Abstract
We report our experience with epidural anesthesia for cesarean section in a morbidly obese parturient with progressive paraplegia from a spinal meningioma. Epidural anesthesia may represent a safe anesthetic choice in such clinical situations.
Keywords: Cesarean, epidural, meningioma, paraplegia, parturient
INTRODUCTION
Although many may consider spinal cord pathology to be a relative contraindication to neuraxial anesthesia, successful epidural catheter placement has been reported in such situations. Takiguchi et al previously reported the successful use of sacral and thoracic catheters for the resection of an L1 intradural neurofibroma in a patient with very poor pulmonary function.1 Epidural anesthetics have also been used successfully in parturients suffering from pseudotumor cerebri and lumbar-peritoneal shunt in situ.2 Brown and Levi reported the successful use of epidural anesthesia during hemilaminectomy, partial facetectomy, and disc excision in 3 parturients suffering from cauda equina syndrome.3 Successful epidural labor analgesia has also been reported in a patient with neurofibromatosis with known L2 subarachnoid neurofibroma.4
CASE REPORT
A 21-year-old gravida 2 para 0 parturient was transferred to our facility at 36 weeks' gestation with new onset bilateral lower extremity paresis and bowel and bladder incontinence. She had no significant past medical or surgical history. She received standard prenatal care until 21 weeks' gestational age when she presented to an outside emergency department secondary to a fall. The patient had 3 additional emergency department visits because of progressive neurological symptoms. At the time of hospital admission, the patient had left lower extremity swelling, bowel and bladder incontinence, and bilateral lower extremity paresis. She was subsequently transferred to our maternal-fetal medicine unit for further work-up and neurosurgical evaluation.
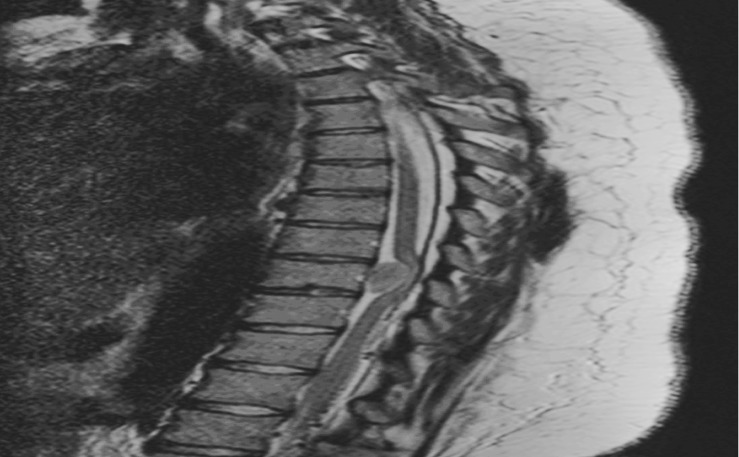
Upon arrival, the patient underwent neurosurgical assessment. Strength was 4/5, deep tendon reflexes were 2+, and sensation was intact in the right lower extremity. On the left side, strength was 2/5, deep tendon reflexes were 3+, and sensation was absent to light touch from pelvis to foot with numbness reported below the knee in the left lower extremity. Initial considerations included spinal cord lesions such as vascular malformation, meningioma, and lipoma. Emergent magnetic resonance imaging of the thoracolumbar spine revealed a 1 × 2.3 × 1.2 cm anterior intradural extramedullary mass centered at the T9 vertebral body level with associated severe spinal canal narrowing and compression of the spinal cord with concomitant edema, most consistent with a diagnosis of spinal meningioma (Figure).
Dexamethasone 10 mg intravenously every 6 hours was initiated. After collaborative consultation among the anesthesiology, neurosurgery, and obstetrics services, clinicians decided to proceed with immediate cesarean delivery, followed by neurosurgical decompression the next day.
