Abstract
Objective
To determine the impact of a video on preferences for the primary goal of care.
Design, subjects, and intervention
Consecutive subjects 65 years of age or older (n=101) admitted to two skilled nursing facilities (SNFs) were randomized to a verbal narrative (control) or a video (intervention) describing goals-of-care options. Options included: life-prolonging (i.e., cardiopulmonary resuscitation), limited (i.e., hospitalization but no cardiopulmonary resuscitation), or comfort care (i.e., symptom relief).
Main measures
Primary outcome was patients' preferences for comfort versus other options. Concordance of preferences with documentation in the medical record was also examined.
Results
Fifty-one subjects were randomized to the verbal arm and 50 to the video arm. In the verbal arm, preferences were: comfort, n=29 (57%); limited, n=4 (8%); life-prolonging, n=17 (33%); and uncertain, n=1 (2%). In the video arm, preferences were: comfort, n=40 (80%); limited, n=4 (8%); and life-prolonging, n=6 (12%). Randomization to the video was associated with greater likelihood of opting for comfort (unadjusted rate ratio, 1.4; 95% confidence interval [CI], 1.1–1.9, p=0.02). Among subjects in the verbal arm who chose comfort, 29% had a do-not-resuscitate (DNR) order (κ statistic 0.18; 95% CI–0.02 to 0.37); 33% of subjects in the video arm choosing comfort had a DNR order (κ statistic 0.06; 95% CI–0.09 to 0.22).
Conclusion
Subjects admitted to SNFs who viewed a video were more likely than those exposed to a verbal narrative to opt for comfort. Concordance between a preference for comfort and a DNR order was low. These findings suggest a need to improve ascertainment of patients' preferences.
Trial Registration: Clinicaltrials.gov Identifier: NCT01233973.
Introduction
Elderly patients admitted to skilled nursing facilities (SNFs), are at a vulnerable point in their medical care.1 These patients are recuperating from an acute illness and often have underlying complex chronic medical conditions. At the same time, SNF providers are likely to be unfamiliar with these patients' medical history and values. The hazards resulting from discontinuity of care between the hospital and SNF setting are well-described.2–5
Emerging health policy initiatives are increasingly focused on reducing avoidable, costly and burdensome rehospitalizations of older patients, particularly when patients' primary goal of care is comfort.6,7 Optimizing advance care planning by ascertaining the patient's care preferences presents a key opportunity to promote goal-directed care that avoids unwanted and costly treatments.8
Over the last decade, an expanding body of evidence suggests that video decision aids help patients make better informed decisions by clarifying treatment options for a variety of life-limiting conditions including cancer and advanced dementia.9–13 Video enhances communication beyond the usual ad hoc verbal approaches to advance care planning by providing realistic and standardized depictions of treatment options. To date, video support tools for advance care planning have not been studied in the post-acute care setting where vulnerable older patients are often required to make value-laden decisions about treatment options.
To address this gap, we conducted a pilot randomized controlled trial of using a goals-of-care video for elderly patients admitted to a SNF after an acute hospitalization. We hypothesized that compared to subjects randomized to a verbal description of the goals of care, those viewing the video decision aid would be more likely to opt for treatments that align with comfort as the primary goal of care. An additional aim was to examine the correlation between a stated preference for comfort with the presence of a do-not-resuscitate (DNR) order in the medical record.
Methods
Subjects
The protocol was approved by the Partners Institutional Review Board and all subjects provided written informed consent. Subjects were recruited from a consecutive sample of patients admitted from acute hospitals to one of two SNFs in the greater Boston area. Both SNFs were located within nursing homes; one facility had 164 beds and the other had 190 beds.
Recruitment occurred between July 1, 2010 and February 28, 2011. At the time of admission, all patients who were 65 years of age or older and English-speaking were identified by the SNF admitting clerk and given a flier outlining the study. Patients were then asked by a SNF staff member (e.g., nurse or social worker) if they were interested in participating in the study. The final eligibility of patients who expressed a willingness to participate was then determined by a research assistant based on an assessment of their cognitive status performed within 72 hours of SNF admission. Patients were excluded if they had a Short Portable Mental Status Questionnaire (SPMSQ) score of less than 7.14
Design
All interviews were conducted in-person by one of two members of the research team (either A.E.V. or E.M.). Subjects underwent a baseline interview within 72 hours of admission to ascertain age, self-reported race, gender, religion, educational status, marital status, self-rated health status (excellent, very good, good, fair, or poor), and self-reported completion of advance directives (designated health care proxy or living will).
