Abstract
A 49-year-old woman presented with visual loss in the right from optic nerve metastatic disease and asymptomatic choroidal lesion at the inferior arcade. Throughout 22 months of follow-up, she developed a total of five different sequential choroidal metastases to the left eye that were non-responsive to chemotherapy but showed prompt tumour regression by fundus examination and fluorescein angiography within 2 weeks after a single intravitreal bevacizumab. The control of the lesion with a single intravitreal injection of bevacizumab reflects the superior choroidal bioavailability of the drug. The persistence of subretinal fluid at the site of prior metastases may be thought to be one sign of persistence of malignant cells, but in the current case and in the literature, it seems a reflection of a diseased retinal pigment epithelium with probable damage from the tumour invasion.
Background
Intravitreal bevacizumab was effective in resolution of metastatic lesions to the choroid in few reported cases that received concomitantly systemic chemotherapies. We present a case that failed chemotherapy and had five consecutive and different foci of choroidal metastases all responding to intravitreal bevacizumab, hence establishing the therapeutic efficacy of this treatment in metastatic choroidal disease.
Case presentation
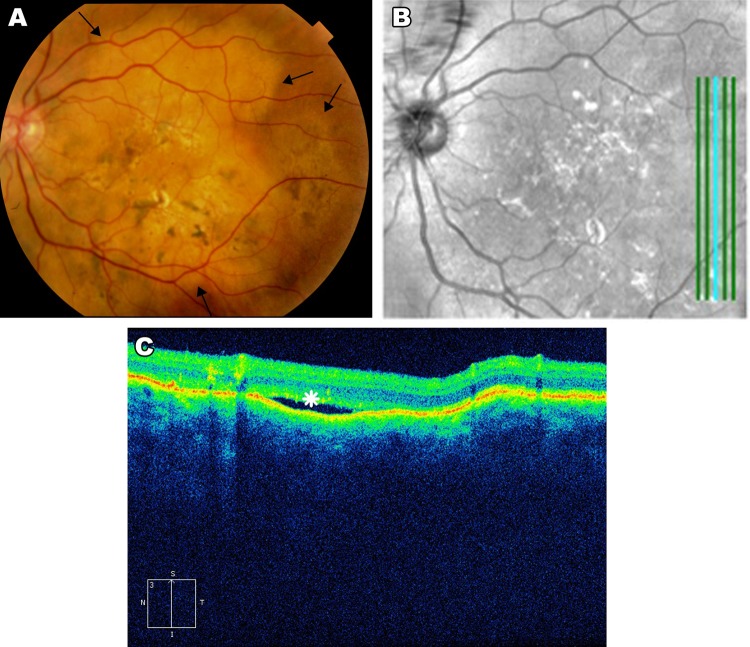
In May 2010, this 49-year-old lady presented with decreased visual acuity in the right eye. She had history of breast cancer with multiple metastases to brain (including right optic nerve), chest, bone and skin from moderately differentiated infiltrating ductal carcinoma. Immunohistochemical stains were positive for oestrogen and progesterone receptors and negative for human epidermal growth factor receptor 2. Following mastectomy with lymph node dissection she also received multiple cycles of radiotherapy and chemotherapy with cisplatin, capecitabine, gemcitabine, paclitaxel and tamoxifen. She had a best corrected visual acuity (BCVA) of 6/60 in the right eye and 6/6 in the left eye. Positive examination disclosed optic nerve atrophy and severe red desaturation in the right eye. An elevated yellowish 4 disk diameter juxtafoveal choroidal lesion extended to the inferior arcade of the left eye (figure 1A) with pinpoint fluorescence and profuse dye leakage on fluorescein angiography (figure 1B). A clinical diagnosis of choroidal metastasis was made. Because the patient’s diffuse metastases failed to respond to chemotherapy, she was offered radiotherapy or intravitreal 2.5 mg bevacizumab injections (IVB) (Avastin; Genentech, San Francisco, California, USA).
Figure 1.
(A) An asymptomatic dome-shaped yellowish 4 disk diameter inferotemporal juxtafoveal choroidal lesion reaching the inferior arcade with best corrected visual acuity of 6/6. (B) Late-phase frame during fluorescein angiography showing multiple pinpoint foci of hyperfluorescence.
