Abstract
BACKGROUND:
Fundoplication is a common pediatric surgery, but little data comparing the laparoscopic approach with the open approach have been published.
OBJECTIVE:
To compare infection rates, complication rates, length of stay, and cost for laparoscopic fundoplication versus open fundoplication among pediatric patients and to examine trends in utilization of laparoscopic fundoplication.
METHODS:
We used the Pediatric Health Information System database to conduct a retrospective study of children (aged <19 years) admitted for a fundoplication between 2005 and 2008. Descriptive characteristics for those undergoing a laparoscopic and open fundoplication were compared. Multivariate regression with random effects specified at the hospital level was used to model the association between laparoscopic fundoplication and the outcomes.
RESULTS:
Fifty-six percent of 7083 fundoplication admissions had laparoscopic fundoplication. Median length of stay was 4 days for laparoscopic and 10 days for open fundoplication. The median cost of laparoscopic fundoplication was $13 003 versus $22 487 for open fundoplication. Laparoscopic fundoplication was associated with a 24% and 51% reduction in the adjusted odds of infection and surgical complications, respectively. The proportion of fundoplications performed laparoscopically increased from 51% in 2005 to 63% in 2008 (P < .001), but there was no increase in the overall fundoplication rate.
CONCLUSIONS:
In a large study of children's hospitals, laparoscopic fundoplication was associated with improved outcomes compared with the open procedure, even after adjustment for patient severity. Laparoscopic fundoplication has become the most common form of antireflux surgery in children over 1 year of age, but this has not been associated with an increase in the overall utilization of the fundoplication procedure. These data have important implications for clinical practice and surgical training.
Keywords: fundoplication, laparoscopic fundoplication, open fundoplication, neurologic impairment, surgical outcomes
WHAT'S KNOWN ON THIS SUBJECT:
Fundoplication is the third most common major surgical procedure performed in children in the United States, and the laparoscopic approach has increased in popularity in the absence of strong evidence to support its adoption.
WHAT THIS STUDY ADDS:
In the study population, laparoscopic fundoplication was associated with shorter length of stay, reduced costs, and lower complication rates when compared with the open approach, even after adjustment for age and severity.
Fundoplication is the third most common abdominal procedure performed by pediatric surgeons in the United States.1 It is considered the surgical treatment of choice for medically refractory reflux in infants and children and can be performed in an open or laparoscopic fashion. To date, research on open versus laparoscopic fundoplication often has relied on potentially nonrepresentative data typically drawn from a single center or hospital.2–5 Although the results of previous studies suggest that the laparoscopic approach has concrete advantages over the open procedure, we do not know the degree to which they are generalizable.6
Research on adults shows that the introduction of laparoscopic fundoplication in the early 1990s led to a substantial increase in total fundoplications.7 In contrast, there is little evidence that the rate of pediatric fundoplication increased after the first laparoscopic fundoplication was reported in 1993.8 In fact, 2 large studies9,10 examined national rates of pediatric fundoplication and found no evidence of a substantial increase in rates. Because the specific procedure code for laparoscopic fundoplication was not introduced until late in 2004, previous studies have not been able to accurately measure changes over time in the use of open and laparoscopic fundoplication.
The primary objective of this study was to compare infection rates, surgical complication rates, length of stay (LOS), and the cost for laparoscopic versus open fundoplication among patients up to 18 years of age admitted to a children's hospital for a fundoplication procedure during the period 2005 through 2008. In addition, we examined hospital-level and physician-level effects on the utilization of laparoscopic fundoplication and compared temporal trends in the utilization of the laparoscope with overall rates of fundoplication.
PATIENTS AND METHODS
The Pediatric Health Information System Database
We conducted a retrospective cohort study of children admitted for a fundoplication using the Pediatric Health Information System (PHIS) database. The database includes demographic, diagnostic, procedural, outcome, and charge data for all pediatric discharges from 42 freestanding, noncompeting children's hospitals in the United States. Together, these hospitals account for ∼70% of acute care admissions to freestanding pediatric hospitals in the United States.11 Publicly available data from 2006 reveal that close to 75% of all fundoplications in children are performed at children's hospitals.12 Thirty-nine hospitals contributed data each year for the entire period under study.
Study Cohort
Our study included pediatric patients younger than 19 years of age who had a fundoplication as their principal procedure between January 1, 2005, and December 31, 2008. To ensure that fundoplication was the primary reason for admission, we excluded patients whose principal procedure was not fundoplication (see Appendix 1). Patients were identified as having either an open or laparoscopic fundoplication as their principal procedure on the basis of the following International Classification of Diseases, Version 9 (ICD-9) procedure codes: 44.66 (open) and 44.67 (laparoscopic). If the same patient appeared more than once during the study period (2005–2008) with a fundoplication as their principal procedure, only the first episode of fundoplication was retained as an index case.
