Abstract
Aim
To conduct a survey in a representative cohort of ambulatory patients with stable, well managed chronic heart failure (CHF) to discover their experiences of air travel.
Methods
An expert panel including a cardiologist, an exercise scientist, and a psychologist developed a series of survey questions designed to elicit CHF patients' experiences of air travel (Appendix 1). The survey questions, information sheets and consent forms were posted out in a self-addressed envelope to 1293 CHF patients.
Results
464 patients (response rate 39%) completed the survey questionnaires. 54% of patients had travelled by air since their heart failure diagnosis. 20% of all patients reported difficulties acquiring travel insurance. 65% of patients who travelled by air experienced no health-related problems. 35% of patients who travelled by air experienced health problems, mainly at the final destination, going through security and on the aircraft. 27% of all patients would not travel by air in the future. 38% of patients would consider flying again if there were more leg room on the aeroplane, if their personal health improved (18%), if they could find cheaper travel insurance (19%), if there were less waiting at the airport (11%), or if there were less walking/fewer stairs to negotiate at the airport (7%).
Conclusion
For most patients in this sample of stable, well managed CHF, air travel was safe.
Keywords: Survey, Risk, Flying, Health problems, Symptoms
1. Introduction
Air travel, for business, family or vacation, is part of modern life in Western societies. Lower costs, greater convenience of travel, and greater longevity mean that older, retired people now frequently wish to travel by air and many of these travellers will have chronic ailments, including chronic heart failure (CHF). Cabin pressure in modern airliners is set to that equivalent to an altitude of approximately 8000 ft (2438 m) above sea level, which gives a partial pressure of oxygen similar to that of breathing approximately 15% oxygen at sea level. In healthy people, this leads to an increased respiratory rate, and a reduction in arterial oxygen partial pressure (PaO2) and arterial oxygen saturation [1–3]. Operation EVEREST III suggested that altitude-induced hypoxaemia led to an increase in heart rate, a decline in stroke volume, an increase in the atrial component of left ventricular filling and a progressive rise in pulmonary vascular resistance, all of which are of potential concern in patients with CHF [4].
The assessment of flight risk has received little attention and we could identify few studies that have formally assessed the risk of air travel in CHF. We showed that in 21 patients with CHF (NYHA class III/IV), lying supine and breathing 15% oxygen for 1 h caused a drop in arterial oxygen saturation to 86% but patients remained asymptomatic throughout [5]. In a study of 38 patients with CHF, exercise testing at sea level and simulated altitudes up to 3000 m using a fraction of inspired oxygen (FiO2) of 14% [6] did not result in any angina, arrhythmias or ECG evidence of ischaemia. At peak exercise at a simulated altitude of 3000 m, the most symptomatic patients had the largest decrease in both arterial oxygen saturation (SaO2, to 88%) and exercise capacity (to 66% of that attained at simulated sea level). The study concluded that patients with stable CHF who do not have effort-induced arrhythmia or myocardial ischaemia can safely ascend to altitudes of 3000 m. The effect of increased altitude on exercise capacity becomes greater the more severe the exercise limitations at sea level [6].
We hypothesised that many CHF patients might not fly due to health concerns. We found no information regarding patients' experiences of air travel, whether they wanted to travel by air, what factors encourage or discourage them from air travel, and what problems they may have encountered during flight and at their destination. We conducted a survey in a cohort of patients with well-treated, stable CHF to find out about their experiences of air travel.
2. Methods
The Hull and East Riding Ethics Committee approved the study, and all patients provided informed consent prior to the survey. Patients were recruited from a community heart failure clinic serving the population of Hull and East Yorkshire. We contacted patients with a previous diagnosis of heart failure defined as the presence of appropriate symptoms, or a history of symptoms controlled by ongoing therapy, due to cardiac dysfunction in the absence of any more likely cause [7]. All patients had left ventricular systolic impairment on 2D echocardiography carried out by one of three trained operators.
An expert panel including a cardiologist (JGFC), an exercise scientist (LI), and a psychologist (SN) developed a series of survey questions designed to elicit CHF patients' experiences of air travel (Appendix 1). The survey questions, information sheets and consent forms were sent together with a return self-addressed envelope to 1293 patients.
