Abstract
OBJECTIVE:
To investigate the effectiveness of brief bedside cardiopulmonary resuscitation (CPR) training to improve the skill retention of hospital-based pediatric providers. We hypothesized that a low-dose, high-frequency training program (booster training) would improve CPR skill retention.
PATIENTS AND METHODS:
CPR recording/feedback defibrillators were used to evaluate CPR quality during simulated arrest. Basic life support–certified, hospital-based providers were randomly assigned to 1 of 4 study arms: (1) instructor-only training; (2) automated defibrillator feedback only; (3) instructor training combined with automated feedback; and (4) control (no structured training). Each session (time: 0, 1, 3, and 6 months after training) consisted of a pretraining evaluation (60 seconds), booster training (120 seconds), and a posttraining evaluation (60 seconds). Excellent CPR was defined as chest compression (CC) depth ≥ one-third anterior-posterior chest depth, rate ≥ 90 and ≤120 CC per minute, ≤20% of CCs with incomplete release (>2500 g), and no flow fraction ≤ 0.30.
MEASUREMENTS AND MAIN RESULTS:
Eighty-nine providers were randomly assigned; 74 (83%) completed all sessions. Retention of CPR skills was 2.3 times (95% confidence interval [CI]: 1.1–4.5; P = .02) more likely after 2 trainings and 2.9 times (95% CI: 1.4–6.2; P = .005) more likely after 3 trainings. The automated defibrillator feedback only group had lower retention rates compared with the instructor-only training group (odds ratio: 0.41 [95% CI: 0.17–0.97]; P = .043).
CONCLUSIONS:
Brief bedside booster CPR training improves CPR skill retention. Our data reveal that instructor-led training improves retention compared with automated feedback training alone. Future studies should investigate whether bedside training improves CPR quality during actual pediatric arrests.
Keywords: pediatric, cardiopulmonary resuscitation, quality appraisal
WHAT'S KNOWN ON THIS SUBJECT:
Low-dose, high-frequency cardiopulmonary resuscitation (CPR) training has not been rigorously evaluated previously.
WHAT THIS STUDY ADDS:
This study is the first to demonstrate that low-dose, high-frequency CPR training can improve CPR skill retention of pediatric providers.
Pediatric cardiac arrest is not a rare event and represents an underestimated public health problem. Approximately 16 000 children in the United States suffer a cardiopulmonary arrest each year.1,2 Although survival outcomes have improved substantially during the last 20 years, still too few children survive with favorable neurologic outcome (2% after out-of-hospital arrest; 17% after in-hospital cardiac arrest).3–6 Therefore, pediatric resuscitation science must develop and evaluate novel interventions (medical, technologic, and educational) designed to improve the survival outcomes of children who suffer a cardiac arrest.
Because the quality of cardiopulmonary resuscitation (CPR) is directly related to survival outcomes,7–10 several studies have implicated the existing educational programs for teaching pediatric CPR skills as a prime target for interventions to improve pediatric survival after cardiac arrest. Not only have varying rates of skill acquisition been documented after traditional American Heart Association (AHA) training classes, but also universally poor skill performance of varying providers 3 to 6 months after CPR training has been established.11–15 Clearly, better programs to improve training success are desirable with the expectation that this would translate into better CPR performed during actual resuscitation attempts.
Highlighting a promising educational technique based on adult learning principles, our group recently established that a single, novel, brief bedside CPR skill retraining program (booster training) achieves successful skill acquisition rates in pediatric hospital-based basic life support (BLS) providers.16 As a continuation of this line of research, in this prospective, randomized interventional trial, we have evaluated whether subsequent brief intermittent refresher CPR training can improve CPR skill retention of these same providers over a 6-month period.
PATIENTS AND METHODS
This investigation was a prospective, randomized interventional trial with the primary objective to investigate the effectiveness of brief bedside CPR booster training sessions to improve skill retention of hospital-based pediatric providers as assessed during simulated pediatric cardiac arrest.
The study protocol, including consent procedures, was approved by the institutional review board at the Children's Hospital of Philadelphia and University of Pennsylvania. Data-collection procedures were completed in compliance with the guidelines of the Health Insurance Portability and Accountability Act to ensure subject confidentiality. Verbal consent was obtained from all health care providers who participated.
