CP ICD-9 code searches was greater in the younger age group, increasing the sensitivity by 45% for perinatal stroke, compared to only 9% for later childhood stroke.
Table 1.
Sensitivity and PPV by search strategy for ischemic stroke cases among children (0–19 years) enrolled in KPMCP, 1993–2003
| Sensitivity* |
PPV |
|||
|---|---|---|---|---|
| Search Strategy | N | % (95%CI) | N | % (95% CI) |
| Strategy 1: ICD-9 code search | ||||
| Stroke ICD-9 | 138 | 34 (26–42) | 277 ** | 29 (23–34) |
| Inpatient§ | 138 | 21 (14–29) | 65 ** | 77 (65–86) |
| Outpatient | 138 | 13 (5–15) | 212 ** | 14 (9.8–20) |
| CP ICD-9 alone¥ | 138 | 24 (18–32) | 866 | 2.2 (1.3–3.4) |
| Stroke + CP ICD-9 | 138 | 59 (50–67) | 1143 ** | 8.7 (7.1–10) |
| Strategy 2: radiology search | ||||
| Radiology | 138 | 83 (75–89) | 439 | 26 (22–31) |
| Combined Strategies | ||||
| Radiology and Stroke ICD-9 | 138 | 95 (90–98) | 716 ** | 28 (24–31) |
| All: Radiology and Stroke + CP ICD-9 | 138 | 100 | 1582 ** | 14 (12–16) |
study period limited to 1997–2003, when radiology databases were comprehensive
patients who received both in-patient and out-patient diagnostic codes are included in the in-patient group only
patients who recevied a cerebral palsy (CP) code but did not receive a stroke ICD-9 code
excludes cases with hemorrhagic stroke codes, 430 and 431
Table 2.
Sensitivity of search strategies for 138 childhood ischemic stroke cases among children (0–19 years) enrolled in KPMCP, 1997–2003, stratified by age group, stroke sub-type, and etiology
| Stroke ICD-9 | Stroke + CP ICD-9 | Radiology | |||
|---|---|---|---|---|---|
| Characteristic | N | % | % | % | p value |
| Overall | 138 | 34 | 59 | 83 | <0.0001 |
| Age group | |||||
| Perinatal | 60 | 12 | 57 | 87 | <0.0001 |
| Later childhood | 78 | 50 | 59 | 79 | <0.0001 |
| Ischemic stroke sub-type | |||||
| Arterial | 120 | 35 | 61 | 81 | <0.0001 |
| Venous | 18 | 22 | 39 | 94 | <0.0001 |
| Etiology | |||||
| Known etiology | 76 | 39 | 55 | 86 | <0.0001 |
| Idiopathic | 62 | 26 | 61 | 79 | <0.0001 |
N= total number of cases in that strata, found by any modality
We compared later childhood ischemic stroke cases that never received a stroke ICD-9 code (as either an in-patient or out-patient) to those that received a stroke code (Table 3). They were younger, more likely to have had their stroke as an in-patient, and less likely to have presented with a hemiparesis or speech-related deficit. They were more likely to have a major infection (mostly meningitis) or trauma as their stroke etiology, suggesting that their deficits may have been directly attributed to those etiologies rather than to stroke as the intermediary.
Table 3.
Comparison of children (>28 days old) with ischemic stroke who received a stroke diagnostic code (n=40) to those who did not (n=38), 1997–2003
| Code | No code | ||
|---|---|---|---|
| Variable | % | % | p-value* |
| Demographics | |||
| Age, years, mean (SD) | 13 (6.3) | 9.0(7.4) | 0.02§ |
| Male gender | 53 | 58 | 0.6 |
| White ethnicity | 43 | 37 | 0.6 |
| Presentation | |||
| Stroke as an in-patient | 5.0 | 32 | 0.002 |
| Hemiparesis | 70 | 44 | 0.02 |
| Dysarthria or aphasia | 50 | 23 | 0.02 |
| Seizure | 23 | 39 | 0.1 |
| Altered mental status | 24 | 47 | 0.04 |
| Past medical history | |||
| Cardiac disease | 10 | 2.6 | 0.4 |
| Hematologic disease | 10 | 7.9 | >0.9 |
| Autoimmune disease | 8.9 | 5.4 | 0.7 |
| Etiology | 0.03 | ||
| Idiopathic | 25 | 16 | |
| Cardiac disease | 13 | 5.3 | |
| Arteriopathy | 33 | 13 | |
| Hypercoaguable state | 7.5 | 5.3 | |
| Meningitis or sepsis | 15 | 45 | |
| Chemotherapy | 5.0 | 2.6 | |
| Hematologic malignancy | 2.5 | 2.5 | |
| Trauma | 0 | 7.9 | |
| Outcome (end of admission) | |||
| Normal (no deficit) | 35 | 22 | 0.2 |
| Dead | 0 | 2.6 | 0.5 |
p-values from chi-square tests, or Fisher’s exact when appropriate
p-value from student’s t-test
PPV of ICD-9 codes
In general, inpatient coding had a higher PPV than outpatient coding, and the hemorrhagic stroke codes had higher PPV’s than the ischemic stroke codes (Table 4). Code 436 was the most frequently utilized code, but had the lowest PPV.