Outcome Measures
Infections and surgical complications were identified by examination and classification of ICD-9 codes, creating mutually exclusive groupings. The infection indicator was further divided into the following subcategories: wound infection; pneumonia; urinary tract infection; bacterial infection, not otherwise specified; sepsis; and other. Similarly, the surgical complications category was divided into the following subcategories: operative laceration; bleeding; cardiac; gastrointestinal; pulmonary; wound dehiscence; and other. The following 2 measures of the time patients spent in the hospital were used: total LOS and postprocedure (postfundoplication) LOS. Total costs were determined on the basis of cost-to-charge ratios submitted by the hospitals on their Medicare cost reports. All costs were adjusted for inflation using the hospital-and-related-services component of the Consumer Price Index and are reported in 2008 US dollars.13
Covariates
Covariates included patient gender, age, race/ethnicity, payer source, severity indicators, and clinical characteristics. Patients were classified into 1 of 4 groups: neonates/infants (aged <1 year); early child (aged 1 to <5 years); late child (5 to <13 years); and adolescent (13–18 years). Race categories included white, black, and other; white was further divided on the basis of Hispanic ethnicity. Payer sources were Medicaid/other government, private, or self-pay/other/missing. We used 2 different measures to account for patient severity: neurologic impairment (a classification system described elsewhere10) and the count of complex chronic conditions (0, 1, 2, 3 or more).14 We also identified admissions using 3 clinical characteristics: concurrent gastrostomy; reflux-related principal diagnosis; or a history of fundoplication. Patients with a concurrent (occurring on the same date) gastrostomy procedure were identified with ICD-9 codes 43.11 and 43.19. The codes used to identify patients with a reflux-related diagnosis are shown in Appendix 2. History of fundoplication was defined as a previous fundoplication within the past 5 years (using PHIS data from 2000 to 2004) and was captured if a patient was admitted to the same participating hospital twice. Thirty-four hospitals contributed admission data starting in 2000, and that number rose to 42 hospitals by 2008.
Statistical Analyses
We calculated laparoscopic fundoplications as a proportion of total fundoplications, as well as fundoplications per inpatient procedure and per hospital admission at each PHIS hospital. Patient characteristics by procedure type were compared using the Pearson χ2 test of association and Mantel-Haenszel χ2 for ordinal categories. Continuous outcomes (LOS and total cost) were summarized by their median and interquartile range because of their skewed distributions, and differences in median values by fundoplication technique were tested using the Mann-Whitney U test. Two hospitals were excluded from the cost analyses because of missing data.
Multivariate Regression Models
Multilevel (hierarchical) multivariate regression analyses with hospital random effects were used to model the association between type of fundoplication and the outcomes of interest, while adjusting for demographic and clinical factors. Covariates were selected on the basis of bivariate association with the outcomes and the association with open or laparoscopic procedure. A logistic distribution was used to estimate the relationship between type of fundoplication and the dichotomous outcomes (infection and surgical complication); a log-linear specification was used to estimate the relationship between type of fundoplication and the continuous outcomes.15 Mean-adjusted LOS and cost were back transformed using the smearing estimate.16 Variation between hospitals was quantified using the intraclass correlation coefficient, which can be interpreted as the proportion of the total variation attributable to variation between hospitals.
Physician and Hospital Effects
Physician variation was examined in a subanalysis of 38 hospitals that provided unique physician data. Using a subset of patients whose principal physician was identified as a pediatric surgeon, a 3-level hierarchical model allowed for the examination of physician variation within hospitals for the specified outcomes. Physician type for the admissions is listed in Appendix 3. The intraclass correlation coefficient was used to assess the proportion of variation in each outcome attributable to physicians within hospitals and between hospitals. All reported P values in our analysis are from two-sided hypothesis tests, and statistical significance was defined at the .05 level. All analyses used SAS version 9.2 (SAS Institute, Cary, NC).
RESULTS
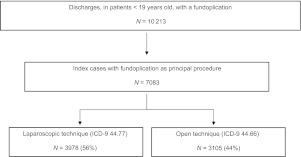
During the 4-year period 2005 through 2008, 10 213 fundoplication procedures were performed on patients under the age of 19 years at 1 of 42 children hospitals in the PHIS network. Of that group, we examined 7083 unique admissions whose principal procedure was fundoplication (see Fig 1). Fifty-six percent had a laparoscopic fundoplication, but there was substantial variation across hospitals in its use. For instance, at 1 hospital, only 8% of fundoplications were done laparoscopically; at another, fully 89% of fundoplications were done laparoscopically.
FIGURE 1.
PHIS fundoplication procedures, 2005–2008.
Age and demographic characteristics of the patients in the sample are presented in Table 1 by type of fundoplication. Notably, the distribution of patients undergoing open procedures was skewed toward neonates and infants, those undergoing concurrent gastrostomy, and higher severity indicators. Although the laparoscopic procedure was associated with significantly lower fatalities, patients undergoing either type of fundoplication had mortality rates lower than 2%. Patients classified with neurologic impairment underwent a laparoscopic procedure 53% of the time compared with 59% of the time for patients without neurologic impairment.
TABLE 1.
