Abstract
Highly pathogenic avian H5N1 influenza A viruses occasionally infect humans, but currently do not transmit efficiently among humans. The viral haemagglutinin (HA) protein is a known host range determinant since it mediates virus binding to host-specific cellular receptors1–3. Here, we therefore assessed the molecular changes in HA that would allow an H5 HA-possessing virus to transmit among mammals. We identified a reassortant virus with H5 HA possessing four mutations in a 2009 pandemic H1N1 virus backbone capable of droplet transmission in a ferret model. The transmissible H5 reassortant virus preferentially recognized human-type receptors, replicated efficiently in ferrets, caused lung lesions and weight loss, but it was not highly pathogenic and did not cause mortality. These results suggest that H5 HA can convert to an HA that supports efficient viral transmission in mammals. However, we do not know whether the four mutations in the H5 HA identified in this study would render a wholly avian H5N1 virus transmissible. The genetic origin of the remaining seven viral genes may also critically contribute to transmissibility in mammals. Nevertheless, as H5N1 viruses continue to evolve and infect humans, receptor-binding variants of H5N1 viruses with pandemic potential, including avian-human reassortant viruses as tested here, may emerge. Our findings emphasize the need for pandemic preparedness for H5 HA-possessing viruses and will help individuals conducting surveillance in regions with circulating H5N1 viruses to recognize key residues that predict the pandemic potential of isolates, which will inform the development, production, and distribution of effective countermeasures.
Although H5N1 viruses continue to cause outbreaks in poultry with human cases in Indonesia, Viet Nam, Egypt and elsewhere (http://www.who.int/influenza/human_animal_interface/H5N1_cumulative_table_archives/en/index.html), they have not acquired the ability to cause human-to-human transmission. Investment in H5N1 vaccines has therefore been questioned. However, since humans lack immunity to influenza viruses possessing an H5 HA, the emergence of a transmissible H5 HA-possessing virus would likely cause a pandemic. To better prepare for such a scenario, it is critical to understand the molecular changes that may render H5 HA-possessing viruses transmissible in mammals. Such knowledge would allow us to monitor circulating or newly emerging variants for their pandemic potential, focus eradication efforts on viruses that already have acquired subsets of molecular changes critical for transmission in mammals, stockpile antiviral compounds in regions where such viruses circulate, and initiate vaccine generation and large-scale production prior to a pandemic. Here, we therefore studied the molecular features that would render H5 HA-possessing viruses transmissible in mammals.
Previous studies suggested that HA plays a major role in host range restriction of influenza A viruses1–3. The HA of human isolates preferentially recognizes sialic acid linked to galactose by α2,6-linkages (Siaα2,6Gal), whereas the HA of avian isolates preferentially recognizes sialic acid linked to galactose by α2,3-linkages (Siaα2,3Gal)3. A small number of avian H5N1 viruses isolated from humans show limited binding to human-type receptors, a property conferred by several amino acid changes in HA4–9. None of the H5N1 viruses tested transmitted efficiently in a ferret model10–13, although, while our paper was under review, Chen et al.14 reported that a virus with a mutant H5 HA and a neuraminidase (NA) of a human virus in the H5N1 virus background caused respiratory droplet transmission in one of two contact ferrets. A previous study reported that H5N1 and 2009 pandemic H1N1 viruses show high genetic compatibility15,16, providing an opportunity for the generation of avian-human reassortant H5N1 viruses. To assess the pandemic potential of such reassortants, we generated a virus possessing the HA from an H5N1 virus and the seven remaining gene segments from a 2009 pandemic H1N1 virus (H5HA/pdm09). In receptor-binding studies and animal experiments, we identified a derivative of this reassortant virus that possessed four mutations in its HA protein.
The mutant H5 HA reassortant (H5HA-mutant/pdm09) was capable of respiratory droplet transmission in ferrets, which are widely accepted as an animal model for influenza virus transmissibility and pathogenesis studies. In this transmission experiment, we placed naïve ferrets in wireframe cages next to ferrets inoculated with 106 plaque-forming units (PFU) of virus. This experimental setting allowed the exchange of respiratory droplets between the inoculated and non-inoculated ferrets, but prevented transmission by direct or indirect contact. Similar to previous transmission experiments17, a pdm09 virus was efficiently transmitted via respiratory droplets to all three contact ferrets, as evidenced by the detection of virus in nasal washes and haemagglutinin-inhibition (HI) antibody in these animals (Table 1 and Fig. 1). As expected, the H5HA/pdm09 virus was not transmitted; neither virus shedding nor seroconversion was detected in any contact animals. In the H5HA-mutant/pdm09-inoculated group, virus was recovered from 4 of the 6 contact ferrets between days 3 and 7 post-contact. Moreover, seroconversion was detected in all six animals. No animals died in the course of these transmission experiments. Significantly, the transmission pattern with the H5HA-mutant/pdm09 virus was comparable to that of the 1918 pandemic H1N1 virus when tested under the same experimental conditions; the 1918 pandemic virus was recovered from the nasal washes of 2 of 3 contact animals (unpublished data). These findings demonstrate that an H5 HA can support respiratory droplet transmission of an avian-human reassortant virus among ferrets.
Table 1.