2.1. Statistical analysis
PASW (SPSS version 17.0) was used to analyse the data. Continuous variables are presented as mean ± SD, and categorical data are presented as percentages. An arbitrary level of 5% statistical significance was used throughout (two-tailed). We conducted an age-adjusted logistic regression analysis to determine which element of the journey was more likely to predict symptoms of breathlessness in our patients.
3. Results
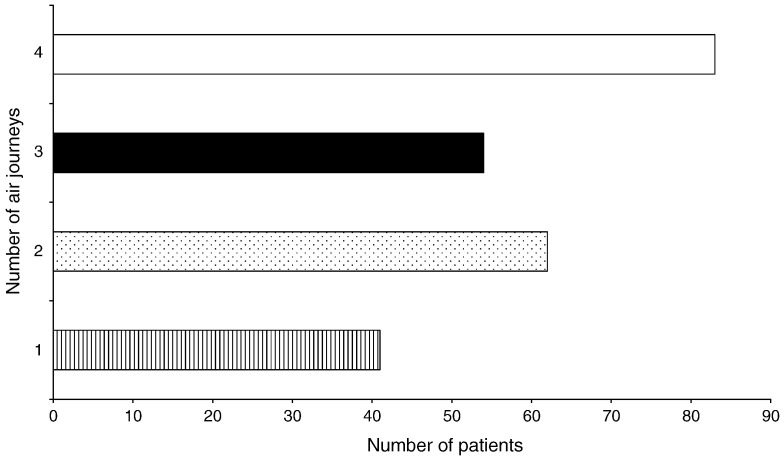
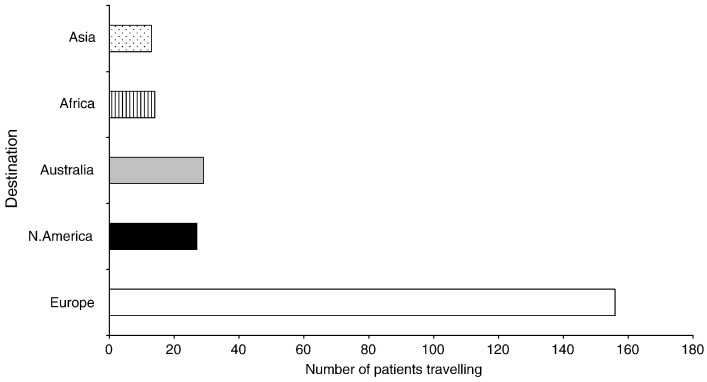
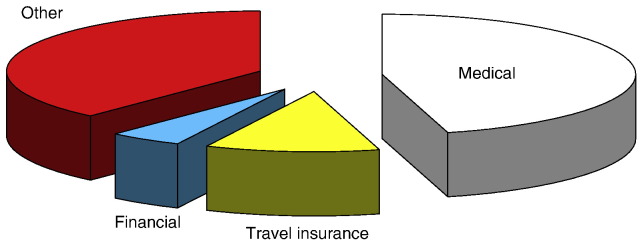
464 CHF patients (response rate = 39%) returned completed survey questionnaires. Table 1 shows baseline clinical characteristics of patients. 54% (252/464) of patients had travelled by air since their heart failure diagnosis. Of those who had flown, 21% had taken one flight, 25% 2 flights, 21% 3 flights, and 33% at least 4 flights (Fig. 1). 60% of patients who had flown had visited countries within Europe, 12% had flown to Australia, and other longer-haul destinations included North America (10%); Africa (6%); and Asia (6%) (Fig. 2). For patients who had not travelled by air, reasons for not travelling included medical concerns (33%), travel insurance problems (7%), and a proportion (27%) had no desire to travel abroad citing reasons such as “too old”, “too much hassle”, and “don't like flying” (Fig. 3).
Table 1.