Immediately after the baseline interview, subjects were randomized into one of two decision-making modalities: (1) listening to a verbal narrative describing potential goals of care (control group) or (2) viewing a 6-minute video visually depicting treatments comprising the various potential goals of care (intervention group). We used simple randomization at each site based on a computer-generated scheme. Individual assignments were concealed in numbered envelopes. At the end of the trial, the randomization order of subjects was checked against the computer-generated list.
The video and verbal narratives were presented to the subjects in a quiet room in the SNF by a trained member of the research team who followed a structured script. Subjects randomized to the verbal control group were read a description of the three goals of medical care framework (life-prolonging care, limited medical care, and comfort care) developed in our previous work.12,13,15,16 This framework was generated from a review of the advance care planning literature, and consultations with geriatric, critical care, palliative care, health literacy, and decision-making experts. Early versions of the framework were tested and validated with elderly subjects.12,13,15,16
The first option presented, life-prolonging care, was described as aiming to prolong life using all available medical care, and includes cardiopulmonary resuscitation and treatments in the intensive care unit. The second option presented, limited medical care, was described as aiming to maintain physical and mental functioning. It includes treatments such as hospitalization, intravenous fluids, antibiotics, but excludes cardiopulmonary resuscitation and treatments in the intensive care unit. The third option presented, comfort care, was described as aiming to maximize comfort and to relieve pain. It includes oxygen and analgesics, but excludes intravenous therapies and hospitalization unless necessary to provide comfort.
Subjects randomized to the intervention group viewed the video decision aid, shown on a portable computer. The 6-minute video depicts the three categories of medical care using the same definitions used in the verbal narrative, but includes visual images of the typical treatments comprising each goal. For example, life-prolonging care images includes: an intensive care unit with a ventilated patient being tended to by respiratory therapists; a simulated code on a mannequin with clinicians conducting cardiopulmonary resuscitation and intubation; and vasopressors administered through a venous catheter. Visual images to depict limited medical care include: a patient getting antibiotics via a peripheral intravenous catheter; scenes from a typical medical ward service; and a patient wearing a nasal cannula for oxygen delivery. The video depiction of comfort care includes: a patient on home hospice care receiving pain medications; a patient with a nasal cannula for oxygen at home; and, a medical attendant assisting a patient with self-care.
The development of the video decision aid followed a systematic approach, starting with a review of the advance care planning literature. The video's design, content, and structure were reviewed and edited for appropriateness and accuracy by geriatricians, critical care intensivists, palliative care physicians, and decision-making experts using an iterative process. The video was filmed without the use of prompts or stage directions to convey a candid realism in the style known as cinema verite.17,18 All filming and editing was done by the investigative team (A.E.V. and A.D.D.) following previously published filming criteria.19
After exposure to either the verbal narrative or video, subjects were asked to select which level of care they would prefer if their medical condition worsened while at the SNF. Specifically, they were asked: “Imagine that you became very ill and in need of medical treatment, which general approach of medical care would you want provided: life-prolonging care, limited care, or comfort care?” Subjects unable to select a level of care were considered “uncertain.”
For those subjects randomized to the video group, a four-point scale was used to assess perceived value of the video by asking subjects whether they were comfortable watching the video, whether they would recommend it to others, and whether they found the video helpful in their understanding of the goals-of-care options. Subjects who stated they did not find the video helpful were asked to comment why, which was transcribed by the interviewer.
Last, a chart abstraction by the research assistant was performed immediately after exposure to the verbal or video narratives to ascertain whether or not the patient had a DNR order.
Statistical analysis
All subject characteristics and outcomes were described using proportions for categorical variables, and means and standard deviations (SD) for continuous variables. The primary outcome was a preference for comfort care (versus life prolongation, limited care or uncertain) as the goal of care and compared between the two groups using the exact χ2 test. Additional analyses were conducted between subject characteristics (age, gender, education, marital status, health status, presence of advance directive, race, and randomization arm) and desire for comfort care for the entire cohort (i.e., both arms of the study). Rate ratios (RR) and 95% confidence interval (CI) were used to summarize the associations.
