Abstract
Objectives
Coronary artery disease and osteoporosis increase in women after menopause. Computed tomography (CT) scans of the heart used to evaluate coronary arterial calcification include images of the thoracic vertebrae. The utility of using these images to assess bone health in women remains to be defined. Analyses of thoracic spine volumetric bone mineral density (vBMD) from CT scans of the heart were performed to determine how specific calibration affects the ability to assess vBMD in recently menopausal women and to evaluate how vBMD relates to areal bone mineral density (aBMD) using dual-energy X-ray absorptiometry (DEXA).
Methods
Women (n = 111) enrolled in the Kronos Early Estrogen Prevention Study (KEEPS) at Mayo Clinic underwent a CT scan of the heart that included calibration phantoms and a DEXA of the lumbar spine. The Spine Cancer Assessment program was used to determine vBMD of thoracic vertebrae with and without the calibration correction.
Results
Trabecular bone vBMD at T8 averaged 163.57 ± 28.58 and 157.94 ± 27.55 mg/cc (mean ± standard deviation, SD) for calibrated and uncalibrated values, respectively. The relationship between calibrated and uncalibrated measures approached unity (R = 0.98). Lumbar spine (L2–4) aBMD was 1.19 ± 0.16 g/cm2 (mean ± SD). Both calibrated and uncalibrated thoracic vBMD correlated positively and significantly with lumbar aBMD, but the relationship was less than unity (R =0.63).
Conclusion
Uncalibrated measures of thoracic spine vBMD obtained from CT scans of the heart may provide clinically relevant information about bone health and osteoporosis/osteopenia risk in recently menopausal women.
Keywords: COMPUTED TOMOGRAPHY, THORACIC VERTEBRAE, LUMBAR SPINE, VOLUMETRIC BONE MINERAL DENSITY
INTRODUCTION
Osteoporosis and coronary artery disease are two common disorders associated with aging. Multiple studies now demonstrate that diagnosis of one of these disorders predicts increased complications and risk of the other1. For example, postmenopausal women with osteoporosis have an approximately four-fold increased risk for cardiovascular events2. Similarly, postmenopausal women with a recent cardiovascular event have a doubled risk of hip fracture3. Therefore, a screening test that could assess simultaneously for both cardiovascular disease and osteoporosis would be useful clinically.
Many individuals receive coronary computed tomography (CT) to screen for coronary calcifications as a marker of coronary artery disease. Assessment of thoracic spine volumetric bone mineral density (vBMD) from images acquired during coronary CT scan is feasible4-7. Current clinical coronary CT scan protocols do not routinely involve the placement and scanning of a calibration standard for the spine, but clinical quantitative CT (QCT) bone density scan protocols to assess vBMD of the lumbar spine acquire images with a calibration standard. Existing investigations have not determined whether thoracic spine vBMD measured with a calibration standard provides a more useful assessment of vBMD than measurement without a calibration standard. Furthermore, it is less clear how values of vBMD obtained from the thoracic spine compare with areal bone mineral density (aBMD) measurements of the lumbar vertebrae using dual-energy X-ray absorptiometry (DEXA)8, a clinically standard measure of bone mass. To answer these questions, we analyzed images of thoracic vertebrae obtained from coronary CT scans performed with a calibration standard and compared vBMD based on calibrated calculation to vBMD based on uncalibrated calculation, then each thoracic vBMD measurement was compared to aBMD values obtained from lumbar spine DEXA.
MATERIALS AND METHODS
Subjects
Women (n = 111) enrolled in the Kronos Early Estrogen Prevention Study (KEEPS) (NCT00154180) at Mayo Clinic (Rochester, MN, IRB protocol # 2241) participated in this study. KEEPS is a multicenter, randomized, double-blind trial to test the hypothesis that early initiation of menopausal hormone treatment reduces progression of cardiovascular disease as measured by changes in carotid intimal medial thickness and coronary arterial calcification9,10. Women were within 6 months to 3 years of menopause and 42–58 years old (Table 1). All women gave informed consent. Women underwent computed tomography to assess calcification of their coronary arteries and DEXA of the lumbar spine prior to randomization to hormone treatments.
