Abstract
OBJECTIVE:
Oxygen therapy for infants and small children in developing countries is often not available. Entrainment devices may provide an accurate and precise concentration of oxygen when used at the flow rates appropriate for infants and small children.
METHODS:
A continuously adjustable entrainment device was tested to determine the concentrations and flows of oxygen delivered by using low inlet flow rates suitable for therapy for infants and small children and 3 distinct oxygen delivery systems that varied in their resistive load.
RESULTS:
The use of long and large bore, low resistance tubing (similar to a mask) resulted in the delivery of oxygen concentrations that tracked closely (accurate and precise) to values indicated by the entrainment device. The directly connected system with lower resistance (similar to a hood) produced a similar profile of concentrations and flow rates to the large bore tubing but with even greater accuracy. The use of a long and narrow tubing with higher resistance (similar to a cannula) did not deliver accurate oxygen concentrations. In fact, this high-resistance system failed to work as intended, and instead of entraining air, a large proportion (sometimes >50%) of the oxygen delivered to the entrainment device was ejected through its vents.
CONCLUSIONS:
Entrainment devices can deliver accurate oxygen concentrations at low flow rates if used with low resistance delivery systems; however, entrainment devices are not suitable for use with high resistance delivery systems such as a standard nasal cannula.
Keywords: Venturi, infants, mortality, pneumonia, developing countries, entrainment
WHAT'S KNOWN ON THIS SUBJECT:
Oxygen is an effective treatment, but its availability is limited in some settings, particularly in developing countries. Entrainment devices offer promise for simplifying oxygen delivery, decreasing the cost of oxygen therapy, and increasing its availability.
WHAT THIS STUDY ADDS:
Entrainment devices can be used to deliver specific oxygen concentrations to infants and small children. With appropriate delivery systems, these devices can deliver blended gas with accuracy and precision at the low flows required by infants and small children.
Mortality rates of infants and children younger than 5 in many developing countries in sub-Saharan Africa and southeast Asia are ∼10 times those of developed countries.1 Pneumonia is the leading killer of infants and children in the developing world.2 Many infants and children with pneumonia and other conditions need oxygen therapy to promote survival.3 In the developed world, oxygen is delivered with blenders that mix compressed oxygen and compressed air to provide accurate and precise concentrations and flow rates. Use of these blenders in developing countries is hindered by multiple factors including cost, maintenance, and lack of local availability of compressed air. These blenders are expensive and somewhat complex, which further limits their use in developing countries.
Compressed oxygen cylinders are readily available in most areas of the world and are transportable to remote areas with difficulty. Both the oxygen cylinders (100% oxygen) and oxygen concentrators provide near-pure oxygen (up to 95%), although performance varies considerably among brands.4 Medical oxygen in the developing world produced by portable oxygen concentrators is increasingly common; however, cost and a consistent supply of electricity are limiting factors.5,6 However, prolonged treatment with higher-than-needed concentrations of oxygen is not appropriate early in life because of the potential risk of blindness, death, cerebral palsy, and other conditions.7–9 It would be desirable for oxygen therapy in these low technology environments to have a source of oxygen with adjustable concentrations ranging from near atmospheric (21%) to pure oxygen (100%) concentrations at varying flow rates.
Low-cost devices for blending compressed oxygen and ambient air exist for use in home-based and hospital-based oxygen therapies for adults and older children. These devices are typically part of an apparatus that includes a mask and noncollapsible large bore tubing10 and have been in common use since they were first developed in the 1960s.11–14 These devices use a small diameter jet of compressed oxygen to entrain (draw in) room air through an orifice. The ratio of entrained air to compressed oxygen emitted from the jet can be varied by altering the diameter of the jet (and thus the speed of the jet) and/or the size of the entrainment orifice.15,16 These devices are generally specified by the manufacturer for use with inlet flow rates of >4 L/minute.17,18 This produces outlet flow rates that are generally much higher than those required to treat infants using oxygen masks. Waste is a serious concern in developing countries where oxygen supplies are constrained; therefore, optimization of oxygen inlet flow is vital to increasing the availability of oxygen therapy.