Characteristics of Study Patients
| All Patients, n = 7083, % | Open, n = 3105, % | Laparoscopic, n = 3978, % | P | |
|---|---|---|---|---|
| Demographics | ||||
| Male | 56 | 54 | 57 | .02 |
| Age | <.01 | |||
| Neonate/infant, aged <1 year | 42 | 51 | 35 | |
| Early child, aged 1 year to <5 years | 32 | 29 | 34 | |
| Late child, aged 5 years to <13 years | 17 | 14 | 20 | |
| Adolescent, aged 13 years to <19 years | 9 | 7 | 11 | |
| Race/ethnicity | <.01 | |||
| White/non-Hispanic | 55 | 53 | 57 | |
| Black | 17 | 18 | 16 | |
| White/Hispanic | 14 | 16 | 13 | |
| Other/missing | 14 | 13 | 14 | |
| Payer source | <.01 | |||
| Medicaid/other government source | 55 | 58 | 52 | |
| Private | 29 | 28 | 30 | |
| Self-pay/other/missing | 16 | 14 | 18 | |
| Year | <.01 | |||
| 2005 | 27 | 30 | 24 | |
| 2006 | 26 | 28 | 25 | |
| 2007 | 25 | 23 | 26 | |
| 2008 | 23 | 19 | 25 | |
| Died | 1.0 | 1.6 | 0.4 | <.01 |
| Clinical characteristics | ||||
| Concurrent gastrostomy | 59 | 65 | 55 | <.01 |
| Reflux-related principal diagnosis | 62 | 51 | 71 | <.01 |
| History of previous fundoplication | 3 | 5 | 2 | <.01 |
| Severity indicators | ||||
| Neurologically impaired | 49 | 53 | 47 | <.01 |
| Number of complex chronic conditions | <.01 | |||
| 0 | 44 | 36 | 49 | |
| 1 | 36 | 36 | 36 | |
| 2 | 15 | 20 | 11 | |
| ≥3 | 6 | 8 | 4 |
Outcomes by Type of Fundoplication
The top section of Table 2 presents unadjusted outcomes for the patients in our sample. The laparoscopic approach was associated with lower unadjusted rates of infection and surgical complication. These associations held true for all subcategories of infection and surgical complication examined. The typical (that is, median) patient receiving the laparoscopic procedure spent 4 days in the hospital versus 10 days in the hospital for the open procedure. The typical patient receiving the laparoscopic procedure accrued $13 003 in costs during their hospital stay, whereas the typical patient who had open fundoplication accrued $22 487 in costs. However, the median per-day cost was significantly less for patients undergoing open compared with laparoscopic fundoplication ($2721 vs $3224; P < .01).
TABLE 2.
Unadjusted Outcomes of Study Patients Who Underwent Laparoscopic Versus Open Fundoplication
| Outcome | All Patients | Open | Laparoscopic |
|---|---|---|---|
| n | 7083 | 3105 | 3978 |
| Infection, % | 21.0 | 27.6 | 15.7 |
| Wound infection | 2.2 | 2.9 | 1.7 |
| Pneumonia | 6.3 | 8.2 | 4.9 |
| Urinary tract infection | 3.1 | 4.3 | 2.2 |
| Bacterial infection, NOS | 9.4 | 13.0 | 6.6 |
| Sepsis | 2.7 | 4.2 | 1.5 |
| Other | 9.7 | 13.0 | 7.1 |
| Surgical complications, % | 17.9 | 25.5 | 12.0 |
| Operative laceration | 1.1 | 1.7 | 0.6 |
| Bleeding | 0.5 | 0.9 | 0.2 |
| Cardiac | 0.6 | 0.9 | 0.5 |
| Gastrointestinal | 8.8 | 13.3 | 5.2 |
| Pulmonary | 5.0 | 6.0 | 4.3 |
| Wound dehiscence | 0.9 | 1.8 | 0.2 |
| Other | 4.7 | 7.0 | 3.0 |
| Total costs, $a | 15 699 (8786–41 876) | 22 487 (10 313–63 971) | 13 003 (8069–29 243) |
| Cost per day, $b | 2992 (2230–3994) | 2721 (2055–3542) | 3224 (2409–4421) |
| Total LOS, d | 6 (3–19) | 10 (4–28) | 4 (2–13) |
| Postprocedure LOS, d | 4 (3–8) | 6 (4–12) | 3 (2–6) |
| Reflux-related principal diagnosis, n | 4411 | 1586 | 2825 |
| Total costs, $a | 11 209 (7796–19 590) | 13 099 (8397–23 729) | 10 602 (7444–17 519) |
| Cost per day, $b | 3159 (2384–4315) | 2706 (2106–3573) | 3453 (2581–4738) |
| Total LOS, d | 4 (2–7) | 5 (3–10) | 3 (2–6) |
| Postprocedure LOS, d | 3 (2–6) | 5 (3–7) | 3 (2–5) |
| Neurologically impaired patients, n | 3495 | 1629 | 1866 |
| Total costs, $a | 20 785 (10 621–53 104) | 26 955 (12 332–69 981) | 17 495 (9928–41 169) |
| Cost per day, $b | 2871 (2130–3738) | 2654 (1989–3433) | 3045 (2263–3994) |
| Total LOS, d | 9 (4–23) | 12 (5–30) | 6 (3–19) |
| Postprocedure LOS, d | 5 (3–10) | 7 (4–13) | 4 (3–7) |
Infection and surgical complication reported as column percentages. Costs and LOS are given as medians (interquartile ranges). All outcomes show statistically significant differences by surgical technique (open and laparoscopic: P value < 0.01 with the exception of cardiac surgical complications, P = .04).
