Abstract
Introduction
Sexuality is a key aspect of women’s physical and psychological health. Research shows both patients and physicians face barriers to communication about sexuality. Given their expertise and training in addressing conditions of the female genital tract across the female life course, obstetrician/gynecologists (ob/gyns) are well-positioned among all physicians to address sexuality issues with female patients. New practice guidelines for management of female sexual dysfunction and the importance of female sexual behavior and function to virtually all aspects of ob/gyn care, and to women’s health more broadly, warrant up-to-date information regarding ob/gyns’ sexual history-taking routine.
Aims
To determine obstetrician/gynecologists’ practices of communication with patients about sexuality, and to examine the individual and practice-level correlates of such communication.
Methods
A population-based sample of 1154 practicing U.S. obstetrician/gynecologists (53% male; mean age 48 years) was surveyed regarding their practices of communication with patients about sex.
Main Outcome Measures
Self-reported frequency measures of ob/gyns’ communication practices with patients including whether or not ob/gyns discuss patients’ sexual activities, sexual orientation, satisfaction with sexual life, pleasure with sexual activity, and sexual problems or dysfunction, as well as whether or not one ever expresses disapproval of or disagreement with patients’ sexual practices. Multivariable analysis was used to correlate physicians’ personal and practice characteristics with these communication practices.
Results
Survey response rate was 65.6%. Sixty-three percent of ob/gyns reported routinely assessing patients’ sexual activities; 40% routinely asked about sexual problems. Fewer asked about sexual satisfaction (28.5%), sexual orientation/identity (27.7%), or pleasure with sexual activity (13.8%). A quarter of ob/gyns reported they had expressed disapproval of patients’ sexual practices. Ob/gyns practicing predominately gynecology were significantly more likely than other ob/gyns to routinely ask about each of the five outcomes investigated.
Conclusion
The majority of U.S. ob/gyns report routinely asking patients about their sexual activities, but most other areas of patients’ sexuality are not routinely discussed.
Keywords: Female Sexuality, Patient-Physician Communication, Sexual History-Taking, Female Sexual Health
INTRODUCTION
The introduction of sildenafil citrate and other effective therapies to treat male erectile dysfunction has prompted renewed attention to female sexuality and the development of definitions and treatments for female sexual dysfunction.1, 2, 3, 4 Recently, the American College of Obstetricians and Gynecologists published its first Practice Bulletin on female sexual dysfunction.5 As women become more aware of the biological and medical aspects of female sexual dysfunction, they are likely to increase their demand for medical counsel regarding sexuality. Studies show patients would like to discuss sexuality-related issues with their physicians but are often reluctant to do so because of fear the physician will be embarrassed or will dismiss their concern.6, 7 Similarly, studies of physicians suggest that lack of time or training, fear of embarrassing themselves or their patients, and physicians’ own religious beliefs8 influence discussion about sexuality-related issues with patients.9–11
Recent studies estimate that about a third of young and middle-aged women12 and about half of older women13 experience some sort of sexual problem such as low desire, difficulty lubricating, pain during intercourse, lack of pleasure, or inability to orgasm. Sexual behavior, such having multiple partners, having unprotected sex, or having sex with high risk individuals, has been associated with various health risks, including sexually transmitted infections, HIV, and pelvic inflammatory disease. These conditions can compromise women’s reproductive and overall health.14 Many sexuality-related issues, like some sexually transmitted infections, anorgasmia, lack of sexual satisfaction, and sexual desire disorders, show no physical signs, making patient-physician communication particularly important for identifying problems and promoting positive sexual health outcomes.
Few studies have investigated the specific content of the physician sexual-history taking or how physicians assess patients’ sexual function and satisfaction. Physician characteristics such as gender,10, 11, 15, 16 age,10, 11, 17 race,17 sexual orientation,18 location of medical education,15 and type of practice15 have been investigated with mixed results in studies of physicians of various medical specialties. Some studies show female physicians are significantly more likely to discuss sexual activity11 and screen patients for Chlamydia,16 while others reported no significant association between gender and sexual history-taking15 or screening for sexual dysfunction.10 Previous studies show younger physicians are significantly associated with better HIV prevention practices17 and more likely to take sexual histories19 while others found no significant association between physician age and asking about sexual activity11 or screening patients for sexual dysfunction.10 Previous studies are limited by small samples15, 18 or samples drawn from single states or cities in the U.S.,11, 16, 18, 20 which lack sufficient power to generate national estimates about obstetrician/gynecologist (ob/gyn) practices.
Previous studies that include physicians across various specialties show that ob/gyns are more likely than other physicians to report taking a sexual history,11, 16 to have more positive attitudes toward treating and counseling patients about sexually-transmitted infections,20 and to ask about specific sexual health risk factors such as condom use and high-risk sex partners.21 Despite the importance of female sexual behavior and function to virtually all aspects of ob/gyn care, little is known about the sexual history-taking routines of ob/gyns.
Ob/gyns, because of the depth and specialization of expertise and training in female genital tract and reproductive health across the life course, are well positioned among physicians to address sexuality issues with female patients. This study uses a national probability sample to investigate U.S. ob/gyns’ self-reported practices of communication with patients regarding sexuality focusing specifically on those ob/gyns who routinely incorporate sexual history-taking into their interactions with patients. It explores a hypothesized association between those communication practices and ob/gyns’ practice and individual characteristics. Knowledge about these practices is important to the successful implementation of the recent ACOG Practice Guidelines and to quality improvement in women’s health care.5
METHODS
Study Population
The methods for this national survey have been described in detail in another publication.22–24 In 2008, a national probability sample of currently practicing physicians from across the U.S. listing ob/gyn as their primary specialty was selected from the American Medical Association Physician Master File, a database intended to include all physicians in the U.S..
Eligible physicians were notified by mail that they would receive a questionnaire soon on topics related to sexual and reproductive health. The letter asked for their cooperation in completing and sending back the questionnaire. Because all of the respondents were adults and the survey was conducted completely by mail, the respondent’s return of the questionnaire constituted their informed consent to participate. This protocol and the questionnaire were reviewed and approved by a University of Chicago Institutional Review Board.
