Abstract
Background
The recognition and assessment of psychomotor retardation may have implications for better definition of the clinical phenotypes of depression. The aim of this study was to assess the clinical correlates of psychomotor retardation endorsed at any time during the patients lifetime (LPR).
Methods
The study sample included 291 patients with non-psychotic Major Depressive Disorder (MDD) participating in the clinical trial, “Depression: The Search for Treatment-relevant Phenotypes.” Psychomotor Retardation was measured using a factor derived from the Mood Spectrum Self-Report (MOODS-SR) assessment.
Using a pre-defined cut-off score on the lifetime psychomotor retardation (LPR) factor of the MOODS-SR, participants were classified into high and low scorers. Logistic regression analysis was used to evaluate the relationship between LPR and subthreshold bipolarity.
Results
Compared to low scorers, participants with high scores on LPR factor had greater severity of depression and more bipolarity indicators.
Conclusions
The MOODS-SR appears to be helpful to identify clinical phenotypes of unipolar depression and to highlight the usefulness of a lifetime approach to the assessment of psychopathology in the characterisation of patients with unipolar depression.
Keywords: Retardation, phenotype, major depression
INTRODUCTION
There is growing evidence that the diagnosis of major depressive disorder, as defined in the DSM-IV, is heterogeneous in nature and includes subgroups that exhibit different responses to treatment (Akiskal et al., 2000; Angst et al., 2003; Zimmermann et al, 2009). Thus, contemporary clinical research is focusing on the need to identify specific subgroups among patients participating in clinical trials (Targum et al., 2008; Papakostas and Fava et al., 2009) or neuroimaging and genetic investigations (Keener & Phillips, 2007; Bearden & Freimer, 2006). For this reason, attention has been directed to the recognition of specific psychopathological dimensions or symptom clusters that may help to identify homogeneous and clinically useful groups of patients (Cassano et al, 2008; Gelenberg et al., 2008, Hasler et al, 2004).
Among a number of psychopathological dimensions, psychomotor retardation has proven to have both diagnostic and prognostic value in major depression (Sabin & Sackeim, 1997; Lecubrier, 2006). In DSM-IV-TR, the presence of "marked psychomotor retardation or agitation" is included among the criterion symptoms required for the diagnosis of a depressive episode and psychomotor disturbances are one of the main characteristics of the depressive subtype with melancholic features.
Psychomotor retardation usually characterises the depressive phase of bipolar depression, (so-called “shutdown depression”), and has been associated with “atypical” symptoms of depression, such as hypersomnia and hyperphagia (Goodwin & Jamison, 1990; Mitchell et al, 2001). Moreover, several authors have suggested that psychomotor retardation may represent a marker for bipolarity in patients with MDD (Parker et al., 2000; Akiskal. et al., 2000; Mitchell et al.,2001; Cassano et al.,2004; Akiskal et al.,2005; Benazzi & Akiskal, 2008). Thus, it appears that psychomotor retardation may be a primary component of a specific phenotype of unipolar depression with bipolar features, characterised by more severe symptoms and poorer response to treatment, especially when associated with early age at onset, higher tendency to recurrences, previous mixed depressive episodes, and a family loading for bipolarity (Akiskal et al.,2000; Cassano et al., 2004; Benazzi & Akiskal, 2008). This phenotype could be located along a continuum that embraces unipolar and bipolar disorders using a unitary approach, harkening back to a Kraepelinian view of manic-depressive illness (Kraepelin, 1921).
Assessment of psychomotor retardation has been typically conducted using interviewer-rated scales based on observable signs and symptoms (Widlocher, 1983; Parker and Hadzi-Pavlovic; 1996; Sobin et al., 1998); in a recent factor analysis of the depressive spectrum symptoms of the Mood Spectrum Self-Report Questionnaire (MOODS-SR), we identified a Lifetime Psychomotor Retardation (LPR) factor. As shown in Table 1, the MOODS-SR LPR factor includes 14 items from both the cognitive and motor domain and their impact on performance of daily activities (Cassano et al., 2008).