Subjects
All pediatric in-hospital care providers with BLS training (registered nurses, medical resident physicians) working on the general inpatient wards or in the emergency department at Children's Hospital of Philadelphia were eligible for inclusion in this study. ICUs were excluded because of an existing bedside CPR training program in these acute care areas.17 Providers were approached during their normal working hours, and all shifts were included (ie, both day and night) in enrollment procedures. In addition, any providers who had previous exposure to training with the Heartstart MRx/Q-CPR system in the previous 12 months also were excluded.
Quantitative CPR Recording Defibrillator
A commercial monitor/defibrillator system (Heartstart MRx/Q-CPR [Philips Healthcare, Andover, MA]) was used in this investigation to record CPR quality data and provide automated feedback when dictated by study design. Using a compression sensor (dimensions: 127 × 62 × 24 mm) placed under the hand of the CPR provider, quantitative CPR information is recorded and stored. This system can also provide audiovisual feedback to the rescuer on the basis of the following age-appropriate AHA18 specifications: chest compression (CC) depth ≥ 38 mm (1.5 inches) or ∼one-third anterior-posterior chest depth,19–21 rate ≥ 90 CC per minute or ≤ 120 CC per minute; < 2500 g of residual leaning force (incomplete release between CCs); and CC pauses of ≤15 seconds.
Booster Training/Evaluation Sessions
CPR was performed on a pediatric prototype manikin, the Voice Advisory Manikin Junior (Laerdal Medical, Stavanger, Norway), which is anatomically similar to a 7-year-old child and engineered for pediatric CPR training and evaluation. Participants performed 2-rescuer pediatric BLS CPR according to the current AHA guidelines18 (15:2 chest compression: ventilation ratio with a target minimal pediatric depth of one-third anterior-posterior chest depth [∼38 mm19–21]). The participants delivered chest compressions; an investigator delivered standardized, AHA-specified ventilations (1-second inflation time). There was no changeover of provider role. These sessions were completed during the participant's normal working hours in the patient care areas (ie, at the bedside). However, all sessions were completed out of view of other participants to avoid training arm contamination.
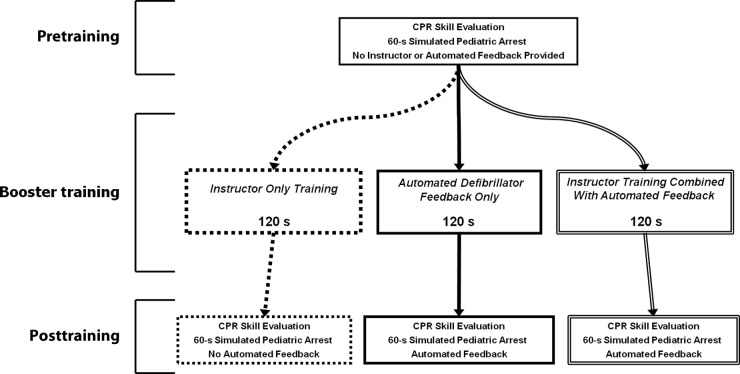
Training sessions occurred at entry into the study (time 0: initial skill acquisition) and then 1, 3, and 6 months after study entry. All sessions were of identical length. There were 3 training arms and 1 control arm used in this study: (1) instructor-only training; (2) automated defibrillator feedback only; (3) instructor training combined with automated feedback; and (4) control (no structured training). At each session, in sequential fashion, participants completed a pretraining evaluation (60 seconds) and a booster training session (120 seconds), followed by a posttraining evaluation (60 seconds); however, in the control (no structured training) group, only a 60-second evaluation at each session was completed. During all pretraining evaluations, there was no feedback given to participants. However, in the posttraining evaluations, groups who received automated feedback in their booster session (automated defibrillator feedback only and instructor training combined with automated feedback), tested with the assistance of the defibrillator feedback. The instructor-only training group did not receive instructor feedback during posttraining evaluations. Please see Fig 1 for study flow sheet diagram. Briefly described below, additional details about study arms including randomization procedures, are reported in our previous publication regarding skill acquisition.16
FIGURE 1.
Study design flow sheet.
Instructor-Only Training
The training consisted of a short (∼30-second) scripted verbal instruction on how to perform high quality CPR immediately followed by manikin practice time for the remainder of the session (∼90 seconds). During this time participants were given additional unscripted verbal feedback on their CPR performance as assessed by the instructor leading the session.
Automated Defibrillator Feedback Only
The training consisted of a short (∼30-second) scripted verbal introduction to the feedback supplied by the MRx defibrillator (ie, they were familiarized with the auditory prompts and visual feedback), immediately followed by manikin practice for the remainder of the session (∼90 seconds). During this time participants were given audiovisual automated feedback assistance.