Data Collection
Questionnaires were administered by postal mail between October 2008 and January 2009 including an advance letter, post card reminder, and three rounds of questionnaire mailings. Respondents were incentivized with a $20 bill included in the first mailing, and an additional $30 was offered in the third mailing. Of 1800 potential respondents, forty were declared out of scope: 38 surveys were returned after multiple attempts were made to contact respondents at different addresses, one respondent had retired, and another had moved out of the country.
Building on prior work,8, 13, 25, 26 the overall purpose of the survey was to obtain national estimates of ob/gyns’ knowledge, attitudes, and practices regarding aspects of patient care that may be considered by some as morally or ethically challenging, and how physicians’ individual, including religious, characteristics influence these domains. A self-administered questionnaire was developed after qualitative interviews with a purposive sample of ob/gyn physicians8 and in consultation with prominent ob-gyn physician researchers and ethicists in the field. Interviews were conducted with a small purposive sample of physicians around the country on selected questions to assess comprehensibility and relevance to practice. Questionnaires were pre-tested with ob-gyn faculty members at The University of Chicago Pritzker School of Medicine.
Respondents were asked to provide individual (demographic, religious) and practice characteristics using 41 close-ended questionnaire items. This included the frequency with which ob/gyns addressed various aspects of patients’ sexuality. Self-reported communication with patients about sexuality was assessed using the following statement and items: “We are interested in doctors’ practices about talking to their patients about sexuality. Please take a minute to think back and indicate how often you do each of the following: a) ask patients about their sexual activities, b) ask patients about their sexual orientation or identity, c) ask patients if they are satisfied with their sexual life, d) ask patients if they experience pleasure with sexual activity, e) ask patients questions to assess for sexual problems or dysfunction, f) express to patients disapproval of or disagreement with their sexual practices.” Response options were “routinely,” “sometimes,” “rarely,” or “never.”
Analysis
Descriptive analyses stratified by physician gender were performed. Bivariate and multivariable logistic regression were used to analyze each of the 6 outcomes. Likelihood of asking patients about sexual activities, orientation/identity, satisfaction, pleasure, and problems/dysfunction were each modeled dichotomously comparing those who reported they “routinely” asked versus all others. Likelihood of expressing disapproval of or disagreement with patients’ sexual practices was modeled dichotomously comparing those who reported they “never” did versus all others.
Informed by prior research on physician characteristics known to influence communication11, 15, 16 and by bivariate findings, these multivariable models included as covariates self-reported: gender (male, female), age group (45 years and younger, 46–59 years, 60 years and older), type of patients seen, location of medical school (U.S. vs. foreign), immigration history (American-born, foreign-born), religious affiliation (none, Hindu, Muslim, Jewish, Roman Catholic, Evangelical Protestant, Non-evangelical Protestant), and importance of religion to the physician (most important, very important, fairly important, not important). Type of patients seen was defined as predominantly obstetrics, predominantly gynecology, or general ob/gyn practice. “Predominantly” was defined as seeing more than 60% of a specific patient type (obstetrics, gynecology) per week. “General ob/gyn practice” was defined as seeing 40–60% of gynecology and 40–60% of obstetrics patients per week. Gynecology included outpatient gynecology and operating-room based gynecologic procedures and surgery. Obstetrics included prenatal care and obstetrics/delivery.
Results are presented as adjusted odds ratios with 95% confidence intervals. Respondents leaving questions blank were omitted from the analyses pertaining to those items. A total of 81 respondents across the six regression analyses had missing values on one or more variables. The prevalence of missing values was greater among foreign- versus American-born (9.1% vs. 4.7%, respectively p<.001) and among those with no religious affiliation (11.7%) compared to others (lowest missing 2.2%, Hindu and Non-Evangelical Protestants).
The analyses included case weights to account for sampling strategy and differences in response rate by ethnic surname and foreign medical school graduation status. Weights were used for all analyses to adjust for differential probabilities of selection and differential non-response. All analyses were completed using Stata statistical software, version 10.1.27
Results
Respondent Characteristics
Of 1760 eligible participants, 1154 surveys were completed yielding an unweighted response rate of 65.6% (weighted 67.3%). Seven additional participants were eliminated because they were not board certified in ob/gyn (n=6), and one was no longer practicing medicine. The total number of participants included in this study was 1147. Compared with respondents, non-respondents were more likely to be foreign medical graduates. Mean age of respondents was 48 years (weighted SD 8.95), and 53% were male. Thirty percent identified their religious affiliation as Non-evangelical Protestant, 28% as Roman Catholic, 12% as Jewish, 12% as Evangelical Protestant, and 12% reported no religious affiliation. Forty-three percent saw predominantly gynecology patients. The personal and practice characteristics of respondents are summarized in Table 1.
Table 1.
