Abstract
The functionality and rate of implementation of Anesthesia Information Management Systems (AIMS) has markedly risen over the past decade. These systems have now become much more than the generic automated record keepers, originally proposed and developed in the 1980s. AIMS have now become complex integrated systems, which have been shown to improve patient care and, in some cases, the financial performance of a department. Although the underlying technology has improved greatly over the past 5 years, the process of selecting and completing an AIMS installation still presents a number of challenges, and must be approached carefully in order to maximize the benefits provided by these systems.
Keywords: anesthesia, information systems, AIMS, informatics, software
INTRODUCTION
Anesthesia Information Management Systems (AIMS) allow the automatic and reliable collection, storage, and presentation of patient data during the perioperative period. They are specialized forms of electronic health record (EHR) systems that in addition to providing basic record-keeping functions, typically provide end users with ready access to summary data that can be used to facilitate quality assurance and research functions. A typical AIMS installation will be a hardware/software solution that interfaces with the intraoperative patient monitors. Increasingly these systems also have the ability to read and write data from the main hospital clinical data repositories. While the core functionality of an AIMS centers on the automatic and reliable capture of intraoperative patient data, most AIMS today also include modules for storing pre- and postoperative patient information. The information captured by an AIMS is usually stored in a relational database that supports multi-user access along with archival and backup capabilities. While these databases are most often accessed using a vendor’s commercial front-end application, they may often also be accessed directly using standard database tools.
The financial barriers associated with implementation of AIMS have been the primary obstacles to their widespread adoption. As a result only an estimated 5% of US operating rooms in 2006 had an AIMS installation [1]. However, a recent survey showed that adoption of these systems has accelerated (44% of academic centers are now planning to implement or have implemented an AIMS). This rapid adoption has been driven by (1) a desire to improve routine clinical documentation and (2) a need to mitigate increasing reporting requirements imposed by various regulatory bodies [2]. Table 1 summarizes the key areas where AIMS have been noted to provide positive benefits to, patients, anesthesia departments, and hospital systems.
Table 1.
Key areas impacted by anesthesia information management systems [3]
| Impact on patients |
|
| Impact on departmental management |
|
| Impact on the practice of anesthesia |
|
A summary of the specific benefits afforded by an AIMS installation is shown in Table 2. These benefits will depend on a number of factors including, but not limited to the departmental work flow, the system purchased, and the overall implementation scheme. Institutions which simply replace a paper record keeping system with an electronic version almost never obtain the full benefit of these systems because they do not modify their internal processes to maximize the potential benefits. One example of this occurred at an institution which, after installation of their AIMS, continued to send paper copies of incomplete records to staff physicians through the mail in an attempt to obtain correction of documentation errors. At that hospital, the rate of unbillable cases was unchanged after the AIMS installation, until the department implemented a set of electronic tools linked to the AIMS which were able to facilitate error correction electronically [4].
Table 2.
Summary of AIMS benefits in the peer-reviewed literature
| Clinical decision support and provider education |
| Provision of Clinical Decision Support [5, 6] |
| Facilitation of Provider Education [7] |
| Billing improvements and cost control |
| Reducing anesthesia drug and supply costs [8] |
| Facilitating capture of anesthesia-related billing charges [5, 9] |
| Improving hospital reimbursement for anesthesia services [10, 11] |
| Clinical research and enhanced data quality |
| Facilitation of clinical research [12, 13] |
| Enhanced quality of intraoperative record keeping [14, 15] |
| Patient safety and quality assurance |
| Improved patient safety and quality of care [16] |
| Support of clinical quality improvement programs [17] |
| Enhancement of clinical risk management [18] |
| Detection of controlled substance diversion [19] |
THE BUSINESS CASE/RATIONALE FOR PURCHASING AN AIMS
Anesthesia fundamentally relies on the timely collection and documentation of accurate information because this data becomes the basis for decision making at the point-of-care. As the amount of data available continues to grow and increase in complexity, many departments choose to install electronic systems to facilitate both the capture and interpretation of this information.
