Summary
We retrospectively analysed to demonstrate the selection of the treatment modality and its efficacy in our department. Subjects of the present study comprised patients in whom coil embolization was abandoned due to such reasons as broad neck, whom coil embolization was performed for residual aneurysm following incomplete clipping or recurrent cerebral aneurysm, whom coil embolization was performed after coil compaction, whom coil embolization and clipping were performed for the treatment of multiple cerebral aneurysms.
In the treatment of cerebral aneurysm, selecting proper techniques by considering the characteristics of clipping and coil embolization is desirable.
In other words, strategizing therapy by taking advantages of the merits of clipping and coil embolization is important.
Key words: cerebral aneurysms, embolization, clipping
Introduction and Methods
To clarify the applications and the roles of coil embolization and clipping in the treatment of cerebral aneurysm.
As a general rule, clipping is performed in the treatment of cerebral aneurysm (clipping for acute-phase ruptured aneurysm) by taking into account factors such as patient age, neurological grade, complications and aneurysm location and shape. From February 1994 to August 2004, clipping was performed on a total of 644 patients, comprising 498 patients with ruptured aneurysms and 146 patients with unruptured aneurysms.
Furthermore, we perform coil embolization in the treatment of cerebral aneurysm by taking into account the following:
-
1)
Severe subarachnoid haemorrhage: GradesIV-V
-
2)
Severe systemic complication
-
3)
Age ≥70 years
-
4)
Cerebral aneurysm site (top of the basilar artery) and shape (no broad neck)
-
5)
Intracerebral haematoma
-
6)
Patient preference
During the same period from February 1994 to August 2004, coil embolization was performed at our institution or one of the affiliated institutions on 244 patients*, comprising 132 patients with ruptured aneurysms and 112 patients with unruptured aneurysms.
Subjects of the present study comprised: (figure 1~3)
-
1)
patients in whom coil embolization was abandoned due to such reasons as broad neck (n=25);
-
2)
patients in whom coil embolization was performed for residual aneurysm following incomplete clipping or recurrent cerebral aneurysm (n=10);
-
3)
patients in whom coil embolization was performed after coil compaction (n=10);
-
4)
patients in whom coil embolization and clipping were performed for the treatment of multiple cerebral aneurysms (n=18).
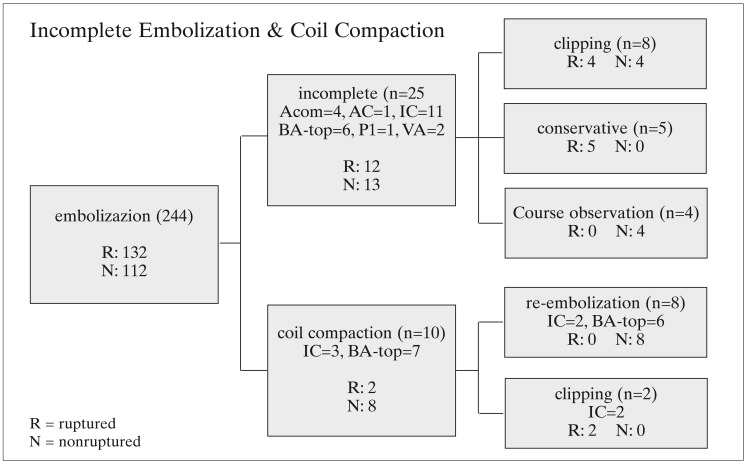
Figure 1.
"incomplete embolization & coil compaction". Application of coil embolization and clipping in the treatment of incomplete embolization & coil compaction in 1994.2~ 2004.8.
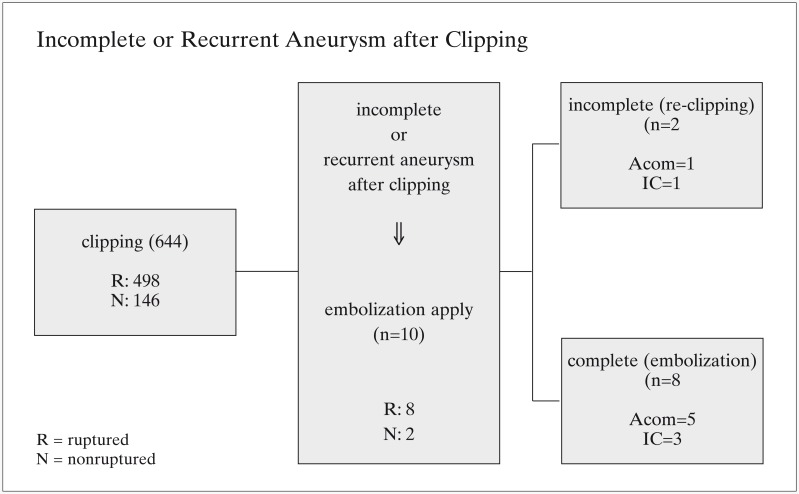
Figure 2.
