Abstract
OBJECTIVES
To investigate patterns in prevalences of chronic medical conditions over the agespan of long-term stay nursing home residents and between the sexes with data from the 2004 National Nursing Home Survey (NNHS).
DESIGN
Retrospective, cross-sectional study.
SETTING
U.S. nursing homes.
PARTICIPANTS
Nationally representative sample comprising 11,788 long-term stay residents (3003 (25%) men and 8785 women) aged 65 years or older.
MEASUREMENTS
Clinical Classifications Software (CCS) was used to group ICD-9 codes to identify the 20 most prevalent chronic medical conditions. SAS survey procedures were used to account for design effects of stratification and clustering to generate nationally representative estimates of prevalences of medical conditions.
RESULTS
Average age was 84 y, with women older than men (85 vs. 81, p=0.02) with 67% of women ages 80–95. Women required more ADL assistance. The most frequent chronic medical conditions were hypertension (53, 56%: men, women), dementia (45, 52%), depression (31, 37%), arthritis (26, 35%), diabetes mellitus (26, 23%), gastrointestinal reflux -GERD (23, 23%), atherosclerosis (24, 20%), congestive heart failure -CHF (18, 21%), cerebrovascular disease (24, 19%) and anemia (17, 20%). Sex differences in prevalences existed for all but constipation, GERD, and hypertension. Diabetes, cerebrovascular disease, and lipid disorders decreased with age in men and women. Atrial fibrillation, anemia, arthritis, CHF, and dementia, and thyroid disease increased with age in both men and women. Age-related patterns differed between the sexes for diabetes, hypertension, and Parkinson’s disease.
CONCLUSION
The profile of chronic medical conditions varies over the agespan of nursing home residents and differs between men and women. This knowledge should guide educational and care efforts in long-term care.
Keywords: nursing home, disease prevalence, chronic medical conditions, agespan, elderly, National Nursing Home Survey
INTRODUCTION
The U.S. population is aging resulting in altered demographics and changing healthcare-related needs.1 The oldest old are the fastest-growing component of many national populations, including the United States. The consequence of the increasing numbers of people over the age of 80 years is a larger number of people with functional and memory impairment and unable to live independently.
Census and survey data describe aging and chronic disease trends for community-dwelling U.S. populations.2, 3 Women have longer life expectancies than men, a larger percentage of women than men report being disabled and more women than men at older ages are severely disabled. It is thus, not surprising that more older women than men reside in nursing homes.4, 5 The typical long-term stay nursing home resident has been described as over age 85 (53%), female (76%) and widowed (60%) with a higher disease prevalence with more conditions per resident and sicker than in prior years, comparing data collected in 2004 to more limited data from 1999.6 Despite the higher numbers of women than men in nursing homes, and increasing disease burden in women, data and trends for nursing home residents are usually presented in aggregate for both sexes.6 Similarly, the potential impact of increasing age on the prevalences of diseases and chronic medical conditions is usually not considered in analyses of nursing home populations. Investigations of disease prevalence and management in nursing home residents tend to focus on the individual disease and treat the nursing home population as a single unit.7–14 Understanding age and sex dependent patterns in the prevalence of medical conditions of nursing home residents as they age is key to anticipating care needs, to identifying areas of unmet needs to optimize care of older people, and for training health care professionals involved in their care.
The National Nursing Home Survey (NNHS) was a large national survey of the approximately 1.5 million people residing in nursing homes in the United States in 2004.15 This was the most recent in a continuing series of surveys.16 It was conducted by the Centers for Disease Control and Prevention's National Center for Health Statistics from August 2004 through January 2005. Our goal was to identify the most common chronic medical conditions and the patterns in prevalence of these medical conditions across age groups and between the sexes. We hypothesized that the pattern and prevalence of chronic medical conditions would differ over the age span of nursing home residents and that the patterns would differ in women compared to men.
METHODS
National nursing home study design and sampling
The 2004 NNHS was conducted between August 2004 and January 2005. The sampling design was a two stage probability design where the first stage was the selection of nursing facilities, and the second was the selection of residents within facilities. Nursing homes were selected using probability sampling proportional to their bed sizes. Data were collected for twelve randomly selected residents in nursing homes with > 12 current residents and for all residents in a nursing home if there were <12 current residents.
There were 1500 facilities selected from a sampling frame of 16,628 nursing homes in the United States drawn from the Centers for Medicare and Medicaid Services and State licensing lists. Facilities that went out of business or that became ineligible by the time the survey was conducted were excluded, leaving a final dataset that included 1174 facilities and 13,507 residents, that when weighted, represent 1.49 million residents in US nursing homes at the time of the survey. Our analyses were limited to the long-term stay nursing home residents identified by eliminating residents assigned to a bed on a specialty unit, a rehabilitation or sub-acute care unit, a behavioral unit, or children with disabilities.
The diagnosis and demographic data presented here were based on the current resident questionnaire. The data for a sampled resident were collected by a trained interviewer by consulting with a designated staff member who was familiar with the resident’s care. Interviewers made an effort to identify the most clinically relevant diagnoses at time of survey. The staff member was instructed to refer to the resident’s medical record for answers to the items. No residents were interviewed directly (details on the study and sampling design are available at http://www.cdc.gov/nchs/data/series/sr_13/sr13_167.pdf: accessed 28 January 2011).
Diagnoses Data
A maximum of 16 current diagnoses listed in the medical record of each sampled resident based on the ICD-9-CM (International Classification of Disease, 9th Revision, and Clinical Modification) were collected for each resident in the sample. A diagnosis listed in the NNHS resident data file was a disease or injury listed by the attending physician in the resident’s medical record. Over 99% of residents whose data were analyzed had fewer than 16 diagnoses. Data were also collected on admitting diagnoses in the survey. In fifty-seven percent of the resident data that we analyzed, the admitting diagnosis was included in the current diagnosis data. In the remainder, two-thirds of the admission diagnoses were for acute conditions such as fracture, infection, acute cardiovascular event, bleeding, electroyte disorder, respiratory failure, or bowel obstruction. As our focus was on changes in chronic medical conditions of nursing home residents, we did not include analyses of admitting diagnoses.