In addition to helping end users with the particular task of generating an accurate anesthesia record, in a variety of settings AIMS have been shown to improve patient safety and the quality of care delivered by facilitating appropriate clinical care [16, 20]. Many AIMS can now generate point-of-care alerts for important clinical events, such as drug–drug interactions or patient allergies. In addition to end-user alerts, AIMS provide accurate documentation which can be used for retrospective reviews and down-stream detailed analyses. Because of these functionalities, the Anesthesia Patient Safety Foundation has endorsed the use of these systems [21].
While some departments/hospitals may choose to install an AIMS for the safety advantages and clinical benefits they provide, others may choose an AIMS because of the potential to improve a department’s economic performance (in spite of their relatively large upfront capital costs ($4,000–$10,000 per operating room plus an additional $14,000–$45,000 for AIMS server installation). The ultimate return on investment (ROI) depends on the individual institution’s specific financial, billing, and management practices [21]. A recent literature review noted four areas by which an AIMS is able to contribute a positive net return on investment. These areas include (1) more efficient staff scheduling and decreased staff costs, (2) decreased anesthesia drug costs, (3) better charge/billing capture, and (4) increased hospital reimbursement from improved hospital coding [5, 22, 23]. For example, one institution successfully increased their billing rate for epidural catheters, central lines, and arterial catheters by customizing its AIMS such that individual clinicians were prompted with reminders to document invasive procedures when triggering events were detected by the system [4]. Others departments have successfully leveraged their AIMS to reduce time to receive payment for services, thus improving their revenue cycles and accounts payable [9].
Finally, a number of institutions are using AIMS to automatically generate both individual and departmental level quality reports (using metrics such as maintenance of normothermia and administration of antibiotics prior to surgical incision). Without electronic systems, a manual chart review, which is both time consuming and expensive, is required to successfully report on these types of quality measures. Additionally, through the provision of point-of-care clinical decision support, AIMS also offer a means to help providers improve on quality metrics, rather than simply report on them.
FUNCTIONALITY
Recording intraoperative data remains the core strength of most AIMS. Many systems, however, also offer advanced management tools and reporting functionality, preoperative evaluation modules, and the ability to provide customized clinical decision support.
The preoperative modules contained in AIMS may simply be a place to input patient demographics (name, gender, age, ASA physical status) and insert a free-text note. Other systems can provide the end-user with a robust electronic history-taking questionnaire and even suggest preoperative laboratory tests based on customizable algorithms that take into account any patient comorbidities as well as the specific procedure [23]. Preoperative modules that store patient data as structured data elements (rather than free text comments) may provide patient risk stratification information on-the-fly by using algorithms such as the modified Lee-Goldman index [24]. Most AIMS afford a simple method by which end-users can access a completed pre-operative evaluation, either by sending data to a hospital EHR system or providing an information summary. One major advantage of preoperative modules is that they reduce redundant data entry by carrying information (such as a patient’s age and allergies) across into the intraoperative chart. Prior to AIMS selection, one should decide which components are important for the needs of the department, as well as how the system will impact existing work flows. For example, in order to obtain the maximum benefit of a preoperative module, it may be necessary to install the AIMS in the preoperative anesthesia clinic or induction rooms.
Intraoperative charting has been the basis and continues to serve as the core function of any AIMS installation. This functionality encompasses two primary activities: the manual entry of case events (e.g., case times, drug administrations, and airway management events) and the automatic transcription of data from patient monitors (e.g., vital signs and ventilator data) into the accumulating electronic record. The AIMS end-user interface (Figure 1) must facilitate continuous access to the accumulating anesthesia record, since the data is used in real time during a case [21]. The user interface should also facilitate the work flow of end users such that manually recorded events may be easily and rapidly entered. Users should be able to complete basic tasks—such as initiating a case, or documenting an event—with minimal training. Ideally, the AIMS interface should allow users to enter data in ways that complement their existing work flow and at their own pace, rather than forcing users to modify their processes to fit within the requirements of a specific electronic system. Finally, in order to be effective the intraoperative interface should organize and highlight critical pieces of data as they become available, in order to facilitate situational awareness. This allows end users to quickly identify key pieces of information—often by displaying a data element in a different color or a larger font [25]. For example, many AIMS will display an on-screen notification when an antibiotic is due to be re-administered.