"incomplete or recurrence aneurysm after clipping". Application of coil embolization and clipping in the treatment of incomplete or recurrent aneurysm after clipping in 1994.2~2004.8.
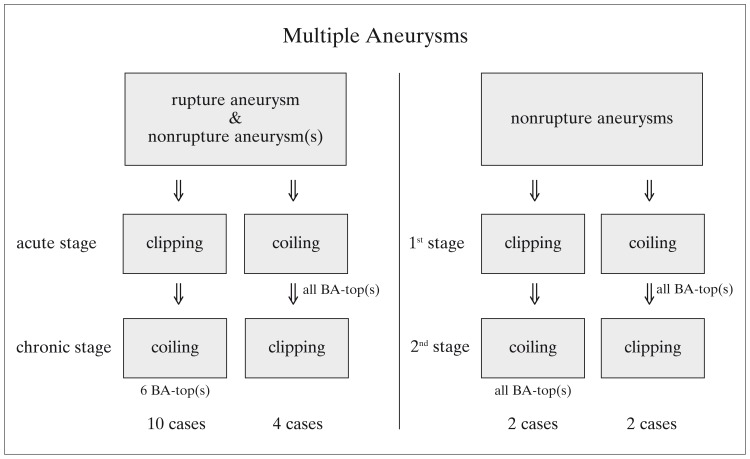
Figure 3.
"multiple aneurysms" Application of coil embolization and clipping in the treatment of multiple aneurysms in 1994.2~2004.8.
Results
1) (figure 1)
In 25 patients (10.2%) (12 ruptured, 13 unruptured), coil embolization was attempted first but was abandoned due to reasons such as broad neck.
The breakdown of site was as follows: anterior communicating artery (ACom) in four patients; anterior cerebral artery (AC) in one patient; internal carotid artery (IC) in eleven patients; top of basilar artery (BA-top) in six patients; P1 segment of posterior cerebral artery (P1) in one patient; and vertebral artery (VA) in two patients. Breakdown of reasons for abandoning coil embolization was as follows: broad neck in 18 patients (balloon neck-plasty was performed on nine of these 18 patients); inaccessible in six patients; and ischemic accident in one patient.
Of the 25 patients in whom coil embolization was attempted first and abandoned, clipping was performed on 16 patients (eight ruptured, eight unruptured). Prognosis was favorable for all 16 patients. Conservative therapy was selected for five ruptured patients who were elderly and/or had severe aneurysm, and prognosis was poor for all five patients, with severe disability or death as outcomes. In the remaining four patients, observation was selected, and future therapy (coil embolization or clipping) was reevaluated.
2) (figure 2)
In ten patients, intra-aneurysmal coil embolization was scheduled to be performed for the treatment of cerebral aneurysm following in-complete clipping (Case 1: figure 4) or recurrent cerebral aneurysm following clipping (Case 2: figure 5).
