Abstract
OBJECTIVE:
The goal of this study was to examine activity pattern associations between Hispanic parents and their preschool-aged children.
METHODS:
We examined baseline data collected as part of a randomized controlled trial. Self-defined Hispanic parents with children aged 3 to 5 years were randomly assigned to either a weekly healthy lifestyle group (intervention) or a monthly school-readiness group (control) for 3 months. There were no weight eligibility criteria. All participants were instructed to wear an accelerometer for up to 7 consecutive days to measure physical activity.
RESULTS:
Of the 106 dyads enrolled in the study, 80 children and 85 parents provided useable actigraphy data. Mean percentage of time spent in sedentary behaviors was 82.0% (SD: 10.4) for parents and 69.8% (SD: 18.5) for preschool-aged children. Percentage of awake time per day spent in sedentary behavior was strongly correlated for parents and children (r = 0.597; P < .001). Correlations between activity level were large (r = 0.895 and 0.739 for low and moderate activity levels, respectively), except for vigorous activity level, for which the parent-child correlation was nonsignificant (P = .64) because of a near-0 level of vigorous parental activity. Child's age (P = .81) and gender (P = .43) were nonsignificant predictors of child activity levels.
CONCLUSIONS:
These results suggest that parental activity levels are a powerful explanation of preschool-aged child activity levels, except for vigorous activity, which children do on their own without parental participation. Hispanic parents play a critical role in setting physical activity patterns in their children.
Keywords: Hispanics, obesity, physical activity, preschoolers, parents
WHAT'S KNOWN ON THIS SUBJECT:
Little is known about how physical activity patterns are set in early childhood. Compared with black or white populations, Hispanics have the least amount of leisure time activity, yet there has been little research that has focused on the activity of preschool-aged Hispanic children.
WHAT THIS STUDY ADDS:
Results suggest that Hispanic parents of preschool-aged children set physical activity patterns at a time of critical development in early childhood. For Hispanic preschool-aged children, sedentary behavior seems to be the norm when Hispanic parents are sedentary themselves.
Increased adiposity and reduced physical activity (PA) have been shown to be strong and independent predictors of mortality from all causes.1–3 Overweight, defined as BMI > 25 for adults and ≥85th BMI percentile for children, depends on several environmental, behavioral, and genetic factors.4 At the most basic level, overweight is a consequence of an imbalance between energy intake and expenditure.
Routine PA represents a healthy body habitus that correlates to good health across the person's life span.5,6 However, patterns of PA vary significantly in different racial/ethnic groups. For example, compared with white and black populations, Hispanic adults are noted to have the least amount of leisure time activity.7 This holds true for Hispanic children as well. When adjusting for generation and acculturation level among 6- to 17-year-old Hispanics, 22.5% of immigrant children, 17.2% of US-born children with 2 immigrant parents, and 14.5% of US-born children with 1 immigrant parent, were physically inactive compared with 9.5% of US-born, non-Hispanic white children.8
Overweight parents tend to have overweight children.9–11 The presence of an obese mother or father increases their child's probability of being overweight or obese in young adulthood by a factor greater than 2.12 In fact, Wrotniak et al13 found that parent BMI z score is an independent predictor of child BMI z score. Parents can promote an obesogenic environment through their nutrition and activity patterns.14 However, it is unclear how PA patterns are set in early childhood.10 Dietz15 posited that the preschool period is a critical period for the development of obesity.
The purpose of our study was to examine the extent to which Hispanic parents' PA levels correlate with their preschool-aged child's PA patterns.
METHODS
Study Population and Design
This study was designed for Hispanic parents with young children and conducted at a local community center in Nashville, Davidson County, Tennessee. A total of 106 Hispanic parent-child (aged 3–5 years) dyads participated in a culturally sensitive, family-based obesity prevention randomized controlled trial (Salud con la familia [Health With the Family]). This study derives from baseline data. The intervention arm program curriculum incorporated the 4 key steps to healthy living: nutritious food and beverage consumption, appropriate portion size, regular PA, and positive parenting practices within a culturally sensitive and sustaining framework. Emphasis on building community and social networks, as well as providing access to a family recreational facility, was encouraged to create a stronger support system that would potentially promote long-term lifestyle and behavioral changes. Participants randomly assigned to the control arm met monthly to discuss how to prepare their child to be a successful bilingual student. The study inclusion criteria included: (1) self-defined Hispanic; (2) having a child aged 3 to 5 years; (3) not enrolled in another healthy lifestyle program(s); (4) being available for contact by telephone; and (5) planning on remaining in the city for the next 6 months. Prospective study participants (parents) provided consent in their language of choice (English or Spanish), and informed consent was read aloud and any questions were answered before obtaining written consent. Child consent was not obtained because of age; however, children were enrolled in research only when their parents or legal guardians provided consent and children clearly assented during data collection.16 The study was approved by the Vanderbilt University Institutional Review Board (institutional review board no. 080673).
