Abstract
Background
Limited data exist, particularly from the more generalizable perspective of a community-wide investigation, about recent trends in ambulance use, and factors associated with ambulance use, in patients hospitalized with acute myocardial infarction.
Objective
The objectives of this population-based prospective epidemiologic study were to describe decade long trends (1997-2007) in the use of emergency medical services (EMS) by residents of the Worcester, Massachusetts, metropolitan area hospitalized for acute myocardial infarction (AMI) and to describe the characteristics of patients with AMI transported to the hospital by EMS (n=3,789) compared with those transported by other means (n=1,505).
Methods
The study population consisted of 5,294 patients hospitalized for AMI at 11 greater Worcester medical centers in 5 annual periods between 1997 and 2007. Information about the use of EMS, and factors associated with EMS use, were obtained through the review of hospital medical records.
Results
There was a progressive increase in the proportion of greater Worcester residents with AMI transported to central Massachusetts hospitals by ambulance over time (66.9% transported in 1997; 74.9% transported in 2007). Patients transported by EMS were older, more likely to be women, and to have a greater prevalence of previously diagnosed comorbidities.
Conclusions
Our findings provide encouragement for the use of EMS in residents of a large central New England community hospitalized with AMI. Despite increasing trends in ambulance use, more research is needed to explore the reasons why patients with AMI do not utilize EMS in the setting of an acute cardiac emergency.
Keywords: emergency medical services, acute myocardial infarction, pre-hospital transport, changing trends
Introduction
Despite encouraging ongoing national declines in the death rates due to coronary heart disease (1,2), acute myocardial infarction (AMI) remains a leading cause of morbidity and mortality in American men and women. A fundamental principle in treating patients with an evolving AMI is that “time is tissue”. Indeed, the faster a patient who is experiencing symptoms of AMI can present to an acute care facility, be accurately diagnosed and early evidence-based therapy instituted, and transferred if necessary for more definitive care, the better their short-term outcomes (3-5). The optimal treatment of persons with symptoms of AMI requires two major steps in the pre-hospital setting. First, patients need to recognize their symptoms as an emergency and activate emergency medical services (EMS). Second, EMS personnel must then expediently transport the patient to the nearest appropriate health care facility.
Several studies have investigated the use of EMS in the management of patients hospitalized with AMI, including the transmission of pre-hospital electrocardiograms, bypassing patients to PCI-capable hospitals, and the early activation of cardiac catheterization centers (5-7). Ambulance transport is the recommended means of hospital transport by the American Heart Association/American College of Cardiology for patients with an evolving AMI (8). However, few studies, particularly during recent periods and from the more generalizable perspective of a community-based investigation, have examined trends in the extent of use and characteristics of patients with AMI who are transported by ambulance compared to persons transported to the hospital by other means.
The purpose of this longitudinal study was to describe the overall utilization of, and decade long trends in, EMS by residents of central Massachusetts hospitalized for AMI at all metropolitan Worcester (MA) medical centers in 5 study years between 1997 and 2007. A secondary study goal was to describe the characteristics of patients transported to greater Worcester medical centers by EMS compared with those who used other means of transportation. The present study extends our previous investigation which examined trends in the use of EMS by residents of the Worcester metropolitan area between 1997 and 2003 (9). Since the early diagnosis and treatment with coronary reperfusion therapy is particularly relevant for patients with ST-segment-elevation MI (STEMI) (10,11), we further examined trends in our principal study endpoints, namely EMS use, and factors associated with EMS use, in this subgroup of patients which was not done in our earlier report (9). Furthermore, we collected information in the present study about the use of pre-hospital ECG's and treatments administered during EMS transport. Data from the Worcester Heart Attack Study were utilized for this investigation (12,13).
Methods
Patient Population Characteristics
The Worcester Heart Attack Study is an ongoing population-based longitudinal investigation which is examining long-term trends in the descriptive epidemiology of AMI in residents of the Worcester (MA) metropolitan area (2000 census = 478,000) who were hospitalized with a discharge diagnosis of AMI and other coronary disease rubrics at all central Massachusetts medical centers (12,13). Greater Worcester residents hospitalized with AMI at all metropolitan Worcester medical centers on a biennial basis beginning in 1997 comprised the population of this report. The periods under study were selected due to the availability of grant funding and for purposes of examining trends in incidence and case-fatality rates of AMI over an alternating yearly basis. All 11 hospitals in the Worcester metropolitan area participated in this community-wide study. Of these hospitals, 3 were tertiary care medical centers. Human subject approval for this study was obtained from the Committee for the Protection of Human Subjects at the University of Massachusetts Medical School.
The details of this study have been described elsewhere (11,12). In brief, the medical records of residents of the Worcester metropolitan area who had been hospitalized for possible AMI, based on the review of several International Classification of Diseases (ICD) rubrics in which AMI may have occurred, were individually reviewed and validated according to pre-defined diagnostic criteria by trained study physicians and nurses. These diagnostic rubrics included ICD-9 codes for AMI (410), angina (411), chronic CHD (412-414), and acute chest pain (786.5). A standardized working definition of STEMI was utilized in this investigation to classify this subgroup of patients (14). This diagnosis was made when new ST-segment elevation was present at the J point in 2 or more contiguous leads. Cases of peri-operative-associated AMI, patients who developed an AMI during hospitalization for another admission were not included in this investigation.