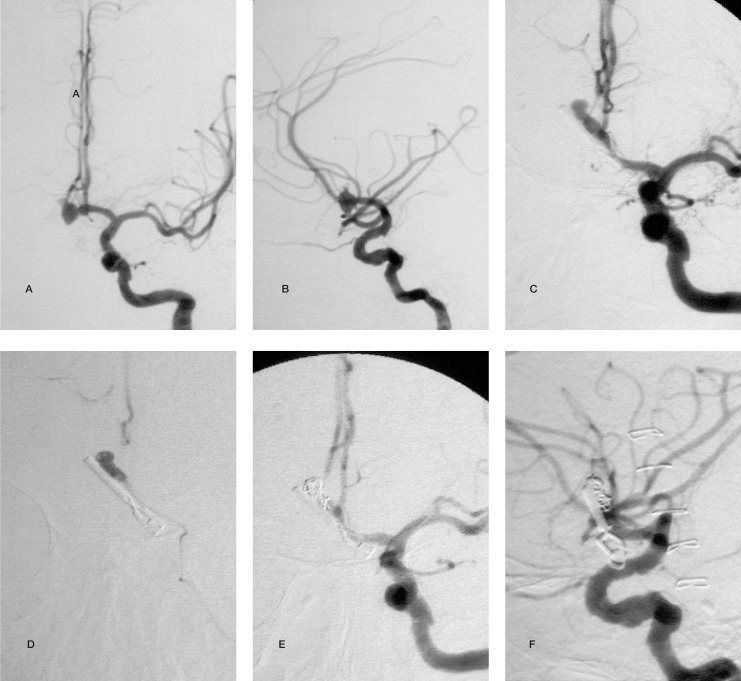
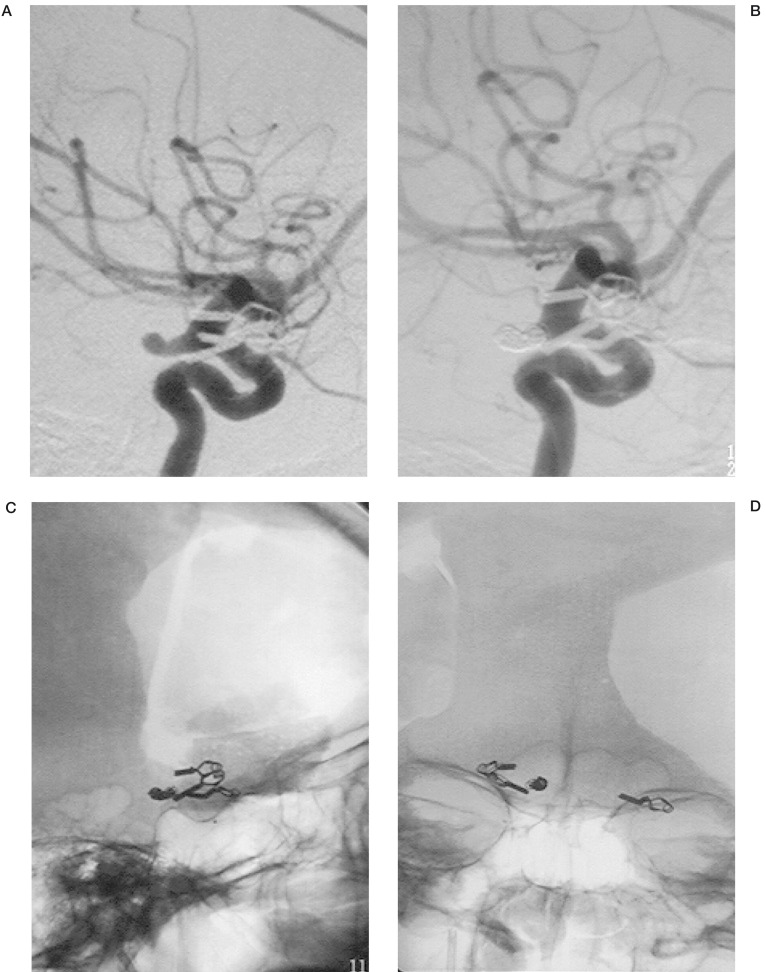
Figure 4.
Case 1. A 78-year-old female. Lt.ICAG showed ruptured Acom aneurysm, clipping at day 0. Embolization for residual aneurysm and intra-arterial injection of papaverine hydrochloride for vasospasm, after incomplete clipping at day six. (grade V → PVS). A,B) pre-clipping angiogram (A-P, lat). C) post-clipping angiogram, residual aneurysm due to incomplete clipping. D) aneurysmal angiogram. E,F) post-embolization angiogram (A-P, lat)
Figure 5.
Case 2. A 54-year-old female. Lt.ICAG showed ruptured Lt.IC-Ach aneurysm, clipping at eleven years ago. Nonruptured Rt.IC-Pc aneurysm, clipping at eight years ago. Ruptured "de novo" Rt.IC-Pc aneurysm, embolization at day one. (grade I → GR). A) pre-embolization angiogram. B) post-embolization angiogram. C) post-embolization craniogram (A-P, lat).