After discussion with the attending neurosurgeon, we considered a slowly dosed epidural anesthetic to be the safest option, taking into consideration the patient's overall clinical picture and neurological status. She received standard pretreatment with sodium citrate, metoclopramide, and famotidine and went to the operating room. She was coloaded with 1 L lactated Ringer's solution and underwent uneventful placement of an epidural catheter at the L2-3 interspace. After a negative test dose, she received 20 mL of lidocaine 20 mg/mL plus epinephrine 5 μg/mL, 2 mL of sodium bicarbonate 75 mg/mL, and fentanyl 80 μg. We administered this dose slowly in 5 mL increments at 5-minute intervals. Using ice, we determined her bilateral sensory level to be at T7. Low transverse cesarean section was performed and the patient gave birth to a healthy female infant weighing 3,165 g with Apgar scores of 8 and 9 at 1 and 5 minutes, respectively.
Blood pressure remained within 20% of baseline throughout the perioperative period without vasopressor supplementation. The following day, the patient underwent general endotracheal anesthesia for T8-10 laminectomy with complete tumor resection without complications. The pathology was consistent with meningioma. The patient received intensive inpatient rehabilitation for the next 10 days prior to hospital discharge. At the time of discharge, she could transfer herself to and from a wheelchair independently and ambulate 100 feet with standby assistance. Persistent left lower extremity weakness limited her mobility. At her 6-week follow-up, she was ambulating without assistance. On lower extremity examination, strength was 5/5, deep tendon reflexes were 3+, and sensation to light touch and pinprick was intact bilaterally. She had full bladder and bowel function recovery. Her only complaint at that time was a neuropathic pain on the lateral aspect of her left leg.
DISCUSSION
Ours is one of few reported cases of spinal meningioma presenting during pregnancy and is unique in that it describes successful epidural anesthesia for cesarean delivery.5-8 Our parturient's presentation was similar to that reported in pregnant patients not receiving neuraxial anesthesia. Progression of neurologic symptoms included sensory changes, gait instability, and radicular pain—all consistent with presenting symptoms reported previously in spinal meningioma patients about to undergo surgery. Additionally, our patient suffered from incontinence at the time of presentation. All reported cases of spinal meningioma during pregnancy had good to excellent functional outcomes, suggesting that most patients with this condition are likely to regain neurological function. Our patient's motor and sensory deficits completely resolved, except for persistent left lower extremity radiculopathy.
The decision to proceed with epidural anesthesia rather than spinal or general anesthesia for delivery was the result of multidisciplinary input. We considered maintaining cord perfusion pressure as central to good neurological recovery. Potential problems with a spinal anesthetic in this patient included rapid sympathectomy with possibility of resultant spinal cord ischemia, unreliable sensory level, and dural puncture with a known intradural tumor. Moreover, epidural anesthesia offered the ability to handle prolonged operative duration, which was a possibility with this morbidly obese parturient. An epidural anesthetic would cause a gradual sympathectomy and allow for slow attainment of an appropriate level of anesthetic.
After much consideration, we decided that general anesthesia was not optimal for our patient. At the time of delivery, her body mass index was 44 kg/m2. Despite her favorable airway examination, the increased risk of morbidity and even mortality from airway complications in this morbidly obese parturient was significant. Furthermore, the potential for hypotension on induction might have compromised spinal cord perfusion.
Rapid induction of general anesthesia is generally accomplished with succinylcholine. In patients with paraplegia, succinylcholine is accompanied by a hyperkalemic response. Therefore, our plan would have included rapid-sequence induction with rocuronium. The increased time to effect would have meant a greater risk of hypoxemia during induction.
We were also concerned about fetal depression from prolonged exposure to anesthetics. Datta et al9 previously suggested an increased risk of fetal acidosis and low Apgar scores when incision to delivery time is longer than 8 minutes during cesarean section performed under general anesthesia. Research has yet to show that such an interval affects neonates during deliveries using regional techniques. Weighing the risks and benefits of the previous anesthetic options therefore yielded epidural anesthesia as the optimal approach. Regardless of the approach taken, the anesthetic goals would be the same: maintaining oxygenation, normocarbia, and baseline blood pressure was vital to providing adequate placental perfusion and avoiding fetal acidosis.