Table 1.
Characteristics of the recently menopausal women (n = 111)
| Mean | Standard deviation | Median | First quartile | Third quartile | |
|---|---|---|---|---|---|
| Age (years) | 52.4 | 2.4 | 52 | 51 | 54 |
| Total menopausal month (months) | 18.5 | 9.5 | 18 | 11 | 24 |
| Body mass index (kg/m2) | 27.0 | 4.2 | 26.8 | 24.0 | 30.8 |
| Systolic blood pressure (mmHg)* | 122 | 14 | 121 | 113 | 130 |
| Diastolic blood pressure (mmHg)* | 75 | 8 | 76 | 70 | 81 |
| Total cholesterol (mg/dl) | 218 | 31 | 217 | 197 | 239 |
| Low density lipoprotein cholesterol (mg/dl) | 134 | 30 | 136 | 116 | 159 |
| High density lipoprotein cholesterol (mg/dl) | 61 | 15 | 61 | 50 | 70 |
| Triglyceride (mg/dl) | 96 | 48 | 84 | 64 | 118 |
| Glucose (mg/dl) | 93 | 9 | 92 | 87 | 98 |
n = 110
Volumetric bone mineral density
QCT data were obtained to measure vBMD. At the time of scanning, a calibration phantom (Mindways Software, Austin, TX, USA) was placed in the field of view of the scanner. Thoracic spine vBMD was measured using the Spine Cancer Assessment (SCA) program developed by Biomedical Imaging Resources, Mayo Clinic from images of the thoracic vertebrae captured during the coronary CT scan7. As each dataset was loaded into the SCA program, the application identified the Mindways phantom and determined the correct scaling factor to calibrate the CT values into QCT data. For each scan, an operator identified the superior and inferior endplates of each vertebra in the field of view. Based on the endplates, a central slice was selected as representative of the vertebra. Regions of interest were identified in the mid-vertebra in both the trabecular and central regions7. The SCA application measured both the uncalibrated and calibrated CT data to obtain vBMD estimates.
Areal bone mineral density
Areal bone mineral density (g/cm2) was obtained by DEXA at Mayo Clinic (GE Lunar Prodigy, GE Health Systems) using manufacturer-supplied software for analysis. The average aBMDs from L2 to L4 in the postero-anterior view were used to compare vBMD of thoracic vertebrae.
Statistics
Descriptive statistics were used to summarize the cohort including medians and interquartile ranges for all continuous parameters. Linear relationships between calibrated thoracic vBMD and uncalibrated thoracic vBMD and between thoracic vBMD and lumbar aBMD were assessed using the Spearman correlation. Statistical significance was accepted for p < 0.05. The JMP statistical software package (version 8.0, SAS Institute Inc., Cary, NC, USA) was used for all analyses.
RESULTS
The median (interquartile range) age of women participating in this study was 52.0 (51.0, 54.0) years with a median menopausal age (time past menopause) of 18.0 (11.0, 24.0) months.
As expected from the KEEPS study design to enroll women without pre-existing cardiovascular disease, cardiometabolic parameters were within normative ranges, although the average body mass index placed these women in the overweight category (Table 1).
The average values and distribution of vBMD for trabecular and central regions of thoracic vertebrae 8 (T8) and 9 (T9), using calibrated and uncalibrated values, were similar (Table 2 and Figure 1). Calibrated and uncalibrated vBMD values were significantly and positively correlated and approaching unity for both trabecular and central bone zones of T8 and T9 (R = 0.98 and R = 0.97 for trabecular and central bone, respectively, Figure 2). Standard deviations of the mean values for trabecular and central regions of T8 were constant over the range of vBMD from 100 to 250 mg/cc and were within 10 mg/cc (Figure 3). Similar results were obtained for T9 (data not shown).
Table 2.