Data Collection
Socio-demographic, medical history, and clinical data were abstracted from the emergency department logs and hospital medical records of eligible patients with AMI by trained study physicians and nurses in whom ongoing quality control checks were routinely performed. Information was collected about a number of key independent variables which may be associated with EMS use. These factors included patient's age, sex, race, year of hospitalization, length of hospital stay, acute symptoms at the time of hospital admission, history of several previously diagnosed comorbidities (e.g., prior diabetes, stroke, heart failure), do not resuscitate (DNR) status, AMI type (STEMI versus Non-STEMI) (14), AMI order (initial episode vs. prior history of MI), and laboratory (e.g., serum glucose values) and physiologic (e.g., baseline blood pressure) findings. Information was collected about the prescribing of different cardiac medications and receipt of coronary interventional procedures. Information was also collected about hospital door to reperfusion time (e.g., receipt of PCI) in patients with an STEMI.
Data Analysis
The statistical significance of decade long trends (1997-2007) in the use of EMS in our study population was examined through the use of chi-square tests for trend. Differences in the distribution of demographic, medical history, and clinical factors in patients with AMI who were transported by EMS, as compared to those who were transported by other means, were examined using chi square and t tests for discrete and continuous variables, respectively.
A logistic multivariable regression analysis was used to examine factors associated with the utilization of EMS in our study population. The factors included in this analysis, in which the dependent variable was use of EMS, were demographic (e.g., age, sex), clinical (e.g., prior comorbidities, AMI order and type), physiologic (e.g., blood pressure findings), and situational (e.g., weekend vs. weekday, time of day or evening) factors. These potential predictor variables were included in our regression models either because they differed between patients transported by EMS as compared to those transported by other means at a p value of <0.20 or because they have been previously shown to be of importance in the prognosis of patients hospitalized with AMI. We also carried out a similar logistic regression analysis in which we examined clinical and demographic factors associated with the utilization of EMS in patients with STEMI.
Results
Study Population Characteristics
During the decade long period under study, a total of 5,294 residents of the Worcester metropolitan area were hospitalized for independently confirmed AMI. Of these, 1,870 (35.3%) experienced an STEMI. The average age of hospitalized patients was 72 years, 55% were male, and the majority were white (Table I). In the overall study population, 72% (3,789/5,294) utilized EMS for transport to the hospital during the 6 years under study; the overall utilization of EMS by patients with an STEMI was essentially similar (71%) (1,325/1,870).
Table I.
Characteristics of Patients Hospitalized With Acute Myocardial Infarction (AMI) According to Whether They Were Transported to Central Massachusetts Medical Centers By Emergency Medical Services (EMS)
| Total Population | Patients With ST-Segment Elevation AMI | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | EMS (+) (n=3,789) | EMS (-) (n=1,505) | P value | EMS (+) (n=1,325) | EMS (-) (n=545) | P value | ||||
| Age (mean, years) | 3,706 | 73.8 | 1,497 | 65.9 | <.001 | 1,305 | 69.7 | 542 | 62.5 | <.001 |
| Age (years) | n | % | n | % | n | % | n | % | ||
| <55 | 374 | 9.9 | 363 | 24.1 | <.001 | 230 | 17.4 | 171 | 31.4 | |
| 55-64 | 526 | 13.9 | 311 | 20.7 | 241 | 18.2 | 128 | 23.5 | <.001 | |
| 65-74 | 767 | 20.3 | 351 | 23.3 | 280 | 21.2 | 125 | 22.9 | ||