Fig. 1.
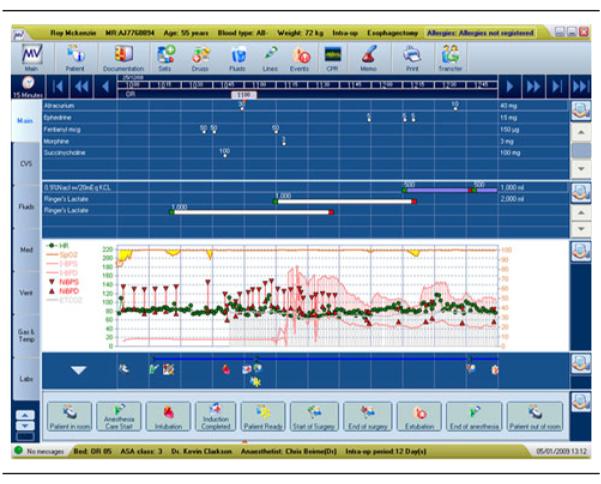
Intraoperative AIM interface (courtesy iMDSoft).
Clinical decision support is a fast-growing area within AIMS product development. The goal of this advanced feature is to allow clinicians to more effectively accomplish a particular task, by providing relevant just-in-time information at the point-of-care. Although clinical decision support is not universally available in all AIMS, this type of functionality can enable both reductions in the total cost and improvements in the quality of care (Table 3). The most rudimentary clinical decision support tools—such as algorithms that provide drug-dosing assistance based on a patient’s weight or baseline renal function—offer passive guidance. More advanced tools have been designed to actively manage clinician’s behavior by using on-screen, paging, or e-mail notifications about changes in a patient’s clinical condition. It is important to decide which features are indispensable for any particular AIMS installation prior to generating a request for proposal, because not every vendor supports all of these functions.
Table 3.
Categories of AIMS-based clinical decision support
| Quality assurance |
| Maintenance of normothermia notifications |
| Presurgical antibiotic management notifications |
| Medication support |
| Drug-drug interaction checking |
| Drug-dose calculations |
| Drug re-dosing reminders |
| Drug-allergy checking |
| Regulatory and compliance support |
| Concurrency checking |
| Ensuring electronic records contain elements required for billing |
| Attending physician attestation statements |
| Case times (Start of Anesthesia Care, End of Anesthesia Care) |
| Case type (General/MAC/Regional) |
| Patient details (ASA physical status) |
| Support around critical events |
| Algorithm display and guidance (Malignant Hyperthermia, ACLS, ASA Difficult Airway Algorithm) |
| Critical event detection (chaotic ECG + no pulse-ox wave form → consider ventricular fibrillation) |
ACLS advanced cardiac life support, ASA American Society of Anesthesiologists, ECG electrocardiogram, MAC monitored anesthesia care.
There are several ways that AIMS can support quality improvement and quality assurance initiatives. First, AIMS can provide insight into deficiencies in processes of care by facilitating the objective and rapid collection of complete patient data sets. The uniform and consistent collection of data elements by an AIMS can allow one to gain tremendous insight into departmental and individual practices. Once deficiencies have been identified, an AIMS can facilitate the planning and execution of process improvement efforts by supporting process changes as well as the collection of additional data. In addition, an AIMS can allow the rapid identification of practice trends through the provision of large and robust electronic data sets, which can be quickly scanned—an effort that often is cost-prohibitive and time consuming when executed with paper patient records. Second, most AIMS can be modified to provide end-users with electronic tools to improve their levels of performance, once areas for improvement have been successfully identified (Table 3 shows a list of decision support features made available within most AIMS). These opportunities may include reductions in missed revenue opportunities or operational improvements. Finally, most AIMS provide their own or can link-out to third party quality-assurance tracking systems [26].
SELECTING AN AIMS
The decision to install an AIMS is one of the most important that a department or hospital will make because it will impact nearly every part of a department (billing processes, clinical operations, physician credentialing, quality assurance, contracting). Additionally, the installation of an AIMS has the potential to impact a number of areas outside of an anesthesia department such as clinical engineering, medical records, safety and compliance, information technology, admitting, and security.