Baseline clinical characteristics in patients with chronic heart failure (mean ± SD or %).
| Variables | CHF patients |
|---|---|
| Age (years) | 67.8 ± 9.5 |
| Males (%) | 82 |
| Body mass index (kg/m2) | 28 ± 6 |
| Left ventricular ejection fraction (%) | 37 ± 5 |
| Beta-blocker (%) | 65 |
| ACE-inhibitor (%) | 51 |
| Loop diuretic (%) | 50 |
| Aetiology of CHF | |
| Ischaemic heart disease (%) | 65 |
| Dilated cardiomyopathy (%) | 16 |
| Unknown (%) | 11 |
| Hypertension (%) | 5 |
| Valvular (%) | 3 |
Baseline data available in 174 of 464 patients (38% of total).
Fig. 1.
Number of air travel journeys since first diagnosis.
Fig. 2.
Furthest air travel destinations reported by CHF patients.
Fig. 3.
Reasons for not engaging in air travel.
20% of all patients (93/464) reported difficulties acquiring travel insurance due to extra premiums being required. In some cases, insurance companies refused to insure patients due to the nature of their condition. 15% of patients who did fly did not tell their insurer about their cardiac condition, and 11% of patients travelled without any insurance.
3.1. Health problems whilst travelling
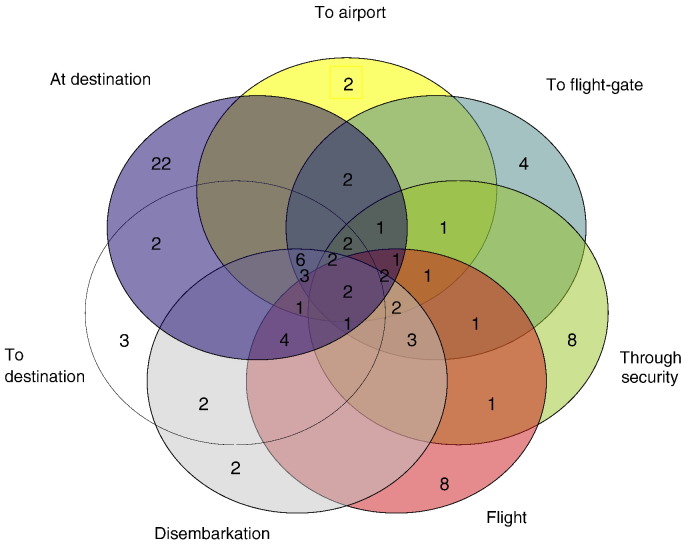
65% (163/252) of patients who flew experienced no health-related problems. 35% (89/252) of patients who flew experienced health-related problems. Fig. 4 shows the location of the problems experienced by the patients. 18% (46/252) experienced a problem at one location; 6% (16/252) experienced problems at two locations; 5% (13/252) experienced problems at three locations; 5% (12/252) experienced problems at more than three locations.
Fig. 4.
Venn diagram showing the location of health-related problems experienced by 89 patients with CHF during air travel.
Of the 89 patients who flew and experienced health problems, 9% (8/89) of patients reported problems going through security at the airport due to pacemaker/ICD problem and breathlessness. During the flight, 9% (8/89) of patients experienced breathlessness, dizziness, swollen ankles, headache, and chest pain. 3 of 8 patients used in-flight oxygen due to breathlessness. At the final destination, 25% (22/89) of patients complained of health-related cardiovascular problems including fatigue, breathlessness, laboured walking, swollen ankles, palpitations, angina, or their defibrillator firing (2 of 22 patients). Following an age-adjusted logistic regression analysis, the final destination was a better predictor of self-reported symptoms of breathlessness than other travel points (i.e. to security, to the flight gate, during air travel, during disembarkation) in our patients (P = 0.047; Hazard Ratio = 0.16; 95% confidence interval = 0.30–0.97).