| 75-84 | 1,218 | 32.2 | 338 | 22.5 | 354 | 26.7 | 88 | 16.2 | ||
| ≥85 | 901 | 23.8 | 142 | 9.4 | 219 | 16.5 | 33 | 6.1 | ||
| Male | 1,922 | 50.7 | 996 | 66.2 | <.001 | 728 | 54.9 | 390 | 71.6 | <.001 |
| White | 3,387 | 89.4 | 1,352 | 89.8 | 0.63 | 1,177 | 88.8 | 490 | 89.9 | 0.50 |
| Prior DNR order | 330 | 8.7 | 35 | 2.3 | <.001 | 70 | 5.3 | 9 | 1.7 | <.001 |
| Medical History | ||||||||||
| Angina | 776 | 20.5 | 282 | 18.7 | 0.15 | 228 | 17.2 | 74 | 13.6 | <.05 |
| Hypertension | 2,725 | 71.9 | 976 | 64.9 | <.001 | 858 | 64.8 | 308 | 56.5 | <.001 |
| Diabetes | 1,321 | 34.9 | 457 | 30.4 | <.005 | 356 | 26.9 | 134 | 24.6 | 0.31 |
| Heart failure | 1,148 | 30.3 | 215 | 14.3 | <.001 | 224 | 16.9 | 43 | 7.9 | <.001 |
| Stroke | 529 | 14.0 | 124 | 8.2 | <001 | 147 | 11.1 | 30 | 5.5 | <.001 |
| Cancer | 606 | 16.0 | 202 | 13.4 | <.05 | 183 | 13.8 | 70 | 12.8 | 0.58 |
| Kidney disease | 733 | 19.4 | 178 | 11.8 | <.001 | 175 | 13.2 | 39 | 7.2 | <.001 |
| Symptoms | ||||||||||
| Chest pain | 2,533 | 66.9 | 1,205 | 80.1 | <.001 | 1,014 | 76.5 | 478 | 87.1 | <.001 |
| Shortness of breath | 2,256 | 59.5 | 801 | 53.2 | <.001 | 728 | 54.9 | 277 | 50.8 | 0.10 |
| Abdominal pain | 292 | 7.7 | 120 | 8.0 | 0.79 | 82 | 6.2 | 40 | 7.3 | 0.36 |
| Arm/shoulder pain | 460 | 12.2 | 302 | 20.1 | <.001 | 202 | 15.3 | 148 | 27.2 | <.001 |
| Left arm pain | 770 | 20.3 | 453 | 30.1 | <.001 | 371 | 28.0 | 209 | 38.4 | <.001 |
| Back pain | 432 | 11.4 | 222 | 14.8 | <.001 | 185 | 14.0 | 85 | 15.6 | 0.37 |
| Rapid heart rate/palpitations | 274 | 7.2 | 101 | 6.7 | 0.55 | 61 | 4.6 | 28 | 5.1 | 0.62 |
| Diaphoresis | 1,360 | 35.9 | 520 | 34.6 | 0.39 | 631 | 47.6 | 254 | 46.6 | 0.69 |
| AMI Characteristics | ||||||||||
| Initial | 2,332 | 61.6 | 1,043 | 69.3 | <.001 | 924 | 69.7 | 427 | 78.4 | <.001 |
| Q Wave | 854 | 22.8 | 357 | 24.0 | 0.35 | 633 | 48.0 | 265 | 48.9 | 0.71 |
| STEMI | 1,325 | 35.0 | 545 | 36.2 | 0.39 | |||||
| Weekend | 1,072 | 28.4 | 465 | 31.2 | <.05 | 390 | 29.6 | 181 | 33.6 | 0.09 |
| Time of Day | ||||||||||
| 12:00 a.m.-5:59 a.m. | 656 | 17.4 | 195 | 13.0 | 223 | 16.9 | 80 | 14.8 | ||
| 6:00 a.m.-11:59 a.m. | 1,190 | 31.5 | 475 | 31.7 | <.01 | 419 | 31.7 | 148 | 27.4 | 0.07 |
| 12:00 p.m.-5:59 p.m. | 1,116 | 29.5 | 508 | 33.9 | 408 | 30.9 | 197 | 36.4 | ||
| 6:00 p.m.-11:59 p.m. | 819 | 21.7 | 320 | 21.4 | 272 | 20.6 | 116 | 21.4 | ||
| Physiologic findings (at hospital admission) | ||||||||||
| Systolic blood pressure (mean, mmHg) | 3,599 | 138.4 | 1,423 | 151.7 | <.001 | 1,242 | 134.6 | 513 | 152.0 | <.001 |
| Diastolic blood pressure (mean, mmHg) | 3,450 | 74.3 | 1,415 | 83.6 | <.01 | 1,194 | 75.7 | 507 | 86.3 | <.001 |
| Laboratory findings (at hospital admission) | ||||||||||
| Serum glucose (mean, mg/dl) | 3,711 | 186.7 | 1,476 | 165.2 | <.001 | 1,291 | 181.7 | 534 | 168.6 | <0.01 |
| Total cholesterol (mean, mg/dl) | 1,721 | 175.2 | 833 | 181.2 | 0.57 | 692 | 176.6 | 325 | 187.6 | <.001 |
| Estimated GFR* (mean) | 3,654 | 56.1 | 1,476 | 65.7 | 0.28 | 1,285 | 62.3 | 532 | 72.0 | <.001 |
glomerular filtration rate (ml/min/1.73m2)
Trends in EMS Use
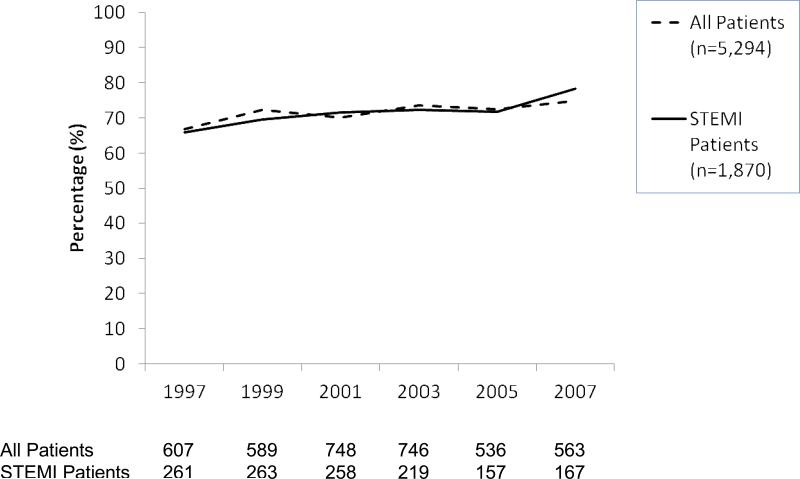
The proportion of all patients with AMI transported by ambulance exhibited a progressive increase over time (Figure 1; p for trend <0.01); the lowest proportion of EMS transports was observed in the earliest study year (67% (607/908) in 1997), whereas the highest utilization rates were observed during the most recent year under study (75% (563/752) in 2007). Since EMS activation is particularly relevant for patients with STEMI, we examined trends in the use of EMS by greater Worcester residents hospitalized with an STEMI during the years under study (Figure 1); trends similar to those noted in the overall study population were observed. Among these patients, 66% (261/396) called for an ambulance in 1997, 72% in 2003 (219/303), and 78% (167/213) in 2007 (p for trend <0.01).