Respondent characteristics of N=1147 US Obstetrician-Gynecologists
| Men (N=613) | Women (N=534) | |
|---|---|---|
|
|
||
| Age | ||
|
| ||
| 60 & over | 18.8 [15.6–22.5] | 4.9 [3.3–7.3] |
|
| ||
| 46–59 | 51.1 [46.8–55.5] | 34.7 [30.4–39.2] |
|
| ||
| 45 & under | 30.0 [26.2–34.2] | 60.4 [55.8–64.9] |
|
| ||
| Race/Ethnicity | ||
|
| ||
| White, non-Hispanic | 82.2 [78.6–85.4] | 73.2 [68.9–77.1] |
|
| ||
| Asian | 10.5 [8.1–13.4] | 15.1 [12.2–18.5] |
|
| ||
| Other | 7.3 [5.2–10.1] | 11.7 [8.9–15.2] |
|
| ||
| Immigration History | ||
|
| ||
| American-born | 79.0 [75.3–82.2] | 80.5 [76.7–83.9] |
|
| ||
| Foreign-born | 21.0 [17.8–24.7] | 19.5 [16.1–23.3] |
|
| ||
| Medical School Graduation | ||
|
| ||
| US Medical Grads | 84.5 [81.3–87.4] | 91.4 [88.7–93.5] |
|
| ||
| Foreign Medical Grads | 15.5 [12.7–18.8] | 8.6 [6.5–11.3] |
|
| ||
| Type of Patients Seen | ||
|
| ||
| Predominately Obstetrics | 30.8 [26.9–35.0] | 21.0 [17.4–25.0] |
|
| ||
| Predominately Gynecology | 40.6 [36.4–44.9] | 45.6 [41.0–50.3] |
|
| ||
| General Ob/Gyn Practice | 28.7 [24.9–32.8] | 33.5 [29.2–38.0] |
|
| ||
| Religious Affiliation | ||
|
| ||
| None | 12.4 [9.7–15.7] | 11.5 [8.8–14.9] |
|
| ||
| Hindu | 1.5 [1.0–2.1] | 4.1 [2.8–5.8] |
|
| ||
| Jewish | 12.3 [9.9–15.1] | 6.8 [4.9–9.4] |
|
| ||
| Muslim | 1.6 [1.1–2.5] | 2.2 [1.4–3.6] |
|
| ||
| Roman Catholic | 27.5 [23.4–31.3] | 26.5 [22.5–31.0] |
|
| ||
| Evangelical Protestant | 12.0 [9.4–15.3] | 7.5 [5.3–10.5] |
|
| ||
| Non-evangelical Protestant | 30.0 [26.0–34.1] | 36.3 [31.8–41.0] |
|
| ||
| Other Religion | 3.1 [1.9–5.1] | 5.0 [3.3–7.5] |
|
| ||
| Importance of Religion in Life | ||
|
| ||
| Most important part | 14.2 [11.4–17.6] | 14.4 [11.4–18.1] |
|
| ||
| Very important part | 34.0 [30.0–38.2] | 32.9 [28.6–37.5] |
|
| ||
| Fairly important part | 27.7 [24.0–31.8] | 26.6 [22.7–31.0] |
|
| ||
| Not important part | 24.1 [20.6–28.1] | 26.1 [22.2–30.5] |
Values are listed as percentages.
Estimates are weighted to account for differential probabilities of selection and differential non-response. Estimates may not add up to 100% due to rounding error.
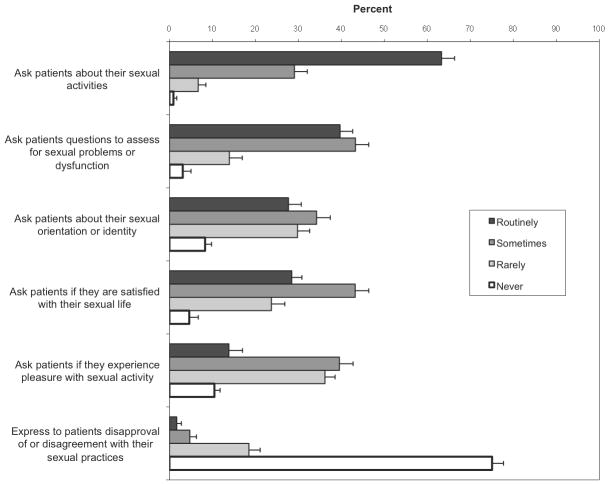
The frequency with which ob/gyns reported addressing sexuality-related topics is illustrated in Figure 1. Sixty-three percent of ob/gyns surveyed reported that they routinely ask about patients’ sexual activities. A smaller proportion reported routinely asking patients about sexual problems or dysfunction (40%), satisfaction with sexual life (29%), and sexual identity or orientation (28%). Only 14% reported routinely asking patients if they experience pleasure with sexual activity; one in ten ob/gyns (10%) never asked this question. The majority of ob/gyns (75%) reported that they never express disapproval of or disagreement with patients’ sexual practices.
Figure 1.
Estimates of Population Frequencies for N=1147 US Obstetrician-Gynecologists’ Practices Regarding Addressing Sexuality
Asking about patient sexuality
In bivariate analyses, female ob/gyns were significantly more likely than male ob/gyns to routinely ask patients about sexual activity (73% vs. 54%, p<.001) and sexual orientation or identity (39% vs. 17%, p<.001). Ob/gyns ages 60 and older were significantly less likely than younger colleagues to routinely ask patients about their sexual orientation or identity (11% as compared to 32% of those 45 years and younger and 28% of those 46–59 years, p<.001). Foreign medical graduates were more likely than U.S. graduates to routinely ask patients about sexual orientation or identity (82% as compared to 71%, p<.01). Ob/gyns born in the U.S. were more likely than foreign-born ob/gyns to routinely ask patients about sexual satisfaction (30% vs. 23%, p<.05) and about sexual problems or dysfunction (42% vs. 33%, p<.05). No significant differences in the likelihood of routinely addressing any of the domains of sexuality were found by physician race, religious affiliation, or importance of religion to the physicians’ life.
Gynecologists were significantly more likely than general ob/gyns and obstetricians to routinely ask patients about sexual activities (71% vs. 59% and 57%, p<.001), orientation or identity (32% vs. 26% and 22%, p<.05), and sexual problems or dysfunction (46% vs. 37% and 33%, p<.01).
As shown in Table 2, multivariable analysis revealed significant associations between ob/gyns’ personal and practice characteristics and their communication practices with patients about sexuality (Table 2). Female ob/gyns were significantly more likely than male ob/gyns to routinely ask about sexual activities (adjusted odds ratio [AOR] 1.98 [95% CI 1.44 – 2.72]) and sexual orientation/identity ([AOR] 2.92 [95% CI 2.09 – 4.08). Physicians younger than 60 years old were significantly more likely than those 60 and older to routinely ask patients about their sexual orientation/identity (46–59 years old, [AOR] 2.50 [95% CI 1.28 – 4.50; 45 years old and younger, [AOR] 2.40 [95% CI 1.32 – 4.73]). Physicians identifying their religious affiliation as Roman Catholic ([AOR] 0.54 [95% CI 0.30 – 0.98]) were significantly less likely to routinely ask patients about their sexual activity. Those listing religion as the most important part of their lives were significantly more likely to routinely ask patients about sexual activities ([AOR] 1.91 [95% CI 1.08 – 3.40]). No significant differences in the likelihood of routinely addressing any of the domains of sexuality were found by physician race, location of medical school, or immigration status.