Table 1.
Frequency of endorsement of Items of the Lifetime Psychomotor Retardation factor.
| Item | Item endorsement |
|---|---|
| 58. difficulty starting to do anything | 0.752 |
| 63. trouble getting out of bed in the morning | 0.740 |
| 62. passive, sluggish | 0.715 |
| 65. fatigued weak, or tired for the smallest task | 0.687 |
| 101. using sleep as an escape | 0.671 |
| 91. trouble thinking or concentrating | 0.670 |
| 92. mentally dull or confused | 0.633 |
| 90. difficulty making even minor decisions | 0.615 |
| 89. your housework/performance deteriorated | 0.608 |
| 61. time as passing very slowly, hanging heavy | 0.599 |
| 59. physically "slowed down" | 0.581 |
| 64. difficulty in taking care of yourself | 0.576 |
| 60. speech or thinking seemed slowed down | 0.513 |
| 132. difficulty working in the early morning | 0.486 |
Like that of many other researchers and clinicians, our evaluation of patients with mood disorders gives considerable weight to the assessment of the lifetime symptoms and course of the disease. Indeed, the lifetime phenomenology very often inform our diagnosis and treatment decisions at least as much as those of the current episode.
The present paper aims to provide evidence that the lifetime assessment of psychomotor retardation in patients with non-psychotic unipolar depression, contributes to the characterization of a phenotype of unipolar depression with specific clinical features and supports the view that LPR is an indicator of a bipolar diathesis in patients with a lifetime history of unipolar depression.
METHODS
Participants
This study was carried out in the Depression and Manic-Depression Prevention Program at the Western Psychiatric Institute and Clinic of the University of Pittsburgh Medical Center and the outpatient psychiatric clinic of the Santa Chiara Hospital of the University of Pisa. Patients aged between 18 and 66 years (inclusive) meeting DSM-IV criteria for a non-psychotic major depressive episode, determined using the SCID interview, and with a Hamilton Rating Scale for Depression, (HRSD), score>=15 were eligible for a clinical trial focused on the identification of treatment-relevant phenotypes of major depression.
Exclusion criteria were: a primary diagnosis of schizophrenia, schizoaffective disorder, bipolar I or II disorder, anorexia or bulimia, meeting criteria for antisocial personality disorder or current alcohol or substance abuse. Individuals with severe, uncontrolled medical illness, those who had been unresponsive to an adequate trial of escitalopram or interpersonal psychotherapy in the current episode and women who were unwilling to practice an acceptable form of birth control were also excluded. Participants were randomly assigned to a treatment sequence that began with pharmacotherapy (SSRI–escitalopram) or interpersonal psychotherapy (IPT) and received the augmentation with the second treatment if they did not respond to the first treatment.
Study procedures were approved by the Institutional Review Board of the University of Pittsburgh and the Ethics Committee of the University of Azienda Ospedaliero-Universitaria of Pisa. All patients signed a written informed consent after receiving a complete description of the study and having an opportunity to ask questions. The study design and protocol are described in detail in Frank et al., 2008 and 2010.
Instruments
Study participants were administered the lifetime Mood Spectrum Self-Report (MOODS-SR) at study baseline. The MOODS-SR includes 161 items coded as present/absent, for one or more periods of at least 3 to 5 days in their lifetime. For some questions exploring temperamental features or the occurrence of specific events, duration is not specified because it would not be applicable. Items are organized into 3 manic/hypomanic and 3 depressive domains, each exploring mood, energy, and cognition, plus a domain that explores disturbances in rhythmicity (e.g., changes in mood, energy, and physical well-being according to the weather, the season, and the phase of menstrual cycle) and vegetative functions (including sleep, appetite and sexual function). The sum of the scores on the 3 manic/hypomanic domains constitutes the “manic component” (62 items) and that of the 3 depressive domains the “depressive component” (63 items). The rhythmicity and vegetative functions domain includes 29 items.