Finally, κ statistics were used to summarize the agreement between stated preferences for comfort and the presence of a DNR order in the medical record among the subjects in the intervention and control groups. A two-sided p value<0.05 was considered statistically significant for all analyses.
With a target of 50 patients in each group, the power of the study was estimated to be 90% to detect a 30% difference in the preference for comfort care between the two groups. Data were analyzed and the randomization table was prepared using SAS software, version 9.2 (SAS Institute Inc., Cary, NC).
Results
Subject flow
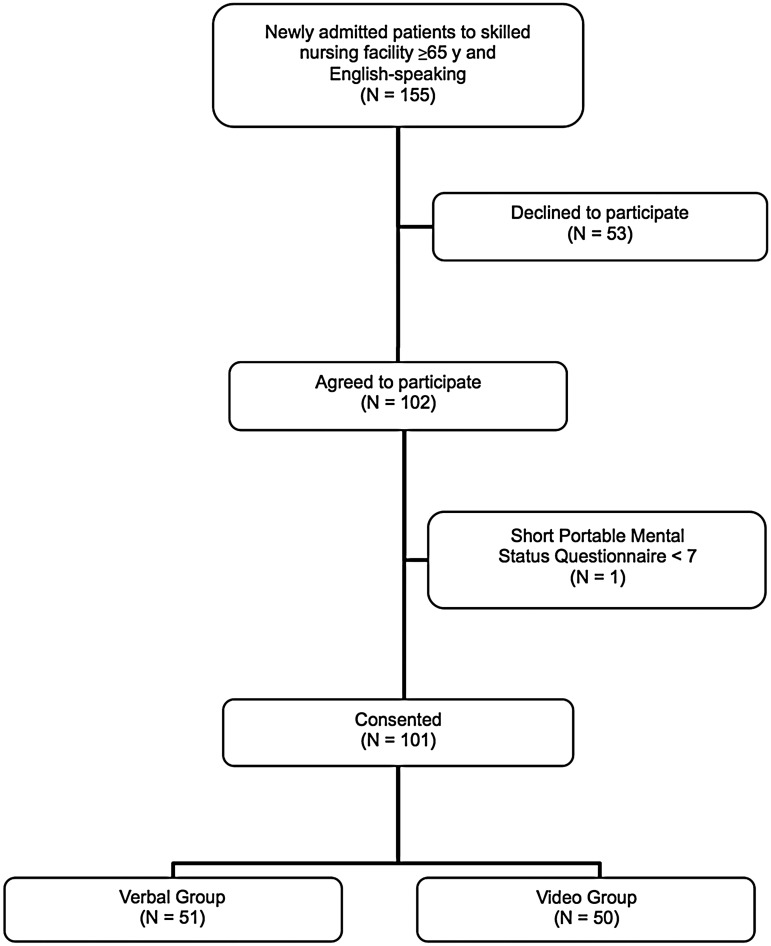
A total of 155 consecutive English-speaking patients 65 years or older admitted to the two SNFs were approached to participate in the study, of whom 102 (66%) agreed to participate. Patients who declined did not differ significantly from the recruited subjects in terms of age, gender, or race. The most common reason given for not participating was lack of interest. Of the 102 patients expressing interest in the study, 1 patient was excluded because her SPMSQ score was less than 7, resulting in a total of 101 study subjects. A total of 51 subjects were randomized to the verbal control group, and 50 subjects were randomized to the video intervention group (Fig. 1). Baseline characteristics of the subjects are shown in Table 1.
FIG. 1.
Flow diagram of study and subjects' flow.
Table 1.