Defining diagnosis categories
We analyzed data for 20 chronic medical conditions: atrial fibrillation, anemia, arthritis, atherosclerosis, congestive heart failure, constipation, chronic obstructive pulmonary disease, cerebrovascular disease, dementia, depression, diabetes, gastroesophageal reflux disease and heartburn and ulcer disease, hypertension, lipid disorder, osteoporosis, Parkinson’s disease, peripheral vascular disease, renal failure, thyroid disorders, benign prostatic hyperplasia and an “all vascular disease” composite diagnosis defined below.
We identified the 20 chronic medical conditions of interest by using the Clinical Classifications Software (CCS) for ICD-9-CM that is one in a family of databases and software tools developed as part of the Healthcare Cost and Utilization Project (HCUP), a Federal-State-Industry partnership sponsored by the Agency for Healthcare Research and Quality. HCUP databases, tools, and software are publicly available (http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccsfactsheet.jsp). This tool has been used extensively in analyses of health care utilization but we are unaware of its use for the analysis of nursing home data. We utilized the single level CCS rankings (http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp) for initial aggregations of chronic medical conditions and then those that were recorded in over 5% of residents. Some related CCS diagnosis categories were collapsed into a single chronic medical condition grouping based on probable common physiologic basis (and in some cases, similar therapeutic regimens) as determined by input of the investigators and an expert panel of consultants to the project (NIA grant RC1-AG036377). A modified Delphi approach was used where expert panel members individually commented on best methods for groupings of ICD9 diagnoses, followed by preliminary groupings by the investigators based on these recommendations and a literature review with final refinements of chronic medical conditions groupings determined with input from the expert panel via videoconference discussion with the investigators. An illustrative example is for hypertension where “Hypertension” and “Hypertension complications” were combined into a single “Hypertension” category. Gastroesophageal reflux disease, heartburn and peptic ulcer disease were combined into a single chronic condition related to acid/peptic acid disease; and, diabetes with and without complications were combined into a single “diabetes” chronic medical condition. In addition, we created a grouping called “All vascular diseases” that represented atherosclerotic disease of the heart, brain and peripheral arteries. All codes that were in CCS categories “Other” or “Unclassified” were examined and included in diagnoses as appropriate. The complete list of ICD-9 codes that appeared in the NNHS dataset and the corresponding grouped chronic medical conditions are available at (http://www.jhsf.org/learning-research.htm)
Statistical Analysis
Due to the complex probability survey design of the data, SAS survey procedures in SAS version 9.2 (SURVEYMEANS, SURVEYFREQ, SURVEYLOGISTIC) designed for analyzing survey data were used to properly account for design effects of stratification and clustering in all analyses to generate nationally representative estimates for U.S. nursing home residents ≥65 years of age. All percentages listed in this paper represent weight- and cluster-adjusted results. Comparisons of characteristics were made between women and men using t-tests for continuous variables using the Taylor series method to estimate sampling errors and Rao-Scott Chi-square tests for categorical variables. Prevalences for each chronic medical condition were estimated by sex for residents age 65 years and older and also by age groups defined in 5 year increments from 65 to 100 within each sex. The standard errors of the prevalence estimates displayed were estimated with the Taylor series linearization method. Differences in prevalence of chronic medical conditions between men and women were assessed using Rao-Scott Chi-square tests. Age patterns in prevalence were estimated separately for men and women using logistic regression. Gender differences in age patterns were examined by including gender by age interaction terms in the logistic regression models. The Box-Tidwell transformation was used to test for evidence of non-linearity of the logit with age 17. Model fits were assessed with residual plot analysis and c-statistics. The false discovery rate control method, which controls the expected proportion of incorrectly rejected null hypotheses, was used to correct for multiple comparisons18 using the SAS MULTTEST procedure.
RESULTS
Data were collected for 11,788 long-term care residents of nursing homes age 65 years and older. Among these subjects, 3003 were men and 8785 women, representative of 328,361 men and 966,594 women after applying sampling weights.
Table 1 provides demographic and clinical characteristics of these residents aged 65 years or older. The largest proportion of residents were white (87% overall; 88% of women and 84% of men, p<0.001). The mean age was 84 years with slightly more than half (52%) aged 85 and older. Women were on average older than men (85 vs. 81, p<0.001) with 77% of women between the ages 80–95 compared to 54% of men. Eighty two percent of nursing home residents over the age of 85 were women. Women required more assistance with activities of daily living (bathing, dressing, toileting, transfers, continence, eating) than men (mean of 4.9 vs. 4.6, respectively, p<0.001). Length of stay since admission (at the time of the survey) was longer for women than men (mean of 865 vs. 735 respectively, p<0.001). The largest differences in the proportion of residents’ sources of payment between women and men were as follows: private pay (72% vs. 62%, p<0.001), Medicare (13% vs. 16%, p<0.001) and Medicaid (63% vs. 55%, p<0.001).
Table 1.