Table 4.
PPV of diagnostic codes for ischemic and hemorrhagic stroke when applied to children in KPMCP, 1993–2003, in the in-patient and out-patient setting
| Inpatient |
Outpatient |
Overall |
||||
|---|---|---|---|---|---|---|
| ICD-9 Code | N | PPV % (95% CI) | N | PPV % (95% CI) | N | PPV % (95% CI) |
| Ischemic Stroke | ||||||
| 433.x (Occlusion of precerebral arteries) | 8 | 38 (9–76) | 3 | 0 (0–71) | 11 | 27 (6–61) |
| 434.x (Occlusion of cerebral arteries) | 31 | 74 (55–88) | 5 | 40 (5–85) | 36 | 69 (52–84) |
| 435.x (Transient cerebral ischemia) | 12 | 67 (35–90) | 40 | 10 (3–24) | 52 | 23 (13–37) |
| 436 (Acute, ill-defined cerebrovascular event) | 13 | 46 (19–75) | 164 | 19 (13–26) | 177 | 21 (15–28) |
| 437 (Other ill-defined cerebrovascular event) | 1 | 100 (3–100) | 0 | -- | 1 | 100 (3–100) |
| Hemorrhagic Stroke | ||||||
| 430 (Subarachnoid hemorrhage) | 39 | 82 (66–92) | 2 | 100 (16–100) | 41 | 83 (68–93) |
| 431 (Intracerebral hemorrhage) | 52 | 79 (65–89) | 71 | 49 (37–61) | 123 | 62 (53–70) |
| All Codes | 156 | 73 (65–80) | 285 | 26 (21–31) | 441 | 43 (38–48) |
N = Total number of potential stroke cases identified by ICD-9 codes search
DISCUSSION
Employing two search strategies for case identification—diagnostic code searches and radiology text string searches—we found an annual incidence of pediatric ischemic stroke of 2.4 per 100,000 person-years in a retrospective cohort of Northern Californian children. We found that radiology searches were more sensitive than diagnostic code searches, particularly for perinatal ischemic stroke, although both search strategies had limited accuracy, with low PPV’s.
Published pediatric stroke incidence rates are difficult to compare because of the multiple variables that could affect these estimates: population, demographics (higher rates in black children),4, 17 study time period (pre or post the MRI era), age range included, and multiple aspects of study design (e.g., retrospective vs. prospective; search strategies; methods of case confirmation). Our overall ischemic stroke incidence rate of 2.4 per 100,000 person-years is 2 to 4 fold higher than previously published estimates in U.S. children that also included perinatal strokes (Table 5).1, 2 Our estimate of 1.3 later childhood (non-neonatal) ischemic strokes per 100,000 person-years also exceeds estimates from those U.S. studies that excluded neonates.3–5 None of these prior reports used radiology searches to identify cases, and the majority of them relied only on inpatient stroke diagnoses.1–5, 18–20 Our study demonstrates the low sensitivity of such diagnostic code searches, suggesting that our expanded case identification methods, with the addition of radiology searches, may explain the higher ischemic stroke rate we observed. Had we relied only on stroke and CP ICD-9 code searches, we would have obtained an overall ischemic stroke incidence rate of only 0.97 per 100,000 person-years (95% CI: 0.78–1.2), a rate comparable to those reported in prior retrospective studies in the U.S. that used ICD-9 code searches alone (Table 5).1, 3–5
Table 5.