Separate factor analyses of the depressive and manic components of MOODS-SR identified 6 depressive factors (Cassano et al, 2008 (a)) and 9 manic-hypomanic factors (Cassano et al, 2008 (b)). “Depressive Mood,” “Psychomotor Retardation,” “Suicidality,” “Drug/illness-related Depression,” “Psychotic Features,” and “Neurovegetative Symptoms” constitute the depressive factors. The factors of mania/hypomania are: “Psychomotor Activation,” “Creativity,” “Mixed Instability,” “Sociability/Extraversion.” “Spirituality/Mysticism/Psychoticism,” “Mixed Irritability,” “Inflated Self-esteem,” “Euphoria,” and “Wastefulness/Recklessness”.
The last-month version of the MOODS-SR, that includes the same items as the lifetime version but refers to the month preceding the index assessment, was also administered at study baseline.
Clinical variables including duration of illness, age at onset of depression, number of depressive episodes, history of suicide attempts (coded as present or absent) were collected at baseline as part of the SCID interview. Severity of depression was rated using both a 17-item and a 25-item version of Hamilton Rating Scale for Depression (HRSD-17; Hamilton et al.,1960; Thase et al., 1983). Family history of psychiatric disorders was collected through a chart review by trained clinicians and coded as present or absent.
Statistical analyses
In order to determine the optimal psychomotor retardation threshold discriminating unipolar from bipolar patients we examined data from a separate sample of 249 patients with unipolar disorder (% F 83.9, mean age=38.0, SD=12.2) and 306 with bipolar disorder (% F 61.4, mean age=45.5, SD=14.8) recorded in the Italian and US spectrum project databases.
Using a ROC analysis, we set this threshold at ≥11 items endorsed; (sensitivity = 52.6%, specificity = 72.9%, area under ROC curve = 0.68, 95% Confidence Interval (CI): 0.63-0.72). Using this cut-off score on the LPR factor, we categorized our study participants into low and high scorers. Chi-square tests or Mann-Whitney tests were used to compare high and low scorers on clinical variables and on the mean scores on the self-report spectrum factors. Logistic regression analysis was carried out to analyse the relationship between LPR factor (coded as high/low) and various indicators of bipolarity, and manic/hypomanic component of the MOODS-SR factors, controlling for baseline severity of depression.
All statistical analyses were carried out with SPSS, version 15.0 (SPSS, Inc. Chicago 2007).
RESULTS
Of the 291 study participants, 286 (% F 71.7, mean age=39.6, SD=12.0) completed the MOODS-SR at baseline. The mean lifetime score on LPR factor was 8.5 (SD=4.1). Using the cut-off score of 11, subjects were classified as low (N=176, 61.5%) and high (N=110, 38.5%) LPR scorers.
LPR and indicators of bipolarity
Compared with low scorers, high LPR scorers had a longer duration of illness, an earlier age of onset, more depressive episodes and were significantly more likely to have a history of suicide attempts (Table 2). After adjusting for baseline severity of depression, gender and age, recurrent depression (OR=2.16 95% CI 1.08–4.31) and age of onset (OR=0.95, 95% CI 0.93–0.98) were significantly associated with being in the high LPR factor group in a logistic regression model (Hosmer & Lemeshow test: p=0.640). Patients with high LPR scores exhibited also higher scores on all lifetime mania-hypomania spectrum factors (except for the sociability/extraversion factor) (Figure 1). Three mania-hypomania spectrum factors were significantly and independently associated with LPR in logistic regression models after controlling for baseline severity of depression (Hosmer & Lemeshow test: p=0.996). These included “Mixed Irritability” (OR=1.25, 95% CI: 1.04–1.50), “Creativity” (OR=1.17, 95% CI: 1.05–1.30) and “Mixed Instability” (OR=1.42, 95% CI: 1.18–1.71). A negative association was found with “Sociability-Extraversion” (OR=0.84, 95% CI: 0.71–0.99). Assuming that LPR scores increase with age, we compared the proportion of high/low LPR scorers in the three age groups defined by the tertiles of distribution. We found that LPR scores were unrelated to age (χ2= 0.98, p=0.612).