Characteristics of the nursing home residents ages 65 and older.
| All participants (n=11,788, nw= 1,294,955)* |
Women (n=8785, nw=966,594) |
Men (n=3003 nw=328,361) |
Sex comparison (p)† |
|
|---|---|---|---|---|
| 84±8 | 85±8 | 81±8 | ||
| Age (y) (mean ± S.D.)‡ | (CI: 84–84)‡ | (CI:85–85) | (CI: 81–82) | <0.001 |
| Age distribution (nw (%))§ | ||||
| 65–69 | 66,676 (5) | 38,168 (4) | 28,508 (9) | |
| 70–74 | 102,928 (8) | 59,062 (6) | 43,866 (13) | |
| 75–79 | 184,931 (14) | 119,181 (12) | 65,750 (20) | |
| 80–84 | 275,541 (21) | 203,619 (21) | 71,922 (22) | |
| 85–89 | 310,976 (24) | 244,110 (25) | 66,866 (20) | |
| 90–95 | 242,741 (19) | 202,785 (21) | 39,956 (12) | |
| 95+ | 111,162 (9) | 99,669 (10) | 11,493 (4) | |
| Hispanic (nw (%)) | 42,876 (3) | 29,432 (3) | 13,444 (4) | 0.02 |
| Race (nw (%))¶ | ||||
| American Indian | 5859 (0.4) | 3301 (0.3) | 2558 (0.8) | |
| Asian | 11,338 (0.9) | 6759 (0.7) | 4579 (1.4) | |
| African American | 143,376 (11) | 99,465 (10) | 43,911 (13) | <0.001 |
| Hawaiian/Pacific Islander | 4554 (0.4) | 3046 (0.3) | 1508 (0.5) | |
| White | 1,130,696 (87) | 854,686 (88) | 276,010 (84) | |
| Number of ADLs requiring | 4.8±1.6 | 4.9±1.6 | 4.6±.17 | |
| assistance (mean ± S.D.) | (CI: 4.7–4.8) | (CI: 4.8–4.9) | (CI: 4.5–4.7) | <0.001 |
| Length of stay (days) (mean ± S.D.) | 832±1092 | 865±1066 | 735±1161 | <0.001 |
| Payer source (nw (%)) | ||||
| Private health insurance | 99,127 (8.0) | 70,345 (7.6) | 28,782 (9.2) | 0.02 |
| Life Care | 5232 (0.4) | 4132 (0.4) | 1100 (0.4) | 0.51 |
| Private pay | 869,817 (69.8) | 674,400 (72.4) | 195,417 (62.2) | <0.001 |
| Medicare# | 170,934 (13.7) | 120,091 (12.9) | 50,843 (16.2) | <0.001 |
| Medicaid** | 762,032 (61.2) | 589930 (63.3) | 172,102 (54.8) | <0.001 |
| Welfare or other government assistance | 7743 (0.6) | 6768 (0.7) | 975 (0.3) | 0.05 |
| Department of Veterans Affairs | 9349 (0.8) | 618 (0.1) | 8731 (2.8) | <0.001 |
| Other payment source | 25,369 (2.0) | 17,903 (1.9) | 7466 (2.4) | 0.29 |
nw represents weighted frequency
Sex comparison p-values based on Rao-Scott Chi-Square test.
S.D. represents standard deviation.
CI represents 95% confidence interval.
Six of the 11782 residents listed more than one race and were excluded from analysis of the race variable.
Includes Medicare HMO
Includes Medicaid HMO.
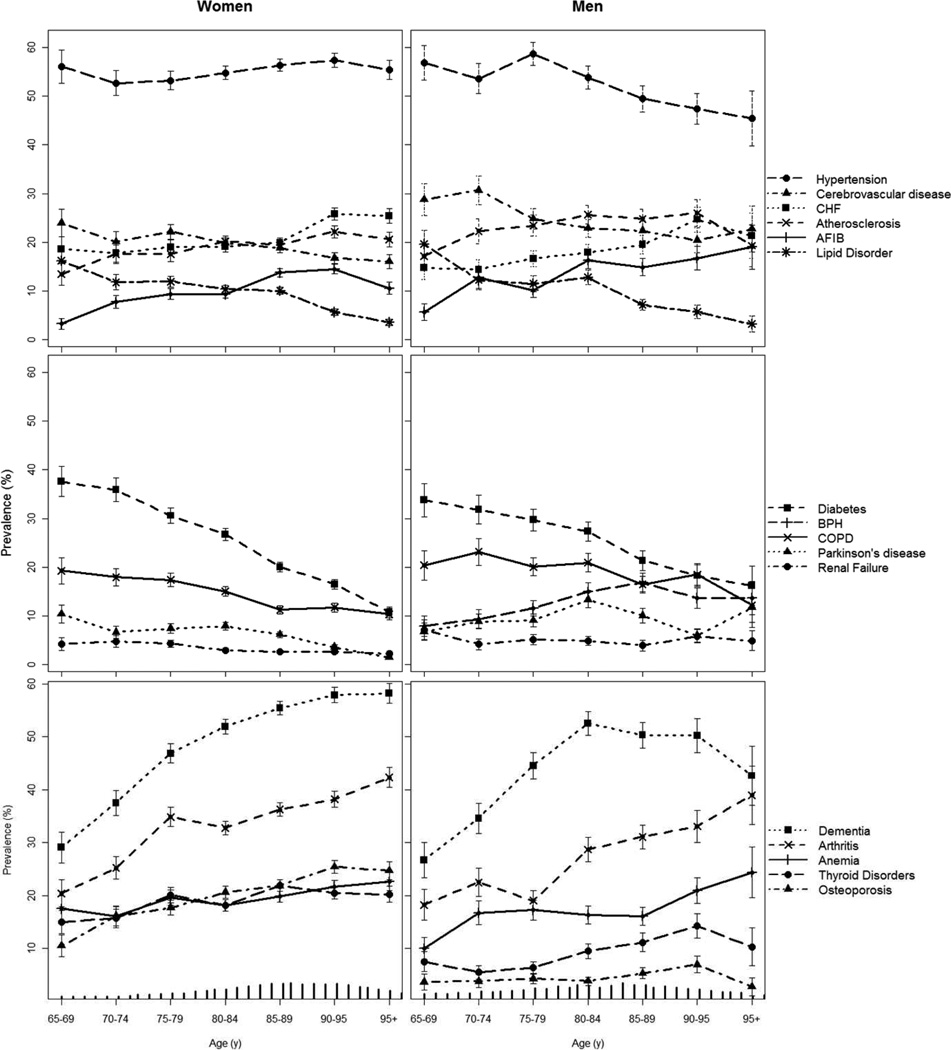
Table 2 provides data on the prevalences of the most frequent chronic medical conditions. Data on diagnosis prevalence by age are presented by sex in Figure 1 with supporting data available in online Appendix Tables A1 and A2. The most frequent conditions overall were hypertension (55%), dementia (51%), depression (35%), arthritis (33%), diabetes mellitus (24%), gastrointestinal reflux (23%), atherosclerosis (21%), congestive heart failure (20%), cerebrovascular disease (20%) and anemia (19%).