Volumetric bone mineral density (vBMD) for trabecular and central regions of the thoracic vertebrae 8 (T8) and 9 (T9). Data are given as mean ± standard deviation
| Calibrated | Non-calibrated | |
|---|---|---|
| T8 vBMD (mg/cc) | ||
| Trabecular | 163.57 ± 28.58† | 157.94 ± 27.55‡ |
| Central | 169.36 ± 38.90† | 161.95 ± 37.48‡ |
| T9 vBMD (mg/cc) | ||
| Trabecular | 167.19 ± 30.21* | 161.57 ± 28.97** |
| Central | 173.18 ± 40.22* | 165.40 ± 37.84** |
n = 111;
n = 110;
n = 106;
n = 107
Figure 1.
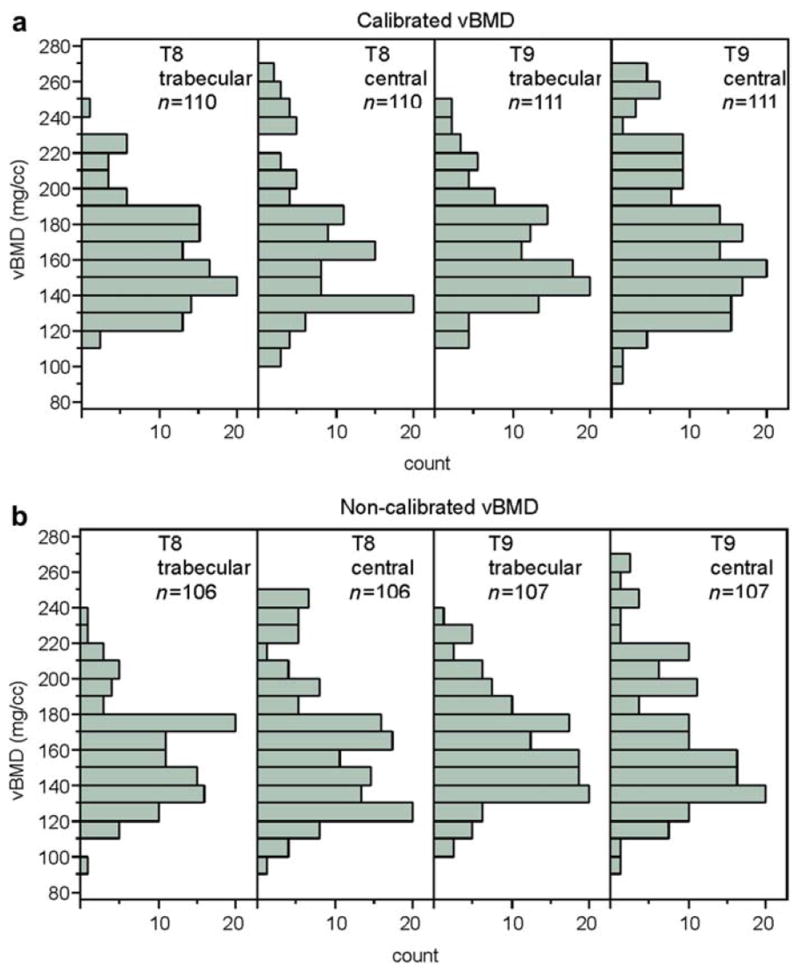
Distributions of volumetric bone mineral density (vBMD) of trabecular and central regions of the thoracic vertebrae 8 (T8) and 9 (T9) using calibrated (upper panels) and non-calibrated (lower panels) calculations in recently menopausal women. Data are shown as number of individuals with each value
Figure 2.