Intra-aneurysmal coil embolization was performed on eight patients (following wrapping in one patient), and re-clipping was performed in the other two patients. Placing a coil or microcatheter into the residual aneurysm was relatively easy during second coil embolization. In one patient with a BA-top aneurysm in whom clipping was difficult, coil embolization was performed after intentional neck-plastic clipping 1. Intra-aneurysmal coil embolization or re-clipping did not exacerbate the condition of any of these patients.
3) (figure 1)
Coil compaction occurred after coil embolization in ten patients (4.1%), and second coil embolization was required. Second coil embolization was performed on eight unruptured patients, while clipping was performed on two ruptured patients (Case 3: figure 6).
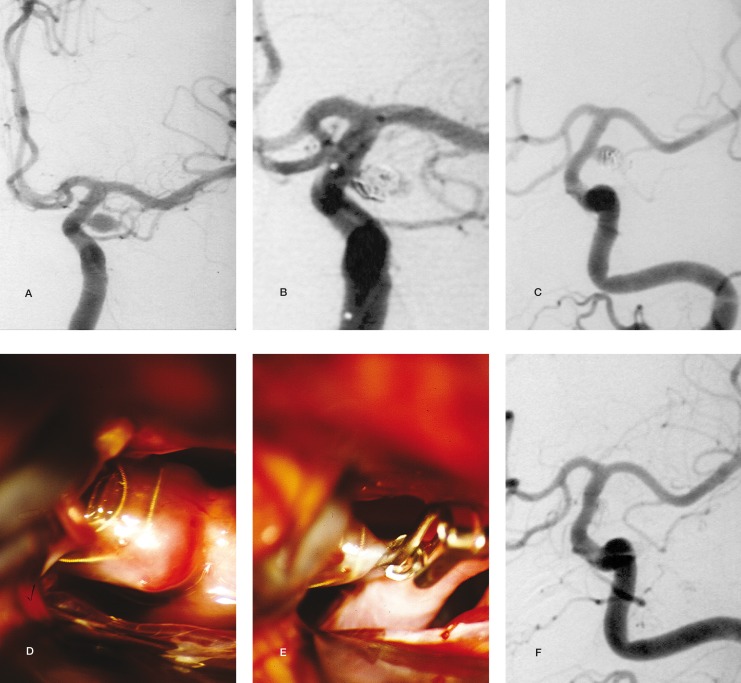
Figure 6.
Case 3. A 51-year-old female. Lt.ICAG showed ruptured Lt.IC-Pc aneurysm, embolization, at day one. Coil compaction later 2.5 Mos. after embolization. Neck clipping and aneurysmal resection at 3 Mos. (grade V → GR). A) pre-embolization angiogram. B) post-embolization angiogram, immediately. C) coil compaction later 2.5 Mos. D,E) during aneurysmal neck clipping. F) post-clipping angiogram.
New neurological symptoms did not appear postoperatively for any of the patients in Results (2) and (3). However, the existing coil in the aneurysm complicated the procedure during re-clipping.
Also, placing a coil or microcatheter into the residual aneurysm was relatively easy during second coil embolization.
4) (figure 3)
In 18 patients, coil embolization and clipping were performed for the treatment of multiple cerebral aneurysms as follows:
a) In four patients, coil embolization and clipping were combined for the treatment of multiple cerebral aneurysms, with clipping followed by coil embolization in two patients (Case 4 2: figure 7), and coil embolization followed by clipping in two patients.
b) In four patients, coil embolization was performed for the treatment of acute ruptured cerebral aneurysm and clipping for the treatment of chronic unruptured cerebral aneurysm.
c) In ten patients, clipping was performed for the treatment of acute ruptured cerebral aneurysm and coil embolization for the treatment of chronic unruptured cerebral aneurysm.