Instructor Training Combined With Automated Feedback
A combination of the first 2 groups, this training included a short (∼30-second) scripted verbal instruction on how to perform high-quality CPR and an introduction to the feedback supplied by the MRx defibrillator. Again, this introduction was immediately followed by manikin practice for the remainder of the session (∼90 seconds), during which participants were given not only instructor-led feedback, but also audio and visual automated feedback assistance from the MRx.
Control: No Structured Training
The training consisted of a 60-second psychomotor skill assessment. During this time participants did not receive either instructor or defibrillator automated feedback assistance.
Outcome Variables
The primary outcome variable was a prospectively designated composite variable, excellent CPR, defined as a CC depth ≥ one-third anterior-posterior chest depth (∼38 mm19–21), compression rate ≥ 90 and ≤ 120 CC per minute, ≤20% of CCs with incomplete release (<2500 g residual leaning force), and a no-flow fraction ≤ 0.30 during a given evaluation session (no-flow fraction: fraction of total resuscitation time without provision of CPR or spontaneous circulation). A single dichotomous variable that represented retention was constructed in the following manner: subjects who met excellent CPR criteria in pretraining evaluation were classified as “successfully retaining their CPR skills.” A priori, the following training targets were defined: (1) skill acquisition after 6 months of training, 75% of participants performed excellent CPR; and (2) skill retention before 6 months of training, 65% of participants performed excellent CPR. These levels of training and retention success were designated because they have face validity and far exceed previous publications.11–15 Baseline demographic data were collected including gender, age (years), time since last formal BLS education (months), primary training discipline (nurse, physician), years of experience in current position, current advanced cardiac life support (ACLS) certification, and primary floor acuity (cardiology, pulmonary, oncology, emergency department, integrated care [technology dependent children], and residents considered high acuity).
Statistical Analysis
A Microsoft Windows-based software program, Q-CPR Review 2.1.0.0 (Laerdal Medical), was used for initial examination and extraction of the quantitative CPR quality data. Standard descriptive statistics were calculated as appropriate for the distribution of each variable. Categorical variables were compared using McNemar's test for paired binary data. In a multivariable model, differences in the retention rate throughout time and between groups were assessed by using generalized estimating equations.22,23 P < .05 was considered statistically significant. Statistical analysis was completed by using Stata-IC 10.0 (Stata Corp, College Station, TX).
RESULTS
Between March 2009 and April 2009, 89 pediatric in-hospital providers were approached for inclusion. All (100%) met inclusion/exclusion criteria and subsequently provided verbal consent to participate. At study end in November 2009, 74 (83%) participants completed all 3 subsequent training/evaluation sessions. Completion rates by study arm were as follows: (1) instructor-only training, 19 of 23 (83%); (2) automated defibrillator feedback only, 20 of 23 (87%); (3) instructor training combined with automated feedback, 21 of 23 (91%); and (4) control (no structured training), 14 of 20 (70%). The average time that follow-up sessions were completed were as follows: 1 month, 38 ± 10 days; 3 months, 108 ± 11 days; and 6 months, 195 ± 18 days. Comparison of participant-demographic data between study groups while available in our publication of skill acquisition,16 is summarized as follows: average age was 30 ± 6 years; average experience in current position was 4 ± 5 years; 91% (n = 81) were female; 88% (n = 78) were registered nurses; 48% (n = 43) worked on an acute floor; and 87% (n = 77) did not have active ACLS certification.
In Table 1 the unadjusted percentages of participants who performed excellent CPR before (retention) and after training are shown. All 3 training groups met or exceeded our a priori training and retention goals. One half of all training sessions (6 of 12) had statistically significant increases in the proportion of providers who performed excellent CPR after the booster training. In an exploratory analysis, data lost to follow-up seems to have occurred at random because there were similar training success and skill retention rates before dropout in participants who did not complete all sessions compared with those who completed all training.
TABLE 1.
Proportion of Subjects With Excellent CPR Performance at Pretraining (Retention) and Posttraining Evaluations (Training Success)
| Retained Pretraining Excellent CPR | Training Success: Posttraining Excellent CPR | P | |
|---|---|---|---|
| Instructor-only training | |||
| Initial training | 17a | 65 | <.01b |
| 1 mo | 59 | 82 | .13 |
| 3 mo | 73 | 82 | .73 |
| 6 mo | 74c | 84d | .63 |
| Automated feedback only | |||
| Initial training | 26a | 65 | <.01b |
| 1 mo | 48 | 81 | .04 |
| 3 mo | 57 | 67 | .77 |
| 6 mo | 65c | 90d | .18 |
| Instructor training combined with automated feedback | |||
| Initial training | 9a | 61 | <.01b |
| 1 mo | 48 | 91 | <.01b |
| 3 mo | 73 | 100 | .03 |
| 6 mo | 67c | 86d | .29 |
Initial skill acquisition, not retention.