Figure 1.
Trends in the Utilization of Emergency Medical Services by Patients Hospitalized With Acute Myocardial Infarction
Characteristics of patients hospitalized with AMI according to EMS use
Patients who utilized EMS transport (n=3,789) were significantly older, more likely to be female, were more likely to have a prior DNR order in their hospital records, and were more likely to have a medical history of several important comorbidities compared to those transported by other means (n=1,505) (Table I). Patients transported by ambulance to greater Worcester hospitals were less likely to have complained of chest pain, left arm or shoulder pain, or back pain at the time of hospital presentation, but were more likely to have complained about shortness of breath, and have a different physiologic and laboratory profile. Patients transported by ambulance were more likely to have had a previously diagnosed MI and sought medical care on the weekends and in the early morning hours as compared to patients transported by other means (Table I).
In a similar manner, we examined the characteristics of the 1,325 patients with STEMI who were transported by ambulance as compared to the 545 patients who were transported by other means (Table I). Similar to the overall study population, patients with STEMI transported by ambulance were older, were more likely to be women, have a previous DNR order in their medical charts, experience different symptoms of AMI, have various comorbidities present, have been previously diagnosed with an AMI, and have a different physiologic profile at the time of hospital presentation than patients who were not transported by EMS.
Among the 1,643 patients undergoing PCI, the median time to the receipt of PCI was significantly shorter in those transported by ambulance as compared to those transported by other means (11.0 vs 20.6 hours) (p<.01).
We carried out a logistic multivariable regression analysis for purposes of identifying those demographic, situational, medical history, and clinical factors that were associated with EMS use, separately in the total study population and in those hospitalized with an STEMI (Table II). The results of this multivariable analysis showed that patients transported by EMS were significantly more likely to be older, nonwhite, female, have a prior DNR order in their medical charts, complain of diaphoresis at the time of hospital presentation, have a history of heart failure or stroke, present with an STEMI, have significantly lower blood pressure values, but higher serum glucose findings, and be hospitalized at all central Massachusetts hospitals in 2003 and in 2007 (Table II). On the other hand, patients who did not complain of chest pain, abdominal pain, or arm/shoulder pain, who did not have a history of diabetes, or who did not experience their symptoms of acute coronary disease between 6 in the morning and 6 at night were significantly less likely to call for an ambulance than respective comparison groups.
Table II.
Factors Significantly Associated With Utilization of Emergency Medical Services in Patients Hospitalized With Acute Myocardial Infarction (AMI)
| Total Population | Patients With ST Segment Elevation AMI | |||
|---|---|---|---|---|
| Characteristic* | Adjusted O.R. | 95% CI | Adjusted O.R. | 95% CI |
| Age (years) | ||||
| 55-64 | 1.59 | 1.28,1.98 | 1.31 | 0.95,1.81 |
| 65-74 | 1.89 | 1.52,2.36 | 1.44 | 1.03,2.02 |
| 75-84 | 2.77 | 2.20,3.48 | 2.36 | 1.62,3.44 |
| ≥85 | 4.12 | 3.11, 5.47 | 2.95 | 1.74,4.99 |
| Male | 0.73 | 0.63,0.84 | 0.74 | 0.57,0.96 |
| White | 0.78 | 0.62,0.96 | ||
| Prior DNR order | 1.78 | 1.18,2.66 | ||
| Symptoms | ||||
| Chest pain | 0.75 | 0.63,0.89 | 0.67 | 0.48,0.95 |
| Abdominal pain | 0.77 | 0.60,0.99 | 0.59 | 0.38,0.92 |
| Arm/shoulder pain | 0.75 | 0.61,0.91 | 0.58 | 0.43,0.79 |
| Diaphoresis | 1.49 | 1.28,1.73 | 1.39 | 1.10,1.77 |
| Medical History | ||||
| Diabetes | 0.77 | 0.65,0.92 | ||
| Heart failure | 1.54 | 1.27,1.87 | ||
| Stroke | 1.33 | 1.06,1.66 | ||
| AMI Characteristics | ||||
| STEMI | 1.30 | 1.11,1.52 | -- | -- |
| Physiologic findings (at hospital admission) Systolic blood pressure (mmHg) | ||||
| 100-119 | 0.98 | 0.74,1.29 | 0.95 | 0.60,1.50 |
| 120-139 | 0.80 | 0.62,1.03 | 0.72 | 0.47,1.11 |
| 140-159 | 0.63 | 0.48,0.82 | 0.54 | 0.35,0.84 |
| ≥160 | 0.45 | 0.34,0.60 | 0.30 | 0.19,0.49 |
| Laboratory findings (at hospital admission) Serum glucose (mg/dl) | ||||
| 120-139 | 0.99 | 0.82,1.20 | 0.87 | 0.63,1.19 |
| 140-159 | 1.13 | 0.91,1.42 | 1.18 | 0.81,1.71 |
| 160-179 | 1.61 | 1.24,2.09 | 1.43 | 0.93,2.20 |
| 180-199 | 1.41 | 1.04,1.92 | 1.25 | 0.77,2.03 |
| ≥200 | 1.71 | 1.38,2.11 | 1.53 | 1.05,2.24 |
| Study Year | ||||
| 2003 | 1.37 | 1.10,1.72 | 1.46 | 1.01,2.12 |
| 2007 | 1.46 | 1.13,1.88 | 1.97 | 1.24,3.14 |
| Time of Day | ||||
| Morning | 0.70 | 0.57,0.86 | ||
| Afternoon | 0.69 | 0.56,0.85 | ||