Data Collection
All data on both the preschool-aged children and participating parents were collected by bilingual trained data collectors at the community center.
Measures
Physical Activity
PA was assessed by using the ActiGraph GT1M accelerometer (ActiGraph, LLC, Pensacola, FL). The ActiGraph is a small, lightweight monitor that is worn on an elastic belt around the waist and measures the intensity of PA associated with locomotion.17 In the present study, the device was programmed to record in continuous 10-second epochs to capture the short, spurt-like activity characteristic of young children. The monitor has been validated for use in preschool-aged and adult populations of Hispanics as well as other ethnicities and has been deemed an objective method of assessing PA levels.18–29 Both parent and child were instructed to wear the ActiGraph for 7 consecutive days during waking hours except when they showered or participated in aquatic activities. Monitors were returned to study staff and data were downloaded using manufacturer-provided software. Validated threshold values were used to derive time spent in rest, sedentary, light, moderate, and vigorous activity.23 The analysis of raw accelerometer data was performed separately for children and adults using a procedure similar to that used to analyze the National Health and Nutrition Examination Survey data.30
Height and Weight
Body weight was measured, while wearing light clothing without shoes after voiding, to the nearest 0.1 kg on a calibrated digital scale (model 758C) (Detecto, Webb City, MO). Body height without shoes was measured to the nearest 0.1 cm with the attached stadiometer. Measurements were collected at the community center by trained study staff.
Body Mass Index
BMI was calculated (weight [kg]/height [m2]).31 Because the amount of body fat varies for children according to age and between girls and boys, BMI percentiles for age and gender were calculated by using the Centers for Disease Control and Prevention calculator.
Demographic Characteristics
Parent participants completed a demographic survey in Spanish that included date of birth of parent and child, child's and parent's gender, highest parental education level, and country of origin of parent and child. Acculturation was measured using the widely used and previously validated Short Acculturation Scale for Hispanics (SASH).33 The SASH asks parents what language they speak, use at home, think in, and use among friends given the following options: Spanish only, Spanish better than English, Spanish and English equally, English better than Spanish, and English only. Scores can range from 1 to 5, and a score <2.99 indicates a low level of acculturation. An internal reliability of the SASH was r = 0.81 in our sample.
Statistical Analysis
After descriptive statistics, we examined Pearson correlations between parental and child PA levels. Given traditional assumptions (80% power, P < .05, 2-tailed), the study provided a minimum detectable effect size of r = 0.31.34 For correlations, Cohen35 describes small/medium/large effects as r = 0.1/0.3/0.5, which suggests that this study had the power to detect medium and large effects. In addition to correlations, we conducted an ordinary least squares linear regression on the child's overall level of PA (compared with inactivity) as a function of parental activity, child gender, and child age. As a precaution, the regression was repeated with a robust regression2,3 to confirm that the moderate nonnormality of activity level did not distort the significance tests.
The variables in Table 1 were tested to determine how actigraphy participants and those who declined participation differed. Parent and child characteristics were treated as binary (eg, Mexican 01) or ordinal. With multiple variables and 106 participants, multiple significance tests might produce false differences.4,5 To avoid this problem, we used a distribution-free bootstrap test6 to control for the false discoveries caused by multiple tests.36
TABLE 1.
Participant Demographic Characteristics
| Participants (N = 106 dyads), n (%) |
||
|---|---|---|
| Child | Parent | |
| Female gender | 54 (50.9) | 103 (97.2) |
| Weight categorya,b | ||
| Underweight | 3 (2.9) | 0 |
| Normal | 57 (54.8) | 21 (18.3) |
| Overweight | 20 (19.2) | 41 (39.4) |
| Obese | 24 (23.0) | 44 (42.3) |
| Country of origin | ||
| United States | 97 (91.5) | 6 (5.7) |
| Mexico | 8 (7.6) | 86 (81.1) |
| Other Latin American country | 1 (0.9) | 14 (13.2) |
| Highest education level | ||
| Less than high school | — | 26 (24.8) |
| Some high school, no diploma | — | 42 (40.0) |
| High school diploma/GED | — | 20 (19.1) |
| Some college, no degree | — | 10 (9.5) |
| College diploma | — | 7 (6.7) |
| Mean (SD), y | 4.2 (0.9) | 31.4 (5.5) |
| BMI percentile, mean (SD)b | 71.3 (26.8) | — |
| BMI, mean (SD)b | — | 30.0 (5.7) |
| SASH summary score, mean (SD) | — | 1.4 (0.55) |
GED indicates General Educational Development.