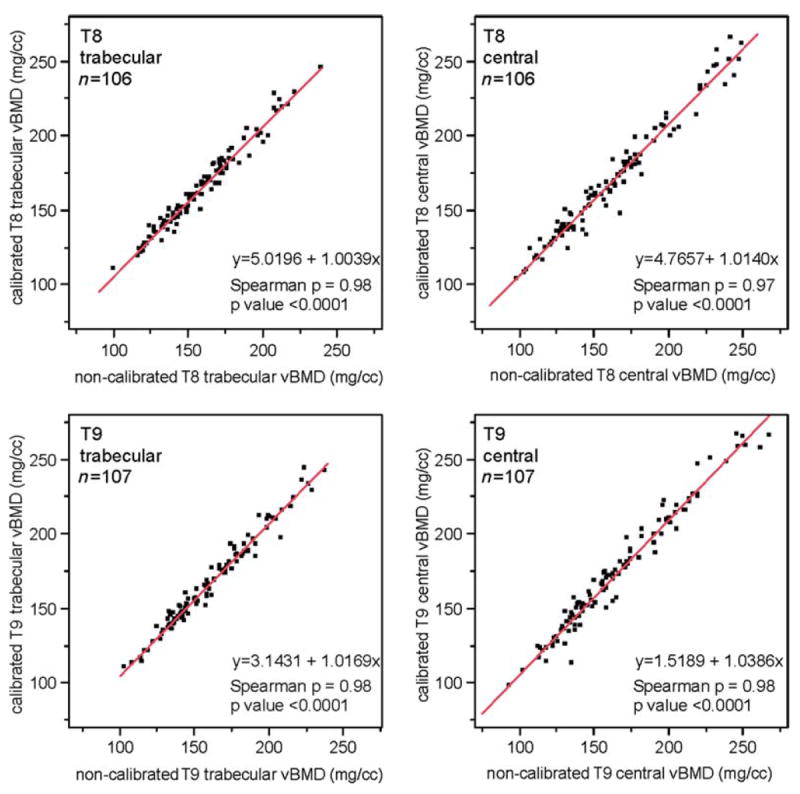
Correlations between calibrated and non-calibrated values of volumetric bone mineral density (vBMD) of trabecular (left panels) and central (right panels) of thoracic vertebrate 8 (T8; upper panels) and 9 (T9; lower panels) obtained from CT scans during assessment of coronary arterial calcification using the Spine Cancer Assessment program in recently menopausal women. Each point represents a value from an individual
Figure 3.

Standard deviations of the means of the calibrated and non-calibrated values of volumetric bone mineral density (vBMD) obtained from CT scans of the heart in recently menopausal women. Each point represents a single woman
The distribution of aBMD for L2–4 is shown in Figure 4. The average aBMD value of L2–4 by DEXA was 1.19 ± 0.16 g/cm2 (mean ± SD); the average T-score was −0.06 ± 1.37. Based on the World Health Organization criteria for osteoporosis, 70.3% of participants had normal bone density (T-score over −1.0), 29.7% had osteopenia (T-score of −2.5 < −1.0), and no participant had osteoporosis (T-score < −2.5).
Figure 4.

Distribution of areal bone mineral density (aBMD) by DEXA in recently menopausal women. Each bar represents the number of individuals with a given value
Both calibrated and uncalibrated vBMD correlated positively and significantly with aBMD, although the relationship was less than unity (Figure 5). The calibrated trabecular vBMD had the strongest correlation coefficient with aBMD of L2–4 by DEXA (R = 0.63).
Figure 5.

Correlations between calibrated (upper panels) and non-calibrated (lower panels) of volumetric bone mineral density (vBMD) (mg/cc) of trabecular and central bone from thoracic vertebrae 8 and 9 (T8 and T9, respectively) from CT scans of the heart with values of areal bone mineral density (aBMD) (g/cm2) of the lumbar spine obtained by DEXA. Each point represents a value from an individual
DISCUSSION
Our analyses confirm the feasibility of measuring vBMD from thoracic vertebral images acquired by coronary CT scan in the KEEPS cohort of healthy, recently postmenopausal women. To evaluate the potential of coronary CT scans as a screening tool for bone health in addition to cardiovascular health, this study evaluates two imaging features. First, it compares calibrated to uncalibrated measures of vBMD. Clinical coronary CT scan protocols do not routinely include a calibration phantom for the spine. As shown in Figure 1, calibrated and uncalibrated data correlate well; however, the slope of the linear regression shows a small bias. Accordingly, the results of bone analyses from uncalibrated CT scans cannot be taken as absolute truth. Routine uncalibrated CT reports the X-ray attenuation coefficients of the data scaled to the Hounsfield scale. The Hounsfield scale is a linear scale with −1000 representative of dry air and 0 representative of pure water at 25°C. Due to environmental factors (as well as local scanner calibration), the Hounsfield values will vary from scanner to scanner and within the same scanner over time. The use of a calibration phantom addresses these issues because each compartment of the phantom contains a known concentration of calcium. After applying the calibration, the QCT data provide true quantitative assessment of bone mass.