referent groups age<55 years, female, non-white race, absence of a prior DNR order, absence of selected acute symptoms, absence of selected comorbid conditions, Non-STEMI, weekday, systolic blood pressure <100 mmHg, serum glucose <120 mg/dl, study year of 1997, 12:00 a.m – 5:59 a.m.
Similarly, in examining factors associated with calling for an ambulance in patients with an STEMI (Table II), patients with STEMI transported by ambulance had a relatively similar demographic, clinical, and situational profile to that of our overall study population, though fewer factors were significantly associated with calling for an ambulance or not.
Since the presence of a prior DNR order was strongly associated with EMS use, and is strongly linked to patient's prognosis, we also carried out a sensitivity analysis for purposes of characterizing factors associated with utilizing EMS restricted to persons without a DNR order. The results of this regression analysis, in which similar demographic, clinical, and situational factors were examined in relation to EMS use, were relatively consistent with our findings in the total study sample and in the subgroup of patients with STEMI (data not shown).
Treatments Received During EMS Transport
Beginning in 2003, information on medications administered to patients during EMS transport was collected in our surveillance study as this information had not been previously collected. Among the 1,845 patients transported by EMS in 2003, 2005, and 2007, the most frequent medications given during EMS transport were nitrates (47%), aspirin (42%), and diuretics (9%). A small proportion of patients received beta blockers (3%), and anti-arrhythmic agents (3%), and fewer than 1% received calcium channel blockers and ACE-inhibitors/ARBs. Among the 543 patients with an STEMI, nitrates, aspirin, and diuretics were administered to 58.9%, 57.1%, and 6.6% of these patients during EMS transport, respectively.
Beginning with new data collection efforts in 2005, we collected data on whether ECG's were performed during ambulance transport. In 2005 and 2007, 1,099 patients were transported by EMS and 26% (n=291) of these patients had an ECG performed during hospital transport. Patients who had an ECG recorded during transport were more likely to receive the following pre-hospital medications during transport compared to patients who used EMS, but did not have a pre-hospital ECG obtained: aspirin (65% vs. 38%), beta blockers (9% vs. 2%), and nitrates (63% vs. 45%) (p<.05). Patients who had an ECG performed en route to greater Worcester hospitals were also more likely to have undergone a PCI during hospitalization (57% vs. 43%), and to have undergone their PCI in a more rapid manner (19 hours vs. 36 hours), than patients in whom an ECG was not performed.
Discussion
The results of the present longitudinal study demonstrate that nearly three quarters of the residents of this large central Massachusetts community who were admitted to the hospital and ultimately diagnosed with an AMI were transported by ambulance during the years under study; this high level of utilization of EMS was observed in all patients hospitalized with AMI as well as in those with an STEMI. Increases in the use of EMS by all patients, and by those with STEMI, were observed between 1997 and 2007. Patients arriving to greater Worcester hospitals by ambulance had different demographic and clinical characteristics than patients transported to all central Massachusetts medical centers by other means.
Arrival to the hospital by EMS allows for the use of effective pre-hospital treatments, decreases delay to the receipt of important hospital-based therapies, and enables critically ill patients to be more effectively identified and treated in the emergency department (8). Despite the benefits from being transported to the hospital by trained pre-hospital providers, the use of EMS by patients with acute coronary disease may be less than optimal (15-18).
In the Atherosclerosis Risk in Communities Study, which was conducted in 4 large U.S. communities between 1987 and 2000, the use of EMS increased from 37% in 1987 to 44% during 2000 (15). Data from the National Registry of Myocardial Infarction showed that, between 1994-1998, approximately one half of patients hospitalized for AMI used EMS, with no significant changes in the use of EMS noted over the limited number of years under study (16). In a recent report from a large national cardiovascular disease registry, EMS transport was used by only 60% of patients with STEMI treated at 372 U.S. hospitals between 2007 and 2009 (18). In a previous report from the Worcester Heart Attack Study, approximately 7 out of every 10 greater Worcester residents hospitalized with AMI at all central Massachusetts medical centers between 1997 and 2003 activated the EMS system (9). The present study expands upon this prior report, demonstrating the slightly higher use of EMS among residents of the Worcester metropolitan area during more recent study years.