When considering the purchase of an AIMS, the first step should be a determination of the overall project scope. This should occur in concert with an effort to identify the specific needs and desires of the department as it relates to its information systems. This process will typically be best facilitated by selected members of the departmental leadership team along with appropriate representatives from the hospital information systems group. The selection of a specific AIMS should only be attempted after the key considerations listed in Table 4 have been addressed [27].
Table 4.
Considerations when selecting an AIMS
| What activities will the AIMS handle? (e.g., preoperative, intraoperative, postoperative activities) |
| How will the system integrate with the existing departmental/hospital work flows? |
| What will be the scope of the AIMS and the overall project? |
| What sites will the AIMS support? (e.g., operating room, labor and delivery, off-site locations, ambulatory surgical area) |
| What physical infrastructure will be required to support system deployment? (e.g., hardware for use in the operating rooms, dedicated or shared network connections, secure location for the primary and backup servers) |
| Who will provide system support personnel? (e.g., hospital or anesthesia department) Will the support be during business hours only or 24/7? |
| Will the AIMS stand alone or will it interface with existing clinical systems? |
| How will the installation, system customization, initial testing, and deployment occur? |
| How will the system be deployed and maintained? (e.g., phased roll-out or all-at-once implementation) |
| Who will provide the initial and ongoing training for end-users? |
| Who will provide the ongoing system maintenance, development, and upgrades? |
| What kind of backup systems will be included? |
| What level of redundancy is built into the AIMS deployment? |
CHOOSING A VENDOR
Once the overall functionality and scope of the project have been chosen, an RFP (request for proposal) should be created. The goal of the RFP is to carefully describe the specific requirements of the proposed installation, the areas impacted, and the exact clinical activities which are to be supported [21]. In order to ensure competitive bids are received and the best vendor/product selected, the RFP should be sent to a wide range of vendors once generated. A list of current AIMS and their respective vendors is shown in Table 5.
Table 5.
List of AIMS which are commercially available
| AIMS vendor | Web site | Contact information | Date founded System name |
|---|---|---|---|
| Acuitec | http://www.acuitec.com | Acuitec, 2233 Cahaba Valley 2007 Drive Birmingham, Al 35242 (800) 761-0486 |
VPIMS and Vigilance |
| Cerner | http://www.cerner.com | Cerner Corporation 2800 1979 Rockcreek Parkway Kansas City, MO 64117 (816) 201-1024 |
SurgiNet |
| DocuSys | http://www.docusys.net | Implementations/Client 1981 Services Office: 739 North University Blvd., Suite 104 Mobile, AL 36608 |
DocuSys AIMS |
| Dräger | http://www.nad.com | Draeger Medical, Inc 3135 1889 Quarry Road Telford, PA 18969 800-437-2437 |
Innovian Anesthesia |
| eko systems, inc. | http://www.ekosystems.com | 1902 Campus Commons 2000 Drive 6th Floor, Suite 650 Reston, VA 20191 (703) 657-8500 |
Frontiers |
| GE Healthcare | http://www.gehealthcare.com | GE Healthcare Integrated IT 1996 Solutions 540 West Northwest Highway Barrington, IL 60010 USA |
Centricity Anesthesia |
| iMDsoft | http://www.imd-soft.com | 300 First Avenue Needham, 1996 MA 02494 |
MetaVision |
| Philips Medical Systems |
http://www.healthcare.philips.com | 800-225-0230 1896 | Compu Record |
| Picis | http://www.picis.com | Headquarters 100 1994 Quannapowitt Parkway, Suite 405 Wakefield, MA 01880 781 557 3000 |
Anesthesia Manager |
The RFP response from each vendor should at a minimum include an itemized implementation costs for software licenses and hardware, details about the included warranty, options for support and training, as well as service agreement pricing. Each vendor should detail their systems ability to handle a catastrophic event (e.g., a server failure, power outage, or network interruption) and the systems for redundancy should be outlined. The RFP should also specify what kind of network connectivity will be required, as well list the specific interfaces needed to connect to both existing equipment (i.e., intraoperative physiologic monitors, anesthesia machines) and hospital clinical information systems (i.e., laboratory, ADT, and billing systems). When going through the process of a product assessment, site visits or live demonstrations can be quite informative. The key points to evaluate during a live AIMS demonstration include the system stability, user interface, system responsiveness and security [21].