Comparison of incidence rate estimates for childhood stroke from prior and the current population-based studies
| Schoenberg2 1978 | Eeg-Olofsson17 1983 | Broderick1 1993 | Giroud20 1995 | Earley3 1998 | Fullerton4 2003 | Chung19 2004 | Zahuranec5 2005 | Present Study | |
|---|---|---|---|---|---|---|---|---|---|
| Number of incident cases (excluding TIA) | 4 | 5 | 16 | 28 | 35 | 2,278 | 94 | 7 | 358 |
| Population | Rochester, MN | Linkoping | Greater Cincinnati | Dijon | Baltimore-D.C. | California | Hong Kong | Nueces Cty, TX | KPMCP |
| Country | USA | Sweden | USA | France | USA | USA | China | USA | USA |
| Study Period | 1965–1974 | 1970–1979 | 1988–1989 | 1985–1993 | 1988 and 1991 | 1991–2000 | 1998–2001 | 2002–2003 | 1997–2003 |
| Age Range (years unless otherwise noted) | 0–15 * | 0–15 | 0–15 | 0–15 | 1–14 | >30 days-19 | >1 month-15 | >1 month-19 | 0–19 years |
| Ethnically diverse | No | No | Yes | No | Yes | Yes | No | Yes | Yes |
| Study Methods | |||||||||
| Retrospective (R) vs. Prospective (P) | R | R | R | P | R | R | R | R | R |
| Search strategy employed | Not stated | Not stated | ICD-9 | Registry | ICD-9 | ICD-9 | ICD-9 | ICD-9 | ICD-9 & radiology |
| In-patient versus out-patient diagnoses | Both | Not stated | In-patient only¥ | Both | In-patient only | In-patient only | In-patient only | In-patient only | Both |
| Case confirmation through chart review | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes |
| Incidence, per 100,000 person-years (95% CI) | |||||||||
| Ischemic | 0.63 (0.016–3.5)§ | Not stated | 1.2 (0.3–2.0) | 7.9 (4.6–12.7) | 0.58 (0.37–1.3) | 1.2 (1.1–1.3) | Not stated | 0.54 (0.01–3.0)§ | 2.4 (2.0–2.9) |
| Hemorrhagic | 1.9 (0.39–5.5)§ | Not stated | 1.5 (0.4–2.3) | 5.1 (2.6–9.1)§ | 0.71 (0.28–1.2) | 1.1 (1.2-1.2) | Not stated | 3.2 (1.2–7.1)§ | 2.1 (1.7–2.5) |
| Total (ischemic and hemorrhagic) | 2.5 (0.69–6.5)§ | 2.1 (0.69–5.0)§ | 2.7 (1.4–4.1) | 13.0 (8.7–18.8)§ | 1.3 (0.82–2.1) | 2.3 (2.2–2.4) | 2.1 (1.7–2.5) | 3.8 (1.5–7.8)§ | 4.6 (4.0–5.2) |
Excluded “strokes associated with birth, intracranial infection, or trauma”
Calculated binomial exact 95% confidence intervals (CI) using numbers reported in manuscript
Except for review of out-patient records from a sickle cell disease clinic
Included only non-Hispanic whites and Mexican-Americans
The highest published rate of childhood ischemic stroke (including perinatal stroke) was from a population-based study in Dijon, France (study period 1988–1989): 7.9 per 100,000 person-years.21 This was the only prospective study (Table 5), and therefore did not rely on any retrospective search strategies for case identification. Rather, it was a registry where all stroke cases were identified prospectively in both the in-patient and out-patient setting as part of a larger epidemiologic stroke study that included adults. Although the higher rate may also reflect a different patient population, it does suggest that incidence rates from retrospective studies are likely underestimates.
In our study, we found that ICD-9 code searches are not only insensitive for pediatric stroke but also fairly inaccurate: the poor PPV of many stroke codes has been previously reported, and was confirmed in our study (Supplemental-Table).6–8 These data have unfortunate implications on pediatric stroke research which has depended largely on retrospective observational studies. Administrative datasets, for example, have been useful because they allow the identification of a large number of subjects with this relatively rare disease. However, these studies typically rely on ICD-9 codes alone for case identification and therefore are not only missing false negative cases, but including false positives. The latter issue can be overcome in studies where cases can be confirmed through chart review, but this is typically not an option for studies utilizing administrative datasets. When available, radiology text-string searches, although time consuming with a low yield, appear to be a better option for retrospectively detecting ischemic stroke cases. However, in evaluating and designing studies relying on diagnostic code searches alone, investigators should consider which subjects are most likely to be missed: among the later childhood stroke cases that did not receive an ICD-9 code, almost half had meningitis or sepsis as their stroke etiology, and therefore might actually be excluded from certain stroke studies.