Child categories were defined by using the child BMI percentile adjusted for age and gender: underweight, ≤5th percentile; normal, >5th to <85th percentile; overweight, ≥85th to <95th percentile; obese, >95th percentile. Adult categories were defined by using the adult BMI: normal, BMI ≥ 18.5 to <25; overweight, BMI ≥25 to <30; and obese, BMI ≥ 30.
N = 104.
Physical Activity Data Analysis
The PA was obtained from ActiGraph GT1M accelerometer data collected as raw activity counts without imposition of any external criteria other than determination of wear and nonwear time assessed using criteria proposed by Troiano et al.37 A minimum of 4 hours of continuous monitoring for a child and 8 hours for a parent defined a valid day, and 1 day of simultaneous (parent and child) wearing was required for inclusion of a dyad in the data analysis. Time spent in PA intensities was based on activity counts: thresholds of <420 activity counts for sedentary, 420 to 1679 counts for light, 1680 to 3379 counts for moderate, and >3379 counts for vigorous intensity activity per minute.19 For adults, the thresholds were <500 counts for sedentary, 500 to 2019 counts for light, 2020 to 5999 counts for moderate, and >6000 counts for vigorous activity counts per minute.30 Time spent in sedentary behavior and PA (light, moderate, and vigorous) was determined by summing minutes in a day in which the count met the criterion for that intensity.
RESULTS
The study cohort included 106 parent-child dyads of mostly first-generation Mexican immigrant parents (81%) and second-generation preschool-aged children (92%). Among parents, almost two-thirds (65%) had not completed high school or received a General Educational Development equivalent. Almost all participating adults (97%) had a low level of acculturation, although the majority of them reported living in the United States for 5 to 14 years. Approximately 80% of participating parents were overweight/obese (BMI ≥ 25), and ∼42% of preschool-aged children were overweight/obese (BMI ≥ 85th percentile) (Table 1).
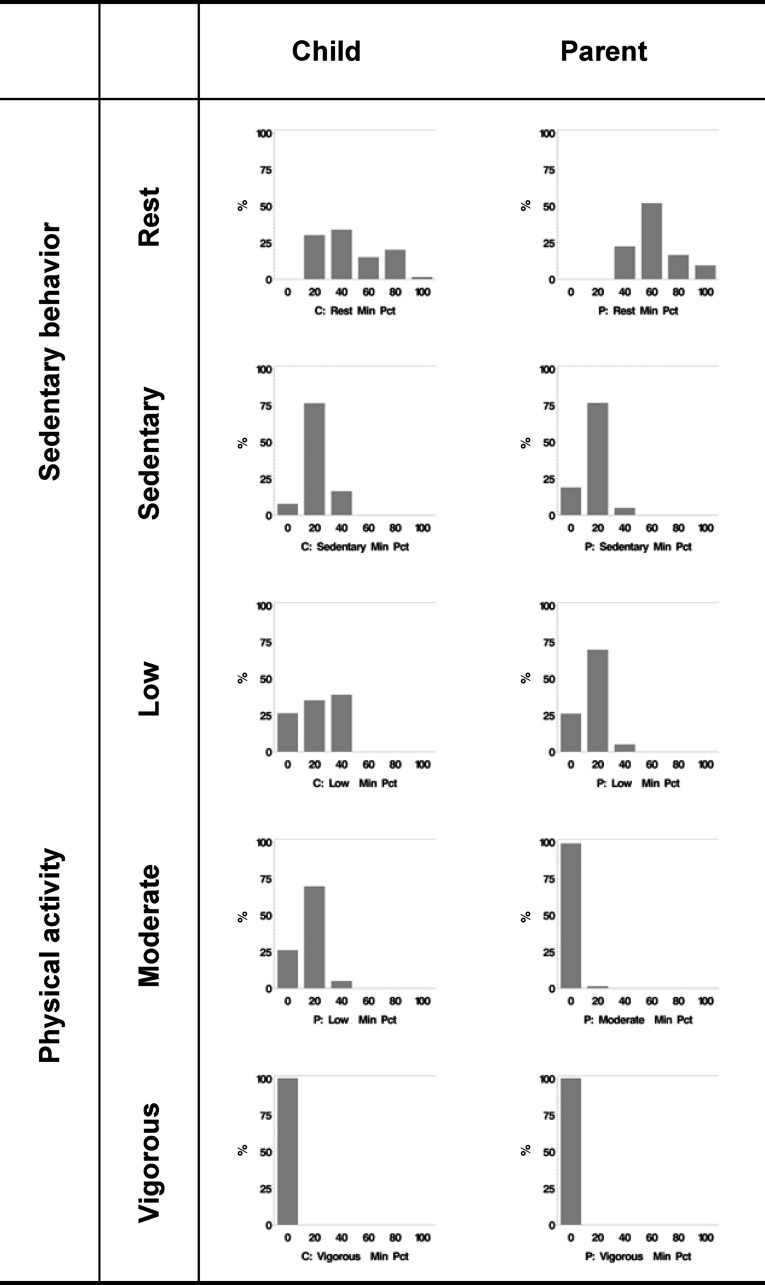
We report on 80 children and 85 parents who provided actigraphy data collected at baseline. The only difference noted between actigraphy participants and those who declined participation was parental BMI, which averaged 29 for volunteers and 33 for those who declined to participate (P = .01). For children, the mean ActiGraph wearing time per day was 491.8 minutes (SD: 172.2), for an average of 3.7 days (SD: 2.2). For adults, the mean ActiGraph wearing time was 530.3 minutes (SD: 187.1), for an average of 3.9 days (SD: 3.89). The total number of minutes per day spent in moderate/vigorous activity