Table 2.
Multivariable Analysis of Factors Associated with Addressing Sexuality with Patients
| Characteristic | Adjusted Odds Ratio (95% CI) | p-value |
|---|---|---|
| Routinely ask patients about their sexual activities | ||
| Gender | ||
| Male | 1.00 [Referent] | |
| Female | 1.98 (1.44, 2.72) | <0.001 |
| Type of Patient | ||
| General Ob/Gyn | 1.00 [Referent] | |
| Predominately Obstetrics | 0.96 (0.67, 1.39) | |
| Predominately Gynecology | 1.79 (1.27, 2.50) | 0.001 |
| Religious Affiliation | ||
| None | 1.00 [Referent] | |
| Hindu | 1.55 (0.64, 3.77) | |
| Jewish | 0.83 (0.44, 1.58) | |
| Muslim | 1.26 (0.50, 3.20) | |
| Roman Catholic | 0.54 (0.30, 0.98) | 0.04 |
| Evangelical Protestant | 0.51 (0.24, 1.09) | |
| Non-evangelical Protestant | 0.56 (0.31, 1.01) | |
| Other Religion | 1.18 (0.44, 3.14) | |
| Importance of Religion in Life | ||
| Not important part | 1.00 [Referent] | |
| Fairly important part | 1.14 (0.74, 1.76) | |
| Very important part | 1.39 (0.89, 2.15) | |
| Most important part | 1.91 (1.08, 3.40) | 0.03 |
| Routinely ask patients about their sexual orientation or identity | ||
| Gender | ||
| Male | 1.00 [Referent] | |
| Female | 2.92 (2.09, 4.08) | < 0.001 |
| Age | ||
| 60 & over | 1.00 [Referent] | |
| 46–59 | 2.50 (1.28, 4.50) | 0.005 |
| 45 & under | 2.40 (1.32, 4.73) | 0.006 |
| Type of Patient | ||
| General Ob/Gyn | 1.00 [Referent] | |
| Predominately Obstetrics | 0.98 (0.64, 1.51) | |
| Predominately Gynecology | 1.51 (1.05, 2.17) | 0.03 |
| Routinely ask patients if they are satisfied with their sexual life | ||
| Type of Patient | ||
| General Ob/Gyn | 1.00 [Referent] | |
| Predominately Obstetrics | 1.06 (0.70, 1.59) | |
| Predominately Gynecology | 1.47 (1.02, 2.11) | 0.04 |
| Routinely ask patients if they experience pleasure with sexual activity | ||
| Type of Patient | ||
| General Ob/Gyn | 1.00 [Referent] | |
| Predominately Obstetrics | 1.08 (0.62, 1.90) | |
| Predominately Gynecology | 1.81 (1.13, 2.92) | 0.01 |
| Routinely ask patients questions to assess for sexual problems or dysfunctions | ||
| Type of Patient | ||
| General Ob/Gyn | 1.00 [Referent] | |
| Predominately Obstetrics | 0.79 (0.55, 1.16) | |
| Predominately Gynecology | 1.58 (1.14, 2.19) | 0.006 |
Estimates are weighted to account for differential probabilities of selection and differential non-response All models included gender, age, race/ethnicity, immigration history, medical school graduation, type of patients seen, religious affiliation, and importance of religion in the physicians’ life as covariates.
Ob/gyns practicing predominately gynecology were significantly more likely than other ob/gyns to routinely ask about each of the five outcomes investigated.
Expressing disapproval of patients’ sexual practices
In a bivariate analysis, foreign medical school graduates were significantly more likely than U.S. medical graduates to report ever expressing disapproval of or disagreement with patients’ sexual practices (32% vs. 24%, p<.05). This finding remained when adjusting for other factors in multivariable analysis (Table 3). Foreign medical graduates were more likely than U.S. medical graduates to be male (p<.001) and age 60 or older (p<.001). Fifty-eight percent were educated in the Middle East, 20% in Latin America, and 14% in Europe. Neither foreign medical school location (U.S./Canada, Latin America, Europe, Middle Eastern, African, or Asian) nor types of school funding (private vs. public) were found to be significant predictors of expressing disapproval or disagreement with patients’ sexual practices.
Table 3.
Multivariable Analyses of Factors Associated with Ever Expressing Disapproval of or Disagreement with Patients’ Sexual Practices
| Characteristic | Adjusted Odds Ratio (95% CI) | p-value |
|---|---|---|
| Medical School Graduation | ||
| US Medical Grads | 1.00 [Referent] | |
| Foreign Medical Grads | 2.10 (1.09, 4.02) | 0.03 |
| Religious Affiliation | ||
| None | 1.00 [Referent] | |
| Hindu | 1.01 (0.36, 2.83) | |
| Jewish | 0.98 (0.47, 2.09) | |
| Muslim | 1.40 (0.49, 4.00) | |
| Roman Catholic | 0.77 (0.38, 1.59) | |
| Evangelical Protestant | 1.04 (0.46, 2.37) | |
| Non-evangelical Protestant | 1.17 (0.58, 2.33) | |
| Other Religion | 0.55 (0.18, 1.73) | |
| Importance of Religion in Physician’s Life | ||
| Not very important | 1.00 [Referent] | |
| Fairly important | 1.65 (0.98, 2.77) | |
| Very important part | 2.07 (1.23, 3.47) | 0.006 |
| Most important part | 2.75 (1.49, 5.04) | 0.001 |
Estimates are weighted to account for differential probabilities of selection and differential non-response.
All models included gender, age, race/ethnicity, immigration history, medical school graduation, type of patients seen, religious affiliation, and importance of religion in the physicians’ life as covariates.
Those ob/gyns who considered religion the most important part of their lives were significantly more likely than those who considered religion very, fairly, of not very important to express disapproval or disagreement with patients’ sexual practices (35% vs. 28%, 25% and 17%, p<.001).