The utilization of EMS among greater Worcester residents hospitalized with AMI is relatively high compared to other previously published reports (15-18). An urban environment and proximity to large teaching hospitals have been previously associated with increased EMS use and these characteristics may be playing a role in the greater Worcester community. Another possible explanation for increased EMS use, particularly in the most recently hospitalized cohort, may be the implementation of universal health care coverage in Massachusetts in 2006. Other possible explanations for this higher utilization include patients hospitalized during a more recent period under study compared to prior investigations, greater patient familiarity and previous positive experiences with the local EMS, education by local primary care physicians and cardiologists about the benefits of hospital transport by EMS, or that a greater proportion of our study population was comprised of individuals that have been shown to be more likely to use EMS, namely the sick, the elderly, migrants, and the poor (16,19).
Despite encouraging increases in the use of EMS by greater Worcester residents during the years under study, approximately one quarter of central Massachusetts residents with AMI did not utilize EMS. These patients, by definition, could not receive pre-hospital ECG's and/or various treatment modalities en route to the hospital or have communication between EMS personnel and local hospitals. Previous studies have shown that, despite intensive community-based interventions and ongoing attempts of education of the general public, pre-hospital delay times have not significantly improved over time. Further increases in the utilization of EMS may be required before the average, as well as distribution of, pre-hospital delay times for patients experiencing signs and symptoms of acute coronary disease in the broader community setting can be improved upon.
Several prior studies have shown that patients with acute coronary disease who use EMS tend to be older, women, and have different racial characteristics in comparison to self-transported patients (16,17). On the other hand, conflicting findings have been reported on the symptom profiles and socioeconomic status of those using, compared to those not using, EMS (15,16,19). In the large multi-site national cardiovascular disease registry, STEMI patients who used EMS were significantly more likely to be older, women, were more likely to have government funded insurance, and were more likely to be hemodynamically unstable compared to STEMI patients who did not arrive at participating hospitals by ambulance (18).
The results of our study are consistent with these reports in showing that patients transported by ambulance tended to be female, older, of non-white race, and more ill than those using other means for transport (15,20). The finding that EMS users were also more likely to have a DNR order in their medical charts further supports the notion that users of EMS are in general more ill and elderly than those who use private transportation.
The present findings may help inform community-based educational efforts which are needed to not only identify patients who may be less likely to call for an ambulance in the setting of AMI symptoms but also to identify at risk groups, such as younger patients with AMI, who would benefit from this means of transport. Enhanced regionalization of the Worcester EMS system may have led to not only increased use by greater Worcester residents but may eventually prove to be effective in improving treatment times for the elderly, minorities, and women. Indeed, STEMI treatment times have been shown to improve in vulnerable patient subgroups of women, the elderly, and minorities through the use of a coordinated regional treatment protocol throughout North Carolina which included EMS transport (21). Health care providers and patient advocates need to encourage patients to both respond in a timely manner to the symptoms of AMI and to do so by calling 911. Patients with STEMI who were transported by ambulance have been previously shown to have shorter delays in symptom onset to arrival time and door to reperfusion time in comparison with self-transported patients (15).
Though emergency medical technicians are able to begin treatments in transit, relatively little is known about the treatments provided by EMS in the broader community setting. In the present study, the most common medications given en route to the hospital were nitrates and aspirin; this is likely due to these medications being part of a standard protocol for emergency medical technicians. However, while these medications were frequently given, their overall use was less than optimal.
Partial explanations for the suboptimal treatment of these patients may be that aspirin is usually administered when chest pain or angina is present and patients transported by EMS were less likely to have chest pain present. It may also be that since there was a higher prevalence of diabetes in patients transported by EMS, as well as older and potentially more cognitively impaired patients, that these patients were less apt to feel or report pain and be less aggressively treated. Moreover, some knowledgeable patients may have already taken certain medications for their acute symptoms, such as aspirin, prior to EMS arrival without the need for additional medications en route to the hospital or documentation of recent acute aspirin use by EMS personnel.
While the importance of obtaining a pre-hospital ECG is both well-established and recommended (8), the frequency of pre-hospital ECG's has remained low in our central Massachusetts community. The ACTION Registry reported that approximately one quarter of patients transported by EMS received a pre-hospital ECG in 2007 (22), and the results of our study are consistent with the findings from this national registry. Early ECG findings have only been shown to be effective in decreasing the time to angioplasty and coronary reperfusion when combined with the activation of an AMI hospital management team (23,24). The low overall use of pre-hospital ECGs in our study may be indicative of technology limitations in our local EMS system, or it may also be that the elderly patients transported by EMS in the present study had more non-specific symptoms which were less likely to result in the acquisition of a pre-hospital ECG. Further studies are needed to understand the barriers to having ECGs performed during hospital transport and whether new protocols can help improve the frequency of pre-hospital ECG's in the community and their transmission to emergency department physicians.