3.2. Views on future air travel
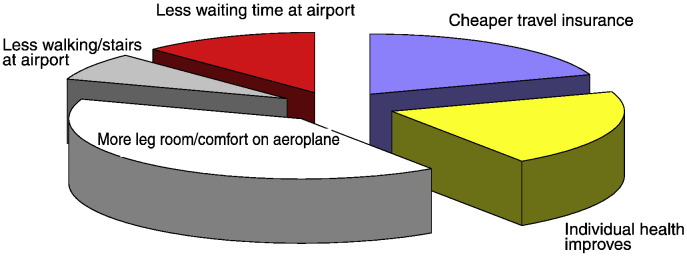
27% (125/464) of all patients that we surveyed would not fly in the future. 32% (148/464) stated that it was too difficult, 25% (116/464) of patients were worried about their health, 23% (107/464) had no wish to travel by air, and 11% (51/464) had no insurance cover. 38% (176/464) of all patients stated that they would consider flying again if there were more leg room/more comfort on the aeroplane during the flight, if their personal health improved (18%; 84/464), if they could find cheaper travel insurance (19%; 88/464), if there were less waiting at the airport (11%; 51/464), and if there was less walking/fewer stairs to negotiate at the airport (7%; 32/464) (Fig. 5).
Fig. 5.
Factors that would increase likelihood of future air travel in CHF patients.
46% (212/464) of all patients surveyed had not travelled by air since their diagnosis. 37% (79/212) would consider flying in the future if there were more leg room/comfort on the plane (38%; 30/79), if travel insurance were cheaper (22%; 17/79), if their health improved (18%; 14/79), and if there were less waiting time at the airport (10%; 8/79). 54% (252/464) of all patients surveyed had travelled since their diagnosis. 36% (91/252) would fly again if there were more leg room/comfort on the plane (37%; 34/91), if their health improved (20%; 18/91); if travel insurance were cheaper (19%; 17/91), and if there were less waiting time at the airport (13%; 12/91).
4. Discussion
Our study is the first to gauge heart failure patients' experiences of air travel. We have found that the majority of CHF patients who have flown since a diagnosis was made did not report any health-related problems. This finding is in agreement with the few published experimental studies which suggested that simulated flights did not produce complications in heart failure patients [5,6], and the recently published expert consensus statement [8]. Indeed, we found that there were more health-related problems at the final destination (25% of flying patients) than there were during flight itself (9% of flying patients).
We have found that problems of air travel are not confined to hypoxia. Although we have not specifically asked about the following, considerable exertion is required to walk to and from the plane at the airport, especially if suitcases have to be carried. Take-off and landing in particular may cause stress and anxiety. Implanted devices may cause concerns at security points. Drug therapy may cause a variety of problems including diuretics (toilet access), anti-coagulants (change in diet), ACE inhibitors and aldosterone antagonists (fluid balance due to sweating and diarrhoea). Travel advice needs to recognise these issues in CHF patients.
Recently, Smith and colleagues [8] produced an expert consensus statement on fitness to fly for passengers with cardiovascular disease: they concluded that in CHF, short-term (up to 1 h) exposure to a hypoxic environment produces no significant adverse effects (including patients with NYHA class III/IV symptoms) at rest. Longer-term hypoxic exposure (up to 7 h) can be tolerated in patients with mild-to-moderate stable CHF [8]. The authors also reported that the aircraft could be considered a “relatively alien, restrictive and hostile environment” (p. ii1). The patients that we surveyed would appear to agree. 37% of patients reported that they would only consider flying again if aircraft were more comfortable i.e. having more leg room.
In our study, 32% of patients reported that they would never fly again because it was too “difficult”. Up to 40% of the population have reported a fear of flying [9] which may have been heightened by an increased perception of terrorist activity since 2001 [10]. These factors amongst others may have been concerns for our patients. 11% of patients stated that they were more likely to fly again if there were less waiting time at the airport terminal. Patients are often advised to arrive at the airport in plenty of time to avoid rushing and to give the airline notice of special requirements such as wheelchair access or supplementary oxygen [8]. Longer waiting times can cause frustration and anger for some patients at the airport [11]. Strike and colleagues [12] reported that anger is one of the precursors that can provoke myocardial ischaemia in stressful situations. Further, 6% of patients stated that the long walks around the airport caused breathlessness and 7% would not fly again due to the amount of walking required. The amount of walking around the airport terminal, perhaps with heavy luggage, and in conjunction with staircase-use, may cause deterioration in the patients' condition [8]. Whilst many airports offer excellent transport services for “disabled” passengers — many patients may not be aware of these services or how they can book them prior to arrival at the airport.