Table 2.
Clinical correlates of the LPR factor
| LPR (N = 176) < 11 | LPR≥11 (N = 110) | Mann-Whitney U test / Chi-square test | P | |
|---|---|---|---|---|
| Age at onset of depression, mean (SD) | 30.6 (12.9) | 23.2 (11.8) | −4.66 | <0.001 |
| Duration of illness (years), mean (SD) | 9.7 (11.5) | 15.2 (13.2) | −4.26 | <0.001 |
| Number of episodes, median | 2 | 3 | −4.00 | <0.001 |
| History of suicide attempts, N (%) | 17 (9.8) | 22 (20.0) | 5.95 | 0.015 |
| Family history for psychiatric disorders, N (%) | 78 (48.4) | 32 (25.6) | 15.5 | <0.001 |
Figure 1.
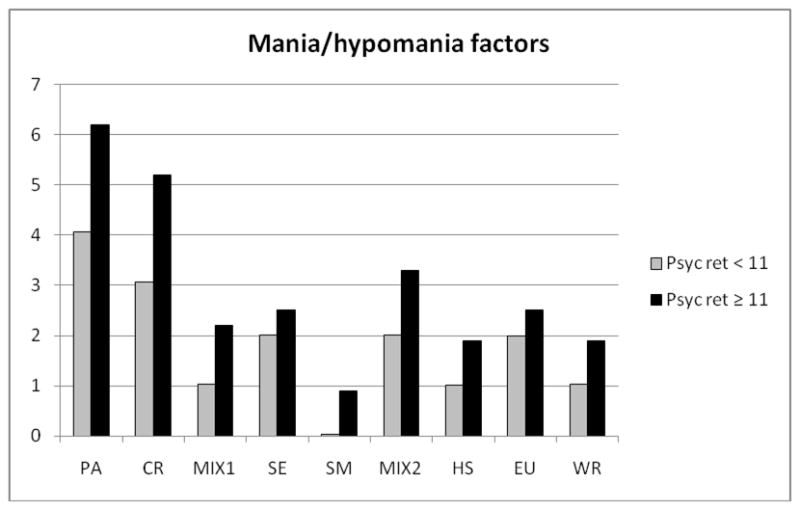
LPR factor in mania-hypomania component
Mania/hypomania factors: PA=Psychomotor Activation, CR=Creativity, MIX1=Mixed Instability, SE=Sociability/Extraversion, SM=Spirituality/Mysticism/Psychoticism, MIX2=Mixed Irritability, HS=Inflated self-esteem, EU=Euphoria, WR=Wastefulness/Recklessness.
Finally, we examined the relationship between lifetime LPR scores and last-month LPR scores. On average, participants endorsed 7.5 (SD=4.2) LPR items in the month preceding the baseline assessment (range 0-14). The difference between the lifetime and the last-month score was 1.1 (SD=3.6), z (Wilcoxon test) = 5.68, p<0.001.
DISCUSSION
Our results, based on a spectrum approach to the assessment of psychopathology (Cassano et al., 2004), indicate that lifetime psychomotor retardation is associated with greater lifetime severity of depression and more indicators of bipolarity. In particular, patients with high levels of psychomotor retardation exhibited an earlier age at onset, longer duration of illness, higher frequency of episodes, more lifetime suicide attempts and a positive family history of psychiatric disorders. These patients were also more likely to endorse subthreshold bipolar features such as “Mixed Irritability”, “Mixed Instability” and “Creativity.” Moreover such associations appear to be stable even when adjusting for baseline severity of depression. Contrary to our hypothesis, psychomotor retardation was unrelated to age (younger, middle-aged, older). However, other reports indicate that psychomotor retardation is higher in elderly depressed patients compared with middle-aged patients (Brodaty, 1997; Sobin and Sackeim, 1997). Because our study includes adults (age 18-66 years) but not elderly patients, we failed to find an association between age and LPR scores.