Characteristics of Older Subjects Randomized to the Verbal Narrative and Video Decision Aid Groups
| Characteristics | Verbal (n=51) | Video (n=50) |
|---|---|---|
| Age, mean (SD), y | 76 (7) | 79 (9) |
| Women, n (%) | 31 (61%) | 30 (60%) |
| Race, n (%) | ||
| Black or African American | 33 (65%) | 27 (54%) |
| Hispanic or Latino | 2 (4%) | 2 (4%) |
| White | 16 (31%) | 21 (42%) |
| Education, n (%) | ||
| Elementary | 8 (16%) | 8 (16%) |
| Some high school | 7 (14%) | 7 (14%) |
| High school graduate | 16 (31%) | 16 (32%) |
| Some college | 10 (20%) | 7 (14%) |
| College graduate | 6 (12%) | 6 (12%) |
| Postgraduate or professional | 4 (8%) | 6 (12%) |
| Marital status, n (%) | ||
| Married or with partner | 17 (33%) | 16 (32%) |
| Widowed | 13 (25%) | 17 (34%) |
| Divorced | 6 (12%) | 7 (14%) |
| Never married | 15 (29%) | 9 (18%) |
| Not answered | 0 | 1 (2%) |
| Self-reported health status, n (%) | ||
| Excellent | 5 (10%) | 5 (10%) |
| Very good | 9 (18%) | 5 (10%) |
| Good | 14 (27%) | 18 (36%) |
| Fair | 11 (22%) | 17 (34%) |
| Poor | 12 (24%) | 5 (10%) |
| Have an advance directive,an (%) | 28 (55%) | 29 (58%) |
Subjects were asked if they had an advance directive, either a living will or health care proxy.
SD, standard deviation.
Outcomes
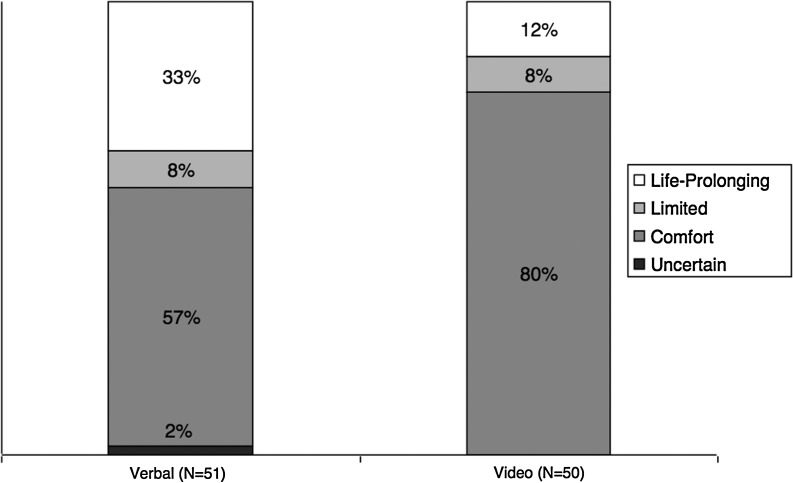
Among the 51 subjects receiving the verbal narrative, 29 (57%) preferred comfort care, 4 (8%) chose limited care, 17 (33%) desired life-prolonging care, and 1 (2%) was uncertain. Among the 50 subjects receiving the video decision aid, 40 (80%) chose comfort care, 4 (8%) chose limited care, and 6 (12%) desired life-prolonging care (Fig. 2). The proportion of subjects opting for comfort care was significantly higher in the intervention group (p=0.02).
FIG. 2.
Subjects' preferences for their goals of care.
Subjects randomized to the video group had a greater likelihood of opting for comfort care (versus other responses; RR 1.4; 95% CI 1.1 to 1.9). None of the other subject characteristics were significantly associated with a preference for comfort care (Table 2).
Table 2.