was 43.9 minutes (SD: 42.7) for children, representing 2% (SD: 4.5) of their wearing time. Figure 1 displays the time that parents and children spent in different forms of PA throughout their awake wearing time. There were statistically significant mean differences between parent and child sedentary behavior and PA levels such that parents were more sedentary and less physically active than their preschool-aged child (Table 2). However, the percentage of awake time per day spent in sedentary behavior was strongly correlated for parents and preschool-aged children (r = 0.597; P < .0001).
FIGURE 1.
Distribution of sedentary behavior and activity levels of Hispanic parents and their preschool-aged children. C indicates child; P, parent; Min Pct, minimum percentage.
TABLE 2.
Mean Comparison Between Parent and Child Sedentary Behavior and PA Levels
| Activity Level | Parent (N = 85) |
Child (N = 80) |
P | ||
|---|---|---|---|---|---|
| Mean, % | SD | Mean, % | SD | ||
| Sedentary | 82.0 | 10.4 | 69.8 | 18.5 | <.001 |
| Active | 18.0 | 10.4 | 30.1 | 18.5 | <.001 |
| Low | 5.2 | 9.2 | 7.2 | 12.3 | <.001 |
| Moderate | 0.9 | 1.8 | 1.9 | 3.7 | <.001 |
| Vigorous | 0. | 0.5 | 1.5 | 1.9 | 0.64 |
Parent-child Pearson correlations in activity level were significant and large for low (r = 0.895; P < .0001) and moderate (r = 0.739; P < .0001) PA levels but not for vigorous PA levels (r = −.07; P = .56). When correlations were broken out by child age brackets (2–3 years, 4 years, and 5–6 years), the results were unchanged. To understand the low correlation between parent and child vigorous PA levels, we examined the means of vigorous activity, which were close to floors of 0 for both parents (0.1%) and children (1.5%). Because these values were so close to 0, they have almost no variance and therefore cannot correlate with each other.
For a more general look at overall PA, we calculated proportion of activity out of a total (activity + inactivity). Averages for this total were 31% for children and 18% for parents; ranges were 2% to 66% for children and 1% to 48% for adults. This outcome had significant nonnormality for both children (P < .0001) and parents (P = .008). The parent-child correlation in overall PA was Pearson r = 0.61 (Spearman ρ = 0.58), a “large” correlation according to the guidelines of Cohen.35 In the linear regression, the effect of parental activity was significant (P < .0001), but the effects of child's age (P = .81) and gender (P = .43) were not. Because activity was not normally distributed, we replicated the analysis with a robust regression model.2,3 Extremely similar results suggested that the parent-child correlation in activity was real.