Our study builds upon prior work showing that retardation is an indicator of clinical severity of depression, a validator’ of a bipolar diathesis in unipolar patients (Benazzi & Akiskal, 2008; Mitchell et al., 2008; Akiskal et al., 2005; Akiskal et al., 2000; Parker et al., 2000; Mitchell et al, 2001; Cassano et al 2004; Fink et al.,2007; Parker et al. 2007; Benazzi, 2002; Angst et al., 2008; Mitchell et al., 2001; Parker et al., 2000; Himmelhoch, 1998) and is a non-specific predictor of delayed response to treatment with either interpersonal psychotherapy or SSRI pharmacotherapy (Frank et al., 2010). Future studies could profitably be directed toward studying the comparative effect of serotonergic, noradrenergic and dopaminergic antidepressants in patients characterized along this dimension.
The present study has a number of limitations. The lifetime version of the MOODS-SR has the advantage of looking at MDD as a lifetime disorder, giving appropriate weight to the complete lifetime picture. However, each item is considered as endorsed if it has been present at any time during the subject s lifetime. Hence, the instrument does not permit one to evaluate whether the LPR factor items have ever been present as a cluster during the same time period. Moreover, the retrospective assessment of symptoms and behaviors carries the possibility of recall bias. However, concern about such bias is somewhat mitigated by the fact that the mean difference between the number of LPR items endorsed in the lifetime and in the last month is 1.1 (SD=3.6), suggesting that the majority of PR symptoms were also experienced during the current episode. The family history was collected through a chart review and not through a standardized interview. Therefore, we could not investigate in deeper detail the presence or absence of specific disorders in the family of the patient.
Concluding Remarks
The lifetime presence of psychomotor retardation correlates with a more pernicious clinical course and with the endorsement characteristics of mania/hypomania in patients with unipolar disorder.
A spectrum approach to the assessment of psychopathology may offer clinicians a tool to reliably identify subgroups of patients with unipolar disorder and may have important implications for research on the neurobiology, genetics, and treatment of unipolar depression.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Akiskal HS. The dark side of bipolar depression in its pleomorphic expressions. J Affect Disord. 2005;84:107–15. doi: 10.1016/j.jad.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 2.Akiskal HS, Bourgeois ML. Re-evaluating the prevalence of and diagnostic composition within the broad clinical spectrum of bipolar disorders. J Affect Disord. 2000;59(Suppl 1):S5–S30. doi: 10.1016/s0165-0327(00)00203-2. [DOI] [PubMed] [Google Scholar]
- 3.Angst J, Gamma A, Benazzi F, Ajdacic V, Eich D, Rossler W. Toward a redefinition of subthreshold bipolarity: epidemiology and proposed criteria for bipolar- II, minor bipolar disorders and hypomania. J Affect Disord. 2003;73(1–2):133–146. doi: 10.1016/s0165-0327(02)00322-1. [DOI] [PubMed] [Google Scholar]
- 4.Angst J, Gamma A, Benazzi F, Ajdacic V, Rössler W. Does psychomotor agitation in major depressive episodes indicate bipolarity? Evidence from the Zurich Study. Eur Arch Psychiatry Clin Neurosci. 2009 Feb;259(1):55–63. doi: 10.1007/s00406-008-0834-7. [DOI] [PubMed] [Google Scholar]