Analysis of the Likelihood of Choosing Comfort Care as the Primary Goal of Care as Opposed to Life-Prolonging or Limited Care
| Characteristics | Frequency in subjects choosing comfort care | p Value | Unadjusted rate ratio (95% CI) |
|---|---|---|---|
| Age | |||
| <80 | 40 (65%) | 1.0 [reference] | |
| ≥80 | 29 (74%) | 0.38 | 1.2 (0.9 to 1.5) |
| Gender, n (%) | |||
| Female | 45 (74%) | 1.0 [reference] | |
| Male | 24 (60%) | 0.19 | 0.8 (0.6 to 1.1) |
| Race, n (%) | |||
| White | 28 (76%) | 1.0 [reference] | |
| Black or [r:c4]African American | 38 (63%) | 0.26 | 0.8 (0.6 to 1.1) |
| Hispanic or Latino | 3 (75%) | 1.0 | 1.0 (0.5 to 1.8) |
| Education, n (%) | |||
| Less than college graduate | 52 (66%) | 1.0 [reference] | |
| College graduate or higher | 17 (77%) | 0.44 | 1.2 (0.9 to 1.5) |
| Marital status, n (%) | |||
| Ever married | 53 (70%) | 1.0 [reference] | |
| Never married | 16 (67%) | 0.80 | 1.0 (0.7 to 1.3) |
| Health status, n (%) | |||
| Fair or poor | 32 (71%) | 1.0 [reference] | |
| Good, very good, excellent | 37 (66%) | 0.67 | 0.9 (0.7 to 1.2) |
| Have advance directive, n (%) | |||
| No | 26 (60%) | 1.0 [reference] | |
| Yes | 43 (75%) | 0.13 | 1.2 (0.9 to 1.7) |
| Arm, n (%) | |||
| Verbal | 29 (57%) | 1.0 [reference] | |
| Video | 40 (80%) | 0.02 | 1.4 (1.1 to 1.9) |
CI, confidence interval.
In the verbal group, 28 of the 29 subjects who chose comfort care had a code status documented in their medical record. Only 8 of these 28 subjects (29%) had a DNR order in their medical record (κ statistic 0.18; 95% CI–0.02 to 0.37). In the video group, among the 40 subjects who chose comfort care, only 13 (33%) had a DNR order in their medical record (κ statistic 0.06; 95% CI–0.09 to 0.22). The video decision aid was highly acceptable to subjects in the intervention group: 45 of 50 (90%) subjects said they were “very comfortable” or “somewhat comfortable” viewing the video; 43 (86%) said they would “definitely” or “probably” recommend the video to others. Of the 50 subjects who viewed the video, only 4 (8%) found the video “not helpful.” All 4 subjects who did not find the video helpful stated that they had already made their decisions previously and did not find viewing the video additionally helpful. There were no adverse events in either group.
Discussion
Elderly subjects transitioning from an acute hospital stay to a SNF who view a video decision support tool for advance care planning are more likely to state comfort as a goal of care compared to those who listen to a verbal description about medical options. However, only about a third of subjects in both arms of the study who stated that they preferred comfort-oriented measures had a DNR order documented in their record. Thus, while a video decision aid increased the expressed desire for comfort care, our findings suggest a need to better translate those preferences into a written order to limit treatment.
As the first known randomized controlled trial of a video support tool to help determine the goals of care among elderly patients transitioning from an acute hospital to a SNF, this study supports and extends prior research about video decision-making tools in seriously ill patients.12,13,15,16 In our previous work in advanced dementia and advanced cancer, video decision aids elicited preferences for comfort-oriented care, but these studies were conducted in outpatient settings and with patients who were making hypothetical decisions. Our current study extends this earlier work by showing the efficacy of the video for elderly patients in a clinical environment during periods of serious illness and transitioning across health care settings.
Delivery of medical care to patients that is consistent with their stated preferences is a critical consideration to providing high-quality medical care. The main finding in this study in a SNF is consistent with all earlier trials of video support tools for life-limiting conditions: subjects exposed to the video compared to a verbal narrative are more likely to opt for comfort-focused care (vs. life-prolonging or limited medical care). Our prior work also found that video decision support tools improve patient knowledge about their condition and treatment options, and reduce disparities among patients due poor health literacy.12,13,20 Federal and state bodies will soon legislate the development of decision aids to assist patients and their families facing complex health care decisions.21 Our work supports this initiative and may inform the type of decision support tools selected for further development and implementation.
Our findings show a lack of correlation between documented DNR status and stated preferences for comfort-oriented care regardless of decision-making modality. This suggests that in practice, more attention needs to be placed on providing patients and their families with opportunities to fully discuss preferences and to ensure these preferences are reflected in medical orders, especially during a vulnerable period as elderly patients transition between the hospital and post-acute care settings.22–25 Ideally, an out-of-hospital DNR form would be completed that can travel with patients across sites.