Transmission in ferrets inoculated with H5 avian-human reassortant viruses
| Virus | Inoculated ferrets
|
Contact ferrets
|
|||
|---|---|---|---|---|---|
| Weight loss (%)a | Peak virus titre in nasal wash [mean log10 PFU/ml] (day pi) | Seroconversion: positive/total (HI titre)b | Virus detection in nasal wash: positive/total | Seroconversion: positive/total (HI titre) | |
| pdm09 | 3/3 (15.1) | 7.5 (1) | 3/3 (≥1280, ≥1280, ≥1280) | 3/3 | 3/3 (≥1280, ≥1280, ≥1280) |
| H5HA/pdm09 | 3/3 (5.9) | 5.3 (5) | 3/3 (80, 40, 80) | 0/3 | 0/3 (<10, <10, <10) |
| H5HA-mutant/pdm09 | 6/6 (9.8) | 6.1 (5) | 6/6 (≥1280, ≥1280, 640, ≥1280, ≥1280, ≥1280) | 4/6 | 6/6 (640, 640, ≥1280, 80, ≥1280, 320) |
Maximum percent weight loss is shown.
Haemagglutination inhibition (HI) assays were carried out with homologous virus and turkey red blood cells. pi, post-inoculation. PFU, plaque-forming units.
Figure 1.
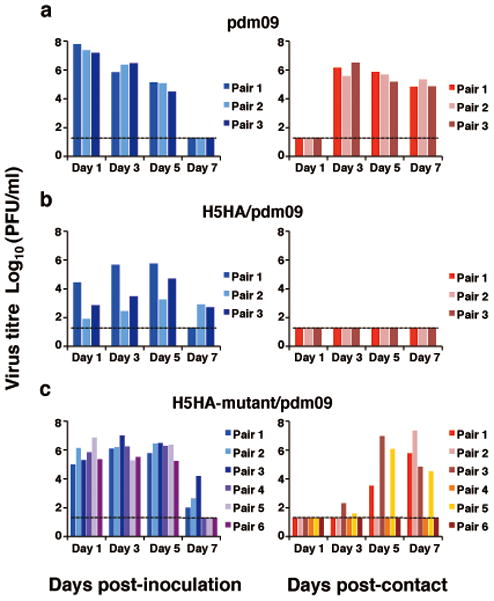
Respiratory droplet transmission of H5 avian-human reassortant viruses in ferrets. Groups of three or six ferrets were inoculated intranasally with 106 PFU of pdm09 (a), H5HA/pdm09 (b), or H5HA-mutant/pdm09 (c). One day post-infection, three or six naive ferrets were placed in each adjacent cage. Nasal washes were collected every other day from both inoculated (left panel) and contact (right panel) animals for virus titration. Virus titres in organs were determined by plaque assay in MDCK cells. The lower limit of detection is indicated by the horizontal dashed line.
To assess the replication and pathogenicity of the transmissible H5N1 avian-human reassortant virus, we infected ferrets with 106 PFU of virus and determined virus titres at 3 and 6 days post-infection. The pdm09 virus replicated efficiently in the respiratory organs of infected animals, and was isolated from the colon, but not from any other organ tested (Fig. 2 and Table 2). The H5HA/pdm09 virus replicated to titres comparable to those of the pdm09 in nasal turbinates, but substantially less in the lungs. The H5HA-mutant/pdm09 virus replicated efficiently in nasal turbinates and was isolated from brain tissue in one of the three ferrets infected.
Figure 2.
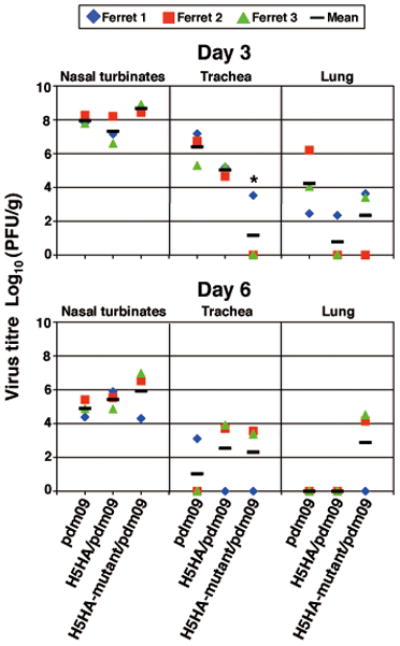
Virus replication in respiratory organs. Ferrets were infected intranasally with 106 PFU of virus. Three ferrets per group were euthanized on days 3 and 6 after infection for virus titration. Virus titres in nasal turbinates, trachea, and lung were determined by plaque assay in MDCK cells. Horizontal bars show the mean. Asterisks indicate virus titres significantly different from that of pdm09 (Dunnett’s test; P < 0.05).
Table 2.
Virus titres in tissues of ferrets infected with H5 avian-human reassortant viruses
| Virus | Days post infection | Virus titre (mean log10 PFU±SD/g) in:
|
||||
|---|---|---|---|---|---|---|
| Nasal turbinates | Trachea | Lungs | Brain | Colon | ||
| pdm09 | 3 | 8.0±0.3 | 6.4±1.0 | 4.2±1.9 | - | 1.9 |
| 6 | 4.9±0.5 | 3.1 | - | - | - | |
|
| ||||||
| H5HA/pdm09 | 3 | 7.3±0.8 | 5.0±0.3 | 2.3 | - | 2.1±0.6 |
| 6 | 5.4±0.5 | 3.7, 3.9 | - | - | 3.0 | |
|
| ||||||
| H5HA-mutant/pdm09 | 3 | 8.7±0.2 | 3.5 | 3.6, 3.4 | 2.9 | - |
| 6 | 5.9±1.4 | 3.6, 3.4 | 4.2, 4.5 | - | - | |
Ferrets were infected intranasally with 106 PFU (500 μl) of virus. Three ferrets per group were euthanized on days 3 and 6 after infection for virus titration. When virus was not recovered from all three ferrets, individual titres were recorded. No virus was detected in liver, kidney or spleen samples.