The vendor should clearly outline and itemize all of the specific costs associated with AIMS installation along with specific dates and clear terms of delivery during the contracting process.
The number of clinical and administrative workstations associated with a new installation will impact the overall cost of a new system. Individual workstations typically cost $3,000–$8,000 per anesthetizing location, and $1,500–$3,500 for each administrative site. The AIMS server itself and the hardware associated with its installation may cost 3–5 times as much as a clinical workstation. Ongoing maintenance fees and support costs which typically run around 20% of the AIMS purchase price should also be clearly outlined during the contracting process. The different features and various hardware solutions provided by specific vendors make all of these costs quite variable [21].
AIMS IMPLEMENTATION
Once an AIMS has been chosen, a detailed implementation scheme should be created that specifies the installation approach (phased or all-at-once) and timing for AIMS deployment. This implementation plan should also take into account changes in the administrative and clinical work flows that will be required to facilitate a successful AIMS installation. One must also carefully consider the requirement for additional support staff and the need for initial and ongoing end-user training. A motivated and committed clinical champion, who can facilitate the initial AIMS interface customization and who is familiar with the departmental/hospital work flows, should be identified. This individual is typically a clinician who has familiarity with both medical devices and information systems [28].
A well-thought out plan for the initial testing and deployment should be outlined and made widely available across the department. This is critically important to make sure that the individuals who will be impacted by the AIMS installation are aware of the upcoming changes—prior to system deployment. It is also important to consider areas outside of the anesthesia department that should be included in this effort—such as nursing, compliance, perioperative services, billing/coding, and medical records. Finally, system failures and unexpected problems should be anticipated and a detailed contingency plan should be developed and disseminated prior to AIMS installation.
AIMS ERGONOMICS
The overall usability and ergonomics of a particular installation will be greatly impacted by the physical setup and specific characteristics of the clinical workstations [29]. Most AIMS vendors recommend the mounting of touch screens either on the anesthesia machine or nearby as shown in Figure 2. An adjustable arm mounted on the side of an anesthesia machine can typically accommodate both the touch screen display and a full keyboard for data entry. The quality of data capture and ease of use is likely to be greatly impacted by the final physical setup.
Fig. 2.

An AIMS workstation (touch screen and full keyboard), shown mounted on an anesthesia machine (image courtesy W. Sandberg).
END-USER TRAINING
All end-users (clinical and non-clinical) will need to be trained on the system to maximize the benefits of an AIMS installation. While the details regarding specific task completion will vary from AIMS to AIMS, all modern systems utilize industry standard graphical user interfaces that should be familiar to most anesthesiologists. All clinical, administrative, and technical support staff should receive training on the AIMS. This is best accomplished by providing separate training sessions emphasizing the system functions unique to each user group. While the initial training may consist of classroom sessions, one-on-one tutorials, or self-paced tutorials, most vendors suggest having dedicated support staff available during the first few weeks of initial system deployment. The initial AIMS training should occur as close as possible to the AIMS go-live date. This will allow end users to practice and reinforce what they have learned [21].
DOCUMENTATION AND DATA DEFINITIONS
The data captured and stored within an AIMS is only as reliable and robust as what end-users put into the system. Clear and consistent definitions of specific data elements and events will facilitate uniform documentation. As with many clinical practices, these definitions often vary across and sometimes even within institutions. For example, there are many different definitions of the “induction of anesthesia” (e.g., administration of a hypnotic, provision of anxiolytics, or start of pre-oxygenation). Data uniformity is important because it facilitates billing, reporting, and increasingly, clinical decision support functions. Finally, the availability of timely information is a means through which many AIMS can provide real-time decision-support. This type of support can be negatively affected by delayed data entry [30].