Our study has several important limitations. First, the research staff collecting data were not blinded to randomization, which could introduce bias into our findings. Previous randomized studies of interventions aimed at improving end-of-life decision-making have seldom been blinded because limiting the number of interviewers eases the burden on subjects of addressing difficult subject matter.26,27 We attempted to reduce the influence of this potential bias by using structured interviews and data collection instruments.
Second, one third of eligible subjects declined to participate in the study, although they did not differ significantly from the recruited subjects in terms of age, gender, or race. Third, videos can be manipulated to favor a particular perspective. Our study used one video exploring the goals of care. We did not assess responses to different videos altering the races and characteristics of the patients in the video. However, the video was evaluated by experts in a range of fields to ensure that it does not present a biased perspective or to otherwise try to influence subjects to choose a specific option. Fourth, we did not incorporate the video into clinical care by informing patients' physicians of their preferences and then following patients longitudinally to determine whether the video support tool had an effect on their advance care planning or actual clinical outcomes over time. This would be an ideal subsequent study to our present pilot study. Finally, our sample was limited to two SNFs in the Boston area. Thus, our findings might not be generalizable to elderly patients in other geographic areas or health care settings.
Discharge from an acute hospital stay to the post-acute care setting is a challenging and critical time of transition for older patients. Upon admission to a SNF, the patient's health status is often tenuous, and elucidation of their goals of care is needed to align ongoing treatments with patient preferences, and to help avoid unwanted and costly interventions for those whose goal of care is comfort. Our findings suggest that video decision aids may be a feasible and effective approach towards addressing this need in the setting of a SNF. However, our findings also demonstrate that ascertainment of goals of care may not be enough, as steps must also be taken to translate those wishes into a medical order (e.g., DNR orders).
In summary, elderly patients often face complex decision-making as they transition from the acute hospital setting to the SNF setting. To secure high-quality medical care at this juncture, patients must be informed about their options regarding end-of-life goals of care. Education of patients using video decision aids offers a more concrete portrait of potential goals of care compared to verbal discussions. As health care organizations look for innovative tools to inform patients at the end of life and to deliver high-quality medical care that is consistent with patient preferences, video decision aids may provide a useful tool. Future initiatives to improve ascertainment of patients' goals-of-care preferences should also include activities to improve the alignment between patient preferences, medical orders documenting patient goals-of-care, and the care that is delivered.
Acknowledgments
This research was supported by a grant from the Foundation for Informed Medical Decision Making. First author was supported by grant number K08HS018780 from the Agency for Healthcare Research and Quality. Dr. Mitchell was supported by grant K24AG033640 from the National Institute on Aging. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality or the National Institute on Aging. None of the funders participated in the collection, analysis, or interpretation of the data or in preparation, review, or approval of the manuscript.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Kane RL. Finding the right level of posthospital care: “We didn't realize there was any other option for him.”. JAMA. 2011;305:284–293. doi: 10.1001/jama.2010.2015. [DOI] [PubMed] [Google Scholar]
- 2.Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51:549–555. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 3.Coleman EA. Berenson RA. Lost in transition: Challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141:533–536. doi: 10.7326/0003-4819-141-7-200410050-00009. [DOI] [PubMed] [Google Scholar]
- 4.Coleman EA. Min SJ. Chomiak A. Kramer AM. Posthospital care transitions: patterns, complications, and risk identification. Health Serv Res. 2004;39:1449–1465. doi: 10.1111/j.1475-6773.2004.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coleman EA. Smith JD. Raha D. Min SJ. Posthospital medication discrepancies: Prevalence and contributing factors. Arch Intern Med. 2005;165:1842–1847. doi: 10.1001/archinte.165.16.1842. [DOI] [PubMed] [Google Scholar]