This study was designed to examine the accuracy and precision of high flow entrainment devices at low inlet flow rates (≤1 L/minute) to evaluate their feasibility to provide oxygen therapy to infants and small children in developing countries. We tested the entrainment device with 3 delivery systems to examine the effect of size and length (delivery circuit resistance) on performance of the entrainment device: (1) a narrow long tube that simulates a nasal cannula; (2) a short connector that simulates an oxygen hood (head box); and (3) a large bore long tube that simulates an oxygen mask.
METHODS
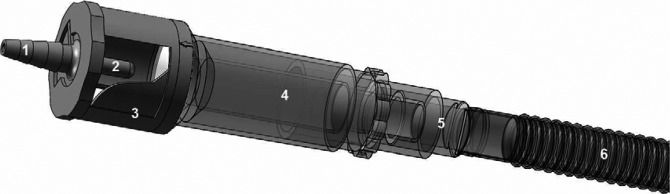
Background research was done to compare various currently available entrainment devices at 1 L/minute. This low flow rate was chosen because it would provide suitable outlet flows for infants and children at many concentrations and was sufficiently lower than previously tested values. The Fischer and Paykel RT0008 device (Huntington Beach, CA) was chosen for evaluation in this study. It is an example of a continuously adjustable entrainment device commonly referred to as a “Venturi.” It should be noted that entrainment devices do not work by the Venturi effect but instead work by the principle of jet mixing; air entrainment occurs through viscous shearing effects.19,20 The device is designed to deliver oxygen concentrations from 28% to 90% with an oxygen supply between 4 and 15 L/minute. This variability of concentration is provided by sliding a plastic guard across the upper part of the main body, which surrounds the “Venturi” jet. This allows for continuous manipulation of the entrainment orifice area (Fig 1).
FIGURE 1.
Rendering of the entrainment device connected to the large bore tubing that was used for these experiments. 1, inlet for oxygen supply line; 2,“Venturi” jet; 3, plastic assembly that consists of sliding guard that adjusts the size of the entrainment windows; 4, mixing area; 5 and 6, connections and tubing (vary for other systems).
To measure the oxygen concentration and flow rate, a Puritan-Bennett PTS2000 tester (Carlsbad, CA) was set up downstream from the outlet of the entrainment device to measure the oxygen concentration and flow rate delivered by the entrainment device by using 3 different delivery systems designed to simulate: (1) an oxygen nasal cannula (91 cm long in noncollapsible with a ∼2.5 mm internal diameter), (2) an oxygen hood (short, direct connection to minimize resistance), and (3) an oxygen mask (61 cm long, noncollapsible ribbed tube with an interior diameter of ∼12.5 mm). The latter 2 systems have substantially lower resistance than the nasal cannula-like system and are compatible with a mask, head box, or similar device but not with a standard cannula.
Standard wall oxygen supply (50 psi) was used for the experiment. It was run through a Bird Low Flow Air/O2 blender (San Diego, CA) set to 100% oxygen at 1 L/minute. Using wall air and oxygen, a 2-point calibration was performed on the Puritan-Bennett tester. The flows were measured, and the blender's regulator manipulated to deliver the desired flow. This fine-tuning of the flow was repeated each time the setup was altered.
The flow rates were observed for 30 seconds until they had stabilized. The manufacturer's stated accuracy for oxygen concentrations and flow measurements with the PTS2000 is ±2% with a 95% confidence level. The testing location was at ∼195 meters above sea level at 24°C and indoor humidity of ∼50%. For each of the 3 delivery systems, data were recorded with 5 replicates for each of the 9 oxygen concentrations (entrainment device-indicated oxygen concentration) to examine accuracy and precision (a total of 27 sets of 5 replicates). Means and confidence intervals were calculated for each configuration.
RESULTS
Oxygen concentrations delivered by each of the systems approximated the oxygen concentrations indicated at the entrainment device (Fig 1). When the entrainment device was set to deliver >40% oxygen, the absolute difference between the delivered and the indicated oxygen concentrations was <4% for both the direct connection and the large bore tubing delivery systems. When the entrainment device was set to deliver <40% oxygen, the direct connection setup had < 3% difference, whereas the large bore tubing resulted in absolute differences of up to 9% (Fig 2). The cannula-like system delivered average oxygen concentrations > 90% for all indicated concentration settings, and the replicate tests were highly variable, which indicates limited entrainment and unstable mixing (Table 1).