The strengths of the present study include its population-based design, its large sample of patients hospitalized with independently validated AMI, and its decade's long perspective. Our study has several limitations, however, that must be kept in mind in interpreting the present study results. Possible changes in the incidence rates of pre-hospital sudden cardiac death may have contributed to the findings observed and changed the case-mix of patients hospitalized with AMI. This study was unable to determine the reasons why patients chose to activate the EMS system and about the correctness of interpretation of their signs and symptoms of acute coronary disease (24,25). We studied predominantly Caucasian patients and our findings may lack generalizability to other racial or ethnic groups or to other EMS systems in communities throughout the U.S. Finally, we did not collect information about patient's educational or financial status, perceived severity of their acute symptoms, or prior ambulance use to examine their association with current EMS use.
In conclusion, the results of our study in residents of central Massachusetts suggest that there have been modest increases in the use of EMS by residents of this large metropolitan area hospitalized with AMI. However, the use of pre-hospital ECG's and treatment by EMS personnel has been modest. Several high risk groups, such as younger patients with AMI, also utilized EMS at less than optimal levels. Future studies should attempt to more fully explore and characterize the reasons why patients do not call 911 in the setting of an acute cardiac emergency, including patient fear, denial, embarrassment, reluctance to burden other family members or their providers, and lack of awareness of the benefits of EMS transport. Moreover, more novel educational interventions need to be designed to reduce the time lag between patient's symptoms of acute coronary disease and the receipt of definitive medical care. Efforts such as the American Heart Association's Mission: Lifeline initiative should continue to be encouraged with concomitant increases in the number of patients who receive timely access to coronary reperfusion, in part due to enhanced patient recognition of acute coronary related symptoms and activation of EMS (26).
Acknowledgements
This research was made possible by the cooperation of participating hospitals in the Worcester metropolitan area. Funding support was provided by the National Institutes of Health (RO1 HL35434). Partial salary support for Drs. Saczynski, Gore, and Goldberg was provided for by the National Institutes of Health grant 1U01HL105268-01. Dr. Saczynski was supported in part by funding from the National Institute on Aging (K01 AG33643).
Abbreviations List
- AMI
acute myocardial infarction
- EMS
emergency medical service
- STEMI
ST elevation myocardial infarction
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart disease and stroke statistics--2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ford ES, Capewell S. Coronary heart disease mortality among young adults in the U.S. from 1980 through 2002: concealed leveling of mortality rates. J Am Coll Cardiol. 2007;50:2128–32. doi: 10.1016/j.jacc.2007.05.056. [DOI] [PubMed] [Google Scholar]
- 3.Terkelsen CJ, Christiansen EH, Sorensen JT, Kristensen SD, Lassen JF, Thuesen L, et al. Primary PCI as the preferred reperfusion therapy in STEMI: it is a matter of time. Heart. 2009;95:362–9. doi: 10.1136/hrt.2007.139493. [DOI] [PubMed] [Google Scholar]
- 4.Maeng M, Nielson PH, Busk M, Mortensen LS, Kristensen SD, Nielsen TT, et al. Time to treatment and three-year mortality after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction-a DANish Trial in Acute Myocardial Infarction-2 (DANAMI-2) substudy. Am J Cardiol. 2010;105:1528–34. doi: 10.1016/j.amjcard.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 5.Le May MR, Dionne R, Maloney J, Poirier P. The role of paramedics in a primary PCI program for ST-elevation myocardial infarction. Prog Cardiovasc Dis. 2010;53:183–7. doi: 10.1016/j.pcad.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Postma S, Dambrink JH, de Boer MJ, Gosselink AT, Eggink GJ, van de Wetering H, et al. Prehospital triage in the ambulance reduces infarct size and improves clinical outcome. Am Heart J. 2011;161:276–82. doi: 10.1016/j.ahj.2010.10.028. [DOI] [PubMed] [Google Scholar]
- 7.Rezaee ME, Conley SM, Anderson TA, Brown JR, Yanofsky NN, Niles WW. Primary percutaneous coronary intervention for patients presenting with ST-elevation myocardial infarction: process improvements in rural prehospital care delivered by emergency medical services. Prog Cardiovasc Dis. 2010;53:210–18. doi: 10.1016/j.pcad.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction--executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction). J Am Coll Cardiol. 2004;44:671–719. doi: 10.1016/j.jacc.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 9.Goldberg RJ, Kramer DG, Yarzebski J, Lessard D, Gore JM. Prehospital transport of patients with acute myocardial infarction: a community-wide perspective. Heart & Lung: The Journal of Acute and Critical Care. 2008;37:266–74. doi: 10.1016/j.hrtlng.2007.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kushner FG, Hand M, Smith SC, Jr, King SB, 3rd, Anderson JL, Antman EM, et al. American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2009 Focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;120:2271–2306. doi: 10.1161/CIRCULATIONAHA.109.192663. [DOI] [PubMed] [Google Scholar]