ADVANTAGES AND LIMITATIONS
The major advantages and potential limitations of AIMS are summarized in Table 6.
Table 6.
Current features and limitations of modern day AIMS
| Features | Limitations |
|---|---|
| Facilitates real-time clinical decision support [4] |
No standards across AIMS vendors and limited system interoperability Mobility and accessibility somewhat limited (while AIMS workstations usually run on desktop computers, pre- and postoperative assessments are typically performed at the bedside) [33] Limited vertical integration (data does not easily transfer from one phase of care to the next) [33] Data collection may be prone to gaps during unrecognized system failures [34] |
| Accurate and automated intraoperative data collection can enhance anesthesia record quality [5] | |
| Increases time providers can provide direct patient care [31] | |
| Improved quality and accessibility of data for research |
Requires significant effort and time for initial implementation and end-user Installation costs and initial expenses may not recovered in small practices |
| Allows automated process monitoring and control [5] |
Limited compatibility and interoperability with other electronic systems Potential introduction of recording/monitoring artifacts into a permanent electronic record |
| Enhances efforts to improve patient safety and quality | |
| May increase revenue capture [32] |
While AIMS adoption has been relatively slow compared to other technologies, it is beginning to accelerate. This is in large part due to the fact that the potential of an AIMS to improve patient care has been less obvious compared to other available technologies, such as newer physiologic monitors or current-generation anesthesia machines [27]. As AIMS continue to demonstrate improved processes of care, billing efficiency, and quality assurance advantages, they will no longer remain in the hands of a few early adopters—but are likely to become an essential modality for providing the lowest-cost, highest-quality care across an anesthesia department [28].
SUMMARY
The recent increased AIMS functionality and increasing pressure to report data for external review, such as with pay-for-performance contracting, is driving the rapid adoption of AIMS.
A number of peer-reviewed studies have shown the ability of these systems to both improve operating room efficiency and increase the quality of care delivered. However, this has only been possible with careful planning. It is important to note that a successful AIMS implementation takes significant resources—often well beyond what will be specified in a vendor contract. A large part of these resources will include the time required for training, installation, and software customization [28]. In the future, it is likely that improved standardization, interoperability, and integration among vendors will allow further improvements in the modern day AIMS.
Acknowledgments
Financial support for the preparation of this manuscript was provided from a Research Fellowship Grant from the Foundation for Anesthesia Education and Research, 5T32GM007592 from the National Institute of Health, as well as by department funds of the Department of Anesthesia, Critical Care, and Pain Medicine, Massachusetts General Hospital. There are no conflicts of interest. Portions of the article were adapted from “Anesthesia Information Management Systems: A Guide to Their Successful Installation and Use” Anesthesiology News, September 2009.
REFERENCES
- 1.Epstein RH, Vigoda MM, Feinstein DM. Anesthesia information management systems: a survey of current implementation policies and practices. Anesth Analg. 2007;105(2):405–411. doi: 10.1213/01.ane.0000270214.58811.c4. [DOI] [PubMed] [Google Scholar]
- 2.Halbeis CB Egger, Epstein RH, Macario A, Pearl RG, Grunwald Z. Adoption of anesthesia information management systems by academic departments in the United States. Anesth Analg. 2008;107(4):1323–1329. doi: 10.1213/ane.0b013e31818322d2. [DOI] [PubMed] [Google Scholar]