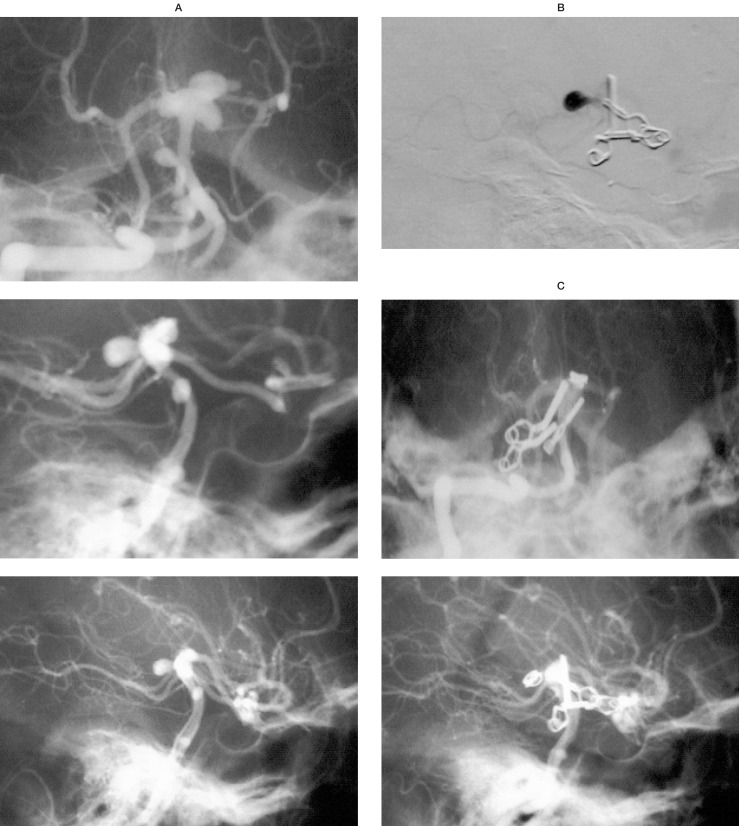
Figure 7.
Case 4. A 38-year-old female. Rt.VAG showed nonruptured multiple(5) basilar aneurysms associated with bilateral IC occlusions. Aneurysms at 2 BA-tops, BA-SCA, BA-trunk and BA-AICA. Clipping for BA-top, BA-SCA and BA-trunk, embolization for BA-top and consevation for BA-AICA. (grade 0 → GR). A) initial angiogram (A-P, oblique, lat). B: post-clipping, aneurysmal angiogram. C) post-embolization angiogram (A-P, lat).
Prognosis was favorable for all patients.
Discussion
Ever since Guglielmi et Al. developed and introduced the Guglielmi detachable coil (GDC) in 1991, intravascular therapy for cerebral aneurysm has advanced markedly, and this coil is currently being used for elderly patients, patients with severe cerebral aneurysms, patients with severe systemic complications and patients with cerebral aneurysms affecting the posterior circulation, such as lesions on the top of the basilar artery 3,4,5.
In recent years, more institutions in Japan have started performing coil embolization as the first option for treating cerebral aneurysm 6,7. Although GDCs are much better than previous devices, clipping still represents the standard therapy for cerebral aneurysm, and we also believe that clipping is the first option for treating cerebral aneurysm. This is because clipping is better suited to handle the neck of the cerebral aneurysm, coil compaction can occur over time, and the long-term stability of GDC has yet to be proven 8,9.
Whether to perform clipping or coil embolization remains a major point of contention in neurosurgery today, and conclusions cannot be drawn quickly 10. Although cerebral aneurysm is treated in routine practice, designing a form for informed consent based on scientifically sound and highly reliable therapeutic options has been difficult, and this has been discussed by the mass media 11. A sharp response followed a report published by the International Subarachnoid Aneurysm Trial (ISAT) in 2002 12. The report of ISAT compared clipping and coil embolization in the treatment of cerebral aneurysm. We believe that instead of considering clipping and coil embolization as competing techniques, better results can be obtained by taking advantage of the merits of each technique.
Table 1 and table 2 compare the advantages and disadvantages associated with clipping and coil embolization, the two techniques that are often compared in the treatment of cerebral aneurysm 13.
Table 1.