In multivariable analysis, compared to ob/gyns for whom their religion is not very important, those for whom it is very important ([AOR] 2.1 [95%CI 1.2 – 3.5]) or most important ([AOR] 2.8 [95%CI 1.5–5.0]) were significantly more likely to ever express disapproval of or disagreement with patients’ sexual practices. Compared to U.S. medical graduates, foreign medical graduates were significantly more likely to express disapproval of or disagreement with patients’ sexual practices ([AOR] 2.1 [95%CI 1.1–4.0]).
No significant differences in the likelihood of expressing disapproval were found by physician religious affiliation, sex, age, race, type of patients seen, or immigration status.
Discussion
This national survey of a probability sample of practicing ob/gyns found that most reported routinely asking about patients’ sexual activities. However, other aspects of female patients’ sexuality, including sexual identity and function, were not reported to be routinely addressed.
Ob/gyns who saw predominantly gynecology patients were significantly more likely than other ob/gyns to routinely address all domains of sexuality included in this study, independent of age and gender. Obstetric visits focus primarily on prenatal testing and maternal-fetal monitoring routines. This finding may in part reflect differences in time allocation and priorities of gynecology versus obstetric visits. Nevertheless, this finding has important implications for clinical obstetrics care. Nearly all women participate in some type of sexual activity during pregnancy.28 Pregnant women have sexual health risks similar to those in non-pregnant women and also risk transmitting STIs and HIV to their offspring.29 Many pregnant women and their partners also experience sexual problems or changes in their sexuality during or as a result of pregnancy.30, 31 Our findings suggest sexual history-taking and anticipatory guidance about sexual changes in pregnancy, based on available evidence, are areas for improvement in obstetric care.
Although those practicing predominantly gynecology were most likely to routinely address sexuality, we found the majority of ob/gyns do not routinely ask questions to assess for sexual problems or dysfunction, nor do they routinely ask patients about pleasure with sexual activity or satisfaction with their sexual lives. These basic elements of a sexual history can reveal information of importance to the patient’s well-being and her overall medical and gynecologic care, though it is recognized that ob/gyns are trained to calibrate their sexual-history taking to individual patient needs. A recent self-report survey of nearly 500 physician members of the American Urogynecologic Society (response rate 49%) found that the majority do not consistently screen for female sexual dysfunction.10 Our study corroborates this finding among a larger, nationally representative sample of ob/gyns. Sexual problems are directly related to women’s satisfaction with their sexual lives and their ability to experience pleasure with sexual activity.
Trainees are expected to be gaining experience with assessment and management of female sexual problems.5, 32 Recent studies, however, indicate medical students33 and ob/gyn residents34 may not be receiving adequate training in sexual health, and little is known about how training influences actual practices. Additionally, a recent review of the literature reports sexual medicine education for physicians and other health professionals is non-standardized, variable, and inadequate, with a discrepancy between knowledge of sexual medicine and clinical practice.35 In accord with the recent ACOG Practice Bulletin on Female Sexual Dysfunction, continuing medical education opportunities on communication about female sexual matters could be expanded to all practicing ob/gyns, with an emphasis on the importance to ob/gyn care across the patient life course. Routine assessment with well-validated measures would advance standardization in clinical care and accelerate research. Comprehensive training offered at specialty meetings, such as those held by the International Society for the Study of Women’s Sexual Health,36 could be adapted for broader audiences or self-learning tools used for maintenance of board certification. Physician adoption of these practices could be supported through sexual history prompts in the electronic medical record, perhaps using validated items such as those developed by the NIH Patient Reported Outcomes Measurement Information System (PROMIS) effort.37 As women adopt their own personal health records, patient prompts may also help support routine communication38 about sexual matters, initiated by the patient. Guidelines for sexual history-taking identify sexual activity and partner status, sexual risk factors, sexual function including pain, contraception, and sexual orientation as basic components for routine assessment.5, 39–41
Less than a third of ob/gyns in our study routinely asked patients about their sexual orientation or identity. Studies show lesbian and bisexual women may present with a range of sexual experiences not obvious to, and therefore overlooked, by physicians. On the one hand, assuming a heterosexual orientation can alienate a non-heterosexual patient and result in misinterpretation of symptoms or misdiagnosis. For example, two studies have found lesbian and bisexual women to have a higher prevalence of risk factors for reproductive and breast cancers42, than heterosexual women, in part due to stigma and perceived discrimination by physicians and others in the health care system.43 On the other hand, without open dialogue about sexual matters, a physician may wrongly assume that a patient who identifies as lesbian may not have heterosexual encounters or want to discuss contraception or pregnancy options.44 Sexual orientation, the sex of a woman’s sexual partner(s), and the quality of a patient’s sexual life are all relevant dimensions of patient counseling, risk assessment, and overall ob/gyn care, and may change over time.