Treatment
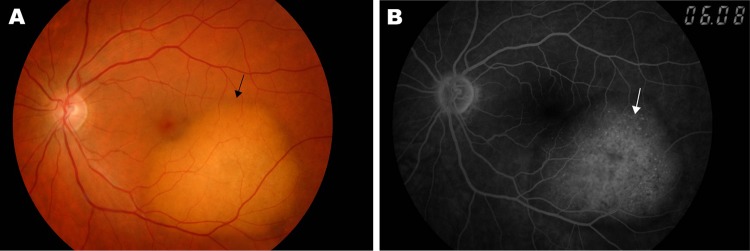
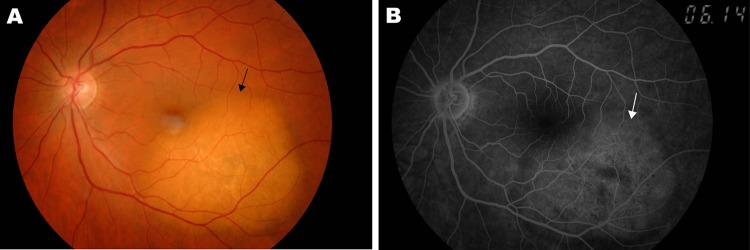
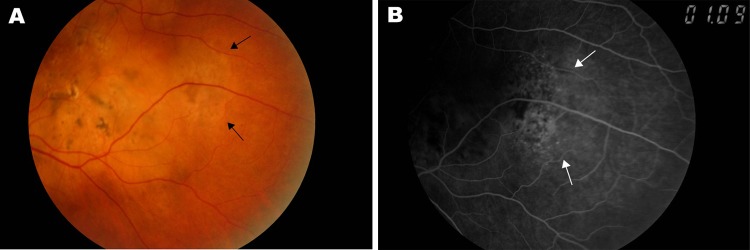
She underwent IVB after a signed informed consent to the off-label use of the drug. Two weeks later, regression of the choroidal mass was evident by funduscopy (figure 2A) and fluorescein angiography (figure 2B) with unchanged BCVA of 6/6. Subsequently, treatment of the right eye metastatic optic nerve disease with systemic bevacizumab failed to halt vision loss to light perception in the right eye. The patient was followed monthly. Four months after the first injection, she complained of sudden central persistent flashes of light in the left eye. She was given three IVB 4, 6 and 7 months from presentation) for suspicion of subclinical metastasis to the choroid despite a negative investigation. Following treatment these symptoms resolved. Ten months after first injection, she had decreased vision and metamorphopsia in the left eye. BCVA had dropped to 6/12 from a new elevated yellowish choroidal lesion at the level of the superior arcade. Two weeks following last IVB, the tumour regressed, BCVA improved to 6/7.5 and metamorphopsia disappeared. Thirteen months after the first injection, visual symptoms appeared again from a new third elevated choroidal yellowish lesion at the temporal midperiphery. The lesion regressed 2 weeks after IVB with resolution of symptoms. Sixteen months after the first injection, BCVA dropped to 6/12 with a large yellowish new lesion involving the macula. She again responded to IVB. Nineteen months after the first injection and with increasing widespread metastases resistant to continued chemotherapy, BCVA was unchanged (6/12) with retinal thickening temporal to the fovea (figure 3A) that leaked on fluorescein angiography (figure 3B). She therefore received IVB and subsequently there was angiographic regression 6 weeks later of the fifth metastatic lesion (figure 4A). Optical coherence tomography (OCT) (figure 4B,C) through the temporal lesion showed persistent subretinal fluid which did not resolve following IVB. Subretinal fluid persisted by OCT 3 weeks after the last (ninth) IVB 22 months after the first injection.
Figure 2.
(A) The choroidal lesion has flattened 2 weeks after the first intravitreal injection of bevacizumab with best corrected visual acuity of 6/6. (B) Absence of dye leakage in late-phase of fluorescein angiography.
Figure 3.
(A) Nineteen months after the first injection, retina was thickened temporally (arrows) away from the previous lesions. (B) Pinpoint hyperfluorescence in late phases confirms the metastatic nature of the new choroidal lesion.
Figure 4.
(A) 22 months after initial injection, the temporal choroidal mass has regressed. (B) A vertical scan of the temporal lesion was done by OCT (after bevacizumab injection) and results are shown below. (C) Persistence of subretinal fluid despite two repeated injections of bevacizumab with resolution of the temporal metastatic lesion.
Discussion
Therapeutic modalities for choroidal metastasis include enucleation, external beam radiotherapy, laser photocoagulation, brachytherapy, chemotherapy and tamoxifen.1–4 Bevacizumab is a full-length recombinant humanised antibody against all isoforms of vascular endothelial growth factor A (VEGF-A), and has been approved by the FDA for intravenous use in metastatic carcinoma of the colon or rectum and for non-small cell lung cancer. Recently, emerging case reports have shown beneficial effects of intravitreal bevacizumab in the control of choroidal metastasis from colon (two cases),5 6 lung (two cases)7 8 and breast (two cases).9 10 The rationale behind bevacizumab use is its antiangiogenic effect by inhibition of tumour-induced angiogenesis thereby preventing the growth of solid tumours. This treatment modality seems attractive because of vision preservation (unlike radiotherapy), local bioavailability of the drug (unlike systemic bevacizumab) and good safety profile (unlike systemic bevacizumab). All reports to date illustrate either partial regression within few weeks after the first IVB5 7 or complete resolution with longer follow-up and with additional injections8–10 of the choroidal mass by fluorescein angiography or OCT. Most improvement occurred within few weeks without local recurrence was noted. Only one report6 showed no response to the drug in one eye with a large choroidal tumefaction while the fellow had marked regression of two smaller metastatic choroidal lesions.