FIGURE 2.
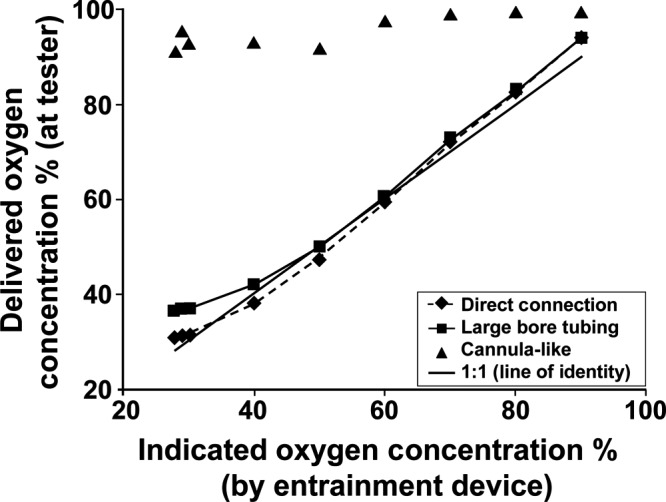
Oxygen concentrations delivered with the direct connection and large bore tubing systems approximated the oxygen concentrations indicated at the entrainment device. The cannula-like system did not deliver appropriate oxygen concentrations.
TABLE 1.
SDs and 95% Confidence Intervals for Each Indicated Oxygen Concentration
| Indicated Oxygen Concentration | Direct Connection |
Large Bore Tubing |
Cannula-Like (Supply Line) |
|||
|---|---|---|---|---|---|---|
| SD | 95% CI | SD | 95% CI | SD | 95% CI | |
| 28 | 0.08 | 30.6–30.8 | 0.55 | 36.0–37.0 | 9.87 | 82.4–99.7 |
| 29 | 0.08 | 31.1–31.3 | 0.63 | 36.5–37.6 | 8.99 | 87.5–100 |
| 30 | 0.04 | 31.5–31.6 | 0.38 | 36.5–37.2 | 7.90 | 86.1–100 |
| 40 | 0.08 | 38.1–38.3 | 0.51 | 41.6–42.5 | 8.67 | 85.5–100 |
| 50 | 0.27 | 47.3–47.7 | 0.81 | 49.3–50.7 | 9.54 | 83.6–100 |
| 60 | 0.47 | 58.8–59.6 | 0.23 | 60.2–60.6 | 2.63 | 95.5–100 |
| 70 | 0.31 | 71.5–72.0 | 0.43 | 72.0–72.8 | 0.58 | 98.5–99.5 |
| 80 | 0.17 | 82.0–82.3 | 0.31 | 82.4–83.0 | 0.42 | 99.2–99.2 |
| 90 | 0.21 | 93.7–94.0 | 0.29 | 93.4–94.0 | 0.13 | 99.5–99.7 |
CI indicates confidence interval.
The delivered flow rates of the direct connection and large bore tubing systems increased as indicated oxygen concentrations were decreased (Fig 2), as would be expected because of their intrinsic relationship; ie, the larger volume of entrained air resulted in increased outlet flow rates while simultaneously diluting the supplied oxygen. Delivered flow rates had roughly an inverse exponential relationship to the indicated oxygen concentrations. The large bore system entrained less air than the directly connected system, which resulted in lower outlet flow rates at certain indicated oxygen concentrations because of the increased resistive load. At all indicated concentrations, the cannula-like system delivered outlet flow rates that were less than the inlet flow rate of pure oxygen, which indicates that air was not properly entrained (Fig 3).
FIGURE 3.

The direct connection and large bore tubing systems delivered flow rates with inverse exponential relationships to the indicated oxygen concentration. The cannula-like system failed to properly entrain air.