Pathological examination revealed similar histological changes and levels of viral antigens in the nasal mucosa of pdm09- and H5HA-mutant/pdm09-infected ferrets (Fig. 3). In the H5HA/pdm09 groups, however, less tissue damage was found in the nasal mucosa compared to the pdm09 group on day 3 post infection (Dunnett’s test; P=0.0057 and 0.0175, respectively; Fig. 3a,c). In addition, all three viruses caused lung lesions (Fig. 3b,c).
Figure 3.
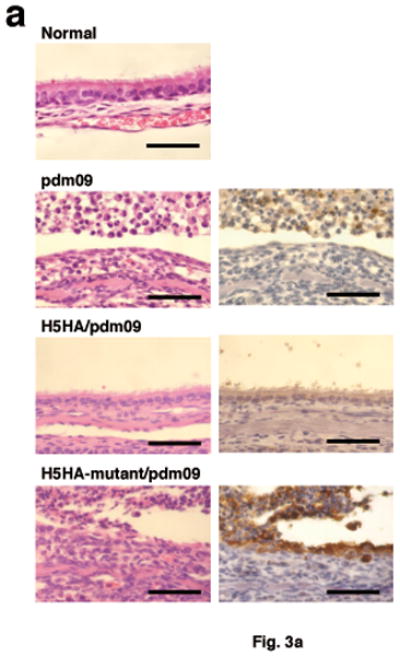
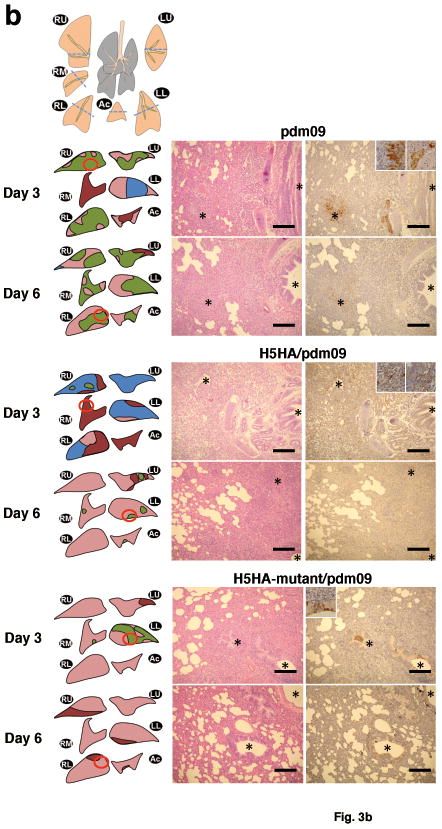
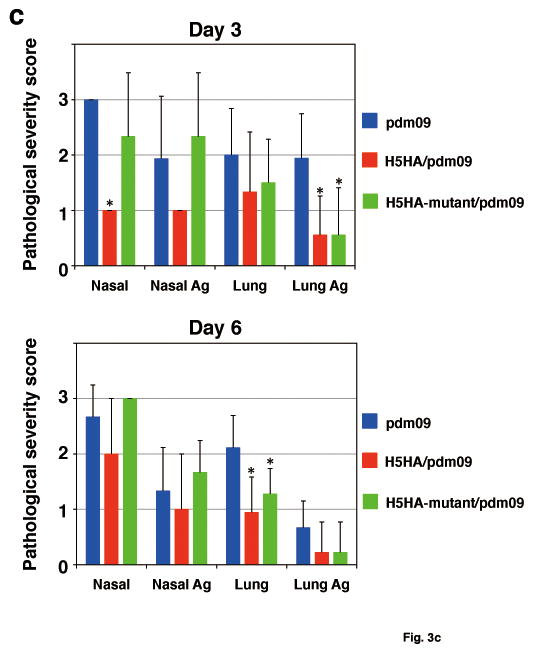
Pathological analyses of H5 avian-human reassortant viruses. a, Representative histological changes in nasal turbinates from influenza virus-infected ferrets. Three ferrets per group were infected intranasally with 106 PFU of virus, and tissues were collected on day 3 after infection for pathological examination. Uninfected ferret tissues served as negative controls (normal). Left panel, haematoxylin-eosin staining. Right panel, immunohistochemical staining for viral antigen detection (brown staining). Bars, 50 μm. b, Representative histological changes in lungs from influenza virus-infected ferrets. Three ferrets per group were infected intranasally with 106 PFU of virus, and tissues were collected on days 3 and 6 after infection for pathological examination. Left panel, the histological findings in the lungs are represented as schematic diagrams for one of the three animals per group. Cutting aspects of each lung lobe are illustrated with lesion distribution: blue, normal appearance; green, bronchopneumonia; red, alveolitis; and pink, interstitial thickening. Red circles indicate the areas shown in the histology sections. RU, right upper lobe; LU, left upper lobe; RM, right middle lobe; LL, left lower lobe; RL, right lower lobe; Ac, accessory lobe. Middle panel, haematoxylin-eosin staining. Right panel, immunohistochemical staining for viral antigen detection (brown staining). Bronchi are indicated by asterisks “*”. Inserts show a higher magnification of the antigen-positive cells. The lesions were diagnosed as bronchopneumonia, when the lung lesion was observed mainly around the inflammatory or viral antigen-positive bronchi/bronchioles. By contrast, the lesions were diagnosed as alveolitis when bronchi and bronchioles remained intact and inflammation was observed mainly in alveoli. Interstitial thickening was occasionally observed as stimulation by inoculum or secondary to the severe inflammation of adjacent tissue. Bars, 200 μm. c, Pathological severity scores in infected ferrets. To represent comprehensive histological changes, respiratory tissue slides were evaluated by scoring the pathological changes and viral antigen expression levels. The pathological scores were determined for each animal in each group (n = 3/group on days 3 and 6 pi) using the following scoring system: 0 = no pathological change/antigen negative; 1 = affected area (<30%) or only interstitial lesion/rare viral antigens; 2 = affected area (<80%, ≥30%)/moderate viral antigens; 3 = severe lesion ( ≥80%)/many viral antigens; Nasal: pathologic changes in the nasal mucosa, Nasal Ag: viral antigens in the nasal mucosa, Lung: pathologic changes in the lungs, Lung Ag: viral antigens in the lungs. Asterisks indicate virus pathological scores significantly different from that of pdm09 (Dunnett’s test; P < 0.05).