Our study has several limitations. Our conclusions regarding the relative advantages of the two search strategies are limited in that we studied only a single large managed care program. Because coding practices may differ in different institutions, our findings may not be generalizable to other settings. This may explain differences in the PPV of some specific ICD-9 codes compared to a prior pediatric report;8 however, overall, PPV’s were remarkably consistent between studies (Supplemental-Table). Another limitation is that we likely failed to detect some cases, despite our use of two search strategies. Of particular concern are KPMCP patients that present acutely to a non-Kaiser hospital; head imaging studies performed outside of the KMPCP system would not have been included in our radiology text-string search. However, diagnostic codes for all out-of-plan care are maintained in KPMCP databases and were searched for this study. In addition, these patients usually return to the KPMCP system for follow-up head imaging and follow-up clinical care. However, missed cases would impact both our stroke incidence estimates and estimates of the sensitivity of the different search strategies. For the latter, the “gold standard” was simply the combination of the different retrospective strategies. Had our gold standard been a thorough and comprehensive prospective registry, as done in Dijon, France, the sensitivity estimates would have been even lower.
Despite these limitations, our study is the first to employ two search strategies to estimate the incidence of pediatric ischemic stroke in the U.S., and found a rate 2 to 4 times higher than prior reports. Although radiology searches appear to have a greater sensitivity for pediatric stroke, both search strategies have relatively low yield. These challenges in retrospective case identification support recent calls for the field to move towards prospective multicenter studies of pediatric stroke.5, 22
Supplementary Material
Acknowledgments
Research Support: American Heart Association Scientific Development Grant; Neurological Sciences Academic Development Award (K12 NS01692); Independent Scientist Award (K02 NS053883).
Footnotes
Disclosure: The authors have no conflicts of interest to disclose.
References
- 1.Broderick J, Talbot GT, Prenger E, Leach A, Brott T. Stroke in children within a major metropolitan area: the surprising importance of intracerebral hemorrhage. J Child Neurol. 1993;8(3):250–255. doi: 10.1177/088307389300800308. [DOI] [PubMed] [Google Scholar]
- 2.Schoenberg BS, Mellinger JF, Schoenberg DG. Cerebrovascular disease in infants and children: a study of incidence, clinical features, and survival. Neurology. 1978;28:763–768. doi: 10.1212/wnl.28.8.763. [DOI] [PubMed] [Google Scholar]
- 3.Earley CJ, Kittner SJ, Feeser BR, Gardner J, Epstein A, Wozniak MA, Wityk R, Stern BJ, Price TR, Macko RF, Johnson C, Sloan MA, Buchholz D. Stroke in children and sickle-cell disease: Baltimore-Washington Cooperative Young Stroke Study. Neurology. 1998;51(1):169–176. doi: 10.1212/wnl.51.1.169. [DOI] [PubMed] [Google Scholar]
- 4.Fullerton HJ, Wu YW, Zhao S, Johnston SC. Risk of stroke in children: Ethnic and gender disparities. Neurology. 2003;61(2):189–194. doi: 10.1212/01.wnl.0000078894.79866.95. [DOI] [PubMed] [Google Scholar]
- 5.Zahuranec DB, Brown DL, Lisabeth LD, Morgenstern LB. Is it time for a large, collaborative study of pediatric stroke? Stroke. 2005;36(9):1825–1829. doi: 10.1161/01.STR.0000177882.08802.3c. [DOI] [PubMed] [Google Scholar]
- 6.Goldstein LB. Accuracy of ICD-9-CM coding for the identification of patients with acute ischemic stroke: effect of modifier codes. Stroke. 1998;29(8):1602–1604. doi: 10.1161/01.str.29.8.1602. [DOI] [PubMed] [Google Scholar]