Advantages and disadvantages associated with clipping and coil embolization.
| Advantages | Disdvantages | |||
|---|---|---|---|---|
| clipping | Surgery is superior to intravascular therapy because: |
Surgery is inferior to intravascular therapy because: |
||
| 1. | Long-term therapeutic effects are clear | 1. | General anesthesia is required | |
| 2. | Accompanying lesions can be treated at the same time |
2. | Conserving perforators near an aneurysm is occasionally difficult |
|
| 3. | Vascular anatomy can be accurately ascertained macroscopically |
3. | Cerebral compression is required | |
| 4. | Intraoperative bleeding can be effectively dealt with |
4. | Blocking circulation may be necessary | |
| 5. | Skills differ between surgeons and institutions | |||
| embolization | Intravascular therapy is superior to surgery because: |
Intravascular therapy is inferior to surgery because: |
||
| 1. | General anesthesia is unnecessary (?) | 1. | Additional angiographies may be needed within a short period of time |
|
| 2. | Systemic complications are not an issue | 2. | Long-term prognosis is unknown | |
| 3. | Perforators near an aneurysm can be conserved |
3. | Embolization may not be possible depending on shape, size or location |
|
| 4. | Brain compression is unnecessary | 4. | A risk of cerebral infarction or parent vessel occlusion is present |
|
| 5. | Cost is less than surgery (?) | 5. | Dealing with intraoperative bleeding is difficult | |
| 6. | Skills differ between surgeons and institutions | |||
Table 2.
Therapeutic guidelines for acute-phase ruptured cerebral aneurysms.
| Coil embolization should be the first option in the following cases: | |
| 1) | Large aneurysm on top of the basilar artery facing superiorly or posteriorly |
| 2) | Symptomatic C3 aneurysm |
| 3) | Systemic complications |
| 4) | Age ≥70 years |
| 5) | if possible embolization after incomplete clipping |
| 6) | Far-advanced cerebral vasospasm |
| 7) | Severe cerebral aneurysm unrelated to intracerebral haematoma or hydrocephalus |
In our study, coil embolization was abandoned in 25 of the 244 patients (10.2%) in whom coil embolization was the first option. A broad neck was the most common reason for abandoning coil embolization. Coil embolization could not be performed even with balloon neck-plasty in some cases, and reports have described coil embolization combined with stent support in recent years 14. Coil embolization is one effective option for treating cerebral aneurysm following incomplete clipping or recurrent cerebral aneurysm following clipping. The reasons for this are that coil embolization is less invasive than re-clipping, and microsurgery is made difficult by the presence of an existing clip. In our patients, inserting a microcatheter into the residual aneurysm was relatively easy 1,15.
In patients with a BA-top aneurysm in whom clipping was difficult to perform, coil embolization was performed after intentional neck-plastic clipping. This therapy proved effective 1,16,17.
When coil embolization was performed after coil compaction, inserting a microcatheter into the residual aneurysm was relatively easy. However, caution must be exercised with re-clipping, as existing coils can make this procedure difficult to perform 18.
Coil embolization is generally performed on patients with ruptured or unruptured multiple cerebral aneurysms or on patients with an aneurysm on top of the basilar artery 2,19.
Conclusions
In general, cerebral aneurysm is treated by clipping while taking into account factors such as severity and age. In recent years, coil embolization has started to be performed more often. In the treatment of cerebral aneurysm, selecting proper techniques by considering the characteristics of clipping and coil embolization is desirable. In other words, strategizing therapy by taking advantages of the merits of clipping and coil embolization is important 2,10.
Footnotes
* including patients who underwent coil embolization at another institution and those in whom coil embolization was abandoned.