DISCUSSION
These experiments demonstrate that entrainment devices can accurately and precisely deliver set oxygen concentrations at flows lower than those for which they are nominally designed, but only if used with low resistance delivery systems. The entrainment device failed to deliver accurate concentrations with a supply line similar in character to a nasal cannula. This was likely because of the higher resistance of the nasal cannula-like delivery system, which led to decreased air entrainment. Thus, there is a threshold at which delivery system resistance prevents entrainment and outlet flow rates fall below inlet flow rates, and oxygen is wasted. Entrainment devices could be used to deliver a specific inspired oxygen concentration. The results of the experiments are important because the entrainment device was very accurate and precise when used with an oxygen hood or mask type system, and thus, could be used to deliver a specific oxygen concentration. However, the flow used with a hood or mask has to be high enough to prevent rebreathing. In addition, the mask may not be tolerated well by infants.
In these experiments we examined the ability of the entrainment device, which has been used to deliver blended oxygen at higher flow rates for adults, to be adapted to deliver appropriate concentrations at the low flows that infants and small children need. The outlet flow is inversely related to the delivered oxygen concentration because of the constant concentrations of the inlet gases. These experiments did not directly examine how the air is entrained. In fact, in some of the experiments with the cannula-like delivery system, there was leakage of oxygen and a relative lack of entrainment. Additional experiments of the mechanisms and studies with patients using pulse oximeters would provide additional important information.
In studies in which the properties of air entrainment devices with inlet flows > 4 L/minute have been examined, the ability to deliver accurate oxygen concentrations has been demonstrated.21,22 However, labels that indicate oxygen concentration should not be accepted without scrutiny because inaccuracies in oxygen concentration delivery can occur.23 To the authors' knowledge, studies in which entrainment devices at the low inlet flow rates examined in this study have been evaluated have not been published previously.
In this study it is indicated that entrainment devices, designed for adults and for use at high flow rates, can act as blenders and provide low cost, low maintenance, low concentration oxygen therapy at the low flows needed by infants and small children. The entrainment devices are fully disposable from the point of oxygen entry to the delivery device. These advantages, when compared with more complex traditional blenders, are somewhat offset by the slight but clinically insignificant decrease in accuracy and precision of delivered oxygen concentrations. According to our results, the entrainment devices can work well with oxygen masks and hoods. However, the entrainment devices cannot be used with the traditional nasal cannulas as a delivery device because of their high resistive load. Alternate patient delivery systems, including masks (with exhalation vents) and hoods, can be used with the entrainment devices, but these alternate delivery systems are not as efficient as cannula because of their larger dead space and the need to prevent carbon dioxide rebreathing. Flow rates of at least 2 to 3 L/kg per are required for hoods to prevent rebreathing.24,25 Data for infants and newborns treated by using oxygen masks are not available.26 Alternatively, nasal cannula delivery systems can be modified by reducing their resistive load. The new resuscitation guidelines recommend oxygen saturation targeting during neonatal resuscitation to avoid hypoxemia and hyperoxemia,27,28 which would require oxygen and air blending. Additional research is needed to test low cost blenders with resuscitation equipment. However, room air resuscitation can reduce neonatal mortality29 and has been done without oxygen blending in large clinical studies.30,31
In clinical studies, hypopharyngeal oxygen concentrations have been shown to be reliable measures of the actual inspired oxygen concentrations.32–38 If hypopharyngeal oxygen concentrations need to be decreased from those achieved with the 100% oxygen source, an entrainment device would be useful in those situations.
CONCLUSIONS
Entrainment devices designed to operate at high flow rates for adults can be operated at lower flow rates and can be used to administer blended oxygen to infants and small children. In this study we show that these devices are sensitive to resistive load but can be used with delivery systems with a low resistive load, such as oxygen masks and hoods. Entrainment devices can eliminate the need for complex and expensive blenders and compressed air. Their low cost and low maintenance requirements would allow targeted, effective oxygen treatment of infants and small children for life-threatening pneumonia and other pulmonary disorders, particularly in resource-limited developing countries.
ACKNOWLEDGMENT
This work was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development Global Network for Women's and Children's Health Research (HD43475 and HD40636).