Table 2.
Prevalences of chronic medical conditions in men and women; change in log odds of medical condition with a 1 year increase in age (slope) across the agespan 65–100 for each sex; age and sex interaction.
| Medical Condition | Women % |
Men % |
Sex p* |
Women Slope Age† |
Women p‡ |
Men Slope AGE |
Men p‡ |
Age*Sex p§ |
|---|---|---|---|---|---|---|---|---|
| Atrial fibrillation | 11 | 14 | 0.012 | 0.029 | <0.001 | 0.034 | <0.001 | 0.909 |
| Anemia | 20 | 17 | 0.005 | 0.013 | 0.004 | 0.019 | 0.025 | 0.909 |
| Arthritis | 35 | 26 | <0.001 | 0.026 | <0.001 | 0.036 | <0.001 | 0.577 |
| Atherosclerosis | 20 | 24 | <0.001 | 0.014 | 0.002 | 0.012 | 0.081 | 0.914 |
| Benign prostatic hyperplasia | NA | 13 | NA | NA | NA | 0.027 | 0.003 | NA |
| Congestive heart failure | 21 | 18 | 0.003 | 0.020 | <0.001 | 0.024 | 0.002 | 0.909 |
| Constipation | 10 | 10 | 0.748 | 0.007 | 0.282 | 0.007 | 0.529 | 0.957 |
| Chronic obstructive pulmonary disease | 14 | 20 | <0.001 | −0.029 | <0.001 | −0.015 | 0.063 | 0.455 |
| Cerebrovascular disease | 19 | 24 | <0.001 | −0.017 | <0.001 | −0.020 | 0.006 | 0.909 |
| Dementia | 52 | 45 | <0.001 | 0.035 | <0.001 | 0.034 | <0.001 | 0.949 |
| Depression | 37 | 31 | <0.001 | −0.005 | 0.133 | −0.008 | 0.212 | 0.909 |
| Diabetes | 23 | 26 | 0.002 | −0.056 | <0.001 | −0.033 | <0.001 | 0.013 |
| Gastroesophageal reflux disease | 23 | 23 | 0.661 | 3×10−4 | 0.980 | −0.007 | 0.378 | 0.820 |
| Hypertension | 56 | 53 | 0.082 | 0.005 | 0.217 | −0.018 | 0.003 | 0.006 |
| Lipid Disorder | 9 | 11 | 0.033 | −0.045 | <0.001 | −0.046 | <0.001 | 0.949 |
| Osteoporosis | 21 | 5 | 0.001 | 0.028 | <0.001 | 0.022 | 0.169 | 0.909 |
| Parkinson’s disease | 6 | 10 | <0.001 | −0.045 | <0.001 | 0.007 | 0.516 | <0.001 |
| Peripheral vascular disease | 11 | 14 | <0.001 | 0.001 | 0.956 | −0.005 | 0.621 | 0.909 |
| Renal failure | 3 | 5 | <0.001 | −0.027 | 0.006 | −0.010 | 0.516 | 0.810 |
| Thyroid disorders | 20 | 9 | <0.001 | 0.011 | 0.008 | 0.037 | 0.002 | 0.111 |
| All vascular disease | 41 | 49 | <0.001 | −7×10−5 | 0.985 | −0.002 | 0.674 | 0.909 |
Sex comparison p-values based on Rao-Scott Chi-Square test.
Slope is the increase in log odds of the medical condition with age. The odds ratios for a 1 year increase in age can be obtained by exponentiating. An odds ratio for a y year age difference can be obtained by multiplying the log odds by y and exponentiating the product.
P-values based on Wald test for age term in logistic model.
P-values based on Wald test for interaction term between age and sex in logistic model.
All p-values have been adjusted for multiple comparisons using the false discovery rate method of adjustment.
NA = not applicable. Sample sizes for races other than White and African American were too small for analyses. With race considered as white or African American ethnicity/race model model estimates were unchanged and thus not presented.
Figure 1.
Prevalence (%) of chronic medical conditions in nursing home residents by age and sex with bars representing standard errors. Data for women are on the left, data for men are on the right. Tick marks across horizontal axes represent the age distribution for the given sex. The top panel presents data on common cardiovascular diseases with data on hyptertension represented by solid circles and long dashed lines ( ), cerebrovascuar disease repesented by triangles and short dash-dot lines (
), cerebrovascuar disease repesented by triangles and short dash-dot lines ( ), CHF=congestive heart failure represented by squares and dotted lines (
), CHF=congestive heart failure represented by squares and dotted lines ( ), atherosclerotic disease represented by×and short dashed lines (
), atherosclerotic disease represented by×and short dashed lines ( ), AFIB=atrial fibrillation represented by plus symbols and solid lines (
), AFIB=atrial fibrillation represented by plus symbols and solid lines ( ), and LIPID=lipid disorder represented by asterisks and long dash-dot lines (
), and LIPID=lipid disorder represented by asterisks and long dash-dot lines ( ). The middle panel presents data on common organ conditions by organ affected with data on diabetes represented by squares and short dashed lines (
). The middle panel presents data on common organ conditions by organ affected with data on diabetes represented by squares and short dashed lines ( ), BPH= benign prostatic hyperplasia repesented by plus symbols and long dashed lines (
), BPH= benign prostatic hyperplasia repesented by plus symbols and long dashed lines ( ), COPD= chronic obstructive pulmonary disease represented by×and solid lines (
), COPD= chronic obstructive pulmonary disease represented by×and solid lines ( ), Parkinson’s disease represented by triangles and dotted lines (
), Parkinson’s disease represented by triangles and dotted lines ( ), renal failure represented by circles and dash-dot lines (
), renal failure represented by circles and dash-dot lines ( ). The bottom panel presents data on common geriatric conditions with data on dementia represented by squares and dotted lines (
). The bottom panel presents data on common geriatric conditions with data on dementia represented by squares and dotted lines ( ), arthritis repesented by×and and short dashed lines (
), arthritis repesented by×and and short dashed lines ( ), anemia represented by plus symbols and solid lines (
), anemia represented by plus symbols and solid lines ( ), thyroid disorders represented by circles and long dashed lines (
), thyroid disorders represented by circles and long dashed lines ( ), and osteoporosis represented by triangles and short dash-dot lines (
), and osteoporosis represented by triangles and short dash-dot lines ( ).