- 11.Krumholz HM, Bradley EH, Nallamothu BK, Ting HH, Batchelor WB, Kline-Rogers E, et al. A campaign to improve the timeliness of primary percutaneous coronary intervention: Door-to- Balloon: an Alliance for Quality. JACC Interv. 2008;1:97–104. doi: 10.1016/j.jcin.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 12.Floyd KC, Yarzebski J, Spencer FA, Lessard D, Dalen JE, Alpert JS, et al. A 30 year perspective (1975-2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goldberg RJ, Spencer FA, Yarzebski J, Lessard D, Gore JM, Alpert JS, et al. A 25-year perspective into the changing landscape of patients hospitalized with acute myocardial infarction (the Worcester Heart Attack Study). Am J Cardiol. 2004;94:1373–8. doi: 10.1016/j.amjcard.2004.07.142. [DOI] [PubMed] [Google Scholar]
- 14.McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent Trends in the Incidence, Treatment, and Outcomes of Patients with ST and Non-ST-Segment Acute Myocardial Infarction. Am J Med. 2011;124:40–7. doi: 10.1016/j.amjmed.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGinn AP, Rosamond WD, Goff DC, Jr, Taylor HA, Miles JS, Chambless L. Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction experience in 4 U. S. communities from 1987-2000. Am Heart J. 2005;150:392–400. doi: 10.1016/j.ahj.2005.03.064. [DOI] [PubMed] [Google Scholar]
- 16.Canto JG, Zalenski RI, Ornato JP, Rogers WJ, Kiefe CI, Magid D, et al. National Registry of Myocardial Infarction 2 Investigators. Use of emergency medical services in acute myocardial infarction and subsequent quality of care: observations from the national registry of myocardial infarction 2. Circulation. 2002;106:3018–23. doi: 10.1161/01.cir.0000041246.20352.03. [DOI] [PubMed] [Google Scholar]
- 17.Meischke H, Eisenberg MS, Schaeffer SM, Damon SK, Larsen MP, Henwood DK. Utilization of emergency medical services for symptoms of acute myocardial infarction. Heart Lung. 1995;24:11–18. doi: 10.1016/s0147-9563(05)80090-1. [DOI] [PubMed] [Google Scholar]
- 18.Mathews R, Peterson ED, Li S, Roe MT, Glickman SW, Wiviott SD, et al. Use of emergency medical service transport among patients with ST-segment-elevation myocardial infarction. Findings from the National Cardiovascular Data Registry Acute Coronary Treatment Intervention Outcomes Network Registry-Get with the guidelines. Circulation. 2011;124:154–63. doi: 10.1161/CIRCULATIONAHA.110.002345. [DOI] [PubMed] [Google Scholar]
- 19.DeShaw PJ. Use of the emergency department by Somali immigrants and refugees. Minn Med. 2006;89:42–5. [PubMed] [Google Scholar]
- 20.Siepmann DB, Mann NC, Hedges JR, Daya MR. Association between prepayment systems and emergency medical services use among patients with acute chest discomfort syndrome. For the Rapid Early Action for Coronary Treatment (REACT) Study. Ann Emerg Med. 2000;35:573–8. [PubMed] [Google Scholar]
- 21.Glickman SW, Granger CB, Ou F-Sh, O'Brien S, Lytle BL, Cairns CB, et al. Impact of a statewide ST-segment-elevation myocardial infarction regionalization program on treatment times for women, minorities, and the elderly. Circ Cardiovasc Qual Outcomes. 2010;3:514–521. doi: 10.1161/CIRCOUTCOMES.109.917112. [DOI] [PubMed] [Google Scholar]
- 22.Diercks DB, Kontos MC, Chen AY, Pollack CV, Jr, Wiviott SD, Rumsfeld JS, et al. Utilization and impact of pre-hospital electrocardiograms for patients with acute ST-segment elevation myocardial infarction: data from the NCDR (National Cardiovascular Data Registry) ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry. J Am Coll Cardiol. 2009;53:161–6. doi: 10.1016/j.jacc.2008.09.030. [DOI] [PubMed] [Google Scholar]
- 23.Brown JP, Mahmud E, Dunford JV, Ben-Yehuda O. Effect of prehospital 12-lead electrocardiogram on activation of the cardiac catheterization laboratory and door-to-balloon time in ST-segment elevation acute myocardial infarction. Am J Cardiol. 2008;101:158–61. doi: 10.1016/j.amjcard.2007.07.082. [DOI] [PubMed] [Google Scholar]
- 24.Thuresson M, Jarlöv MB, Lindahl B, Svensson L, Zedigh C, Herlitz J. Thoughts, actions, and factors associated with prehospital delay in patients with acute coronary syndrome. Heart Lung. 2007;36:398–409. doi: 10.1016/j.hrtlng.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 25.Ottesen MM, Dixen U, Torp-Pedersen C, Kober L. Prehospital delay in acute coronary syndrome – an analysis of the components of delay. Int J Cardiol. 2004;96:97–103. doi: 10.1016/j.ijcard.2003.04.059. [DOI] [PubMed] [Google Scholar]
- 26.American Heart Association Mission: Lifeline. ( http://www.heart.org)