- 5.Bearden CE, Freimer NB. Endophenotypes for psychiatric disorders: ready for primetime? Trends Genet. 2006;22(6):306–313. doi: 10.1016/j.tig.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 6.Benazzi F. Psychomotor changes in melancholic and atypical depression: unipolar and bipolar-II subtypes. Psychiatry Res. 2002;112(3):211–20. doi: 10.1016/s0165-1781(02)00241-x. [DOI] [PubMed] [Google Scholar]
- 7.Benazzi F, Akiskal HS. How best to identify a bipolar-related subtype among major depressive patients without spontaneous hypomania: superiority of age at onset criterion over recurrence and polarity? J Affect Disord. 2008;107(1–3):77–88. doi: 10.1016/j.jad.2007.07.032. [DOI] [PubMed] [Google Scholar]
- 8.Benvenuti A, Rucci P, Miniati M, Papasogli A, Fagiolini A, Cassano GB, Swartz H, Frank E. Treatment-emergent mania/hypomania in unipolar patients. Bipolar Disord. 2008;10(6):726–32. doi: 10.1111/j.1399-5618.2008.00613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brodaty H, Luscombe G, Parker G, Wilhelm K, Hickie I, Austin MP, Mitchell P. Increased rate of psychosis and psychomotor change in depression with age. Psychol Med. 1997;27(5):1205–13. doi: 10.1017/s0033291797005436. [DOI] [PubMed] [Google Scholar]
- 10.Cassano GB, Dell'Osso L, Frank E, Miniati M, Fagiolini A, Shear MK, Pini S, Maser J. The bipolar spectrum: a clinical reality in search of diagnostic criteria and an assessment methodology. J Affect Disord. 1999;54(3):319–28. doi: 10.1016/s0165-0327(98)00158-x. [DOI] [PubMed] [Google Scholar]
- 11.Cassano GB, Benvenuti A, Miniati M, Calugi S, Mula M, Maggi L, Rucci P, Fagiolini A, Perris F, Frank E. The factor structure of lifetime depressive spectrum in patients with unipolar depression. J Affect Disord. 2009;115(1–2):87–99. doi: 10.1016/j.jad.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cassano GB, Mula M, Rucci P, Miniati M, Frank E, Kupfer DJ, Oppo A, Calugi S, Maggi L, Gibbons R, Fagiolini A. The structure of lifetime manic-hypomanic spectrum. J Affect Disord. 2009;112(1–3):59–70. doi: 10.1016/j.jad.2008.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cassano GB, Rucci P, Frank E, Fagiolini A, Dell'Osso L, Shear MK, Kupfer DJ. The mood spectrum in unipolar and bipolar disorder: arguments for a unitary approach. Am J Psychiatry. 2004;161(7):1264–9. doi: 10.1176/appi.ajp.161.7.1264. [DOI] [PubMed] [Google Scholar]
- 14.Coryell W, Leon AC, Turvey C, Akiskal HS, Mueller T, Endicott J. The significance of psychotic features in manic episodes: a report from the NIMH collaborative study. J Affect Disord. 2001;67(1–3):79–88. doi: 10.1016/s0165-0327(99)00024-5. [DOI] [PubMed] [Google Scholar]
- 15.Dell'Osso L, Rucci P, Cassano GB, Maser JD, Endicott J, Shear MK, Sarno N, Saettoni M, Grochocinski VJ, Frank E. Measuring social anxiety and obsessive-compulsive spectra: comparison of interviews and self-report instruments. Compr Psychiatry. 2002;43(2):81–7. doi: 10.1053/comp.2002.30795. [DOI] [PubMed] [Google Scholar]
- 16.Fink M, Taylor MA. Resurrecting melancholia. Acta Psychiatr Scand. 2007;(Suppl):14–20. doi: 10.1111/j.1600-0447.2007.00958.x. [DOI] [PubMed] [Google Scholar]