).
Differences in prevalence between men and women were not detected for constipation, gastroesophageal reflux disease and heartburn and ulcer disease, and hypertension. The prevalences of the other diagnoses considered differed between men and women. Anemia, arthritis, congestive heart failure, dementia, depression, osteoporosis, and thyroid disease more common in women, while vascular diseases (atherosclerosis, cerebrovascular disease, lipid disorders, peripheral vascular disease) were more common in men, as were atrial fibrillation, chronic obstructive pulmonary disease, diabetes mellitus, Parkinson’s disease, renal failure, and benign prostatic hyperplasia.
Differences in prevalence of 14 of the 20 diagnoses were seen across the agespan of nursing home residents (Table 2). The prevalence of atrial fibrillation, anemia, arthritis, congestive heart failure, dementia and thyroid disorders increased significantly with increasing age in both men and women. The prevalence of diabetes (Figure 1, second panel; Table 2), cerebrovascular disease, and lipid disorders (Figure 1, first panel; Table 2) decreased significantly with increasing age in both men and women.
Examining agespan trends for each sex separately, atherosclerosis and osteoporosis increased with increasing age in women while renal failure, chronic obstructive pulmonary disease, and Parkinson’s disease was less prevalent with increasing age in women. In men, hypertension was less prevalent as age increased (Figure 1; Table 2).
These differences between the sexes for variations with age in prevalence of chronic medical conditions reached statistical significance for diabetes, hyptertension, and Parkinson’s disease. Hypertension had a roughly constant prevalence of about 56% in women but decreased from 57% in men 65–69 years to 45% in the men over 95 years (Figure 1, first panel; Tables 3 and 4). Parkinson’s disease prevalence decreased for women, but slightly increased for men (Figure 1, second panel; with supporting data available in online Appendix Tables A1 and A2). Diabetes mellitus decreased for both men and women, but at a steeper rate for women, from 38% for women 65–69 years to 11% for women over 95 years of age, compared to a prevalence of 34% for men 65–69 years decreasing to 16% for men over 95 years of age (Figure 1, second panel; with supporting data available in online Appendix Tables A1 and A2)
DISCUSSION
Nursing homes are a crucial component of the long-term care system. There were about 1.5 million nursing home residents in 16,100 facilities according to the 2004 NNHS. The number of Americans needing long-term care is projected to double between 2000 and 2050 19. Policymakers, health care providers, and consumers all need accurate and representative information on the characteristics of nursing home residents to best plan long-term care educational and health-care delivery needs.
Predictors of admission to long-term care facilities include both social and medical factors with age, absence of a potential caregiver, severity of cognitive impairment or care needs, and failure to adapt to an adverse event identified as risk factors.20–22 The chief chronic medical conditions associated with nursing home admission have been reported to be dementia, stroke23, cognitive impairment20, 21, and depression22. Once admitted to a nursing home, however, consideration must be given to all the medical conditions of the individual. The NNHS has collected data on chronic medical conditions in nursing home residents but diagnostic data were limited to five or less diagnoses in surveys performed before and including the 1999 survey.16 The 2004 NNHS attempted to both identify the most clinically relevant diagnoses and to provide comprehensive data on medical conditions with data collected on up to sixteen current medical diagnoses per nursing home resident.15 These data provide the first opportunity to comprehensively examine the prevalence of chronic medical conditions in long-term care nursing home residents. While others have used these data to investigate prevalences of single disease processes or use of centrally acting medications,24–26 our goal was to investigate the prevalences of the most common chronic medical conditions and to determine whether medical conditions vary over the continuum of ages seen in nursing home residents or between the sexes. Our analyses focused only on the nursing home residents over the age of 65 years and only on long-term stay residents. Thus, they differ from aggregate data for nursing home residents that are available (http://www.cdc.gov/nchs/data/nnhsd/Estimates/nnhs/Estimates_Diagnoses_Tables.pdf#Table33b) and from most prior studies of risk factors for nursing home admission that did not differentiate between long-term care residents and those admitted to nursing homes for either short term rehabilitation or to palliative care units for end of life care or short term treatment of psychiatric disorders.20
We found both that altered chronic medical condition prevalences changed over the agespan of 65–100 years of long-trem care nursing home residents, and, that for some medical conditions, these findings differed in women compared to men. The overall frequency of the most common medical conditions such as hypertension, dementia, depression, arthritis, diabetes mellitus, atherosclerosis, congestive heart failure, cerebrovascular disease and anemia mirrored prevalences in community-dwelling elderly.27 The prevalence of vascular disease, benign prostatic hypertrophy, chronic obstructive pulmonary disease, and Parkinson’s disease was higher in men overall, as has also been observed in community and younger populations.28, 29 Earlier in life smoking patterns, hormonal influences, presence of a prostate, and genetic influences are likely underlying factors. Women of all ages have been reported to have a higher incidence of inflammatory and immune-related disorders, arthritis, osteoporosis, thyroid disease, and depression and this sex difference was maintained in the nursing home residents.28, 30 Heart failure was more prevalent in the women overall. It is recognized that heart failure is more likely a consequence of hypertension in women that occurs at older ages in women and is then present for longer than in men.27 Heart failure is more likely a consequence of coronary artery disease in men and of the systolic type that may have shorter mean survival times such that our findings may be a consequence of the old age of the nursing home residents overall and the older ages of the women. We found the prevalence of dementia to be similar in men and women until very old age when it was higher in women than men. As the prevalence of dementia increased with age in both the men and the women, the overall higher age of the women and the limited number of men at the oldest ages may have contributed to this difference and may not reflect a sex difference in dementia pathophysiology.