To understand the molecular basis for the transmissibility of the H5HA-mutant/pdm09 virus in ferrets, we evaluated the receptor-binding property of a virus with the mutant H5 HA in solid phase assays. In these experiments, the virus with the mutant H5 HA preferentially bound to human-type receptors, Siaα2,6Gal, as did a virus with the HA of a seasonal human virus (Fig. 4a). A virus containing the wild-type H5 HA bound only to avian-type receptors, Siaα2,3Gal.
Figure 4.
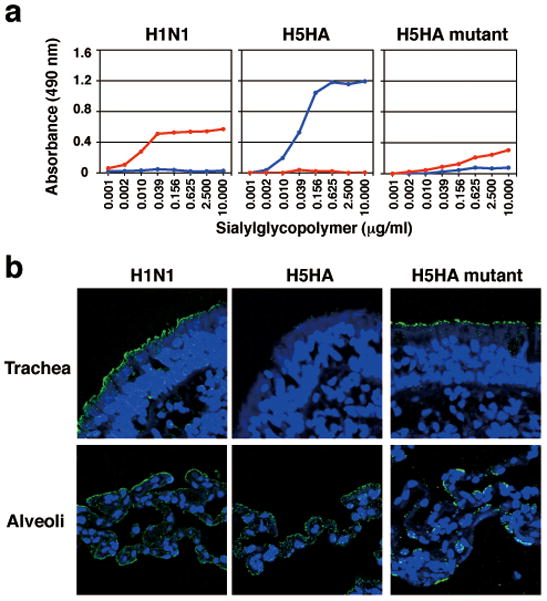
Characterization of the receptor-binding properties of an H5 HA mutant virus possessing four mutations in its HA protein. a, Binding of an H5 HA-mutant virus to sialylglycopolymers in solid-phase binding assays. A human seasonal H1N1 virus, a wild-type avian H5 HA virus, and a mutant H5 HA virus were compared for their ability to bind to sialylglycopolymers containing either α2,3-linked (blue) or α2,6-linked (red) sialic acids. b, Binding of an mutant H5 HA virus to human respiratory tissues. Human, wild-type H5, and mutant H5 HA viruses were incubated with human tissue sections and then stained with the appropriate antibody (anti-human virus antiserum to detect human influenza virus binding or anti-H5 HA antibodies to detect binding by wild-type and mutant H5 HA viruses). All sections were subsequently incubated with fluorescent-labeled secondary antibodies and Hoechst dye (blue). Green stain indicates virus binding.
To determine whether the H5HA-mutant/pdm09 virus with human-type receptor specificity could bind to cells in the human respiratory tract, sections of human tracheal and lung tissues were exposed to viruses with a human virus HA, a wild-type H5 HA and the mutant H5 HA that supports virus transmission. All viruses bound extensively to the alveolar epithelial surface of human lung tissue, where both human- and avian-type receptors are present18 (Fig. 4b). Unlike the virus with the wild-type H5 HA, the virus with the mutant H5 HA attached to human tracheal epithelia, where predominantly human-type receptors are present, as did the virus with the human virus HA. These results suggest that the recognition of human-type receptors present in human respiratory organs is required for virus transmission in mammals. However, findings by others12,14 as well as information in the full version of this paper19 have shown that human-type receptor-binding specificity is not sufficient to confer respiratory droplet transmission in ferrets. This is in line with our hypothesis that a subset of the HA mutations in the H5HA-mutant/pdm09 virus affected HA stability, thus offsetting the decrease in stability conferred by the mutations that directly affect receptor-binding specificity19. Together, these findings suggest that a fine balance of mutations affecting different functions in HA may be critical to confer transmissibility in mammals.