Reported in 2008 US dollars.
Defined as total cost in 2008 US dollars divided by LOS.
The bottom two sections of Table 2 present unadjusted LOS and cost for the subset of patients admitted with a reflux-related diagnosis and unadjusted LOS and cost for the subset of patients admitted with neurologic impairment. Patients admitted with a reflux-related principal diagnosis had, on average, lower LOS and total cost of care than were observed in the full sample. In contrast, patients with neurologic impairment had higher LOS and total cost.
Multilevel Regression Analysis
Estimates of the adjusted relationship between type of fundoplication and the dichotomous outcomes under study are presented in Table 3. The laparoscopic approach was associated with a 24% percent reduction in the odds of experiencing an in-hospital infection (adjusted odds ratio: 0.76 [95% confidence interval: 0.66–0.88]) compared with open fundoplication and a 51% reduction in the odds of having a surgical complication (adjusted odds ratio: 0.49 [95% confidence interval: 0.42–0.58]). The number of chronic conditions was positively associated with the likelihood of infection and surgical complication. A history of previous fundoplication was associated with lower odds of infection but higher odds of surgical complication.
TABLE 3.
Factors Associated with Infection and Surgical Complication in Adjusted Analyses
| Infection, n = 7083, Odds Ratio (95% Confidence Interval) | Surgical Complication, n = 7083, Odds Ratio (95% Confidence Interval) | |
|---|---|---|
| Fundoplication | ||
| Laparoscopic | 0.76 (0.66–0.88)a | 0.49 (0.42–0.58)a |
| Open | Reference | Reference |
| Age on day of fundoplication | ||
| Neonate/infant (aged <1 year) | 1.53 (1.16–2.01)a | 0.47 (0.36–0.61)a |
| Early child (aged 1 year to <5 years) | 1.06 (0.80–1.40) | 0.69 (0.53–0.89)a |
| Late child (aged 5 years to <13 years) | 1.11 (0.82–1.50) | 0.83 (0.63–1.10) |
| Adolescent (aged 13 years to <19 years) | Reference | Reference |
| Number of complex chronic conditions | ||
| 0 | Reference | Reference |
| 1 | 1.78 (1.52–2.09)a | 2.64 (2.19–3.17)a |
| 2 | 2.26 (1.87–2.73)a | 6.83 (5.55–8.42)a |
| ≥3 | 3.02 (2.34–3.90)a | 9.43 (7.17–12.41)a |
| Reflux-related principal diagnosis | ||
| Yes | 0.21 (0.18–0.25)a | 0.42 (0.36–0.49)a |
| No | Reference | Reference |
| History of previous fundoplication | ||
| Yes | 0.37 (0.24–0.56)a | 3.61 (2.58–5.05)a |
| No | Reference | Reference |
Variables included in the multilevel multivariate logistic regression analysis include fixed effects for surgery type (laparoscopic versus open), age group, gender, race/ethnicity, payer source, year of procedure, concurrent gastrostomy, neurological impairment, number of complex chronic conditions, principal diagnosis of reflux, history of fundoplication, and a random effect for hospital.
Statistically significant at the 0.05 level using a two-sided test.
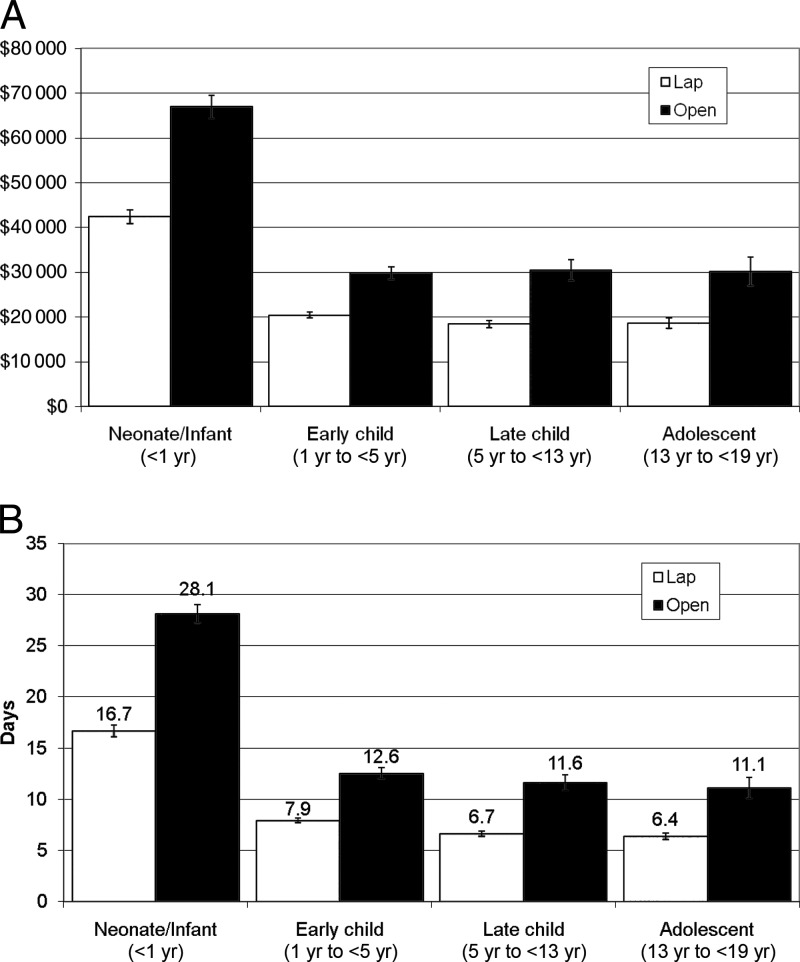
Table 4 shows estimates of the adjusted relationship between type of fundoplication and the continuous outcomes under study. The laparoscopic approach was associated with a 23% (e−0.26 − 1 = −0.23) reduction in total LOS, a 25% (e−0.29 − 1 = −0.25) reduction in postprocedure LOS, and a 16% (e−0.18 − 1 = −0.16) reduction in cost. After adjusting for surgical complications, infections, and LOS, the laparoscopic approach was associated with a statistically significant 5% decrease in total cost. LOS was the most influential of these factors in explaining the cost differential between open and laparoscopic fundoplication. Adjusting for infection and surgical complication, the laparoscopic approach was still associated a substantial (19%) reduction in total LOS. Finally, Fig 2A and B show adjusted-mean LOS and total cost by age group. Reductions in LOS and cost associated with the laparoscopic approach appear to be stable across the 4 age groups examined.