DISCUSSION
Our study revealed a strong and positive correlation between Hispanic parents and their preschool-aged children's daily sedentary, mild, and moderate PA levels. Few studies have examined the correlation in sedentary behavior or PA levels between parents and their children of any age or ethnicity when objectively measured using accelerometry. It seemed that children partook in vigorous activity independent of parental participation. The parental floor effect explains the low parent-child correlations for vigorous activity. For parents, the near-perfect lack of vigorous activity is essentially a constant; it contains little variance rather than a variable capable of correlating with other variables.
In the FLAME Study conducted in New Zealand, Actical accelerometers (Mini-Mitter, Bend, OR) were worn for 5 consecutive days by parents and their child (ages 3, 4, and 5 years). Parental mild and moderate activity were found to be weakly correlated to their child's PA at ages 3 (r = 0.17; P = 0.034) and 4 (r = 0.28; P = .051) years. Although this study was conceptually very similar to ours, the study population was very different, which may explain why PA was only found to be weakly correlated.
In another study, Actiwatch (Mini-Mitter) accelerometers were worn for 3 consecutive days among 4- to 19-year-old Hispanic children to assess PA levels.39 Within this cohort, PA declined markedly with age and was consistently higher in boys versus girls (P < .01). Although this study did not examine correlations with parental PA, it did suggest that at some point, a significant difference develops in activity levels among female and male Hispanic children. This study also implied that the alarmingly high levels of sedentary behavior, seen in our study population of preschool-aged children, will continue to grow as they become older.
This same study demonstrated that when PA was objectively measured using accelerometry, it varied by age and gender among children.39 Boys, even at the preschool age, were significantly more active than girls.37,39–41 However, we found that PA did not vary by age or gender among Hispanic preschool-aged children. This could represent a shift in normative behavior for second-generation preschool-aged children in the United States.
Pediatric obesity has become a national crisis. Today, an alarming 16.3% of US children aged 2 to 19 years are overweight (BMI 85th to 94th percentile) and 15.6% are obese (BMI ≥ 95th percentile).42 Although pediatric obesity has become a nationwide problem, Hispanic youth, specifically Mexican Americans, are disproportionally affected. Among Mexican American children aged 2 to 19 years, 17.1% and 20.9% are clinically overweight and obese, respectively.43 The Hispanic population is the largest and fastest growing minority population in the United States, and by 2030 it is estimated that it will comprise 30% of the total population.43
Approximately 30% of Mexican American children 2 to 5 years of age are already overweight or obese, whereas the national average remains at ∼24.5%.42 These striking figures should not be taken lightly. Overweight and obese status established by preschool has been found to persist into adolescence and adulthood.44 The Centers for Disease Control and Prevention recommends that children and adolescents participate in at least 60 minutes of moderate-intensity PA each day and that adults participate in at least 2.5 hours of moderate-intensity PA and 2 hours of strength training every week.45 A recent review article found that when objectively measured, habitual PA is low and sedentary behavior is high among preschool-aged children, so much so that most children are not meeting the recommended 60 minutes per day of PA during this critical period of human development.46
Activity habits established in early childhood can profoundly influence lifelong trajectories for BMI and health. Longitudinal data from the Framingham Children's Study, collected from preschool-aged children over the span of 8 years, found that increased levels of PA leads to less body fat acquisition during adolescence.5 Other studies have found similar protective effects of PA on the development of obesity throughout periods of critical development in childhood.47–49 These data suggest that establishing normative patterns of PA early in preschool-aged years may prevent adiposity rebound and rapid BMI weight gain in early childhood, factors that are known to be associated with later adult mortality and morbidity.50–52 Establishing routine PA that includes both parents and children earlier in childhood may lead to sustained healthier outcomes later in life. Our study indicates that Hispanic parents' PA levels are powerful in predicting their preschool-aged children's PA levels. Interventions should target both parents and children to change early normative PA behaviors.
STRENGTHS AND LIMITATIONS
Our study has several strengths and some limitations that have to be considered when interpreting the results. Strengths of the study include our unique recent immigrant population with a relatively high ratio (42%) of overweight/obese children. Another strength includes the use of an objective measure of PA in the same time for parent-child dyads. Limitations include relatively short time of observation (1–7 days). The minimum was 1 day of simultaneous (parent and child) monitoring. However, the average wearing time of 4.1 days for children (minimum, 1; maximum, 7) and 4.3 days (minimum, 1; maximum, 8) for parents was similar to that in other studies of Hispanic children.39,53 Also, we assumed that average daily PA counts reflected all physical activities performed by a child or parent. Although accelerometers are considered a relatively objective measure of PA under free-living conditions,54 it is known that they do not adequately measure body movements of upper and lower extremities, which may be especially important in young children.