Footnotes
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
REFERENCES
- 1. Åhman E, Zupan J. Neonatal and Perinatal Mortality: Country, Regional and Global Estimates 2004. Geneva, Switzerland: WHO Press; 2007 [Google Scholar]
- 2. Duke T, Wandi F, Jonathan M, Matai S, Kaupa M, Saavu M, Subhi R, Peel D. Improved oxygen systems for childhood pneumonia: a multihospital effectiveness study in Papua New Guinea. Lancet. 2008;372(9646):1328–1333 [DOI] [PubMed] [Google Scholar]
- 3. Wardlaw TM, Johansson EW, Hodge M. Pneumonia: The Forgotten Killer of Children. New York, NY; Geneva, Switzerland: United Nations Children's Fund/World Health Organization; 2006 [Google Scholar]
- 4. Chatburn RL, Williams TJ. Performance of 4 portable oxygen concentrators. Respir Care. 2010;55(4):433–442 [PubMed] [Google Scholar]
- 5. Mokuolu OA, Ajayi OA. Use of an oxygen concentrator in a Nigerian neonatal unit: economic implications and reliability. Ann Trop Paediatr. 2002;22(3):209–212 [DOI] [PubMed] [Google Scholar]
- 6. Matai S, Peel D, Wandi F, Jonathan M, Subhi R, Duke T. Implementing an oxygen programme in hospitals in Papua New Guinea. Ann Trop Paediatr. 2008;28(1):71–78 [DOI] [PubMed] [Google Scholar]
- 7. SUPPORT Study Group of the Eunice Kennedy Shriver NICHD Neonatal Research Network, Carlo WA, Finer NN, et al. Target ranges of oxygen saturation in extremely preterm infants. N Engl J Med. 2010;362(21):1959–1969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Deopujari S. Oxygen therapy in pediatrics. Indian J Pediatr. 2000;67(12):1461–1469 [DOI] [PubMed] [Google Scholar]
- 9. Gitto E, Pellegrino S, D'Arrigo S, Barberi I, Reiter RJ. Oxidative stress in resuscitation and in ventilation of newborns. Eur Respir J. 2009;34(6):1461–1469 [DOI] [PubMed] [Google Scholar]
- 10. Libby DM, Briscoe WA, King TK, Smith JP. Oxygen concentration from room air: a new source for oxygen therapy in the home. JAMA. 1979;241(15):1599–1602 [PubMed] [Google Scholar]
- 11. Leigh JM. Variation in performance of oxygen therapy devices. Towards the rational employment of “The dephlogisticated air described by Priestley.” Ann R Coll Surg Engl. 1973;52(4):234–253 [PMC free article] [PubMed] [Google Scholar]
- 12. Campbell EJ. Methods of oxygen administration in respiratory failure. Ann N Y Acad Sci. 1965;121:861–870 [DOI] [PubMed] [Google Scholar]
- 13. Schiff MM, Massaro D. Effect of oxygen administration by a Venturi apparatus on arterial blood gas values in patients with respiratory failure. N Engl J Med. 1967;277(18):950–953 [DOI] [PubMed] [Google Scholar]
- 14. Chusid EL, Miller A, Samortin TG, Daly EE. Treatment of hypoxemia: a new mask for delivering controlled low-concentration oxygen. JAMA. 1970;214(5):889–893 [DOI] [PubMed] [Google Scholar]
- 15. Dobson MB. Use of jet mixing devices with an oxygen concentrator. Thorax. 1992;47(12):1060–1062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ihra G, Aloy A. On the use of Venturi's principle to describe entrainment during jet ventilation. J Clin Anesth. 2000;12(5):417–419 [DOI] [PubMed] [Google Scholar]
- 17. Hill SL, Barnes PK, Hollway T, Tennant R. Fixed performance oxygen masks: an evaluation. Br Med J (Clin Res Ed). 1984; 288(6426):1261–1263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Goddard JM. Concentrations of oxygen delivered by air entrainment oxygen masks. Ann R Coll Surg Engl. 1985;67(6):366–367 [PMC free article] [PubMed] [Google Scholar]
- 19. Scacci R. Air entrainment masks: jet mixing is how they work; the Venturi and Bernoulli principles are how they don't. Respir Care. 1979;24:928–931 [Google Scholar]