We detected statistically significant variations in age-related patterns for 14 of the 20 most common medical conditions considered over the 65–100 year agespan of the nursing home population. A number of the patterns were the same in men and women. Increases in the prevalence of atrial fibrillation, anemia, arthritis, congestive heart failure, dementia, and thyroid disease were seen with increasing age in both men and women. We also tried to estimate the prevalence of vascular diseases as a combined diagnostic category (excluding hypertension that had been combined with these diagnoses in earlier NHHS analyses under circulatory diseases16) and found that the prevalence was high in both men and women, affecting almost half of the older long-term care population. These data would suggest that health care professionals caring for nursing home residents will need to be fluent in the management of atrial fibrillation, congestive heart failure, and vascular disease in addition to hypertension and the more traditional geriatric conditions of anemia, arthritis, dementia, thyroid disease, and constipation. In analyses of medication use in nursing home populations, a lower than expected use of heart medications has been reported and the possibility of under-treatment of cardiovascular diseases in institutional settings raised.31 Management of vascular diseases in nursing home patients is an area that might be in need of further investigation and evaluation for the quality of care.
A striking finding was the decrease in the prevalence of diabetes with increasing age in both men and women. The prevalence decreased at a steeper rate in women, from 38% for women aged 65–69 years to 11% for women over 95 years of age, compared to 34% for men 65–69 years decreasing to 16% for men over 95 years of age. Diabetes is increasing in prevalence in the U.S. population and receiving increased efforts for diagnosis and monitoring. Other investigators have reported that the estimated crude prevalence of diabetes mellitus increased from 16.9% in 1995 to 26.4% in 2004 in male nursing home residents and from 16.1% to 22.2% in female residents based on comparisons to earlier NNHS data.14 They also reported the largest increases in crude rates of diabetes prevalence in the 55–64 year old men and in the men staying in nursing homes less than 30 days. Zhang, et al. hypothesized that altered criteria for diagnosing diabetes could explain some of the increase in diabetes diagnoses as well as increasing tendencies to assign diabetes diagnoses related to increased awareness and to explain resident management.32 We believe that there may be an even more important factor related to NHHS methodology. The earlier 1995 and 1999 NHHS surveys collected data on only five diagnoses per resident. The increased prevalence of diabetes in the 2004 survey data may also reflect the collection of up to 16 diagnoses per resident. The differing methodologies we used in that we analyzed only long-term stay residents over the age of 65 years limit comparisons, but it is pertinent that the prevalence of diabetes decreased across the ages of nursing home residents in 2004 as well as in the earlier surveys analyzed by Zhang et al.14 This consistent decrease in diabetes prevalence across the agespan of nursing home residents suggests that the patients with diabetes may be dying at earlier ages. If so, it could indicate subgroups of nursing home patients to target for care improvement similar to the clinical practice guideline efforts to improve care for older adults with diabetes cared for in the community.33 While prevention and better management of diabetes mellitus at earlier ages might improve longevity, the data also suggest diabetes diagnosis, monitoring and treatment will consume fewer resources in the oldest nursing home residents.
Diagnoses of cerebrovascular disease and lipid disorders also decreased with increasing age in both men and women. The decrease in cerebrovascular disease with increasing age could reflect exclusion of the short-term rehabilitation residents from the analysis, earlier deaths of residents with cerebrovascular disease that become long-term stay residents, resolution of acute stroke admission diagnoses or disabilities due to cerebrovascular disease such that it was not considered a current problem, or greater focus on dementia to which cerebrovascular disease may contribute. The decrease in coding of lipid disorder diagnoses is slightly more difficult to understand. It is unlikely that the true prevalence of lipid disorders was low in view of the increased diagnosis of atherosclerosis processes in women with increasing age and the high burden of vascular disease in men and women at all ages in the nursing home residents. It is possible that lipid disorders may not have been listed as current active diagnoses in older nursing home residents for whom treatment for the lipid disorder was not being considered due to administration difficulties, prior adverse effects, presence of liver disease, short life expectancy, or because the risk benefit of lipid treatment might have been considered unfavorable.
Patterns in age-related prevalences differed between men and women for diabetes (discussed above), hypertension, and Parkinson’s disease. Hypertension diagnoses remained constant in women in all age groups but decreased from 57% in men in the young elderly groups 65–69 years to 45% in the men over 95 years. While this finding was statistically significant, it is probably more pertinent that hypertension was a highly prevalent diagnosis at all ages in both men and women. Only the prevalence of dementia at the oldest ages approached or exceeded the prevalence of hypertension. The high prevalence of these diseases throughout the agespan of nursing home residents warrants continued attention to management of these diseases for nursing home residents of all ages. It also stresses the need for an enhanced evidence base to guide treatment of hypertension in the very old and the need for development of effective treatment and prevention strategies for dementia.