- 17.Frank E, Cassano GB, Rucci P, Fagiolini A, Maggi L, Kraemer HC, Kupfer DJ, Pollock B, Bies R, Nimgaonkar V, Pilkonis P, Shear MK, Thompson WK, Grochocinski VJ, Scocco P, Buttenfield J, Forgione RN. Addressing the challenges of a cross-national investigation: lessons from the Pittsburgh-Pisa study of treatment-relevant phenotypes of unipolar depression. Clin Trials. 2008;5(3):253–61. doi: 10.1177/1740774508091965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Frank E, Cassano GB, Rucci P, Thompson WK, Kraemer HC, Fagiolini A, Maggi L, Kupfer DJ, Shear MK, Houck PR, Calugi S, Grochocinski VJ, Scocco P, Buttenfield J, Forgione RN. Predictors and Moderators of Time to Remission of Major Depression with Interpersonal Psychotherapy and SSRI Pharmacotherapy. Psychol Med. 2010;12:1–12. doi: 10.1017/S0033291710000553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gelenberg AJ, Thase ME, Meyer RE, Goodwin FK, Katz MM, Kraemer HC, Potter WZ, Shelton RC, Fava M, Khan A, Trivedi MH, Ninan PT, Mann JJ, Bergeson S, Endicott J, Kocsis JH, Leon AC, Manji HK, Rosenbaum JF. The history and current state of antidepressant clinical trial design: a call to action for proof-of-concept studies. J Clin Psychiatry. 2008;69(10):1513–28. doi: 10.4088/jcp.v69n1001. [DOI] [PubMed] [Google Scholar]
- 20.Goodwin FK, Jamison KR. Manic-depressive illness. Oxford University Press; New York: 1990. [Google Scholar]
- 21.Goodwin FK, Jamison KR. Manic-Depressive Illness: Bipolar Disorders and Recurrent Depression. Oxford University Press; New York: 2007. [Google Scholar]
- 22.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hantouche EG, Akiskal HS. Bipolar II vs. unipolar depression: psychopathologic differentiation by dimensional measures. J Affect Disord. 2005;84(2–3):127–32. doi: 10.1016/j.jad.2004.01.017. [DOI] [PubMed] [Google Scholar]
- 24.Hasler G, Drevets WC, Manji HK, Charney DS. Discovering endophenotypes for major depression. Neuropsychopharmacol. 2004;29:1765–81. doi: 10.1038/sj.npp.1300506. [DOI] [PubMed] [Google Scholar]
- 25.Himmelhoch JM. Social anxiety, hypomania and the bipolar spectrum: data, theory and clinical issue. J Affect Disord. 1998;50:203–213. doi: 10.1016/s0165-0327(98)00139-6. [DOI] [PubMed] [Google Scholar]
- 26.Kawahara Y, Kawahara H, Kaneko F, Tanaka M. Long-term administration of citalopram reduces basal and stress-induced extracellular noradrenaline levels in rat brain. Psychopharmacology (Berl) 2007;194(1):73–81. doi: 10.1007/s00213-007-0826-8. [DOI] [PubMed] [Google Scholar]
- 27.Keener MT, Phillips ML. Neuroimaging in bipolar disorder: a critical review of current findings. Curr Psychiatry Rep. 2007;9(6):512–20. doi: 10.1007/s11920-007-0070-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kraepelin E. Manic depressive insanity and paranoia. E. Livingstone; Edinburgh: 1921. [Google Scholar]
- 29.Malhi GS, Parker GB, Greenwood J. Structural and functional models of depression: from sub-types to substrates. Acta Psychiatr Scand. 2005;111:94–105. doi: 10.1111/j.1600-0447.2004.00475.x. [DOI] [PubMed] [Google Scholar]
- 30.Kraemer HC. DSM categories and dimensions in clinical and research contexts. Int J Methods Psychiatr Res. 2007;16(Suppl 1):S8–S15. doi: 10.1002/mpr.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lecrubier Y. Physical components of depression and psychomotor retardation. J Clin Psychiatry. 2006;67(Suppl 6):23–6. [PubMed] [Google Scholar]
- 32.Mitchell PB, Wilhelm K, Parker G, Austin MP, Rutgers P, Malhi GS. The clinical features of bipolar depression: a comparison with matched major depressive disorder patients. J Clin Psychiatry. 2001;62:212–216. [PubMed] [Google Scholar]