- 20. Kittredge P. Neither Venturi nor Bernoulli. Lancet. 1983;1(8317):182. [DOI] [PubMed] [Google Scholar]
- 21. Leigh JM. Variation in performance of oxygen therapy devices. Anaesthesia. 1970;25(2):210–222 [DOI] [PubMed] [Google Scholar]
- 22. Friedman S, Weber B, Briscoe WA, Smith JP, King TK. Oxygen therapy. evaluation of various air-entraining masks. JAMA. 1974;228(4):474–478 [DOI] [PubMed] [Google Scholar]
- 23. Cohen JL, Demers RR, Saklad M. Air-entrainment oxygen masks: a performance evaluation. Respir Care. 1977;22(3):277–282 [PubMed] [Google Scholar]
- 24. Frey B, Shann F. Oxygen administration in infants. Arch Dis Child Fetal Neonatal Ed. 2003;88(2):F84–F88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bernet V, Hug MI, Frey B. Predictive factors for the success of noninvasive mask ventilation in infants and children with acute respiratory failure. Pediatr Crit Care Med. 2005;6(6):660–664 [DOI] [PubMed] [Google Scholar]
- 26. Duke T. Neonatal pneumonia in developing countries. Arch Dis Child Fetal Neonatal Ed. 2005;90(3):F211–F219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Perlman JM, Wyllie J, Kattwinkel J, et al. ; Neonatal Resuscitation Chapter Collaborators Part 11: Neonatal resuscitation: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2010;122(16 suppl 2):S516–S538 [DOI] [PubMed] [Google Scholar]
- 28. Kattwinkel J, Perlman JM, Aziz K, et al. ; American Heart Association Neonatal resuscitation: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics. 2010;126(5). Available at: www.pediatrics.org/cgi/content/full/126/5/e1400 [DOI] [PubMed] [Google Scholar]
- 29. Saugstad OD, Ramji S, Vento M. Resuscitation of depressed newborn infants with ambient air or pure oxygen: a meta-analysis. Biol Neonate. 2005;87(1):27–34 [DOI] [PubMed] [Google Scholar]
- 30. Carlo WA, Goudar SS, Jehan I, et al. Newborn-care training and perinatal mortality in developing countries. N Engl J Med. 2010;362(7):614–623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Carlo WA, McClure EM, Chomba E, et al. Newborn care training of midwives and neonatal and perinatal mortality rates in a developing country. Pediatrics. 2010;126(5). Available at: www.pediatrics.org/cgi/content/full/126/5/e1064 [DOI] [PubMed] [Google Scholar]
- 32. Kaye W, Summers JT, Jr, Monast R, McEnany MT. Nasal oxygen sampler. Heart Lung. 1981;10(4):679–685 [PubMed] [Google Scholar]
- 33. Schacter EN, Littner MR, Luddy P, Beck GJ. Monitoring of oxygen delivery systems in clinical practice. Crit Care Med. 1980;8(7):405–409 [DOI] [PubMed] [Google Scholar]
- 34. Vain NE, Prudent LM, Stevens DP, Weeter MM, Maisels MJ. Regulation of oxygen concentration delivered to infants via nasal cannulas. Am J Dis Child. 1989;143(12):1458–1460 [DOI] [PubMed] [Google Scholar]
- 35. Kuluz JW, McLaughlin GE, Gelman B, et al. The fraction of inspired oxygen in infants receiving oxygen via nasal cannula often exceeds safe levels. Respir Care. 2001;46(9):897–901 [PubMed] [Google Scholar]
- 36. Fan LL, Voyles JB. Determination of inspired oxygen delivered by nasal cannula in infants with chronic lung disease. J Pediatr. 1983;103(6):923–925 [DOI] [PubMed] [Google Scholar]
- 37. Finer NN, Bates R, Tomat P. Low flow oxygen delivery via nasal cannula to neonates. Pediatr Pulmonol. 1996;21(1):48–51 [DOI] [PubMed] [Google Scholar]
- 38. Shann F, Gatchalian S, Hutchinson R. Nasopharyngeal oxygen in children. Lancet. 1988;2(8622):1238–1240 [DOI] [PubMed] [Google Scholar]