Our transmissible H5HA-mutant/pdm09 virus possesses seven segments (all but the HA segment) from a human pandemic 2009 H1N1 virus. Human virus-characteristic amino acids in these seven segments may have critically contributed to the respiratory droplet transmission of the H5HA-mutant/pdm09 virus in ferrets. Examples include amino acids in the PB2 polymerase protein that confer efficient replication in mammalian, but not avian cells20–24. Since the PB2 gene of the H5HA-mutant/pdm09 virus is of human virus origin, the virus possesses high replicative ability in mammalian cells. In contrast, most avian virus PB2 proteins lack these human-type amino acids, although one of these changes (a glutamic acid-to-lysine mutation at position 627) is found in highly pathogenic avian H5N1 viruses circulating in the Middle East25.
As a second example, the viral NA gene may contribute to viral transmissibility. The NA protein cleaves α-ketosidic linkages between a terminal sialic acid and an adjacent sugar residue, an activity that balances the sialic acid-binding activity of HA. A recent study found that a human virus NA gene was critical to confer limited transmissibility to a mutant H5 avian-human reassortant virus14. In general, a human-type receptor-recognizing H5 HA alone may not be sufficient to confer transmissibility in mammals, but may have to act in concert with other human virus-characteristic traits (in PB2, NA, and/or other viral proteins). Therefore, at this point, we cannot predict whether the four mutations in the H5 HA identified in our study would render a wholly avian H5N1 virus transmissible.
To assess if current control measures may be effective against the mutant transmissible virus, we examined the reactivity of sera from individuals vaccinated with an H5N1 prototype vaccine26 against a virus possessing the mutant H5 HA gene, the NA gene of a H5N1 virus, and the remaining six genes from A/Puerto Rico/8/34 (H1N1) (PR8) (designated H5HA-mutant/PR8). We found that pooled human sera from individuals immunized with this vaccine reacted with the H5HA-mutant/PR8 at a higher titre than with a virus possessing the HA and NA genes of a H5N1 virus and the remaining genes from PR8 (designated H5HA/PR8) (Table 3), suggesting that current H5N1 vaccines would be efficacious against H5HA-mutant/pdm09 virus. In addition, the transmissible reassortant mutant virus was highly susceptible to a licensed NA inhibitor, oseltamivir (Table 4). These experiments show that appropriate control measures would be available to combat the transmissible virus described in this study.
Table 3.
Haemagglutination inhibition (HI) reactions of H5 HA reassortant viruses against post-vaccination sera
| Virus | Human seruma
|
|
|---|---|---|
| High titer pool (NR4109) | Low titer pool (NR4110) | |
| H5HA/PR8 | 40 | 20 |
| H5HA-mutant/PR8 | 160 | 40 |
Pooled human sera from individuals vaccinated with a monovalent influenza subvirion vaccine, rgA/Vietnam/1203/2004×A/PR/8/34 (H5N1), were obtained from BEI Resources (Manassas, VA).
Table 4.
Virus susceptibility to oseltamivir in cell culture
| Virus | IC50 of oseltamivir carboxylatea (nM) |
|---|---|
| A/California/04/2009 (H1N1) (oseltamivir-susceptible control) | 1.4 ± 0.3b |
| A/Osaka/180/2009 (H1N1) (oseltamivir-resistant control) | 1133.5 ± 14.9 |
| H5HA-mutant/pdm09 | 1.0 ± 0.3 |
Oseltamivir carboxylate is the active form of oseltamivir.
IC50 value: mean ± standard deviation from triplicate assays of oseltamivir concentration needed to inhibit neuraminidase activity by 50%.
Since highly pathogenic H5N1 viruses first emerged in the late 1990s, pandemic preparations have been underway to develop appropriate vaccines and expand the array of effective antivirals that might be needed should these viruses acquire the ability to transmit in humans. We do not know whether the mutations that we identified in this study that allowed the H5HA-mutant/pdm09 virus to become transmissible in ferrets would also support sustained human-to-human transmission. However, as H5N1 viruses continue to evolve and infect people, receptor-binding variants of H5N1 viruses including avian-human reassortant viruses as tested here may emerge.
Our study suggests the pandemic potential of viruses possessing an H5 HA. Although current H5N1 vaccines may protect against a virus similar to that tested here, the continued evolution of H5N1 viruses reinforces the need to prepare and update candidate vaccines to H5 viruses. We strongly endorse sharing our data globally. They will help individuals conducting surveillance in regions with circulating H5N1 viruses (e.g., Egypt, Indonesia, Viet Nam) to recognize key residues that predict the pandemic potential of isolates. Rapid responses in a potential pandemic situation are essential to generating appropriate vaccines and initiating other public health measures to control infection. Our findings are of critical importance to those making public health and policy decisions.
Our research answers a fundamental question in influenza research: can H5 HA-possessing viruses support transmission in mammals? Details available in the full version of this paper19 advance our understanding of influenza host specificity and the evolution of the HA molecule. These findings could form the basis for additional experiments to increase our understanding of the basic biology of influenza virus transmission.
Methods
Cells
Madin-Darby canine kidney (MDCK) cells were maintained in Eagle’s minimal essential medium containing 5% newborn calf serum in 5% CO2 at 37°C.