Lumbar vBMD by QCT has been measured using internal (muscle and subcutaneous fat) instead of external references such as the calibration phantom we employed11,12. Other investigators have constructed a ‘calibration curve’ from the calibration phantoms of dedicated QCT bone density scans to correlate CT attenuation in Hounsfield units to BMD in milligrams per milliliter13. This ‘calibration curve’ was then used to convert the trabecular bone CT attenuation to BMD estimation. However, the standard clinical QCT bone density assessment still uses an external calibration phantom to decrease variability between measures, especially important for longitudinal assessments.
The second imaging feature that the present study evaluates is relationships between calibrated vBMD or uncalibrated vBMD for both trabecular and central zone thoracic vertebrae, with aBMD of L2–4 by DEXA. A significant and positive correlation was found, with similar results for both the calibrated and uncalibrated analyses. Calibrated trabecular vBMD had the strongest correlation coefficient with aBMD of L2–4 by DEXA. This relationship is consistent with the concept that aBMD reflects the whole vertebral body.
We found that both calibrated and uncalibrated measures of thoracic vBMD moderately correlated with lumbar aBMD, similar to that reported previously6. Our correlation is also similar to that between lumbar aBMD (DEXA) and lumbar vBMD (QCT) (0.596)14, as well as between lumbar aBMD assessed by older methods (dual-photon absorptiometry) and lumbar vBMD by QCT (0.65)15. The moderate degree of correlation between the thoracic vBMD and the lumbar aBMD assessment reflects not only technologic differences between CT and DEXA measures but also known biologic differences in trabecular BMD distribution in the spine. Trabecular BMD gradually increases from the lower lumbar to the first thoracic vertebrae16. Correlations of vBMD within the spine are highest between adjacent vertebrae and moderate between more distant vertebrae16. Other reported methods to assess thoracic vBMD from coronary CT scans have used the average of three vertebrae distal to the left circumflex coronary artery rather than identifying exact vertebrae4,6. Our average values for trabecular vBMD from T8 and T9 were about 13% lower than mean thoracic vBMD for women aged 50 years obtained from the average of three vertebrae from T6–9 (188.6 mg/cc) in another study4, probably reflecting known regional differences in trabecular vBMD, as noted. Although the positive correlation of vBMD with aBMD indicates that a lower thoracic vBMD would suggest lower overall bone health, additional work is required to evaluate the distribution of the vBMD in a young reference population and in a population with vertebral fractures.
Our study subjects were healthy, recently postmenopausal women, reflecting the selection criteria for enrollment in the KEEPS trial. Applicability/validity of uncalibrated vs. calibrated thoracic vBMD assessment from coronary CT scans in other groups including men requires additional investigations. It is known that bone marrow fat, which increases with age, can affect the accuracy of measurements of spine BMD by QCT, but this should not be a significant factor in our results as the women studied were relatively young. None of the women in the present studied had osteoporosis based on DEXA scans, so the spectrum of bone density represented in the group is limited. Others have found that the correlation between lumbar QCT and lumbar DEXA assessment is weaker in osteoporotic women than in younger, healthy, early postmenopausal women17.
It is also important to note that our data were obtained at one time point for each patient in a highly controlled environment. A single scanner was used to obtain all data. In addition, the scanner underwent extensive quality assurance tests to ensure that additional error was not introduced as a result of data acquisition. It is unreasonable to expect this type of rigor or repeated use of a dedicated scanner in routine clinical practice. As such, this work would benefit from a longitudinal study in which patients are scanned multiple times on single and multiple machines. If these results are found to be consistent over time, then the technique would be considered to be robust to the operational environment.