Husemeyer and White10 looked at the effect of 10 mL of local anesthetic on extradural pressures. When injected epidurally over 30 to 70 seconds, this volume initially increased the mean extradural pressure to 29 cm H2O. Pressure subsequently decreased to 13 cm H2O after 1 minute and to 11.4 cm H2O after 2 minutes. Such a transient increase in extradural pressure would not likely lead to spinal cord ischemia sufficient to affect long-term outcome. The entry site of the epidural anesthesia was at least 5 spinal segments away from the lesion, so the transient increase in extradural pressure would not have contributed to an overall increased local mass effect of the tumor. Husemeyer and White10 did not evaluate the effect of epidural injection on intradural pressure, which was our main concern. Although our patient received a higher volume of epidural injectate, the injection time was significantly longer. We believed that any increase in intradural pressure near the tumor would be minimal because the site of injection was 5-6 vertebral levels away and the injection was carried out gradually.
We were also confident that because our needle insertion site and catheter were remote from the tumor site, we need not be concerned about issues such as tumor bleeding and metastatic seeding. Regarding the potential risks associated with lumbar punctures for patients with intracranial mass lesions, the same risks do not translate to intraspinal mass lesions. The concern of causing iatrogenic herniation syndrome is based on the idea of a differential pressure gradient between the intracranial and intraspinal cerebrospinal fluid spaces caused by obstructive hydrocephalus and/or cerebral edema. In this case, a focal thoracic intradural mass would not cause a cerebrospinal fluid pressure gradient, so a wet tap would not pose any significant risk of herniation.
CONCLUSION
We report our experience with epidural anesthesia for cesarean section in a morbidly obese parturient with progressive paraplegia from a spinal meningioma. Epidural anesthesia may represent a safe anesthetic choice in such clinical situations.
Figure.
Intradural T9 meningioma.
Footnotes
The authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care and Medical Knowledge.
REFERENCES
- 1.Takiguchi T, Okano T, Okuda Y, Kitajima T. Excision of spinal tumor in a patient with severe pulmonary dysfunction using combined spinal and epidural anesthesia with two epidural catheters. Reg Anesth Pain Med. 1999 May-Jun;24(3):267–271. doi: 10.1016/s1098-7339(99)90141-4. [DOI] [PubMed] [Google Scholar]
- 2.Kim K, Orbegozo M. Epidural anesthesia for cesarean section in a parturient with pseudotumor cerebri and lumboperitoneal shunt. J Clin Anesth. 2000 May;12(3):213–215. doi: 10.1016/s0952-8180(00)00133-1. [DOI] [PubMed] [Google Scholar]
- 3.Brown MD, Levi AD. Surgery for lumbar disc herniation during pregnancy. Spine (Phila Pa 1976) 2001 Feb 15;26(4):440–443. doi: 10.1097/00007632-200102150-00022. [DOI] [PubMed] [Google Scholar]
- 4.Dounas M, Mercier FJ, Lhuissier C, Benhamou D. Epidural analgesia for labour in a parturient with neurofibromatosis. Can J Anaesth. 1995 May;42((5 Pt 1)):420–422. doi: 10.1007/BF03015490. discussion 422-424. [DOI] [PubMed] [Google Scholar]
- 5.Bailey P, Bucy PC. Tumors of the spinal canal. Surg Clin N Amer. 1930 Apr;10(2):233–257. [Google Scholar]
- 6.Cioffi F, Buric J, Carnesecchi S, Romoli S, Conti P. Spinal meningiomas in pregnancy: report of two cases and review of the literature. Eur J Gynaecol Oncol. 1996;;17(5):384–388. [PubMed] [Google Scholar]
- 7.Mealey J, Jr, Carter JE. Spinal cord tumor during pregnancy. Obstet Gynecol. 1968 Aug;32(2):204–209. [PubMed] [Google Scholar]
- 8.Rath S, Mathai KV, Chandy J. Multiple meningiomas of the spinal canal. Case report. J Neurosurg. 1967 Jun;26(6):639–640. doi: 10.3171/jns.1967.26.6.0639. [DOI] [PubMed] [Google Scholar]
- 9.Datta S, Ostheimer GW, Weiss JB, Brown WU, Jr, Alper MH. Neonatal effect of prolonged anesthetic induction for cesarean section. Obstet Gynecol. 1981 Sep;58(3):331–335. [PubMed] [Google Scholar]
- 10.Husemeyer RP, White DC. Lumbar extradural injection pressures in pregnant women. An investigation of relationships between rate of infection, injection pressures and extent of analgesia. Br J Anaesth. 1980 Jan;52(1):55–60. doi: 10.1093/bja/52.1.55. [DOI] [PubMed] [Google Scholar]