References
- 1.Miyazaki H, Ito S, et al. Intentional Neck Plasty for Preservation of Perforating Arteries followed by Coil Embolization for Basilar Tip Aneurysm [in Japanese] Jpn J Neurosurg (Tokyo) 2003;12:559–563. [Google Scholar]
- 2.Konishi Y, Sato E, et al. A combined surgical and endovascular treatment for a case with five vertebro-basilar aneurysms and bilateral internal carotid artery occlusions. Surg Neurol. 1998;50:363–366. doi: 10.1016/s0090-3019(97)00282-6. [DOI] [PubMed] [Google Scholar]
- 3.Guglielmi G, Vinuela F, et al. Electrothrombosis of saccular aneurysms via endovascular approach. Part 1: Electrochemical basis, technique, and experimental results. J Neurosurg. 1991;75:1–7. doi: 10.3171/jns.1991.75.1.0001. [DOI] [PubMed] [Google Scholar]
- 4.Guglielmi G, Vinuela F, et al. Electrothrombosis of saccular aneurysms via endovascular approach. Part 2: Preliminary clinical experience. J Neurosurg. 1991;75:8–14. doi: 10.3171/jns.1991.75.1.0008. [DOI] [PubMed] [Google Scholar]
- 5.Richling B, Bavinzski G, et al. Early clinical outcome of endovascular (GDC) or microsurgical techniques. A single center experience. Interventional Neuroradiology. 1995;1:19–27. doi: 10.1177/159101999500100105. [DOI] [PubMed] [Google Scholar]
- 6.Tone O, Tomita, et al. Endovascular Surgery as the First-Choice Treatment for Ruptured Cerebral Aneurysms: How Far Has It Come? Interventional Neuroradiology. 2004;10(Suppl 2):41–47. doi: 10.1177/15910199040100S209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hirohata M, Abe T, et al. Clinical Outocomes of Coil Embolization for Acutely Ruptured Aneurysm - Comparison with Results of Neck Clipping when Coil Embolization is Considered the First Option. Interventional Neuroradiology. 2004;10(Suppl 2):49–53. doi: 10.1177/15910199040100S210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Byrne JV, Sohn MJ, et al. Five-year experience in using coil embolization for ruptured intracranial aneurysms: outocome and incidence of late rebleeding. J Neurosurg. 1999;90:656–663. doi: 10.3171/jns.1999.90.4.0656. [DOI] [PubMed] [Google Scholar]
- 9.Mericle RA, Wakhloo AK, et al. Delayed aneurysm re-growth and recanalization after Guglielmi detachable coil teratment. J Neurosurg. 1998;89:142–145. doi: 10.3171/jns.1998.89.1.0142. [DOI] [PubMed] [Google Scholar]
- 10.Raftopoulos C, Mathurin P, et al. Prospective analysis of aneurysm treatment in a series of 103 consecutive patients when endovasucular embolization is censidered the first option. J Neurosurg. 2000;93:175–182. doi: 10.3171/jns.2000.93.2.0175. [DOI] [PubMed] [Google Scholar]
- 11.Gupta S. To clip or to coil? Today patients with cerebral aneurysms fece a difficult choice: brain surgery or a less proven alternativ. Time Mar 4; 2002;159:78. [PubMed] [Google Scholar]
- 12.International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. Lancet. 2002;360:1267–1274. doi: 10.1016/s0140-6736(02)11314-6. [DOI] [PubMed] [Google Scholar]
- 13.Shiokawa Y, Sato E, et al. Management Strategies for Vertebro-basilar Artery Aneurysms: Selection of the Treatment, Clipping or Coil [in Japanese] Surg Cereb Stroke (Jpn) 2000;28:137–141. [Google Scholar]
- 14.Lylyk P, Cohen JE, et al. Comvined endovascular treatment of dissecting vertebral artery aneurysms by using stents and coils. J Neurosurg. 2001;94:427–432. doi: 10.3171/jns.2001.94.3.0427. [DOI] [PubMed] [Google Scholar]
- 15.Bendok BR, Ali MJ, et al. Coiling of Cerebral Aneurysm Remnants after Clipping. Neurosurgery. 2002;51:693–698. [PubMed] [Google Scholar]
- 16.Tanaka Y, Kobayashi S, et al. Intentional body clipping of wide-necked basilar artery bifurcation aneurysms. J Neurosurg. 2000;93:169–174. doi: 10.3171/jns.2000.93.2.0169. [DOI] [PubMed] [Google Scholar]
- 17.Cockroft KM, Marks MP, et al. Planned Dierct Dualmadality Treatment of Complex Broad-necked Intracranial Aneurysms: Four Technical Case Reports. Neurosurgery. 2000;46:226–231. [PubMed] [Google Scholar]
- 18.Matsumaru Y, Sato H, et al. Retreatment of Cerebral Aneursyms after Guglielmi Detachable Coil Embolization. Interventional Neuroradiology. 2004;10(Suppl 1):167–171. doi: 10.1177/15910199040100S129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McDougall CG, Halbach VV, et al. Endovascular treatment of basilar tip aneurysm s using electrolytically detachable coils. J Neurosurg. 1996;84:393–399. doi: 10.3171/jns.1996.84.3.0393. [DOI] [PubMed] [Google Scholar]