Plasmid construction and reverse genetics
Plasmid constructs for viral RNA production (pPolI), containing the genes of the H1N1 and H5N1 influenza A viruses flanked by the human RNA polymerase I promoter and the mouse RNA polymerase I terminator, were constructed as described27. All transfectant viruses were generated by using reverse genetics essentially as described by Neumann et al.27. Recombinant viruses were amplified in MDCK cells and stored at −80°C until use. All experiments with the wild-type H5HA/pdm09, H5HA-mutant/pdm09 reassortants, and pdm09 viruses were performed in enhanced biosafety level 3 (BSL-3) containment laboratories approved for such use by the Centers for Disease Control and Prevention (CDC) and the United States Department of Agriculture (USDA).
Experimental infection of ferrets
We used 6- to 10-month-old female ferrets (Triple F Farms) that were serologically negative by HI assay for currently circulating human influenza viruses. Six ferrets per group were anesthetized intramuscularly with ketamine and xylazine (5-30 mg and 0.2-6 mg per kg of body weight, respectively) and inoculated intranasally with 106 PFU (500 μl) of viruses. On days 3 and 6 post-infection, 3 ferrets per group were euthanized for virologic and pathologic examinations. The virus titres in various organs were determined by plaque assays in MDCK cells.
Excised tissue samples of nasal turbinates, trachea, lungs, brain, liver, spleen, kidney, and colon from euthanized ferrets were preserved in 10% phosphate-buffered formalin. Tissues were then trimmed and processed for paraffin embedding and cut into 5-μm thick sections. One section from each tissue sample was stained by using a standard hematoxylin-and-eosin procedure, while another was processed for immunohistological staining with a mixture of two anti-influenza virus rabbit antibodies (1:2000; R309 and anti-H5HA; both prepared in our laboratory) that react with pdm09 and H5HA/pdm09, respectively. Specific antigen-antibody reactions were visualized by using an indirect two-step dextran-polymer technique (Dako EnVision system; Dako) and 3,3′ diaminobenzidine tetrahydrochloride staining (Dako).
Ferret transmission study
For transmission studies in ferrets, animals were housed in adjacent transmission cages that prevented direct and indirect contact between animals but allowed spread of influenza virus through the air (Showa Science). Three or six ferrets were inoculated intranasally with 106 PFU (500 μl) of virus (inoculated ferrets). Twenty-four hours after infection, three or six naïve ferrets were each placed in a cage adjacent to an inoculated ferret (contact ferrets). The ferrets were monitored for changes in body weight and the presence of clinical signs. To assess viral replication in nasal turbinates, we determined viral titres in nasal washes collected from virus-inoculated and contact ferrets on day 1 after inoculation or co-housing, respectively, and then every other day. Animal studies were performed in accordance with Animal Care and Use Committee guidelines of the University of Wisconsin-Madison.
Serologic tests
Serum samples were collected between days 14 and 20 post-infection, treated with receptor-destroying enzyme, heat-inactivated at 56°C for 30 min, and tested by use of an HI assay with 0.5% turkey red blood cells (TRBCs)28. Viruses bearing homologous HA were used as antigens for the HI test.
NA inhibition assay
To assess the sensitivity of viruses to the NA inhibitor oseltamivir, NA inhibition assays were performed as described previously17.
Solid-phase binding assay
Viruses were grown in MDCK cells, clarified by low-speed centrifugation, laid over a cushion of 30% sucrose in phosphate-buffered saline (PBS), and ultracentrifuged at 25,000 rpm for 2 h at 4°C. Virus stocks were aliquoted and stored at −80°C. Virus concentrations were determined by using HA assays with 0.5 % (vol/vol) TRBC. The direct receptor-binding capacity of viruses was examined by use of a solid-phase binding assay as previously described9. Microtitre plates (Nunc) were incubated with the sodium salts of sialylglycopolymers [poly-L-glutamic acid backbones containing N-acetylneuraminic acid linked to galactose through either an α2,3 (Neu5Acα2,3Galβ1,4GlcNAcβ1-pAP) or an α2,6 (Neu5Acα2,6Galβ1,4GlcNAcβ1-pAP) bond] in PBS at 4°C overnight. After the glycopolymer solution was removed, the plates were blocked with 0.15 ml of PBS containing 4% bovine serum albumin (BSA) at room temperature for 1 h. Following four successive washes with ice-cold PBS, the plates were incubated in a solution containing influenza virus (8 to 32 HA units in PBS) at 4°C overnight. After washing as described above, the plates were incubated for 2 h at 4°C with rabbit polyclonal antiserum to either human H1N1 or avian H5N1 virus. The plates were then washed again as before and incubated with horseradish peroxidase (HRP)-conjugated goat anti-rabbit IgG antiserum for 2 h at 4°C. After washing, the plates were incubated with O-phenylenediamine (Sigma) in PBS containing 0.01% H2O2 for 10 min at room temperature, and the reaction was stopped with 0.05 ml of 1 M HCl. The optical density at 490 nm was determined in a plate reader (Infinite M1000; Tecan).