In this study, younger ob/gyns were more likely than others to report discussing sexual identity or orientation with their patients. Prior studies, which surveyed physicians from a variety of specialties including pediatrics, internal medicine, family medicine, and ob/gyn, report mixed results between physician age and inquiry about patients’ sexuality. Some report a significant correlation between physician age and likelihood to inquire about sexuality and others found no significant difference.10, 11, 18 With respect to gender, previous studies corroborate our finding that female physicians are significantly more likely than male physicians to routinely address various aspects of patients’ sexuality. 11, 18, 19, 45 A study of 901 female patients from a community hospital system reported 83% chose a female ob/gyn provider with more than half selecting their provider based on gender or age.46 In the same study, younger patients chose younger ob/gyns, and single patients chose female ob/gyns. Other studies find that female physicians spend more time with patients, and patients share more biomedical and psychosocial information with female providers.47, 48 One study of nearly 80 physicians from a single multi-specialty practice in the U.S. found physicians were significantly more uncomfortable taking sexual histories when the patient was of the opposite gender.49 This suggests a further barrier in communication regarding sexuality particularly for ob/gyn practice, as all patients are female yet may have a male physician. While males still represent the majority of practicing ob/gyns, more than two-thirds of incoming ob/gyn residents are female. As ob/gyn becomes a more female dominated field, it is possible communication regarding sexual issues may improve. Our findings support this in regard to communication about sexual orientation or identity. Ob/gyns’ comfort and willingness to discuss sexual identity and orientation with patients remains an important area for further research; improved care for women of sexual minority groups may require interventions tailored to the age and/or gender of the ob/gyn physician. Recommendations to assist ob/gyns in engaging women of sexual minority groups, including STI screening, counseling, and family planning, are available from the American Congress of Obstetrics and Gynecology.50
The vast majority of ob/gyns in this study reported never expressing disapproval of or disagreement with patients’ sexual practices. Those who did tended to be foreign medical graduates and/or to consider religion most or very important in their lives. Foreign medical graduates were more likely than U.S. medical graduates to be older and male. More than half were educated in the Middle East, and a smaller proportion in Latin America and Europe. Neither school location nor school funding were found to be significant predictors of expressing disapproval or disagreement with patients’ sexual practices. Further research is needed to explain this association, which may be due to unmeasured factors such as differences in medical school curriculum, and cultural practices and beliefs about human sexuality. These findings may be most relevant for U.S. women receiving ob/gyn care in settings with a high concentration of ob/gyns who are foreign medical graduates or for women receiving care in the countries where U.S. foreign medical graduates are educated.
Most religions have strong norms regarding sexual practices; these norms have been found to influence ob/gyns’ medical practice.8, 22, 24 We found that those for whom religion is more important are more likely to have ever expressed disapproval of or disagreement with their patient’s sexual practices. These findings parallel those of an earlier study, which found that physicians who are more religious tend to be more supportive of describing to patients one’s moral objections to controversial clinical practices.51 In prior qualitative work, some ob/gyns who self-identified as religious believed it appropriate to encourage patients to change their sexual behaviors if the physician believed doing so was in the patient’s best interest.8 We can only speculate about why Roman Catholic ob/gyns were less likely to ask patients about sexual activity. The Roman Catholic Church has explicit dogmatic teachings regarding sexuality that are followed by only a minority of Catholics.52 As such, perhaps Catholic ob/gyns have a tendency to not ask about patient behavior that could reveal violation of Catholic teaching. Together, these data provide yet more evidence that physicians’ clinical practices are shaped in part by their religious and other moral convictions. Further research is needed to translate these findings to improved patient-physician communication and outcomes in the area of female sexual health.
This study had limitations. As in most other studies on this topic, physician responses were self-reported. In this case, self-report may have resulted in overestimation of physician history-taking practices and under-estimation of the prevalence of expressing disapproval, due to social response bias. Differences in social response bias by religious or cultural norms may partially explain the differences in response to the question about ever expressing disapproval or disagreement with patients’ sexual practices, and should be further explored. Furthermore, additional work is needed to better understand the meaning and implications of a physician’s expression of disapproval in this context. It is conceivable, for example, that some respondents may have considered counseling patients about risky sexual behaviors as an expression of disapproval. By not specifically defining answers to questions (eg., routinely, sometimes, rarely, never) it is possible that different respondents understood these terms differently. We were also unable to evaluate the quality or specific content of ob/gyns’ communication with patients about sexuality. Future research could include chart audits or direct observations of patient-physician encounters and should aim to develop a systematic approach to studying sexual history-taking content and quality in order to better evaluate and improve physician practices. The survey response rate was high, but non-responders were more likely to be foreign medical graduates. The number cases not included in the analyses was very low overall, but higher item non-response by those who were foreign-born and those with no religious affiliation may have introduced bias. Other characteristics, not investigated in this study, may have affected physicians’ willingness to participate and their responses to the studied items. Also, because the sample is comprised solely of U.S. ob/gyns, generalizability to other physician populations may be limited.
Conclusion
Obstetrician/gynecologists’ expertise, training and focus on female genital tract and reproductive health position them as important providers of female sexual health care. Yet, when ob/gyns talk about sex with their patients, conversations tend to focus rather narrowly on sexual activities. Ob/gyns tend not to talk about sexual identity or orientation, satisfaction, pleasure, or sexual problems/dysfunction, although these factors are salient to the diagnosis and/or treatment of many ob/gyn conditions. Our findings suggest that there are areas for improvement in ob/gyn practices with respect to communication with patients about the comprehensive range of sexual matters that relate to women’s health. Improvement will likely depend on graduate and continuing physician education, patient demand, availability of effective treatments for female sexual concerns, and an environment of care that facilitates the patient-physician relationship.
Acknowledgments
Funding
This study was supported by grants from the Greenwall Foundation, John Templeton Foundation, the National Center for Complementary and Alternative Medicine (1 K23 AT002749, to Dr. Farr Curlin), and the National Institute on Aging (NIH/NIA 1K23AG032870-01A1 and NIH/NIA 5P30 AG 012857 to Dr. Stacy Lindau).
Footnotes
Conflict of Interest: None
This study was conducted at The University of Chicago, Chicago, IL.
Title adapted from the following: Carter, Raymond. What We Talk About When We Talk About Love. USA: Vintage Books, 1989.