Screening tests are often used to detect asymptomatic diseases including osteoporosis and coronary atherosclerosis that progress silently until an event such as fracture or myocardial infarction occurs. The large body of studies indicate that osteoporosis and coronary atherosclerosis often exist in the same individual, and, whether independent of aging or not, may share common pathophysiologic pathways1. Assessment of the risk of both fracture and myocardial infarction by a single screening test, such as coronary CT scan, would be clinically very useful. In addition, combination screening would likely be attractive to patients and to clinicians since reductions in medical sources of radiation exposure could be accomplished, an area of growing concern in adults as it has been in children18. Similar combination screening by CT for colon polyps and bone mass assessment is being investigated by others13. Our findings demonstrate feasibility that coronary CT scan can assess bone health by uncalibrated thoracic vBMD as well as assess coronary atherosclerosis.
In summary, our investigations show that calculation of vBMD using the Spine Cancer Assessment program applied to uncalibrated CT scans of the heart provides measurements which correlate highly with values derived from measurements using calibration phantoms in a group of healthy, early postmenopausal women. Both measures of thoracic vBMD (calibrated and uncalibrated) correlated with lumbar spine aBMD. These observations imply that measures of thoracic spine vBMD obtained from heart CT scans may provide clinically relevant information about bone health and osteoporosis/osteopenia risk. As mid-thoracic spine and the thoraco-lumbar regions are sites with a high prevalence of vertebral fracture8, it may be reasonable to assess vBMD of thoracic vertebra for early changes by sensitive measures. Repeated measures of vBMD of the thoracic spine and aBMD of the lumbar spine in KEEPS participants over the 4 years of the study will provide valuable information about changes in vBMD in women as they age, effects of hormonal treatments on the thoracic spine, and the relevance of these values to aBMD to provide clinically useful information about bone health with a single screening test.
Acknowledgments
As authors, we gratefully acknowledge all participants in this study and KEEPS study coordinator, Teresa G. Zais (Mayo Clinic center). Dr Miyabara is a visiting scientist from the Tokyo Women’s Medical University.
The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official view of the National Center for Research Resources (NCRR) or the National Institutes of Health (NIH).
Source of funding This work was supported by a grant from Aurora Foundation to the Kronos Longevity Research Institute, 1 UL1 RR024150 from the NCRR, a component of the NIH, and the NIH Roadmap for Medical Research and The Mayo Foundation for Medical Education and Research. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Reengineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov.
Footnotes
Conflict of interest The authors report no conflicts of interest.
References
- 1.den Uyl D, Nurmohamed MT, van Tuyl LH, Raterman HG, Lems WF. (Sub)clinical cardiovascular disease is associated with increased bone loss and fracture risk; a systematic review of the association between cardiovascular disease and osteoporosis. Arthritis Res Ther. 2011;13:R5. doi: 10.1186/ar3224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tanko LB, Christiansen C, Cox DA, Geiger MJ, McNabb MA, Cummings SR. Relationship between osteoporosis and cardiovascular disease in postmenopausal women. J Bone Miner Res. 2005;20:1912–20. doi: 10.1359/JBMR.050711. [DOI] [PubMed] [Google Scholar]
- 3.Sennerby U, Farahmand B, Ahlbom A, Ljunghall S, Michaelsson K. Cardiovascular diseases and future risk of hip fracture in women. Osteoporos Int. 2007;18:1355–62. doi: 10.1007/s00198-007-0386-0. [DOI] [PubMed] [Google Scholar]