Statistical significance for each individual testing session (McNemar's test for paired binary data).
Retention goals achieved.
Training success goals achieved.
In the control group (no training), there was no increased likelihood of subjects performing excellent CPR during the next session (odds ratio [OR]: 1.1 [95% confidence interval (CI): 0.9–1.4]; P = .25). In a multivariable model adjusted for gender and age of participant, profession (ie, doctor or nurse), ACLS certification, acuity of primary working floor, and days since last formal CPR training, subjects, as part of the overall cohort, were more likely to retain their excellent CPR skills after each subsequent skill evaluation compared with the first training session: after 2 previous trainings (3-month pretraining), subjects were 2.3 times more likely to retain their skills (95% CI: 1.1–4.5; P = .02) and after 3 previous trainings (6-month pretraining), subjects were 2.9 times more likely to retain their skills (95% CI: 1.4–6.2; P = .005). Subjects who received automated defibrillator feedback only were less likely to retain skills compared with the instructor-only training group (OR: 0.41 [95% CI: 0.17–0.97]; P = .043). There were no statistically significant differences noted between the instructor combined with automated feedback group and the automated defibrillator feedback only group (OR: 1.6 [95% CI: 0.7–3.6]; P = .31) or between the instructor combined with automated feedback group and the instructor-only training group (OR: 0.64 [95% CI: 0.3–1.5]; P = .3).
DISCUSSION
This study represents the first evidence to establish that brief low-dose, high-frequency, bedside CPR skill retraining (booster training) is effective to improve retention of CPR skills in pediatric BLS-certified in-hospital providers. In stark contrast with traditional CPR training methods that have had poor 6-month retention success (ie, high-dose, low-frequency paradigm), this new training technique holds promise as the resuscitation science community looks for ways to improve CPR education methods. We achieved prospectively targeted training success goals (>75% of participants performed excellent CPR at the end of the study), but more importantly, more than 65% of participants performed excellent CPR before their final 6-month prebooster training. These compliance rates far exceed those published previously.11–15 These goals were achieved despite the brevity of the training program (∼20 minutes total, 5 minutes at each of the 4 sessions) and the rigorous outcome variable used to define “excellent CPR.” Interestingly, we also found that the group that did not use an instructor (ie, automated defibrillator feedback only) had lower retention rates compared with the group led by a BLS instructor without automated feedback assistance (instructor-only training).
In a previous study, our group established that booster training can improve CPR skill acquisition rates of pediatric in-hospital providers,16 but the durability of such training was in question. The idea that a brief, relatively infrequent training could improve CPR performance seemed illogical considering that the high-intensity standard AHA programs revealed poor retention rates. However, taking into account the principles of adult learning, the success of this program should not be surprising. Adult-learning theory states that there are certain characteristics common to successful adult educational programs: they must be relevant; focused; self-directed; and practical; the need for obtaining the information must be apparent; and there must be a reward to the participant for achieving the training goals.24–26 These booster trainings fulfill nearly all these requirements. Rather than participants attending formal classroom instruction, we brought the learning to the learners, which made the program both practical and relevant (ie, on-the-job training of a necessary skill). We concentrated the “curriculum” to limit instruction time to <2 minutes and allowed participants to complete the sessions at their convenience; in essence, allowing participants to direct their own learning at a convenient time. Moreover, we have targeted the relevant population of individuals most likely to respond before the arrival of highly trained ICU providers during those initial critical moments of a pediatric arrest. As a reward for the training, these first responders were given the confidence to provide excellent BLS skills in an otherwise terrifying situation before arrival of the pediatric code-blue team. In short, these facts reinforce the importance and relevance of this study to resuscitation education.