- 33.Mitchell PB, Goodwin GM, Johnson GF, Hirschfeld RM. Diagnostic guidelines for bipolar depression: a probabilistic approach. Bipolar Disord. 2008;101:44–52. doi: 10.1111/j.1399-5618.2007.00559.x. [DOI] [PubMed] [Google Scholar]
- 34.Papakostas GI, Fava M. Does the probability of receiving placebo influence clinical trial outcome? A meta-regression of double-blind, randomized clinical trials in MDD. Eur Neuropsychopharmacol. 2009;19:34–40. doi: 10.1016/j.euroneuro.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 35.Parker G. Defining melancholia: the primacy of psychomotor disturbance. Acta Psychiatr Scand Suppl. 2007;433:21–30. doi: 10.1111/j.1600-0447.2007.00959.x. [DOI] [PubMed] [Google Scholar]
- 36.Parker G, Hadzi-Pavlovic D, Wilhelm K, Austin MP, Mason C, Samuels A, Mitchell P, Eyers K. Defining the personality disorders: description of an Australian database. Aust N Z J Psychiatry. 1996;30(6):824–33. doi: 10.3109/00048679609065051. [DOI] [PubMed] [Google Scholar]
- 37.Parker G, Roy K, Wilhelm K, Mitchell P, Hadzi-Pavlovic D. The nature of bipolar depression: implications for the definition of melancholia. J Affect Disord. 2000;59(3):217–24. doi: 10.1016/s0165-0327(99)00144-5. [DOI] [PubMed] [Google Scholar]
- 38.Shear MK, Frank E, Rucci P, Fagiolini A, Grochocinski VJ, Houck P, Cassano GB, Kupfer DJ, Endicott J, Maser JD, Mauri M, Banti S. Panic-agoraphobic spectrum: reliability and validity of assessment instruments. J Psychiatr Res. 2001;35(1):59–66. doi: 10.1016/s0022-3956(01)00002-4. [DOI] [PubMed] [Google Scholar]
- 39.Schrijvers D, Hulstijn W, Sabbe BG. Psychomotor symptoms in depression: a diagnostic, pathophysiological and therapeutic tool. J Affect Disord. 2008;109:1–20. doi: 10.1016/j.jad.2007.10.019. [DOI] [PubMed] [Google Scholar]
- 40.Sobin C, Sackeim HA. Psychomotor symptoms of depression. Am J Psychiatry. 1997;154:4–17. doi: 10.1176/ajp.154.1.4. [DOI] [PubMed] [Google Scholar]
- 41.Sobin C, Mayer L, Endicott J. The motor agitation and retardation scale: a scale for the assessment of motor abnormalities in depressed patients. J Neuropsychiatry Clin Neurosci. 1998;10(1):85–92. doi: 10.1176/jnp.10.1.85. [DOI] [PubMed] [Google Scholar]
- 42.Szabo ST, de Montigny C, Blier P. Progressive attenuation of the firing activity of locus coeruleus noradrenergic neurons by sustained administration of selective serotonin reuptake inhibitors. Int J Neuropsychopharmacol. 2000;3:1–11. doi: 10.1017/S1461145700001772. [DOI] [PubMed] [Google Scholar]
- 43.Thase ME, Hersen M, Bellack AS, Himmelhoch JM, Kupfer DJ. Validation of a Hamilton subscale for endogenomorphic depression. J Affect Disord. 1983;5(3):267–78. doi: 10.1016/0165-0327(83)90050-2. [DOI] [PubMed] [Google Scholar]
- 44.Targum SD, Pollack MH, Fava M. Redefining affective disorders: relevance for drug development. CNS Neurosci Ther. 2008;14:2–9. doi: 10.1111/j.1527-3458.2008.00038.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Widlocher DJ. Psychomotor retardation: clinical, theoretical, and psychometric aspects. Psychiatr Clin North Am. 1983;6(1):27–40. [PubMed] [Google Scholar]
- 46.Zimmermann P, Brückl T, Nocon A, Pfister H, Lieb R, Wittchen H-U, Holsboer F, Angst J. Heterogeneity of DSM-IV Major Depressive Disorder as a Consequence of Subthreshold Bipolarity. Arch Gen Psychiatry. 2009;66(12):1341–1352. doi: 10.1001/archgenpsychiatry.2009.158. [DOI] [PubMed] [Google Scholar]