In this case report, throughout 22 months of follow-up, the patient developed five different sequential choroidal metastases that were non-responsive to chemotherapy but showed prompt tumour regression by fundus exam and fluorescein angiography within 2 weeks after a single IVB. The control of the lesion with a single injection reflects the superior choroidal bioavailability of the drug.11 The persistence of subretinal fluid may be one sign of persistence of malignant cells, but in the current case and in the literature,7 it seems a reflection of a diseased retinal pigment epithelium. The indications for intravitreal injection have included asymptomatic choroidal masses, ocular symptoms (metamorphopsia), subretinal fluid by OCT and leakage by fluorescein angiography. To the best of our knowledge, this is the first report that shows prompt resolution (unrelated to failed chemotherapy) after IVB of five new choroidal foci of metastasis without any signs of tachyphylaxis. We conclude that a single IVB is sufficient for control of certain choroidal metastases and that monthly follow-up is necessary to detect new foci in such subjects.
Learning points.
Intravitreal bevacizumab can be the first line of therapy in metastatic choroidal disease causing complete tumour regression with preservation of vision.
A single intravitreal bevacizumab injection is often sufficient to control metastatic disease.
Monthly follow-up is necessary to detect new metastatic foci in the choroid in subjects with metastatic disease not responding to chemotherapy.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Giuliari GP, Sadaka A. Uveal metastatic disease: current and new treatment options (review). Oncol Rep 2012;27:603–7. [DOI] [PubMed] [Google Scholar]
- 2.Kanthan GL, Jayamohan J, Yip D, et al. Management of metastatic carcinoma of the uveal tract: an evidence-based analysis. Clin Experiment Ophthalmol 2007;35:553–65. [DOI] [PubMed] [Google Scholar]
- 3.Chen CJ, McCoy AN, Brahmer J, et al. Emerging treatments for choroidal metastases. Surv Ophthalmol 2011;56:511–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.George B, Wirostko WJ, Connor TB, et al. Complete and durable response of choroid metastasis from non-small cell lung cancer with systemic bevacizumab and chemotherapy. J Thorac Oncol 2009;4:661–2. [DOI] [PubMed] [Google Scholar]
- 5.Kuo IC, Haller JA, Maffrand R, et al. Regression of a subfoveal choroidal metastasis of colorectal carcinoma after intravitreous bevacizumab treatment. Arch Ophthalmol 2008;126:1311–3. [DOI] [PubMed] [Google Scholar]
- 6.Lin CJ, Li KH, Hwang JF, et al. The effect of intravitreal bevacizumab treatment on choroidal metastasis of colon adenocarcinoma–case report. Eye (Lond) 2010;24:1102–3. [DOI] [PubMed] [Google Scholar]
- 7.Amselem L, Cervera E, Díaz-Llopis M, et al. Intravitreal bevacizumab (Avastin) for choroidal metastasis secondary to breast carcinoma: short-term follow-up. Eye (Lond) 2007;21:566–7. [DOI] [PubMed] [Google Scholar]
- 8.D’Antonio C, Viterbo A, Romiti A, et al. Complete regression of a non-small cell lung cancer choroidal metastasis with intravitreal bevacizumab. J Thorac Oncol 2012;7:468–9. [DOI] [PubMed] [Google Scholar]
- 9.Kim SW, Kim MJ, Huh K, et al. Complete regression of choroidal metastasis secondary to non-small-cell lung cancer with intravitreal bevacizumab and oral erlotinib combination therapy. Ophthalmologica 2009;223:411–3. [DOI] [PubMed] [Google Scholar]
- 10.Yao HY, Horng CT, Chen JT, et al. Regression of choroidal metastasis secondary to breast carcinoma with adjuvant intravitreal injection of bevacizumab. Acta Ophthalmologica 2010;58:131–9. [DOI] [PubMed] [Google Scholar]
- 11.Talty P, Hickey-Dwyer M, Wong SJ, et al. Intraocular bevacizumab levels 24 hours after intravitreal injection in a normal eye. Retinal Cases Brief Reports 2012;6:65–8. [DOI] [PubMed] [Google Scholar]