TABLE 4.
Variables Associated with Length of Stay and Cost
| Variable | Log LOS, n = 7083a |
Log Cost, n = 6125 |
||
|---|---|---|---|---|
| Total LOS | Postprocedure LOS | Total Costa | Total Cost: Model Including Infection, Complication, and LOSb | |
| Fundoplication | ||||
| Laparoscopic | −0.26 (0.021)c | −0.29 (0.018)c | −0.18 (0.024)c | −0.05 (0.017)c |
| Open | Reference | Reference | Reference | Reference |
| Surgical complication | ||||
| Yes | — | — | — | 0.13 (0.021)c |
| No | Reference | |||
| Infection | ||||
| Yes | — | — | — | 0.50 (0.021)c |
| No | Reference | |||
| Total LOS | — | — | — | 0.02 (<0.001)c |
| Age on day of fundoplication | ||||
| Neonate/infant (aged <1 year) | 0.55 (0.036)c | 0.26 (0.030)c | 0.39 (0.040)c | 0.19 (0.029)c |
| Early child (aged 1 year to <5 years) | 0.07 (0.035) | 0.01 (0.030) | −0.08 (0.039) | −0.08 (0.028)c |
| Late child (aged 5 years to <13 years) | 0.01 (0.038) | 0.01 (0.032) | −0.06 (0.042) | −0.08 (0.029)c |
| Adolescent (aged 13 years to <19 years) | Reference | Reference | Reference | Reference |
| Number of complex chronic conditions | ||||
| 0 | Reference | Reference | Reference | Reference |
| 1 | 0.21 (0.021)c | 0.16 (0.018)c | 0.24 (0.024)c | 0.15 (0.017)c |
| 2 | 0.44 (0.029)c | 0.40 (0.025)c | 0.51 (0.033)c | 0.23 (0.024)c |
| ≥3 | 0.63 (0.043)c | 0.62 (0.036)c | 0.73 (0.049)c | 0.29 (0.035)c |
| Reflux-related principal diagnosis | ||||
| Yes | −0.92 (0.021)c | −0.44 (0.018)c | −0.96 (0.024)c | −0.46 (0.018)c |
| No | Reference | Reference | Reference | Reference |
| History of previous fundoplication | ||||
| Yes | −0.41 (0.054)c | −0.18 (0.046)c | −0.37 (0.059)c | −0.11 (0.042)c |
| No | Reference | Reference | Reference | Reference |
Regression coefficients and SEs are reported. Regression coefficients were obtained from multilevel, multivariate log-linear regression models.
Variables included in the multilevel multivariate log-linear regression analysis include fixed effects for surgery type (laparoscopic versus open), age group, gender, race/ethnicity, payer source, year of procedure, concurrent gastrostomy, neurological impairment, number of complex chronic conditions, principal diagnosis of reflux, history of fundoplication, and a random effect for hospital.
Model controls for all variables listed above as well as infection, surgical complication, and LOS.
Statistically significant at the 0.05 level using a two-sided test.
FIGURE 2.
A, Adjusted mean total cost of laparoscopic and open fundoplication by age group. All costs reported as means with 95% confidence intervals in 2008 US dollars. B, Adjusted mean length of stay for laparoscopic and open fundoplication by age group. Mean length of stay reported with 95% confidence intervals. Variables included in the multilevel multivariate regression analysis were fixed effects for surgery type (laparoscopic versus open), age group, gender, race/ethnicity, payer source, year of procedure, concurrent gastrostomy, neurological impairment, number of complex chronic conditions, principal diagnosis of reflux, history of fundoplication, and a random effect for hospital.