- 6.Mor V. Besdine RW. Policy options to improve discharge planning and reduce rehospitalization. JAMA. 2011;305:302–303. doi: 10.1001/jama.2010.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mor V. Intrator O. Feng Z. Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff. 2010;29:57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berkowitz RE. Jones RN. Rieder R, et al. Improving disposition outcomes for patients in a geriatric skilled nursing facility. J Am Geriatr Soc. 2011;59:1130–1136. doi: 10.1111/j.1532-5415.2011.03417.x. [DOI] [PubMed] [Google Scholar]
- 9.Barry MJ. Involving patients in medical decisions: How can physicians do better? JAMA. 1999;282:2356–2357. doi: 10.1001/jama.282.24.2356. [DOI] [PubMed] [Google Scholar]
- 10.Entwistle V. The potential contribution of decision aids to screening programmes. Health Expect. 2001;4:109–115. doi: 10.1046/j.1369-6513.2001.00141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Estabrooks C. Goel V. Thiel E. Pinfold P. Sawka C. Williams I. Decision aids: Are they worth it? A systematic review. J Health Serv Res Policy. 2001;6:170–182. doi: 10.1258/1355819011927431. [DOI] [PubMed] [Google Scholar]
- 12.El-Jawahri A. Podgurski LM. Eichler AF, et al. Use of video to facilitate end-of-life discussions with patients with cancer: A randomized controlled trial. J Clin Oncol. 2010;28:305–110. doi: 10.1200/JCO.2009.24.7502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Volandes AE. Paasche-Orlow MK. Barry MJ, et al. Video decision support tool for advance care planning in dementia: Randomised controlled trial. BMJ. 2009;338:b2159. doi: 10.1136/bmj.b2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 15.Volandes AE. Barry MJ. Chang Y. Paasche-Orlow MK. Improving decision making at the end of life with video images. Medical Decision Making. 2010;30:29–34. doi: 10.1177/0272989X09341587. [DOI] [PubMed] [Google Scholar]
- 16.Volandes AE. Ferguson LA. Davis AD, et al. Assessing end-of-life preferences for advanced dementia in rural patients using an educational video: A randomized controlled trial. J Palliat Med. 2011;14:169–177. doi: 10.1089/jpm.2010.0299. [DOI] [PubMed] [Google Scholar]
- 17.Nichols B. Introduction to Documentary. Bloomington, IN: Indiana University Press; 2001. [Google Scholar]
- 18.Grant BK. Sloniowski J. Documenting the Documentary: Close Readings of Documentary Film and Video. Detroit, MI: Wayne State University Press; 1998. [Google Scholar]
- 19.Gillick MR. Volandes AE. The psychology of using and creating video decision aids for advance care planning. In: Lynch TE, editor. Psychology of Decision Making in Medicine and Health Care. New York, NY: Nova Science Publishers; 2007. pp. 193–206. [Google Scholar]
- 20.Volandes AE. Mitchell SL. Gillick MR. Chang Y. Paasche-Orlow MK. Using video images to improve the accuracy of surrogate decision-making: A randomized controlled trial. J Am Med Dir Assoc. 2009;10:575–580. doi: 10.1016/j.jamda.2009.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The Patient Protection and Affordable Care Act. 2010. Public Law No: 111-148.
- 22.Coleman EA. Parry C. Chalmers S. Min SJ. The care transitions intervention: Results of a randomized controlled trial. Arch Intern Med. 2006;166:1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 23.Coleman EA. Smith JD. Frank JC. Min SJ. Parry C. Kramer AM. Preparing patients and caregivers to participate in care delivered across settings: The Care Transitions Intervention. J Am Geriatr Soc. 2004;52:1817–1825. doi: 10.1111/j.1532-5415.2004.52504.x. [DOI] [PubMed] [Google Scholar]
- 24.Naylor M. Brooten D. Jones R. Lavizzo-Mourey R. Mezey M. Pauly M. Comprehensive discharge planning for the hospitalized elderly. A randomized clinical trial. Ann Intern Med. 1994;120:999–1006. doi: 10.7326/0003-4819-120-12-199406150-00005. [DOI] [PubMed] [Google Scholar]
- 25.Naylor MD. Brooten D. Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281:613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 26.SUPPORT: A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). The SUPPORT Principal Investigators. JAMA. 1995;274:1591–1598. [PubMed] [Google Scholar]
- 27.Hofmann JC. Wenger NS. Davis RB, et al. Patient preferences for communication with physicians about end-of-life decisions. SUPPORT Investigators. Study to Understand Prognoses and Preference for Outcomes and Risks of Treatment. Ann Intern Med. 1997;127:1–12. doi: 10.7326/0003-4819-127-1-199707010-00001. [DOI] [PubMed] [Google Scholar]