One threat to the study's generalizability is that some parents declined actigraphic measurement; however, in analysis the only significant difference identified was for parental BMI. This finding suggests that heavier adults may be more reluctant to permit monitoring of their activity level and that of their children.
By design, the ActiGraph accelerometers are not waterproof and thus are unable to record PA levels in aquatic environments. Thus, among our study cohort, we could not accurately measure how much aquatic activities affected our assessment. However, we did ask parents to document if their child participated in an aquatic form of PA, and from those who returned forms, <5% reported any aquatic activities during the measurement period.
The impact of acculturation on PA level could not be assessed in this study because 81% of the parent participants were first-generation immigrants and 97% had a low level of acculturation as measured by the SASH.
CONCLUSIONS
In Hispanic preschool-aged children, sedentary behavior already seems to be the norm when Hispanic parents are sedentary themselves. Conversely, preschool-aged children are more likely to engage in mild and moderate PA if their parent does. Hispanic parents of preschool-aged children set PA patterns at a time of critical development in early childhood.
ACKNOWLEDGMENTS
This study was funded by the state of Tennessee (Project Diabetes Implementation grant GR-09-25517-00 [Dr Barkin, principal investigator]), Vanderbilt CTSA (National Center for Research Resources/National Institutes of Health) grant 1 UL1 RR024975, and Vanderbilt Diabetes Research and Training Center grant DK20593 from the National Institutes of Health.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
COMPANION PAPER: A companion to this article can be found on page 881 and online at www.pediatrics.org/cgi/doi/10.1542/peds.2010-3218.
- PA
- physical activity
- SASH
- Short Acculturation Scale for Hispanics
REFERENCES
- 1. Hu FB, Willett WC, Li T, Stampfer MJ, Colditz GA, Manson JE. Adiposity as compared with physical activity in predicting mortality among women. N Engl J Med. 2004;351(26):2694–2703 [DOI] [PubMed] [Google Scholar]
- 2. Koster A, Harris TB, Moore SC, et al. Joint associations of adiposity and physical activity with mortality: the National Institutes of Health-AARP Diet and Health Study. Am J Epidemiol. 2009;169(11):1344–1351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW., Jr Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341(15):1097–1105 [DOI] [PubMed] [Google Scholar]
- 4. Stovitz SD, Schwimmer JB, Martinez H, Story MT. Pediatric obesity: the unique issues in Latino-American male youth. Am J Prev Med. 2008;34(2):153–160 [DOI] [PubMed] [Google Scholar]
- 5. Moore LL, Gao D, Bradlee ML, et al. Does early physical activity predict body fat change throughout childhood? Prev Med. 2003;37(1):10–17 [DOI] [PubMed] [Google Scholar]
- 6. Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ. 2006;174(6):801–809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Crespo CJ, Smit E, Andersen RE, Carter-Pokras O, Ainsworth BE. Race/ethnicity, social class and their relation to physical inactivity during leisure time: results from the Third National Health and Nutrition Examination Survey, 1988–1994. Am J Prev Med. 2000;18(1):46–53 [DOI] [PubMed] [Google Scholar]
- 8. Singh GK, Yu SM, Siahpush M, Kogan MD. High levels of physical inactivity and sedentary behaviors among US immigrant children and adolescents. Arch Pediatr Adolesc Med. 2008;162(8):756–763 [DOI] [PubMed] [Google Scholar]
- 9. Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379 [DOI] [PubMed] [Google Scholar]
- 10. Crossman A, Anne Sullivan D, Benin M. The family environment and American adolescents' risk of obesity as young adults. Soc Sci Med. 2006;63(9):2255–2267 [DOI] [PubMed] [Google Scholar]
- 11. Wareham NJ, van Sluijs EM, Ekelund U. Physical activity and obesity prevention: a review of the current evidence. Proc Nutr Soc. 2005;64(2):229–247 [DOI] [PubMed] [Google Scholar]
- 12. Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869–873 [DOI] [PubMed] [Google Scholar]