Physician and Hospital-Level Variation
The subspecialty of the principal physician associated with each admission was reported for 86% of the study patients. The physician subspecialty was reported as “pediatric surgeon” in over 83% of the admissions, and the remainder of admissions was associated with physicians of various subspecialties listed in Appendix 3. Unique identification of pediatric surgeons (n = 291 pediatric surgeons) within hospitals allowed for examination of both physician- and hospital-level variation. When accounting for clustering at both the physician and hospital levels, less than 1% of the total variation in infection and just over 2% in surgical complication was attributable to variation between physicians after adjustment for patient level factors. For both cost and LOS, the total variation attributable to physicians was 3%. Over the 4 years examined, the majority of pediatric surgeons (66%) performed both open and laparoscopic fundoplication, whereas 14% performed laparoscopic exclusively and 20% performed open surgery exclusively. In 2008, the percentage of pediatric surgeons performing laparoscopic fundoplication exclusively reached a peak of 28%. When we modeled the choice of open versus laparoscopic fundoplication, we found that 59% of the variation was explained at the level of the patient, 26% at the level of the surgeon, and 15% at the level of the hospital. Variation between hospitals accounted for 5% of the total variation in both cost and LOS.
Temporal Trends
Over the observation period, laparoscopic fundoplications as a portion of total fundoplications increased from a low of 51% in 2005 to a high of 63% in 2008 (P < .001). As the rate of laparoscopic fundoplications increased, there was no evidence of a concomitant rise in the overall fundoplication rate. In 2005, there were 6.7 principal fundoplications per 1000 hospital procedures compared with 5.4 in 2008 (correlation −0.98, P = .02). The number of fundoplications per 1000 admissions showed a similar downward trend (correlation −0.98, P = .02).
DISCUSSION
This study is the first to use data from the PHIS network to examine laparoscopic fundoplication and its association with quality and cost outcomes. A number of single-center retrospective studies have examined patient outcomes by type of pediatric fundoplication. For instance, Somme et al5 examined 55 infants who underwent fundoplication from 1996 through 2000 and found that the time to initiation of feeding postoperatively was shorter in the laparoscopic group. Mattioili et al4 examined a group of 66 children who underwent fundoplication from 1993 through 1997 and found a lower postoperative LOS in the laparoscopic group. Diaz et al3 examined 762 patients and found evidence that open fundoplication resulted in lower reoperation rates than the laparoscopic approach. These and similar studies2,17–19 have added to our knowledge, but all suffered from shortcomings of some kind, including the inherent bias in analyzing one's own work, the uncontrolled nature of the patient selection, and the lack of a standard set of outcome measures. In contrast, we used a large, multicenter dataset, attempted to control for case mix using multiple methods, and examined standard outcome measures.
We found that the laparoscopic approach is the most prevalent form of antireflux surgery in the population studied, but open fundoplication was more common among children who were less than 1 year old. In addition, we found that patients on whom the laparoscopic procedure was performed had fewer surgical complications and infections, shorter LOS, and lower cost of care than their counterparts who had open fundoplication, although their unadjusted per-day costs were higher. Multivariate regression analysis confirmed that the laparoscopic approach was associated with lower risks of surgical complication and infection as well as shorter LOS. In addition, the multivariate regression analysis showed that laparoscopic fundoplication was associated with lower total cost of care, but the strength of this association was substantially reduced when LOS, surgical complication, and infection were added to the estimating model, consistent with the hypothesis that these are important mediating factors.
It is known that children with neurologic impairment present an enormous challenge with regard to fundoplication. They suffer more reflux- and aspiration-related morbidity and have higher surgical complication rates from fundoplication.9,20,21 Our results were consistent with those of previous studies. Specifically, we found that neurologic impairment or complex chronic conditions increased the odds of infection and surgical complication. In addition, they showed that the laparoscopic approach was associated with fewer surgical complications for children with neurologic impairment.
We found substantial variation across hospitals in the use of the laparoscopic procedure. At the same time, most of the hospitals studied showed a consistent trend toward more procedures being performed laparoscopically. Publicly available data from Health Care Cost and Utilization Project show that in 2006 ∼44% of all pediatric fundoplications in the United States were performed in the laparoscopic fashion.12 This is ∼8 percentage points lower than what we found in the PHIS data. If we assume that the PHIS database is sentinel in nature, patients seen at general hospitals and children's units may see a rise in the percentage of fundoplications done laparoscopically.
Our physician-level data may have important training implications. We showed that there is a cadre of pediatric surgeons who do not utilize the laparoscopic approach and that the variation in the choice of procedure was associated with the individual surgeon. If the superiority of the laparoscopic technique is confirmed in prospective studies, this group of surgeons may benefit from additional training.