In this study, lower rates of retention were observed in the training group that did not use a live instructor (automated defibrillator feedback only) compared with the group that used an instructor without automated feedback (instructor-only training). This finding is particularly interesting in light of the study design because one could argue that the automated feedback groups received additional training during their posttraining evaluation sessions (ie, these groups received automated feedback prompts during testing while the instructor group did not). We suspect that the robustness of this particular finding is also likely related to adult-learning principles.24–26 Although the automated feedback provided was targeted to CPR psychomotor skill errors, these systems do not provide constructive positive feedback. Instructors have an advantage: they were able to comment not only on skills done incorrectly, but also praise good performance. This type of positive reinforcement, an established component of successful adult instructional programs, is particularly important for increasing retention, and likely separated the instructor-led group to achieve higher retention rates.24–26 Although we did not see statistically significant differences between the combined training (instructor combined with automated feedback) compared with the individual training methods alone (automated defibrillator feedback only and instructor-only training), the point estimates obtained from our model were consistent with our other findings. To illustrate, the instructor combined with automated feedback group was more likely (OR: 1.6) to have subjects retain CPR skills compared with the automated defibrillator feedback only group (ie, consistent with instructor training improving retention). Moreover, the instructor combined with automated feedback group was less likely to have subjects retain CPR skills compared with the instructor-only group (OR: 0.6). One could speculate that because the addition of automated feedback (ie, additional training) to an instructor group decreased retention compared with an instructor alone, participants may have been using the automated feedback as a form of “crutch” and were unable to perform good CPR when not supplied this assistance (ie, during pretraining sessions to assess retention). Although interesting, these findings warrant additional study.
This simulation manikin training study has notable limitations. First, whereas we have demonstrated improved skill retention throughout 6 months, more work is needed. It would be desirable if all participants performed excellent CPR. We cannot comment on how many of these trainings would be needed to maintain such a high level of competency, but even if repetition is needed on a monthly basis to maintain skills, the limited burden of these trainings would be outweighed by the benefit of improved resuscitative care when concentrated to an area where arrests are more likely to occur (ie, in the ICU).17 Second, given that most of the study participants were female nurses, there is a theoretical concern that it will be difficult to generalize our findings more broadly to other care providers. However, the success of this program is most likely attributable to its focus on the needs of the adult learner and should be applicable to not only other pediatric care providers, but also hospital-based adult responders. It is important to note that although we have demonstrated improvements in CPR quality variables in manikins, we do not know if this will translate to higher quality CPR performed during actual resuscitation attempts. Third, our sessions were required to be as brief as possible so as not to interfere substantially with a given individual's workday. Because of the brevity of the sessions, providers were not required to switch roles, and this limited evaluation of 2 important aspects of CPR quality: no-flow time and ventilation error.
CONCLUSIONS
In this investigation we establish that brief low-dose, high-frequency bedside CPR booster training is effective to improve CPR skill retention of pediatric in-hospital BLS providers during simulated resuscitation. Our data reveal that instructor-led training may improve retention compared with automated feedback training alone. Future studies should investigate whether low-dose, high-frequency bedside training improves CPR quality during actual pediatric cardiac arrests.
ACKNOWLEDGMENTS
This work was supported by the Laerdal Foundation for Acute Care Medicine, the University of Pennsylvania School of Medicine, the Endowed Chair of Pediatric Critical Care Medicine at the Children's Hospital of Philadelphia, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (award number K23HD062629).
FINANCIAL DISCLOSURE: Drs Nadkarni and Sutton and Ms Niles received unrestricted research grant support from the Laerdal Foundation for Acute Care Medicine, and Dr Abella received unrestricted research grant support from Philips Healthcare and Cardiac Science Corp; the other authors have no financial relationships relevant to this article to disclose.