Virus binding to human airway tissues
Paraffin-embedded normal human trachea (US Biological) and lung (BioChain) tissue sections were deparaffinized and rehydrated. Sections were then blocked by using 4% BSA in PBS and covered with virus suspensions (64 HA units in PBS) at 4°C overnight. After being washed four times in ice-cold PBS, the sections were incubated with primary antibodies for 3 h at 4°C. The primary antibodies used were as follows: a pool of mouse anti-H5 HA monoclonal antibodies or rabbit anti-human H1N1 virus polyclonal antibodies. Antibody binding was detected by using an IgG secondary antibody conjugated with Alexa Fluor 488 (Molecular Probes). Sections were also counterstained with Hoechst 33342, trihydrochloride, trihydrate (Molecular Probes). The samples were examined by using confocal laser scanning microscopy (model LSM 510; Carl Zeiss).
Statistical Analysis
All statistical analyses were performed using JMP 9.0.0 (SAS Institute Inc.). The statistical significance of differences between pdm09, H5HA/pdm09, and H5HA-mutant/pdm09 viruses was determined by using Dunnett’s test. P values of < 0.05 were considered significant.
Special comments regarding biosafety & biosecurity
All recombinant DNA protocols were approved by the University of Wisconsin-Madison’s Institutional Biosafety Committee after risk assessments were conducted by the Office of Biological Safety, and by the University of Tokyo’s Subcommittee on Living Modified Organisms, and, when required, by the competent minister of Japan. In addition, University of Wisconsin-Madison Biosecurity Task Force regularly reviews the research program and ongoing activities of the laboratory. The task force has a diverse skill set and provides support in the areas of biosafety, facilities, compliance, security, and health. Members of the Biosecurity Task Force are in frequent contact with the principal investigator and laboratory personnel to provide oversight and assure biosecurity. Experiments with viruses possessing the wild-type HA cleavage site were performed in enhanced BSL3 containment laboratories approved for such use by the CDC and the USDA. Biosecurity monitoring of the facility is ongoing. All personnel undergo Select Agent security risk assessment by the United States Criminal Justice Information Services Division and complete rigorous biosafety, BSL3, and Select Agent training prior to participating in BSL3-level experiments. Refresher training is scheduled on a regular basis. The principal investigator participates in training sessions and emphasizes compliance to maintain safe operations and a responsible research environment. The laboratory occupational health plan is in compliance with the University of Wisconsin-Madison Occupational Health Program. The research program, procedures, occupational health plan, documentation, security, and facilities are reviewed at regular intervals by the CDC and the Animal and Plant Health Inspection Service (APHIS) as part of the University of Wisconsin-Madison Select Agent Program.
Supplementary Material
Acknowledgments
The authors would like to acknowledge D. Holtzman for his contributions to the initial concept for this project and thoughtful scientific discussions. We thank M. McGregor, R. Moritz, L. Burley, K. Moore, A. Luka, J. Bettridge, N. Fujimoto, and M. Ito for technical support; S. Watson for editing the manuscript. This work was supported by the Bill & Melinda Gates Foundation (Grants #48339 and #OPPGH5383), by a Grant-in-Aid for Specially Promoted Research from the Ministry of Education, Culture, Sports, Science, and Technology of Japan, by ERATO (Japan Science and Technology Agency), and by the National Institute of Allergy and Infectious Diseases Public Health Service Research grants. The following reagents were obtained from the NIH Biodefense and Emerging Infections Research Resources Repository, NIAID, NIH: Polyclonal Anti-Monovalent Influenza Subvirion Vaccine rgA/Vietnam/1203/2004 (H5N1), (antiserum, Human), High Titer Pool, NR-4109 and Low Titer Pool, NR-4110.
Footnotes
Contributions
M.I., T.W., M.H., S.C.D., M.O., K.S., G.Z., A.H., H.K., S.W., C.L., S.Y., M.K., Y.S., E.A.M., G.N. and Y.K. designed the experiments; M.I., T.W., M.H., S.C.D., M.O., K.S., G.Z., A.H., H.K., S.W. C.L., S.Y. and M.K. performed the experiments; M.I., T.W., M.H., S.C.D., M.O., K.S., G.Z., A.H., H.K., S.W., C.L., E.K., S.Y., M.K., Y.S., E.A.M., G.N. and Y.K. analyzed the data; M.I., T.W., M.H., S.C.D., K.S., E.A.M., G.N. and Y.K. wrote the manuscript. M.I., T.W. and M.H. contributed equally to this work.
Competing financial interests
Y.K. has received speaker’s honoraria from Chugai Pharmaceuticals, Novartis, Daiichi-Sankyo, Toyama Chemical, Wyeth, and GlaxoSmithKline; grant support from Chugai Pharmaceuticals, Daiichi Sankyo Pharmaceutical, Toyama Chemical, Otsuka Pharmaceutical Co., Ltd.; is a consultant for Theraclone and Crucell, and is a founder of FluGen. G.N. is a consultant for Theraclone and a founder of FluGen.