We sought to determine whether the introduction of the laparoscope technique resulted in an increase in the overall utilization of fundoplication. Early experience with adult laparoscopic cholecystectomy provides a cautionary tale: there was a 17% increase in total inpatient spending for gall bladder surgery because the threshold for performing the procedure was lowered.22 Our data are reassuring: laparoscopic fundoplication is associated with lower adjusted hospital costs, and yet the threshold for performing the procedure does not seem to have shifted.
Limitations
Our data source does not include all pediatric fundoplications performed in the country, and this could limit its generalizability. Moreover, the PHIS database is based on administrative records, which have important limitations, including possible coding errors and the inability to randomize. Our sample excluded patients whose primary surgical procedure was not fundoplication, and, therefore, we cannot draw conclusions about these patients. Our analysis had a look-back period of 5 years, but not all hospitals contributed data during the look-back period; as a result, the history of previous fundoplication was underestimated. The PHIS database has no information on physician charges, which would impact the overall cost of the procedure, and it is possible that some pediatric surgeons moved from one participating hospital to another. Decisions about short gastric-vessel division, the tightness of the wrap, crural dissection and repair, and partial fundoplications could not be determined but may have impacted outcomes. Finally, we were unable to account for any procedures that were “converted” from a laparoscopic to open approach intraoperatively.
CONCLUSIONS
In a large study of children's hospitals, laparoscopic fundoplication was associated with improved clinical outcomes compared with the open procedure, even after adjustment for patient severity. Laparoscopic fundoplication has become the most common form of antireflux surgery performed on children over 1 year of age at representative children's hospitals, but this has not been associated with an increase in the overall utilization of the fundoplication procedure. These data have important implications for clinical practice and surgical training and underline the importance of additional comparative effectiveness research in the examination of pediatric surgical outcomes.
ACKNOWLEDGMENTS
This investigation was funded by a grant (D55HP05157) from the Department of Health and Human Services, Health Resources and Services Administration to the Department of Pediatrics, School of Medicine, University of Colorado, Denver, Colorado.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Department of Health and Human Services.
The authors thank the Colorado Health Outcomes Program and the Children's Outcomes Research Program for their assistance.
Appendix 1.
Top Ten Principal Procedures of Admissions That had a Fundoplication (n = 10 213)
| ICD-9 Code | Description | Frequency | Percent |
|---|---|---|---|
| 44.67 | Laparoscopic procedures for creation of esophagogastric sphincteric competence | 4062 | 39.77 |
| 44.66 | Other procedures for creation of esophagogastric sphincteric competence | 3209 | 31.42 |
| 53.7 | Repair of diaphragmatic hernia, abdominal approach | 324 | 3.17 |
| 31.1 | Temporary tracheostomy | 215 | 2.11 |
| 39.0 | Systemic to pulmonary artery shunt | 159 | 1.56 |
| 38.85 | Other surgical occlusion of vessels NEC | 145 | 1.42 |
| 39.65 | Extracorporeal membrane oxygenation | 128 | 1.25 |
| 42.7 | Esophagomyotomy | 108 | 1.06 |
| 31.29 | Other permanent tracheostomy | 96 | 0.94 |
| 96.72 | Continuous mechanical ventilation for 96 hours or more | 75 | 0.73 |
Appendix 2.
Diagnostic Codes Used for “Reflux-Related Principal Diagnosis” Variable (n = 4411)
| ICD-9 Code | Description | Frequency | Percent |
|---|---|---|---|
| 530.10 | Esophagitis, unspecified | 19 | 0.43 |
| 530.11 | Reflux esophagitis | 109 | 2.47 |
| 530.12 | Acute esophagitis | 0 | – |
| 530.19 | Other esophagitis | 20 | 0.45 |
| 530.81 | Esophageal reflux | 4247 | 96.28 |
| 536.2 | Persistent vomiting | 3 | 0.07 |
| 536.8 | Dyspepsia/Other specified disorders of stomach function | 4 | 0.09 |
| 787.03 | Vomiting alone | 9 | 0.20 |
| 787.1 | Heartburn | 0 | – |
Appendix 3.
Principal Physician Specialty Associated with PHIS Fundoplication Admission (n = 7083)
| Frequency | Percent | |
|---|---|---|
| Pediatric surgery | 5911 | 83.45 |
| Not reported/specified | 989 | 13.96 |
| Orthopedic surgery | 60 | 0.85 |
| General pediatrics | 49 | 0.69 |
| Pulmonology | 25 | 0.35 |
| Gastroenterology | 12 | 0.17 |
| Neonatologist | 8 | 0.11 |
| Cardiologist | 7 | 0.10 |
| Otolaryngologist | 6 | 0.08 |
| Plastic surgery | 4 | 0.06 |
| Critical care | 3 | 0.04 |
| Nephrology | 2 | 0.03 |
| Psychiatry | 2 | 0.03 |
| Dermatology | 1 | 0.01 |
| Endocrinology | 1 | 0.01 |
| Genetics | 1 | 0.01 |
| Radiology | 1 | 0.01 |
| Neurosurgery | 1 | 0.01 |
FINANCIAL DISCLOSURE: The authors have indicated that they have no personal financial relationships relevant to this article to disclose.