The number of nursing home residents below the age of 65 years has been constant from 1977 to 2004 while the number of residents over the age of 65 years has increased seventeen per cent (http://www.cdc.gov/nchs/hdi.htm). Within the group over the age of 65 years of age, women have comprised a stable seventy-four per cent of the nursing home population but the proportion of nursing home residents over the age of 85 years increased from 40 per cent to 51 per cent. The group of “younger elderly” nursing home residents aged 65–75 years decreased from nineteen to thirteen per cent of elderly nursing home residents. Previously, there were few data on the impact of the age patterns on the disease profiles of this changing very old and vulnerable population. Our data show there is not one “typical nursing home resident” and that disease prevalences differ as age increases from 65 to over 100 years and the profile may differ in men and women. We found hypertension, vascular disease and neurocognitive disease to be the most prevalent among male and female nursing home residents at the oldest ages while diabetes become less prevalent, especially in women.
The data make it clear that long-term care sites of the future will need to develop effective plans for the management of the increasing number of very old nursing home residents with high care burdens related to vascular disease and dementia. Our work highlights the need to increase the capacity to better care for nursing home residents with dementia with better therapies, improved housing options, training of health care professionals in non-harmful treatment strategies as well as the societal need to develop strategies to prevent dementia. Nursing homes will need to give increased attention to the treatment of vascular diseases in both older men and older women. Strategies for the management of the pain, stiffness, and limitation of activity due to the burden of arthritis as well as development of improved mobility aids and arthritis friendly physical environments will be needed. Our data also suggest a need to continue to evaluate and further develop the management of chronic conditions of hypertension, depression, anemia, atrial fibrillation, constipation, lipid abnormalities, osteoporosis, gastroesophageal reflux, and diabetes that are common in the aging nursing home populations.
Our study has some limitations. It was a cross-sectional snapshot of residents in U.S. nursing homes with little ethnic diversity. Due to the predominance of whites, we did not detect any effect of race (white, African American) on our model estimates. The racial composition of nursing homes, however, has been changing over time with whites comprising 94% of U.S. nursing home residents in 1973–1974{Zappolo, 1977 #49} and 87% reported as white and 10% as African American in this analysis. Should the composition of nursing home residents continue to change, disease prevalences and patterns may be influenced by ethnicity changes. Our analyses and conclusions may not reflect changes in the diagnoses or health care needs of non-white ethnic groups of similar age and disability. The diagnostic data were recorded for clinical and reimbursement purposes and not for research purposes so that some error in diagnostic classifications may be inherent and the clinical significance of each condition including treatment status, stability, acuity or chronicity was not specified. In addition, other reporting errors, non-response bias, and interviewer effects could affect the findings. Finally, the data were collected from 2004–2005 and diagnostic criteria, medications and adverse effects of medications, and treatment options inevitably change over time and may alter frequencies of chronic medical conditions diagnoses in subsequent years and in subsequent surveys.
In summary, we have identified both the conditions that appear across the agespan of nursing home residents and disease profiles that differ as older nursing home residents age from 65–100 years. This clearer understanding of the high prevalence of diseases related to vascular disease processes and those that increase with frequency in the older nursing home populations can identify the areas to be augmented in both education and training as well as care guidelines for the older long-term care nursing home population.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank the expert panel members: Darrell Abernethy, MD, PhD; Ron Finley, BS Pharm, RPh; Jerry Gurwitz, MD; Joe Hanlon, PharmD, MS; Lynn Kane, RN; Kate Lapane, PhD.
This work was supported by NIA grants RC1 AG 036377 and K23AG030999, and with funds from the Jewish Home of San Francisco
Sponsor’s Role: The funding institutes that supported this research did not participate in the study design, methods, subject recruitment, data collection, analysis, or preparation of the manuscript.
Footnotes
Conflict of Interest: The authors do not have any conflict of interest related to the subject matter of the manuscript.
Author Contributions: study design and analysis: Janice B. Schwartz and Kelly L. Moore, manuscript contributions: Michael Steinman, John Boscardin, Manuscript preparation: Janice B. Schwartz and Kelly L. Moore, Manuscript review and editing: Michael Steinman and John Boscardin.
REFERENCES
- 1.Kinsella K, He W. International population reports. Washington DC: U.S. Department of Health and Human Services National Institutes of Health, National Institute on Aging, U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau; 2009. An aging world: 2008. [Google Scholar]
- 2.Freedman VA, Schoeni RF, Martin LG, et al. Chronic conditions and the decline in late-life disability. Demography. 2007;44:459–477. doi: 10.1353/dem.2007.0026. [DOI] [PubMed] [Google Scholar]
- 3.Lafortune G, Balestat G, Members DSEG. Trends in Severe Disability Among Elderly People: Assessing the Evidence in 12 OECD Countries and the Future Implications in, OECD Health Working Papers. 2007. [Google Scholar]
- 4.Newman AB, Brach JS. Gender gap in longevity and disability in older persons. Epidemiol Rev. 2001;23:343–350. doi: 10.1093/oxfordjournals.epirev.a000810. [DOI] [PubMed] [Google Scholar]