References
- 1.Clayton A, Jayne C, Jacobs M, Kimura T, Pyke R, Lewis-D’Agostino D. Efficacy of flibanserin as a potential treatment for Hypoactive Sexual Desire Disorder in North American premenopausal women: results from the DAHLIA trial. Journal of Sexual Medicine. 2009;6:408–409. [Google Scholar]
- 2.Krapf JM, Simon JA. The role of testosterone in the management of hypoactive sexual desire disorder in postmenopausal women. Maturitas. 2009 Jul;63(3):213–219. doi: 10.1016/j.maturitas.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 3.Basson R, Berman J, Burnett A, et al. Report of the international consensus development conference on female sexual dysfunction: definitions and classifications. The Journal of Urology. 2000;163(3):888–893. [PubMed] [Google Scholar]
- 4.Diagnostic and statistical manual of mental disorders. 4. Washington D.C: American Psychiatric Association; 2000. Revised. [Google Scholar]
- 5.Practice Bulletin: Female Sexual Dysfunction. 119. American College of Obsetrics and Gynecology; Apr, 2011. [DOI] [PubMed] [Google Scholar]
- 6.Marwick C. Survey says patients expect little physician help on sex. JAMA-Journal of the American Medical Association. 1999 Jun;281(23):2173–2174. doi: 10.1001/jama.281.23.2173. [DOI] [PubMed] [Google Scholar]
- 7.Lindau ST, Gavrilova N, Anderson D. Sexual morbidity in very long term survivors of vaginal and cervical cancer: A comparison to national norms. Gynecologic Oncology. 2007 Aug;106(2):413–418. doi: 10.1016/j.ygyno.2007.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Curlin FA, Dinner SN, Lindau ST. Of more than one mind: Obstetrician-gynecologists’ approaches to morally controversial decisions in sexual and reproductive healthcare. Journal of Clinical Ethics. 2008 Spr;19(1):11–21. [PubMed] [Google Scholar]
- 9.Bachmann G. Female sexuality and sexual dysfunction: Are we stuck on the learning curve? Journal of Sexual Medicine. 2006 Jul;3(4):639–645. doi: 10.1111/j.1743-6109.2006.00265.x. [DOI] [PubMed] [Google Scholar]
- 10.Pauls RN, Kleeman SD, Segal JL, Silva WA, Goldenhar LM, Karram MM. Practice patterns of physician members of the American Urogynecologic Society regarding female sexual dysfunction: results of a national survey. International Urogynecology Journal. 2005 Dec;16(6):460–467. doi: 10.1007/s00192-005-1286-5. [DOI] [PubMed] [Google Scholar]
- 11.Wimberly YH, Hogben M, Moore-Ruffin J, Moore SE, Fry-Johnson Y. Sexual History-Taking among Primary Care Physicians. Journal of the National Medical Association. 2006;98(12):1924–1929. [PMC free article] [PubMed] [Google Scholar]
- 12.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States - Prevalence and predictors. JAMA-Journal of the American Medical Association. 1999 Feb;281(6):537–544. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 13.Lindau ST, Schumm LP, Laumann EO, Levinson W, O’Muircheartaigh CA, Waite LJ. A study of sexuality and health among older adults in the United States. New England Journal of Medicine. 2007 Aug;357(8):762–774. doi: 10.1056/NEJMoa067423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holmes K, Sparling PF, Mardh P-A, et al. Sexually Transmitted Diseases. 3. New York: McGraw-Hill; 1999. [Google Scholar]
- 15.Kushner M, Solorio MR. The STI and HIV testing practices of primary care providers. Journal of the National Medical Association. 2007 Mar;99(3):258–263. [PMC free article] [PubMed] [Google Scholar]
- 16.Guerry SL, Bauer HM, Packel L, et al. Chlamydia Screening and Management Practices of Primary Care Physicians and Nurse Practitioners in California. Journal of General Internal Medicine. 2005;20(12):1102–1107. doi: 10.1111/j.1525-1497.2005.00240.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gemson DH, Colombotos J, Elinson J, Fordyce EJ, Hynes M, Stoneburner R. Acquired-ImmunoDeficiency-Syndrome Prevention- Knowledge, Attitudes, and Practices of Primary Care Physicians. Archives of Internal Medicine. 1991 Jun;151(6):1102–1108. doi: 10.1001/archinte.151.6.1102. [DOI] [PubMed] [Google Scholar]
- 18.Wilson IB, Kaplan S. Physician-patient communication in HIV disease: the importance of patient, physician, and visit characteristics. Journal of Acquired Immune Deficiency Syndromes: JAIDS. 2000 Dec 15;25(5):417–425. doi: 10.1097/00042560-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 19.Lewis CE, Freeman HE. The Sexual History-Taking and Counseling Practices of Primary Care Physicians. Western Journal of Medicine. 1987 Aug;147(2):165–167. [PMC free article] [PubMed] [Google Scholar]
- 20.Ashton MR, Cook RL, Wiesenfeld HC, et al. Primary care physician attitudes regarding sexually transmitted diseases. Sexually Transmitted Diseases. 2002 Apr;29(4):246–251. doi: 10.1097/00007435-200204000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Kerr SH, Valdiserri RO, Loft J, et al. Primary care physicians and their HIV prevention practices. Aids Patient Care and Stds. 1996;10(4):227–235. doi: 10.1089/apc.1996.10.227. [DOI] [PubMed] [Google Scholar]
- 22.Lawrence RE, Rasinski KA, Yoon JD, Curlin FA. Factors influencing physicians’ advice about female sterilization in USA: a national survey. Human Reproduction. Jan;26(1):106–111. doi: 10.1093/humrep/deq289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yoon JD, Rasinski KA, Curlin FA. Conflict and emotional exhaustion in obstetrician-gynaecologists: a national survey. Journal of Medical Ethics. Dec;36(12):731–735. doi: 10.1136/jme.2010.037762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lawrence RE, Rasinski KA, Yoon JD, Curlin FA. Obstetrician-gynecologist physicians’ beliefs about emergency contraception: a national survey. Contraception. Oct;82(4):324–330. doi: 10.1016/j.contraception.2010.04.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lindau ST, Tetteh A, Kasza K, Gilliam M. What Schools Teach Our Patients About Sex: Content, Quality, and Influences on Sex Education. Obstetrics & Gynecology. 2008;111(2 Part 1):256–266. doi: 10.1097/01.AOG.0000296660.67293.bf. [DOI] [PubMed] [Google Scholar]