- 7.Broderick J, Brott T, Kothari R, Miller R, Khoury J, Pancioli A, Gebel J, Mills D, Minneci L, Shukla R. The Greater Cincinnati/Northern Kentucky Stroke Study: preliminary first-ever and total incidence rates of stroke among blacks. Stroke. 1998;29(2):415–421. doi: 10.1161/01.str.29.2.415. [DOI] [PubMed] [Google Scholar]
- 8.Golomb MR, Garg BP, Saha C, Williams LS. Accuracy and yield of ICD-9 codes for identifying children with ischemic stroke. Neurology. 2006;67(11):2053–2055. doi: 10.1212/01.wnl.0000247281.98094.e2. [DOI] [PubMed] [Google Scholar]
- 9.Fullerton HJ, Wu YW, Sidney S, Johnston SC. Risk of recurrent childhood arterial ischemic stroke in a population-based cohort: the importance of cerebrovascular imaging. Pediatrics. 2007;119(3):495–501. doi: 10.1542/peds.2006-2791. [DOI] [PubMed] [Google Scholar]
- 10.Fullerton HJ, Wu YW, Sidney S, Johnston SC. Recurrent hemorrhagic stroke in children: a population-based cohort study. Stroke. 2007;38(10):2658–2662. doi: 10.1161/STROKEAHA.107.481895. [DOI] [PubMed] [Google Scholar]
- 11.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82(5):703–710. doi: 10.2105/ajph.82.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee J, Croen LA, Backstrand KH, Yoshida CK, Henning LH, Lindan C, Ferriero DM, Fullerton HJ, Barkovich AJ, Wu YW. Maternal and infant characteristics associated with perinatal arterial stroke in the infant. Jama. 2005;293(6):723–729. doi: 10.1001/jama.293.6.723. [DOI] [PubMed] [Google Scholar]
- 13.Wu YW, Croen LA, Shah SJ, Newman TB, Najjar DV. Cerebral palsy in a term population: Risk factors and neuroimaging findings. Pediatrics. 2006 doi: 10.1542/peds.2006-0278. in press. [DOI] [PubMed] [Google Scholar]
- 14.Lynch JK, Nelson KB. Epidemiology of perinatal stroke. Curr Opin Pediatr. 2001;13(6):499–505. doi: 10.1097/00008480-200112000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Golomb MR, MacGregor DL, Domi T, Armstrong DC, McCrindle BW, Mayank S, deVeber GA. Presumed pre- or perinatal arterial ischemic stroke: risk factors and outcomes. Ann Neurol. 2001;50(2):163–168. doi: 10.1002/ana.1078. [DOI] [PubMed] [Google Scholar]
- 16.Everitt BS. The Cambridge Dictionary of Statistics in the Medical Sciences. Cambridge: Cambridge University Press; 1995. [Google Scholar]
- 17.Fullerton HJ, Chetkovich DM, Wu YW, Smith WS, Johnston SC. Deaths from stroke in US children, 1979 to 1998. Neurology. 2002;59(1):34–39. doi: 10.1212/wnl.59.1.34. [DOI] [PubMed] [Google Scholar]
- 18.Eeg-Olofsson O, Ringheim Y. Stroke in children. Clinical characteristics and prognosis. Acta Paediatr Scand. 1983;72(3):391–395. doi: 10.1111/j.1651-2227.1983.tb09734.x. [DOI] [PubMed] [Google Scholar]
- 19.Biagioni E, Cioni G, Cowan F, Rutherford M, Anker S, Atkinson J, Braddick OJ, Canapicchi R, Guzzetta A, Mercuri E. Visual function and EEG reactivity in infants with perinatal brain lesions at 1 year. Dev Med Child Neurol. 2002;44(3):171–176. doi: 10.1017/s0012162201001888. [DOI] [PubMed] [Google Scholar]
- 20.Chung B, Wong V. Pediatric stroke among Hong Kong Chinese subjects. Pediatrics. 2004;114(2):e206–212. doi: 10.1542/peds.114.2.e206. [DOI] [PubMed] [Google Scholar]
- 21.Giroud M, Lemesle M, Gouyon J, Nivelon J, Milan C, Dumas R. Cerebrovascular disease in children under 16 years of age in the city of Dijon, France: a study of incidence and clinical features from1985 to 1993. J Clin Epidemiol. 1995;48(11):1343–1348. doi: 10.1016/0895-4356(95)00039-9. [DOI] [PubMed] [Google Scholar]
- 22.Lynch JK, Hirtz DG, DeVeber G, Nelson KB. Report of the National Institute of Neurological Disorders and Stroke workshop on perinatal and childhood stroke. Pediatrics. 2002;109(1):116–123. doi: 10.1542/peds.109.1.116. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.