- 4.Budoff MJ, Hamirani YS, Ismaeel H, et al. Measurement of thoracic bone mineral density by quantitive CT. Radiology. 2010;257:434–40. doi: 10.1148/radiol.10100132. [DOI] [PubMed] [Google Scholar]
- 5.Wong ND, Kouwabunpat D, Vo AN, et al. Coronary calcium and atherosclerosis by ultrafast computed tomography in asymptomatic men and women: relation to age and risk factors. Am Heart J. 1994;127:422–30. doi: 10.1016/0002-8703(94)90133-3. [DOI] [PubMed] [Google Scholar]
- 6.Lenchik L, Shi R, Register TC, Beck S, Langefeld CD, Carr JJ. Measurement of trabecular bone mineral density in the throacic spine using cardiac gated quantitative computed tomography. J Comput Assist Tomogr. 2004;28:11234–9. doi: 10.1097/00004728-200401000-00023. [DOI] [PubMed] [Google Scholar]
- 7.Miyabara Y, Camp JJ, Holmes D, III, et al. Coronary arterial calcification and thoracic spine mineral density in early menopause. Climacteric. 2011;14:438–44. doi: 10.3109/13697137.2010.537409. [DOI] [PubMed] [Google Scholar]
- 8.Yu W, Gluer C, Grampp S, et al. Spinal bone mineral assessment in postmenopausal women: A comparison between dual X-ray absorptiometry and quantitative computed tomography. Osteoporos Int. 1995;5:433–9. doi: 10.1007/BF01626604. [DOI] [PubMed] [Google Scholar]
- 9.Harman SM, Brinton EA, Cedars M, et al. KEEPS: The Kronos Early Estrogen Prevention Study. Climacteric. 2005;8:3–12. doi: 10.1080/13697130500042417. [DOI] [PubMed] [Google Scholar]
- 10.Miller VM, Black DM, Brinton EA, et al. Using basic science to design a clinical trial: baseline characteristics of women enrolled in the Kronos Early Estrogen Prevention Study (KEEPS) J Cardiovasc Transl Res. 2009;2:228–39. doi: 10.1007/s12265-009-9104-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gudmundsdottir H, Jonsdottir B, Kristinsson S, Johannesson A, Goodenough D, Sigurdsson G. Vertebral bone density in Icelandic women using quantitative computed tomography without an external reference phantom. Osteoporos Int. 1993;3:84–9. doi: 10.1007/BF01623378. [DOI] [PubMed] [Google Scholar]
- 12.Boden SD, Goodenough DJ, Stockham CD, Jacobs E, Dina T, Allman RM. Precise measurement of vertebral bone density using computed tomography without the use of an external reference phantom. J Digit Imaging. 1989;2:31–8. doi: 10.1007/BF03168013. [DOI] [PubMed] [Google Scholar]
- 13.Summers RM, Handwerker LR, Pickhardt PJ, et al. Performance of a previously validated CT colonography computer-aided detection system in a new patient population. Am J Roentgenol. 2008;191:168–74. doi: 10.2214/AJR.07.3354. [DOI] [PubMed] [Google Scholar]
- 14.Kleerekoper M, Nelson DA, Flynn MJ, Pawluszka AS, Jacobsen G, Peterson EL. Comparison of radiographic absorptiometry with dual-energy x-ray absorptiometry and quantitative computed tomography in normal older white and black women. J Bone Miner Res. 1994;9:1745–9. doi: 10.1002/jbmr.5650091111. [DOI] [PubMed] [Google Scholar]
- 15.Sambrook PN, Bartlett C, Evans R, Hesp R, Katz D, Reeve J. Measurement of lumbar spine bone mineral: a comparison of dual photon absorptiometry and computed tomography. Br J Radiol. 1985;58:621–4. doi: 10.1259/0007-1285-58-691-621. [DOI] [PubMed] [Google Scholar]
- 16.Hayashi T, Chen H, Miyamoto K, et al. Analysis of bone mineral density distribution at trabecular bones in thoracic and lumbar vertebrae using X-ray CT images. J Bone Miner Metab. 2011;29:174–85. doi: 10.1007/s00774-010-0204-1. [DOI] [PubMed] [Google Scholar]
- 17.Reinbold WD, Genant HK, Reiser UJ, Harris ST, Ettinger B. Bone mineral content in early-postmenopausal and postmenopausal osteoporotic women: comparison of measurement methods. Radiology. 1986;160:469–78. doi: 10.1148/radiology.160.2.3726129. [DOI] [PubMed] [Google Scholar]
- 18.Goske MJ, Applegate KE, Boylan J, et al. The ‘Image Gently’ campaign: increasing CT radiation dose awareness through a national education and awareness program. Pediatr Radiol. 2008;38:265–9. doi: 10.1007/s00247-007-0743-3. [DOI] [PubMed] [Google Scholar]