- ICD-9
- International Classification of Diseases, Version 9
- LOS
- length of stay
- PHIS
- Pediatric Health Information System
REFERENCES
- 1. HCUPnet, Healthcare Cost and Utilization Project 2006 Agency for Healthcare Research and Quality, Rockville, MD: Agency for Healthcare Research and Quality (AHRQ). [serial online] 2008;Accessed January 10, 2010 [Google Scholar]
- 2. Barsness KA, Feliz A, Potoka DA, Gaines BA, Upperman JS, Kane TD. Laparoscopic versus open Nissen fundoplication in infants after neonatal laparotomy. JSLS. 2007;11(4):461–465 [PMC free article] [PubMed] [Google Scholar]
- 3. Diaz DM, Gibbons TE, Heiss K, Wulkan ML, Ricketts RR, Gold BD. Antireflux surgery outcomes in pediatric gastroesophageal reflux disease. Am J Gastroenterol. 2005;100(8):1844–1852 [DOI] [PubMed] [Google Scholar]
- 4. Mattioli G, Repetto P, Carlini C, et al. Laparoscopic vs open approach for the treatment of gastroesophageal reflux in children. Surg Endosc. 2002;16(5):750–752 [DOI] [PubMed] [Google Scholar]
- 5. Somme S, Rodriguez JA, Kirsch DG, Liu DC. Laparoscopic versus open fundoplication in infants. Surg Endosc. 2002;16(1):54–56 [DOI] [PubMed] [Google Scholar]
- 6. Rangel SJ, Henry MC, Brindle M, Moss RL. Small evidence for small incisions: pediatric laparoscopy and the need for more rigorous evaluation of novel surgical therapies. J Pediatr Surg. 2003;38(10):1429–1433 [DOI] [PubMed] [Google Scholar]
- 7. Finlayson SR, Laycock WS, Birkmeyer JD. National trends in utilization and outcomes of antireflux surgery. Surg Endosc. 2003;17(6):864–867 [DOI] [PubMed] [Google Scholar]
- 8. Lobe TE, Schropp KP, Lunsford K. Laparoscopic Nissen fundoplication in childhood. J Pediatr Surg. 1993;28(3):358–360 [DOI] [PubMed] [Google Scholar]
- 9. Goldin AB, Garrison M, Christakis D. Variations between hospitals in antireflux procedures in children. Arch Pediatr Adolesc Med. 2009;163(7):658–663 [DOI] [PubMed] [Google Scholar]
- 10. Lasser MS, Liao JG, Burd RS. National trends in the use of antireflux procedures for children. Pediatrics. 2006;118(5):1828–1835 [DOI] [PubMed] [Google Scholar]
- 11. Gerber JS, Coffin SE, Smathers SA, Zaoutis TE. Trends in the incidence of methicillin-resistant Staphylococcus aureus infection in children's hospitals in the United States. Clin Infect Dis. 2009;49(1):65–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. HCUPnet, Healthcare Cost and Utilization Project Agency for Healthcare Research and Quality, Rockville, MD: Agency for Healthcare Research and Quality (AHRQ). [serial online] 2006;Accessed January 10, 2010 [Google Scholar]
- 13. Archived Consumer Price Index Detailed Report Information Bureau of Labor Statistics, Department of Labor. [serial online] 2010; Accessed September 11, 2009 [Google Scholar]
- 14. Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980–1997. Pediatrics. 2000;106(1 pt 2):205–209 [PubMed] [Google Scholar]
- 15. Stock JH, Watson MW. Introduction to econometrics. Boston, MA: Addison Wesley, 2003 [Google Scholar]
- 16. Duan N. Smearing Estimate: A Nonparametric Retransformation Method. J Am Stat Assoc. 78:605–610 [Google Scholar]
- 17. Meehan JJ, Georgeson KE. Laparoscopic fundoplication in infants and children. Surg Endosc. 1996;10(12):1154–1157 [DOI] [PubMed] [Google Scholar]
- 18. Rothenberg SS. Laparoscopic Nissen procedure in children. Semin Laparosc Surg. 2002;9(3):146–152 [PubMed] [Google Scholar]
- 19. Ostlie DJ, St Peter SD, Snyder CL, Sharp RJ, Andrews WS, Holcomb GW., III A financial analysis of pediatric laparoscopic versus open fundoplication. J Laparoendosc Adv Surg Tech A. 2007;17(4):493–496 [DOI] [PubMed] [Google Scholar]
- 20. Smith CD, Othersen HB, Jr, Gogan NJ, Walker JD. Nissen fundoplication in children with profound neurologic disability. High risks and unmet goals. Ann Surg. 1992;215(6):654–658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Vernon-Roberts A, Sullivan PB. Fundoplication versus post-operative medication for gastro-oesophageal reflux in children with neurological impairment undergoing gastrostomy. Cochrane Database Syst Rev. 2007;CD006151. [DOI] [PubMed] [Google Scholar]
- 22. Legorreta AP, Silber JH, Costantino GN, Kobylinski RW, Zatz SL. Increased cholecystectomy rate after the introduction of laparoscopic cholecystectomy. JAMA. 1993;270(12):1429–1432 [PubMed] [Google Scholar]