- 13. Wrotniak BH, Epstein LH, Paluch RA, Roemmich JN. Parent weight change as a predictor of child weight change in family-based behavioral obesity treatment. Arch Pediatr Adolesc Med. 2004;158(4):342–347 [DOI] [PubMed] [Google Scholar]
- 14. Müller MJ, Danielzik S, Pust S. School- and family-based interventions to prevent overweight in children. Proc Nutr Soc. 2005;64(2):249–254 [DOI] [PubMed] [Google Scholar]
- 15. Dietz WH. Periods of risk in childhood for the development of adult obesity: what do we need to learn? J Nutr. 1997;127(9):1884S–1886S [DOI] [PubMed] [Google Scholar]
- 16. Office of Human Subjects Research, National Institutes of Health Regulations and Ethical Guidelines. Bethesda, MD: US Department of Health and Human Services; 2005. Available at: http://ohsr.od.nih.gov/guidelines/45cfr46.html Accessed March 2011 [Google Scholar]
- 17. Choi L, Chen KY, Acra SA, Jr, Buchowski MS. Distributed lag and spline modeling for predicting energy expenditure from accelerometry in youth. J Appl Physiol. 2010;108(2):314–327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Swartz AM, Strath SJ, Bassett DR, Jr, O'Brien WL, King GA, Ainsworth BE. Estimation of energy expenditure using CSA accelerometers at hip and wrist sites. Med Sci Sports Exerc. 2000;32(9 suppl):S450–S456 [DOI] [PubMed] [Google Scholar]
- 19. Pate RR, Almeida MJ, McIver KL, Pfeiffer KA, Dowda M. Validation and calibration of an accelerometer in preschool children. Obesity (Silver Spring). 2006;14(11):2000–2006 [DOI] [PubMed] [Google Scholar]
- 20. Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc accelerometer. Med Sci Sports Exerc. 1998;30(5):777–781 [DOI] [PubMed] [Google Scholar]
- 21. Bassett DR, Jr, Ainsworth BE, Swartz AM, Strath SJ, O'Brien WL, King GA. Validity of four motion sensors in measuring moderate intensity physical activity. Med Sci Sports Exerc. 2000;32(9 suppl):S471–S480 [DOI] [PubMed] [Google Scholar]
- 22. Welk GJ, Blair SN, Wood K, Jones S, Thompson RW. A comparative evaluation of three accelerometry-based physical activity monitors. Med Sci Sports Exerc. 2000;32(9 suppl):S489–S497 [DOI] [PubMed] [Google Scholar]
- 23. Puyau MR, Adolph AL, Vohra FA, Butte NF. Validation and calibration of physical activity monitors in children [published correction appears in Obes Res. 2006;14(3):528]. Obes Res. 2002;10(3):150–157 [DOI] [PubMed] [Google Scholar]
- 24. Trost SG, Way R, Okely AD. Predictive validity of three ActiGraph energy expenditure equations for children. Med Sci Sports Exerc. 2006;38(2):380–387 [DOI] [PubMed] [Google Scholar]
- 25. Schmitz KH, Treuth M, Hannan P, et al. Predicting energy expenditure from accelerometry counts in adolescent girls. Med Sci Sports Exerc. 2005;37(1):155–161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. de Vries SI, Bakker I, Hopman-Rock M, Hirasing RA, van Mechelen W. Clinimetric review of motion sensors in children and adolescents. J Clin Epidemiol. 2006;59(7):670–680 [DOI] [PubMed] [Google Scholar]
- 27. Brage S, Wedderkopp N, Andersen LB, Froberg K. Influence of step frequency on movement intensity predictions with the CSA accelerometer: a field validation study in children. Pediatr Exer Sci. 2003;35(5):277–287 [Google Scholar]
- 28. Treuth MS, Schmitz K, Catellier DJ, et al. Defining accelerometer thresholds for activity intensities in adolescent girls. Med Sci Sports Exerc. 2004;36(7):1259–1266 [PMC free article] [PubMed] [Google Scholar]
- 29. Mattocks C, Leary S, Ness A, et al. Calibration of an accelerometer during free-living activities in children. Int J Pediatr Obes. 2007;2(4):218–226 [DOI] [PubMed] [Google Scholar]
- 30. Tudor-Locke C, Johnson WD, Katzmarzyk PT. Accelerometer-determined steps per day in US adults. Med Sci Sports Exerc. 2009;41(7):1384–1391 [DOI] [PubMed] [Google Scholar]
- 31. Mei Z, Grummer-Strawn LM, Pietrobelli A, Goulding A, Goran MI, Dietz WH. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. Am J Clin Nutr. 2002;75(6):978–985 [DOI] [PubMed] [Google Scholar]