- 26.Curlin FAMD, Chin MHMDMPH, Sellergren SAMA, Roach CJBS, Lantos JDMD. The Association of Physicians’ Religious Characteristics With Their Attitudes and Self-Reported Behaviors Regarding Religion and Spirituality in the Clinical Encounter. Medical Care. 2006;44(5):446–453. doi: 10.1097/01.mlr.0000207434.12450.ef. [DOI] [PubMed] [Google Scholar]
- 27.StataCorp. Stata Statistical Software: Release 10. College Station, TX: StataCorp LP; 2007. [Google Scholar]
- 28.Pauleta JR, Pereira NM, Graca LM. Sexuality During Pregnancy. Journal of Sexual Medicine. 2010 Jan;7(1):136–142. doi: 10.1111/j.1743-6109.2009.01538.x. [DOI] [PubMed] [Google Scholar]
- 29.Newell M-L. Mechanisms and timing of mother-to-child transmission of HIV-1. AIDS. 1998;12(8):831–837. doi: 10.1097/00002030-199808000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Bartellas E, Crane JMG, Daley M, Bennett KA, Hutchens D. Sexuality and sexual activity in pregnancy. British Journal of Obstetrics and Gynaecology. 2000;107(8):964–968. doi: 10.1111/j.1471-0528.2000.tb10397.x. [DOI] [PubMed] [Google Scholar]
- 31.Barrett G, Pendry E, Peacock J, Victor C, Thakar R, Manyonda I. Women’s sexual health after childbirth. BJOG: An International Journal of Obstetrics & Gynaecology. 2000;107(2):186–195. doi: 10.1111/j.1471-0528.2000.tb11689.x. [DOI] [PubMed] [Google Scholar]
- 32.Educational Objectives, A Core Curriculum in Obstetrics and Gynecology. 9. New York: Council on Resident Education in Obstetrics and Gynecology, Professional Publishing Group, Ltd; 2009. [Google Scholar]
- 33.Malhotra S, Khurshid A, Hendricks KA, Mann JR. Medical school sexual health curriculum and training in the United States. Journal of the National Medical Association. 2008 Sep;100(9):1097–1106. doi: 10.1016/s0027-9684(15)31452-8. [DOI] [PubMed] [Google Scholar]
- 34.Pancholy AB, Goldenhar L, Fellner AN, Crisp C, Kleeman S, Pauls R. Resident Education and Training in Female Sexuality: Results of a National Survey. The Journal of Sexual Medicine. 8(2):361–366. doi: 10.1111/j.1743-6109.2010.02117.x. [DOI] [PubMed] [Google Scholar]
- 35.Parish SJ, Clayton AH. Sexual medicine education: Review and commentary. Journal of Sexual Medicine. 2007 Mar;4(2):259–268. doi: 10.1111/j.1743-6109.2007.00430.x. [DOI] [PubMed] [Google Scholar]
- 36.International Society for the Study of Women’s Sexual Health. http://www.isswsh.org/
- 37.Patient-Reported Outcomes Measurement Information System (PROMIS) United States Department of Health and Human Services, National Institute of Health; 2004. [Google Scholar]
- 38.Bodenheimer T, Grumbach K. Electronic Technology. JAMA: The Journal of the American Medical Association. 2003 Jul 9;290(2):259–264. doi: 10.1001/jama.290.2.259. [DOI] [PubMed] [Google Scholar]
- 39.Nusbaum MRH, Hamilton CD. The proactive sexual health history. American Family Physician. 2002 Nov;66(9):1705–1712. [PubMed] [Google Scholar]
- 40.A Guide to Taking a Sexual History. US Department of Health and Human Services, Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 41.A Clinician’s Guide to Sexual History Taking. California STD/HIV Prevention Training Center; May, 2011. [Google Scholar]
- 42.Valanis BG, Bowen DJ, Bassford T, Whitlock E, Charney P, Carter RA. Sexual Orientation and Health: Comparisons in the Women’s Health Initiative Sample. Arch Fam Med. 2000 Sep 1;9(9):843–853. doi: 10.1001/archfami.9.9.843. [DOI] [PubMed] [Google Scholar]
- 43.Case P, Austin SB, Hunter DJ, et al. Sexual orientation, health risk factors, and physical functioning in the Nurses’ Health Study II. Journal of Womens Health. 2004;13(9):1033–1047. doi: 10.1089/jwh.2004.13.1033. [DOI] [PubMed] [Google Scholar]
- 44.Carroll NM. Optimal gynecologic and obstetric care for lesbians. Obstetrics and Gynecology. 1999 Apr;93(4):611–613. [PubMed] [Google Scholar]
- 45.Merrill JM, Laux LF, Thornby JI. Why doctors have difficulty with sex histories. Southern Medical Journal. 1990;83(6):613–617. doi: 10.1097/00007611-199006000-00004. [DOI] [PubMed] [Google Scholar]
- 46.Schnatz PF, Murphy JL, O’Sullivan DM, Sorosky JI. Patient choice: comparing criteria for selecting an obstetrician-gynecologist based on image, gender, and professional attributes. American Journal of Obstetrics and Gynecology. 2007;197(5):548.e541–548.e547. doi: 10.1016/j.ajog.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 47.Roter DL, Hall JA. Physician gender and patient-centered communication: A critical review of empirical research. Annual Review of Public Health. 2004;25:497–519. doi: 10.1146/annurev.publhealth.25.101802.123134. [DOI] [PubMed] [Google Scholar]
- 48.Roter D. The enduring and evolving nature of the patient-physician relationship. Patient Education and Counseling. 2000;39(1):5–15. doi: 10.1016/s0738-3991(99)00086-5. [DOI] [PubMed] [Google Scholar]
- 49.Burd ID, Nevadunsky N, Bachmann G. Impact of Physician Gender on Sexual History Taking in a Multispecialty Practice. Journal of Sexual Medicine. 2006;3(2):194–200. doi: 10.1111/j.1743-6109.2005.00168.x. [DOI] [PubMed] [Google Scholar]
- 50.Special Issues in Women’s Health. American Congress of Obstetricians & Gynecologists; 2005. [Google Scholar]
- 51.Curlin FA, Lawrence RE, Chin MH, Lantos JD. Religion, conscience, and controversial clinical practices. New England Journal of Medicine. 2007 Feb;356(6):593–600. doi: 10.1056/NEJMsa065316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Greeley A. The Catholic myth: The behavior and beliefs of American Catholics. New York, NY: Touchstone; 1990. [Google Scholar]