- 3.Thys DM. The role of information systems in anesthesia. Anesth Patient Saf Found Newslett. 2001;16(2):3–5. [Google Scholar]
- 4.Spring SF, Sandberg WS, Anupama S, Walsh JL, Driscoll WD, Raines DE. Automated documentation error detection and notification improves anesthesia billing performance. Anesthesiology. 2007;106(1):157–163. doi: 10.1097/00000542-200701000-00025. [DOI] [PubMed] [Google Scholar]
- 5.Sandberg WS, Sandberg EH, Seim AR, et al. Real-time checking of electronic anesthesia records for documentation errors and automatically text messaging clinicians improves quality of documentation. Anesth Analg. 2008;106(1):192–201. doi: 10.1213/01.ane.0000289640.38523.bc. Table of contents. [DOI] [PubMed] [Google Scholar]
- 6.Merry AF, Webster CS, Mathew DJ. A new, safety-oriented, integrated drug administration and automated anesthesia record system. Anesth Analg. 2001;93(2):385–390. doi: 10.1097/00000539-200108000-00030. 383rd contents page. [DOI] [PubMed] [Google Scholar]
- 7.Edsall DW. Computerization of anesthesia information management–users’ perspective. J Clin Monit. 1991;7(4):351–358. doi: 10.1007/BF01619360. [DOI] [PubMed] [Google Scholar]
- 8.Gillerman RG, Browning RA. Drug use inefficiency: a hidden source of wasted health care dollars. Anesth Analg. 2000;91(4):921–924. doi: 10.1097/00000539-200010000-00028. [DOI] [PubMed] [Google Scholar]
- 9.Reich DL, Kahn RA, Wax D, Palvia T, Galati M, Krol M. Development of a module for point-of-care charge capture and submission using an anesthesia information management system. Anesthesiology. 2006;105(1):179–186. doi: 10.1097/00000542-200607000-00028. quiz 231-172. [DOI] [PubMed] [Google Scholar]
- 10.Meyer-Jark T, Reissmann H, Schuster M, et al. Realisation of material costs in anaesthesia. Alternatives to the reimbursement via diagnosis-related groups. Anaesthesist. 2007;56(4):353–362. 364–355. doi: 10.1007/s00101-007-1136-6. [DOI] [PubMed] [Google Scholar]
- 11.Martin J, Ederle D, Milewski P. CompuRecord—a perioperative information management-system for anesthesia. Anasthesiol Intensivmed Notfallmed Schmerzther. 2002;37(8):488–491. doi: 10.1055/s-2002-33172. [DOI] [PubMed] [Google Scholar]
- 12.Hollenberg JP, Pirraglia PA, Williams-Russo P, et al. Computerized data collection in the operating room during coronary artery bypass surgery: a comparison to the hand-written anesthesia record. J Cardiothorac Vasc Anesth. 1997;11(5):545–551. doi: 10.1016/s1053-0770(97)90001-x. [DOI] [PubMed] [Google Scholar]
- 13.Ehrenfeld JM, Walsh JL, Sandberg WS. Right- and left-sided Mallinckrodt double-lumen tubes have identical clinical per-formance. Anesth Analg. 2008;106(6):1847–1852. doi: 10.1213/ane.0b013e31816f24d5. [DOI] [PubMed] [Google Scholar]
- 14.Cook RI, McDonald JS, Nunziata E. Differences between handwritten and automatic blood pressure records. Anesthesiology. 1989;71(3):385–390. doi: 10.1097/00000542-198909000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Devitt JH, Rapanos T, Kurrek M, Cohen MM, Shaw M. The anesthetic record: accuracy and completeness. Can J Anaesth. 1999;46(2):122–128. doi: 10.1007/BF03012545. [DOI] [PubMed] [Google Scholar]
- 16.O’Reilly M, Talsma A, VanRiper S, Kheterpal S, Burney R. An anesthesia information system designed to provide physician-specific feedback improves timely administration of pro-phylactic antibiotics. Anesth Analg. 2006;103(4):908–912. doi: 10.1213/01.ane.0000237272.77090.a2. [DOI] [PubMed] [Google Scholar]
- 17.Rohrig R, Junger A, Hartmann B, et al. The incidence and prediction of automatically detected intraoperative cardiovascular events in noncardiac surgery. Anesth Analg. 2004;98(3):569–577. doi: 10.1213/01.ane.0000103262.26387.9c. Table of contents. [DOI] [PubMed] [Google Scholar]