We recommend that more experimental work is required to find out if flying is really safe in patients with CHF. Current findings would appear to suggest that short- to longer-term hypoxic exposure is safe in most stable heart failure patients.
4.1. Limitations
Demographic data including age, sex, BMI, LVEF, drug therapy, and aetiology of CHF was collected in 174 of 464 patients (38% of total) due to a printing error with an initial batch of questionnaires.
A limitation of the postal survey is selection bias, often only patients with strong positive or negative experiences will respond.
Within the survey we did not ascertain what family doctors had actually told patients regarding their suitability for air travel. Lainscak and colleagues [13] reported that recall of, and adherence to medical advice was disappointing in a large pan-European cross-sectional survey of 3261 CHF patients. Therefore, it is possible that some of our patients may have misinterpreted medical advice from their family doctor regarding their suitability to undertake air travel.
5. Conclusions
Ours is the first study to document CHF patients' experiences of air travel. Health-related problems were only experienced in a minority of patients, therefore, we can conclude that air travel is safe in stable, well managed CHF patients. Future air travel experiences could be improved if flying were more comfortable, travel insurance were cheaper, and there were less waiting time and less walking at airports.
Conflict of interest
None.
Financial disclosures
This study was supported by the British Heart Foundation.
Acknowledgement
The authors of this manuscript have certified that they comply with the Principles of Ethical Publishing in the International Journal of Cardiology[14].
Appendix 1
A pilot study examining risk associated with air travel in patients with impaired hearts.
We would like you to consider the following questions, which will ask you about your experiences of air travel. Please think about your experiences SINCE you were diagnosed with your heart condition. Thank you for your co-operation in this matter.
Please note the answers to the following questions will be kept anonymous and your name will not be used unless we receive your written consent.
-
1.
Would you describe the severity of your health-related problem as:
NOT APPLICABLE MILD MODERATE SEVERE
(Please circle)
-
2.
Have you travelled by air since you started taking water pills for your heart condition?
YES NO
(Please circle)
If “YES”, how many times have you travelled? (Please circle)-
a)1
-
b)2–3
-
c)4–6
-
d)7+
-
e)Where did you travel to?
If “NO”, please explain why (Please circle all that apply)-
f)Too difficult — go to Question 8
-
g)Worried about health — go to Question 8
-
h)Cannot get appropriate medical insurance cover — go to Question 8
-
i)Other reasons — please specify — go to Question 8…………………………………………………………………………
-
j)No desire to travel by air — please state why………………………………………………………………………………………
-
a)
-
3.
Medical insurance cover:
-
a)Did you tell your insurer you had a heart condition?YES NO (Please circle)
-
b)Did you have trouble getting medical insurance cover?YES NO (Please circle)If “YES” please specify why?………………………………………………………………………………………….
-
c)Who was your insurer?………………………………………………………………………………………
-
d)Did you decline to take out any medical insurance and travel without cover?YES NO (Please circle)
-
a)
-
4.When you flew, did you encounter any health-related problems:
-
a)Getting to the airport: YES NO (Please circle)
- If “YES”, please specify
- ………………………………………………………………………………………
-
b)Getting through security: YES NO (Please circle)If “YES”, please specify………………………………………………………………………………………
-
c)Getting to the flight gate: YES NO (Please circle)If “YES”, please specify………………………………………………………………………………
-
d)During the flight: YES NO (Please circle)If “YES”, please specify………………………………………………………………………………………
-
e)During disembarkation: YES NO (Please circle)If “YES”, please specify………………………………………………………………………………………
-
f)Travelling to your destination after disembarkation: YES NO (Please circle)If “YES”, please specify………………………………………………………………………………………
-
g)Whilst at your destination: YES NO (Please circle)If “YES”, please specify……………………………………………………………………………………….
-
a)
-
5.
Did you have to slow down or stop to catch your breath during any of the above activities in Question 4?
-
YES NO (Please circle)
If so, which ones?
………………………………………………………………………………………
-
6.
Did you have to seek medical help at any time during your travel?
-
YES NO (Please circle)
If “YES”, please specify
……………………………………………………………………………………
-
7.
Did you have problems taking your medicines or with side effects whilst away?