References
- 1.Glaser L, et al. A single amino acid substitution in 1918 influenza virus hemagglutinin changes receptor binding specificity. J Virol. 2005;79:11533–11536. doi: 10.1128/JVI.79.17.11533-11536.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matrosovich M, et al. Early alterations of the receptor-binding properties of H1, H2, and H3 avian influenza virus hemagglutinins after their introduction into mammals. J Virol. 2000;74:8502–8512. doi: 10.1128/jvi.74.18.8502-8512.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rogers GN, Paulson JC. Receptor determinants of human and animal influenza virus isolates: differences in receptor specificity of the H3 hemagglutinin based on species of origin. Virology. 1983;127:361–373. doi: 10.1016/0042-6822(83)90150-2. [DOI] [PubMed] [Google Scholar]
- 4.Auewarakul P, et al. An avian influenza H5N1 virus that binds to a human-type receptor. J Virol. 2007;81:9950–9955. doi: 10.1128/JVI.00468-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gambaryan A, et al. Evolution of the receptor binding phenotype of influenza A (H5) viruses. Virology. 2006;344:432–438. doi: 10.1016/j.virol.2005.08.035. [DOI] [PubMed] [Google Scholar]
- 6.Stevens J, et al. Recent avian H5N1 viruses exhibit increased propensity for acquiring human receptor specificity. Journal of molecular biology. 2008;381:1382–1394. doi: 10.1016/j.jmb.2008.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang W, et al. Glycosylation at 158N of the hemagglutinin protein and receptor binding specificity synergistically affect the antigenicity and immunogenicity of a live attenuated H5N1 A/Vietnam/1203/2004 vaccine virus in ferrets. J Virol. 2010;84:6570–6577. doi: 10.1128/JVI.00221-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Watanabe Y, et al. Acquisition of human-type receptor binding specificity by new H5N1 influenza virus sublineages during their emergence in birds in Egypt. PLoS pathogens. 2011;7:e1002068. doi: 10.1371/journal.ppat.1002068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yamada S, et al. Haemagglutinin mutations responsible for the binding of H5N1 influenza A viruses to human-type receptors. Nature. 2006;444:378–382. doi: 10.1038/nature05264. [DOI] [PubMed] [Google Scholar]
- 10.Jackson S, et al. Reassortment between avian H5N1 and human H3N2 influenza viruses in ferrets: a public health risk assessment. J Virol. 2009;83:8131–8140. doi: 10.1128/JVI.00534-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maines TR, et al. Lack of transmission of H5N1 avian-human reassortant influenza viruses in a ferret model. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:12121–12126. doi: 10.1073/pnas.0605134103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maines TR, et al. Effect of receptor binding domain mutations on receptor binding and transmissibility of avian influenza H5N1 viruses. Virology. 2011;413:139–147. doi: 10.1016/j.virol.2011.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yen HL, et al. Inefficient transmission of H5N1 influenza viruses in a ferret contact model. J Virol. 2007;81:6890–6898. doi: 10.1128/JVI.00170-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen LM, et al. In vitro evolution of H5N1 avian influenza virus toward human-type receptor specificity. Virology. 2012;422:105–113. doi: 10.1016/j.virol.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cline TD, et al. Increased pathogenicity of a reassortant 2009 pandemic H1N1 influenza virus containing an H5N1 hemagglutinin. J Virol. 2011;85:12262–12270. doi: 10.1128/JVI.05582-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Octaviani CP, Ozawa M, Yamada S, Goto H, Kawaoka Y. High level of genetic compatibility between swine-origin H1N1 and highly pathogenic avian H5N1 influenza viruses. J Virol. 2010;84:10918–10922. doi: 10.1128/JVI.01140-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Itoh Y, et al. In vitro and in vivo characterization of new swine-origin H1N1 influenza viruses. Nature. 2009;460:1021–1025. doi: 10.1038/nature08260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shinya K, et al. Avian flu: influenza virus receptors in the human airway. Nature. 2006;440:435–436. doi: 10.1038/440435a. [DOI] [PubMed] [Google Scholar]
- 19.The full version of this paper. 2012 [Google Scholar]
- 20.Bussey KA, Bousse TL, Desmet EA, Kim B, Takimoto T. PB2 residue 271 plays a key role in enhanced polymerase activity of influenza A viruses in mammalian host cells. J Virol. 2010;84:4395–4406. doi: 10.1128/JVI.02642-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hatta M, Gao P, Halfmann P, Kawaoka Y. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science. 2001;293:1840–1842. doi: 10.1126/science.1062882. [DOI] [PubMed] [Google Scholar]
- 22.Li Z, et al. Molecular basis of replication of duck H5N1 influenza viruses in a mammalian mouse model. J Virol. 2005;79:12058–12064. doi: 10.1128/JVI.79.18.12058-12064.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mehle A, Doudna JA. Adaptive strategies of the influenza virus polymerase for replication in humans. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:21312–21316. doi: 10.1073/pnas.0911915106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yamada S, et al. Biological and structural characterization of a host-adapting amino acid in influenza virus. PLoS pathogens. 2010;6:e1001034. doi: 10.1371/journal.ppat.1001034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salzberg SL, et al. Genome analysis linking recent European and African influenza (H5N1) viruses. Emerging infectious diseases. 2007;13:713–718. doi: 10.3201/eid1305.070013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Treanor JJ, Campbell JD, Zangwill KM, Rowe T, Wolff M. Safety and immunogenicity of an inactivated subvirion influenza A (H5N1) vaccine. The New England journal of medicine. 2006;354:1343–1351. doi: 10.1056/NEJMoa055778. [DOI] [PubMed] [Google Scholar]
- 27.Neumann G, et al. Generation of influenza A viruses entirely from cloned cDNAs. Proceedings of the National Academy of Sciences of the United States of America. 1999;96:9345–9350. doi: 10.1073/pnas.96.16.9345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.WHO. Manual on animal influenza diagnosis and surveillance. 2002. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