- 18.Feldman JM. Do anesthesia information systems increase mal-practice exposure? Results of a survey. Anesth Analg. 2004;99(3):840–843. doi: 10.1213/01.ANE.0000130259.52838.3B. Table of contents. [DOI] [PubMed] [Google Scholar]
- 19.Epstein RH, Gratch DM, Grunwald Z. Development of a scheduled drug diversion surveillance system based on an analysis of atypical drug transactions. Anesth Analg. 2007;105(4):1053–1060. doi: 10.1213/01.ane.0000281797.00935.08. Table of contents. [DOI] [PubMed] [Google Scholar]
- 20.Dexter F, Penning DH, Lubarsky DA, et al. Use of an automated anesthesia information system to determine reference limits for vital signs during cesarean section. J Clin Monit Comput. 1998;14(7–8):491–498. doi: 10.1023/a:1009900810721. [DOI] [PubMed] [Google Scholar]
- 21.Muravchick S, Caldwell JE, Epstein RH, et al. Anesthesia information management system implementation: a practical guide. Anesth Analg. 2008;107(5):1598–1608. doi: 10.1213/ane.0b013e318187bc8f. [DOI] [PubMed] [Google Scholar]
- 22.O’Sullivan CT, Dexter F, Lubarsky DA, Vigoda MM. Evidence-based management assessment of return on investment from anesthesia information management systems. AANA J. 2007;75(1):43–48. [PubMed] [Google Scholar]
- 23.Lutner RE, Roizen MF, Stocking CB, et al. The automated interview versus the personal interview. Do patient responses to preoperative health questions differ? Anesthesiology. 1991;75(3):394–400. [PubMed] [Google Scholar]
- 24.Boersma E, Kertai MD, Schouten O, et al. Perioperative cardiovascular mortality in noncardiac surgery: validation of the Lee cardiac risk index. Am J Med. 2005;118(10):1134–1141. doi: 10.1016/j.amjmed.2005.01.064. [DOI] [PubMed] [Google Scholar]
- 25.Stonemetz J, Ruskin K. Anesthesia informatics. Springer; London: 2008. [Google Scholar]
- 26.Vigoda MM, Gencorelli F, Lubarsky DA. Changing medical group behaviors: increasing the rate of documentation of quality assurance events using an anesthesia information system. Anesth Analg. 2006;103(2):390–395. doi: 10.1213/01.ane.0000221176.27215.20. Table of contents. [DOI] [PubMed] [Google Scholar]
- 27.Williams JR. Anesthesia information management systems. AANA J. 2005;73(3):178–181. [PubMed] [Google Scholar]
- 28.Sandberg WS. Anesthesia information management systems: almost there. Anesth Analg. 2008;107(4):1100–1102. doi: 10.1213/ane.0b013e3181867fd0. [DOI] [PubMed] [Google Scholar]
- 29.Stahl JE, Sandberg WS, Daily B, et al. Reorganizing patient care and workflow in the operating room: a cost-effectiveness study. Surgery. 2006;139(6):717–728. doi: 10.1016/j.surg.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 30.Epstein RH, Dexter F, Ehrenfeld JM, Sandberg WS. Implications of event entry latency on anesthesia information management decision support systems. Anesth Analg. 2009;108(3):941–947. doi: 10.1213/ane.0b013e3181949ae6. [DOI] [PubMed] [Google Scholar]
- 31.Allard J, Dzwonczyk R, Yablok D, Block FE, Jr, McDonald JS. Effect of automatic record keeping on vigilance and record keeping time. Br J Anaesth. 1995;74(5):619–626. doi: 10.1093/bja/74.5.619. [DOI] [PubMed] [Google Scholar]
- 32.Kheterpal S, Gupta R, Blum JM, Tremper KK, O’Reilly M, Kazanjian PE. Electronic reminders improve procedure documentation compliance and professional fee reimbursement. Anesth Analg. 2007;104(3):592–597. doi: 10.1213/01.ane.0000255707.98268.96. [DOI] [PubMed] [Google Scholar]
- 33.Gardner M. Computerized anaesthesia information management systems: are we on the threshold of widespread use? Curr Opin Anaesthesiol. 2001;14(6):643–647. doi: 10.1097/00001503-200112000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Vigoda MM, Lubarsky DA. Failure to recognize loss of incoming data in an anesthesia record-keeping system may have increased medical liability. Anesth Analg. 2006;102(6):1798–1802. doi: 10.1213/01.ane.0000217235.25350.5e. [DOI] [PubMed] [Google Scholar]