Abbreviations:
- CPR
- cardiopulmonary resuscitation
- AHA
- American Heart Association
- BLS
- basic life support
- CC
- chest compression
- ACLS
- advanced cardiac life support
- OR
- odds ratio
- CI
- confidence interval
REFERENCES
- 1. Atkins DL, Everson-Stewart S, Sears GK, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry Cardiac Arrest. Circulation. 2009;119(11):1484–1491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid response teams: a systematic review and meta-analysis. Arch Intern Med. 2010;170(1):18–26 [DOI] [PubMed] [Google Scholar]
- 3. Donoghue AJ, Nadkarni V, Berg RA, et al. Out-of-hospital pediatric cardiac arrest: an epidemiologic review and assessment of current knowledge [see comment]. Ann Emerg Med. 2005;46(6):512–522 [DOI] [PubMed] [Google Scholar]
- 4. Donoghue AJ, Nadkarni VM, Elliott M, Durbin D, et al. American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. Effect of hospital characteristics on outcomes from pediatric cardiopulmonary resuscitation: a report from the national registry of cardiopulmonary resuscitation. Pediatrics. 2006;118(3):995–1001 [DOI] [PubMed] [Google Scholar]
- 5. Meaney PA, Nadkarni VM, Cook EF, et al. Higher survival rates among younger patients after pediatric intensive care unit cardiac arrests. Pediatrics. 2006;118(6):2424–2433 [DOI] [PubMed] [Google Scholar]
- 6. Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295(1):50–57 [DOI] [PubMed] [Google Scholar]
- 7. Abella BS, Sandbo N, Vassilatos P, et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation. 2005;111(4):428–434 [DOI] [PubMed] [Google Scholar]
- 8. Edelson DP, Abella BS, Kramer-Johansen J, et al. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation. 2006;71(2):137–145 [DOI] [PubMed] [Google Scholar]
- 9. Edelson DP, Litzinger B, Arora V, et al. Improving in-hospital cardiac arrest process and outcomes with performance debriefing. Arch Intern Med. 2008;168(10):1063–1069 [DOI] [PubMed] [Google Scholar]
- 10. Kramer-Johansen J, Myklebust H, Wik L, et al. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: a prospective interventional study. Resuscitation. 2006;71(3):283–292 [DOI] [PubMed] [Google Scholar]
- 11. Hamilton R. Nurses' knowledge and skill retention following cardiopulmonary resuscitation training: a review of the literature. J Adv Nurs. 2005;51(3):288–297 [DOI] [PubMed] [Google Scholar]
- 12. Kaye W, Mancini ME. Retention of cardiopulmonary resuscitation skills by physicians, registered nurses, and the general public. Crit Care Med. 1986;14(7):620–622 [DOI] [PubMed] [Google Scholar]
- 13. Madden C. Undergraduate nursing students' acquisition and retention of CPR knowledge and skills. Nurse Educ Today. 2006;26(3):218–227 [DOI] [PubMed] [Google Scholar]
- 14. Mancini ME, Kaye W. The effect of time since training on house officers' retention of cardiopulmonary resuscitation skills. Am J Emerg Med. 1985;3(1):31–32 [DOI] [PubMed] [Google Scholar]
- 15. Semeraro F, Signore L, Cerchiari EL. Retention of CPR performance in anesthetists. Resuscitation. 2006;68(1):101–108 [DOI] [PubMed] [Google Scholar]
- 16. Sutton RM, Niles D, Meaney PA, et al. “Booster” training: evaluation of instructor-led bedside cardiopulmonary resuscitation skill training and automated corrective feedback to improve cardiopulmonary resuscitation compliance of Pediatric Basic Life Support providers during simulated cardiac arrest. Pediatr Crit Care Med. 2010; In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Niles D, Sutton RM, Donoghue A, et al. “Rolling Refreshers”: a novel approach to maintain CPR psychomotor skill competence. Resuscitation. 2009;80(8):909–912 [DOI] [PubMed] [Google Scholar]
- 18. American Heart Association 2005 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: pediatric basic life support. Pediatrics. 2006;117(5). Available at: www.pediatrics.org/cgi/content/full/117/5/e989 [DOI] [PubMed] [Google Scholar]
- 19. Braga MS, Dominguez TE, Pollock AN, et al. Estimation of optimal CPR chest compression depth in children by using computer tomography. Pediatrics. 2009;124(1). Available at: www.pediatrics.org/cgi/content/full/124/1/e69 [DOI] [PubMed] [Google Scholar]
- 20. Kao PC, Chiang WC, Yang CW, et al. What is the correct depth of chest compression for infants and children? A radiological study. Pediatrics. 2009;124(1):49–55 [DOI] [PubMed] [Google Scholar]
- 21. Sutton RM, Niles D, Nysaether J, et al. Pediatric CPR quality monitoring: analysis of thoracic anthropometric data. Resuscitation. 2009;80(10):1137–1141 [DOI] [PubMed] [Google Scholar]
- 22. Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22 [Google Scholar]
- 23. Mancl LA, DeRouen TA. Covariance estimator for GEE with improved small-sample properties. Biometrics. 2001;57(1):126–134 [DOI] [PubMed] [Google Scholar]
- 24. Knowles M. The Adult Learner: A Neglected Species. 4th ed Houston, TX: Gulf Publishing Company; 1990 [Google Scholar]
- 25. DeWitt TG. The application of social and adult learning theory to training in community pediatrics, social justice, and child advocacy. Pediatrics. 2003;112(3 pt 2):755–757 [PubMed] [Google Scholar]
- 26. Kaufman DM. Applying educational theory in practice. BMJ. 2003;326(7382):213–216 [DOI] [PMC free article] [PubMed] [Google Scholar]