-
YES NO (Please circle)
If “YES”, please specify
………………………………………………………………………………………
-
8.
Would you consider travelling by air in the future?
-
YES NO (Please circle)
If “YES” please specify what would make the flying process easier and more enjoyable?
………………………………………………………………………………………
If “NO”, please explain why by circling the appropriate response-
a)Too difficult
-
b)Worried about health
-
c)Cannot get appropriate medical insurance cover
-
d)Other — please specify………………………………………………………………………………………
-
e)No wish to travel by air — please state why
…………………………………………………………………………………………..
-
a)
Date……………………………………………………………………………………...
Hospital Number………………………………………………………………………...
THANK YOU FOR YOUR PARTICIPATION IN THIS QUESTIONNAIRE
References
- 1.Lee A.P., Yamamoto L.G., Relles N.L. Commercial airline travel decreases oxygen saturation in children. Pediatr Emerg Care. 2002;18:78–80. doi: 10.1097/00006565-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Gong H., Jr. Exposure to moderate altitude and cardiorespiratory diseases. Cardiologia. 1995;40:477–488. [PubMed] [Google Scholar]
- 3.Lenfant C., Sullivan K. Adaptation to high altitude. N Engl J Med. 1971;284:1298–1309. doi: 10.1056/NEJM197106102842305. [DOI] [PubMed] [Google Scholar]
- 4.Boussuges A., Molenat F., Burnet H. Operation Everest III (Comex '97): modifications of cardiac function secondary to altitude-induced hypoxia. An echocardiographic and Doppler study. Am J Respir Crit Care Med. 2000;161:264–270. doi: 10.1164/ajrccm.161.1.9902096. [DOI] [PubMed] [Google Scholar]
- 5.Hobkirk J., Damy T., Bennett A. Heart Failure. 2009. Effects of reduced inspired oxygen concentration in patients with chronic heart failure. Nice, France. Proceedings of the European Society of Cardiology. [DOI] [PubMed] [Google Scholar]
- 6.Agostoni P., Cattadori G., Guazzi M. Effects of simulated altitude-induced hypoxia on exercise capacity in patients with chronic heart failure. Am J Med. 2000;109:450–455. doi: 10.1016/s0002-9343(00)00532-5. [DOI] [PubMed] [Google Scholar]
- 7.Remme W.J., Swedberg K. Comprehensive guidelines for the diagnosis and treatment of chronic heart failure. Task force for the diagnosis and treatment of chronic heart failure of the European Society of Cardiology. Eur J Heart Fail. 2002;4:11–22. doi: 10.1016/s1388-9842(01)00231-8. [DOI] [PubMed] [Google Scholar]
- 8.Smith D, Toff W, Joy M, et al. Fitness to fly for passengers with cardiovascular disease. Heart;96 Suppl 2:ii1-16. [DOI] [PubMed]
- 9.Dowdall N. Customer health: a new role for occupational physicians. Occup Med (Lond) 2003;53:19–23. doi: 10.1093/occmed/kqg023. [DOI] [PubMed] [Google Scholar]
- 10.Ito H., Lee D. Assessing the effect of September 11th terrorist attacks on US airline demand. J Econ Bus. 2005;57:75–95. doi: 10.1016/j.jeconbus.2004.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Folkes V., Kaletsky S., Graham J. A field study of causal inferences and consumer reaction: the view from the airport. J Consum Res. 1987;13:534–539. [Google Scholar]
- 12.Strike P.C., Steptoe A. Systematic review of mental stress-induced myocardial ischaemia. Eur Heart J. 2003;24:690–703. doi: 10.1016/s0195-668x(02)00615-2. [DOI] [PubMed] [Google Scholar]
- 13.Lainscak M., Cleland J.G., Lenzen M.J. Recall of lifestyle advice in patients recently hospitalised with heart failure: a EuroHeart Failure Survey analysis. Eur J Heart Fail. 2007;9:1095–1103. doi: 10.1016/j.ejheart.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 14.Shewan L.G., Coats A.J. Ethics in the authorship and publishing of scientific articles. Int J Cardiol. 2010;144:1–2. [Google Scholar]