- 5.Cambois E, Désesquelles A, Ravaud JF. The gender disability gap. Population Soc. 2003;386:1–4. [Google Scholar]
- 6.Kasper J, O'Malley M. Changes in Characteristics, Needs, and Payment for Elderly Nursing Home Residents: 1999 to 2004. Washington, D.C.: Kaiser Family Foundation; 2007. [Google Scholar]
- 7.Chatterjee S, Mehta S, Sherer JT, et al. Prevalence and predictors of anticholinergic medication use in elderly nursing home residents with dementia: Analysis of data from the 2004 National Nursing Home Survey. Drugs Aging. 2010;27:987–997. doi: 10.2165/11584430-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 8.Damian J, Pastor-Barriuso R, Valderrama-Gama E. Descriptive epidemiology of undetected depression in institutionalized older people. J Am Med Dir Assoc. 2010;11:312–319. doi: 10.1016/j.jamda.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 9.Joseph J, Koka M, Aronow WS. Prevalence of moderate and severe renal insufficiency in older persons with hypertension, diabetes mellitus, coronary artery disease, peripheral arterial disease, ischemic stroke, or congestive heart failure in an academic nursing home. J Am Med Dir Assoc. 2008;9:257–259. doi: 10.1016/j.jamda.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Juthani-Mehta M, Quagliarello VJ. Infectious diseases in the nursing home setting: Challenges and opportunities for clinical investigation. Clin Infect Dis. 2010;51:931–936. doi: 10.1086/656411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McClellan WM, Resnick B, Lei L, et al. Prevalence and severity of chronic kidney disease and anemia in the nursing home population. J Am Med Dir Assoc. 2010;11:33–41. doi: 10.1016/j.jamda.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 12.Robinson BE. Epidemiology of chronic kidney disease and anemia. J Am Med Dir Assoc. 2006;7(9 Suppl):S3–S6. doi: 10.1016/j.jamda.2006.09.004. quiz S17-21. [DOI] [PubMed] [Google Scholar]
- 13.Shah SM, Carey IM, Harris T, et al. Identifying the clinical characteristics of older people living in care homes using a novel approach in a primary care database. Age Ageing. 2010;39:617–623. doi: 10.1093/ageing/afq086. [DOI] [PubMed] [Google Scholar]
- 14.Zhang X, Decker FH, Luo H, et al. Trends in the prevalence and comorbidities of diabetes mellitus in nursing home residents in the United States: 1995–2004. J Am Geriatr Soc. 2010;58:724–730. doi: 10.1111/j.1532-5415.2010.02786.x. [DOI] [PubMed] [Google Scholar]
- 15.Jones A, Dwyer L, Bercovitz A, et al. The National Nursing Home Survey: 2004 overview. Vital Health Stat. 2009;167:1–155. [PubMed] [Google Scholar]
- 16.Jones A. The National Nursing Home Survey: 1999 summary. Vital Health Stat. 2002;152:1–116. [PubMed] [Google Scholar]
- 17.Hosmer DW, Lemeshow S. Wiley series in probability and statistics texts and references section. xii. New York: Wiley; 2000. Applied logistic regression. 2nd ed; p. 373. [Google Scholar]
- 18.Benjamini Y, Yekutieli D. Quantitative trait Loci analysis using the false discovery rate. Genetics. 2005;171:783–790. doi: 10.1534/genetics.104.036699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services and U.S. Department of Labor. The future supply of long-term care workers in relation to the aging baby boom generation: Report to Congress. Washington, DC: U.S. Government Printing Offic; 2003. Available from: http://aspe.hhs.gov/daltcp/reports/ltcwork.htm. [Google Scholar]
- 20.Gaugler J, Duval S, Anderson K, et al. Predicting nursing home admission in the U.S.: A meta-analysis. BMC Geriatr. 2007;7:13. doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gaugler J, Yu F, Krichbaum K, et al. Predictors of nursing home admission for persons with dementia. Med Care. 2009;47:191–198. doi: 10.1097/MLR.0b013e31818457ce. [DOI] [PubMed] [Google Scholar]
- 22.Luppa M, Luck T, Weyerer S, et al. Prediction of institutionalization in the elderly. A systematic review. Age Ageing. 2010;39:31–38. doi: 10.1093/ageing/afp202. [DOI] [PubMed] [Google Scholar]
- 23.Van Rensbergen G, Nawrot T. Medical conditions of nursing home admissions. BMC Geriatr. 2010;10:46. doi: 10.1186/1471-2318-10-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karkare S, Bhattacharjee S, Kamble P, et al. Prevalence and predictors of antidepressant prescribing in nursing home residents in the United States. Am J Geriatr Pharmacother. 2011;2:109–119. doi: 10.1016/j.amjopharm.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 25.Seitz D, Gruneir A, Conn D, et al. Cholinesterase inhibitor use in U.S. nursing homes: Results from the national nursing home survey. J Am Geriatr Soc. 2009;57:2269–2274. doi: 10.1111/j.1532-5415.2009.02552.x. [DOI] [PubMed] [Google Scholar]
- 26.Seitz D, Purandare N, Conn D. Prevalence of psychiatric disorders among older adults in long-term care homes: A systematic review. Int Psychogeriatr. 2010;22:1025–1039. doi: 10.1017/S1041610210000608. [DOI] [PubMed] [Google Scholar]
- 27.Schwartz J, Zipes D. Cardiovascular disease in the elderly. In: Bonow R, editor. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. Philadelphia: Elsevier Sauders; 2011. [Google Scholar]
- 28.Legato M, Bilezikian J, editors. Principles of Gender-specific Medicine. Elsevier Academic Press; 2004. p. 1245. [Google Scholar]
- 29.Wirdefeldt K, Adami H, Cole P, et al. Epidemiology and etiology of Parkinson's disease: a review of the evidence. Eur J Epidemiol. 2011;(Suppl 1):S1–S58. doi: 10.1007/s10654-011-9581-6. [DOI] [PubMed] [Google Scholar]
- 30.Voskuhl R. Sex differences in autoimmune diseases. Biol Sex Differ. 2011;2:1. doi: 10.1186/2042-6410-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Briesacher B, Doshi J, Stuart B, et al. Medication Use in Long-term Care Facilities and Community Settings for Medicare Beneficiaries with Cardiovascular Disease. USDHHS, Office of the Assistant Secretary for Planning and Evaluation; 2002. [Google Scholar]
- 32.Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26(Suppl 1):S5–S20. doi: 10.2337/diacare.26.2007.s5. [DOI] [PubMed] [Google Scholar]
- 33.Brown AF, Mangione CM, Saliba D, et al. Guidelines for improving the care of the older person with diabetes mellitus. J Am Geriatr Soc. 2003;51(5 Suppl):S265–S280. doi: 10.1046/j.1532-5415.51.5s.1.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.