- 32. Centers for Disease Control and Prevention BMI calculator for child and teen: English version. Available at: http://apps.nccd.cdc.gov/dnpabmi/Calculator.aspx Accessed December 6, 2007
- 33. Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a Short Acculturation Scale for Hispanics. Hisp J Behav Sci. 1987;9(2):183–205 [Google Scholar]
- 34. Cohen J. A power primer. Psychol Bull. 1992;112(1):155–159 [DOI] [PubMed] [Google Scholar]
- 35. Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry. 2006;63(5):484–489 [DOI] [PubMed] [Google Scholar]
- 36. Westfall P, Tobias R, Rom D, Wolfinger R, Hochberg Y. Multiple Comparisons and Multiple Tests Using the SAS System. Cary, NC: SAS Publishing; 1999 [Google Scholar]
- 37. Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188 [DOI] [PubMed] [Google Scholar]
- 38. Taylor RW, Murdoch L, Carter P, Gerrard DF, Williams SM, Taylor BJ. Longitudinal study of physical activity and inactivity in preschoolers: the FLAME study. Med Sci Sports Exerc. 2009;41(1):96–102 [DOI] [PubMed] [Google Scholar]
- 39. Butte NF, Puyau MR, Adolph AL, Vohra FA, Zakeri I. Physical activity in nonoverweight and overweight Hispanic children and adolescents. Med Sci Sports Exerc. 2007;39(8):1257–1266 [DOI] [PubMed] [Google Scholar]
- 40. Van Der Horst K, Paw MJ, Twisk JW, Van Mechelen W. A brief review on correlates of physical activity and sedentariness in youth. Med Sci Sports Exerc. 2007;39(8):1241–1250 [DOI] [PubMed] [Google Scholar]
- 41. Pate RR, Pfeiffer KA, Trost SG, Ziegler P, Dowda M. Physical activity among children attending preschools. Pediatrics. 2004;114(5):1258–1263 [DOI] [PubMed] [Google Scholar]
- 42. Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299(20):2401–2405 [DOI] [PubMed] [Google Scholar]
- 43. US Census Bureau An older and more diverse nation by midcentury. Available at: www.census.gov/Press-Release/www/releases/archives/population/012496.html Accessed December 22, 2010
- 44. Nader PR, O'Brien M, Houts R, et al. Identifying risk for obesity in early childhood. Pediatrics. 2006;118(3). Available at: www.pediatrics.org/cgi/content/full/118/3/e594 [DOI] [PubMed] [Google Scholar]
- 45. US Department of Health and Human Services Physical Activity Guidelines for Americans. Available at: www.health.gov/paguidelines Accessed July 20, 2009
- 46. Reilly JJ. Physical activity, sedentary behaviour and energy balance in the preschool child: opportunities for early obesity prevention. Proc Nutr Soc. 2008;67(3):317–325 [DOI] [PubMed] [Google Scholar]
- 47. Moore LL, Nguyen US, Rothman KJ, Cupples LA, Ellison RC. Preschool physical activity level and change in body fatness in young children. The Framingham Children's Study. Am J Epidemiol. 1995;142(9):982–988 [DOI] [PubMed] [Google Scholar]
- 48. Klesges RC, Klesges LM, Eck LH, Shelton ML. A longitudinal analysis of accelerated weight gain in preschool children. Pediatrics. 1995;95(1):126–130 [PubMed] [Google Scholar]
- 49. Berkowitz RI, Agras WS, Korner AF, Kraemer HC, Zeanah CH. Physical activity and adiposity: a longitudinal study from birth to childhood. J Pediatr. 1985;106(5):734–738 [DOI] [PubMed] [Google Scholar]
- 50. Baker DW. The meaning and the measure of health literacy. J Gen Intern Med. 2006;21(8):878–883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Barker DJ, Osmond C, Forsén TJ, Kajantie E, Eriksson JG. Trajectories of growth among children who have coronary events as adults. N Engl J Med. 2005;353(17):1802–1809 [DOI] [PubMed] [Google Scholar]
- 52. Leunissen RW, Kerkhof GF, Stijnen T, Hokken-Koelega A. Timing and tempo of first-year rapid growth in relation to cardiovascular and metabolic risk profile in early adulthood. JAMA. 2009;301(21):2234–2242 [DOI] [PubMed] [Google Scholar]
- 53. Olvera N, Bush JA, Sharma SV, Knox BB, Scherer RL, Butte NF. BOUNCE: a community-based mother-daughter healthy lifestyle intervention for low-income Latino families. Obesity (Silver Spring). 2010;18(suppl 1):S102–S104 [DOI] [PubMed] [Google Scholar]
- 54. Chen KY, Bassett DR., Jr The technology of accelerometry-based activity monitors: current and future. Med Sci Sports Exerc. 2005;37(11 suppl):S490–S500 [DOI] [PubMed] [Google Scholar]