Abstract
Study objective
Improving identification and treatment for substance use disorders (SUDs) is a national priority, but data about various drug use disorders encountered in emergency departments (EDs) are lacking. We examined past-year substance use and SUDs (alcohol, 9 drug classes) among adult ED users. Prevalences of substance use and SUDs among ED non-users were calculated for reference purposes.
Methods
Using data from the 2007–2009 National Surveys on Drug Use and Health, we assessed SUDs among noninstitutionalized adults aged ≥18 years who responded to standardized survey questions administered by audio computer-assisted self-interviewing methods.
Results
Of all adults (N=113,672), 27.8% used the ED in the past year. ED users had higher prevalences than ED non-users of coexisting alcohol–drug use (15.2% vs. 12.1%), drug use (any drug, 16.9% vs. 13.0%; marijuana, 12.1% vs. 9.7%; opioids, 6.6% vs. 4.1%), and alcohol or drug disorders (11.0% vs. 8.5%). Among substance users, the ED group on average spent more days using drugs than the non-ED group; ED users manifested higher conditional rates of SUDs than ED non-users (alcohol or drugs, 15.9% vs. 11.7%; marijuana, 16.6% vs. 13.2%; cocaine, 33.2% vs. 22.3%; opioids, 20.6% vs. 10.0%; stimulants, 18.6% vs. 9.2%; sedatives, 35.0% vs. 4.4%; tranquilizers, 12.4% vs. 5.2%). Regardless of ED use status, substance-using young adults, men, and less-educated adults showed elevated odds of having a SUD.
Conclusion
Drug use is prevalent and combined with high rates of drug use disorders among drug users seen in the ED.
Keywords: alcohol use disorders, drug abuse, drug use disorders, prescription drug abuse, substance use disorder
INTRODUCTION
The National Drug Control Strategy and the Patient Protection and Affordable Care Act of 2010 emphasize early identification of individuals with a substance use disorder (SUD) and integration of SUD treatment with medical settings.1,2 Substance-related accidents often result in admissions to emergency departments (EDs).3,4 ED settings thus can provide “a window of opportunity” for screening to facilitate the integration of SUD treatment with mainstream medical care. According to the Drug Abuse Warning Network (DAWN), about 2.1 million ED visits in 2009 involved drug misuse or abuse (1,244,679 visits, prescription drugs; 973,591 visits, illicit drugs; 1,377,342 visits, alcohol and/or drugs).5 Substance-using ED patients are likely to constitute a severe subset, and their contact with medical providers may trigger recognition of a substance problem or motivation to change.6
Due to competing priorities in the ED, substance use—especially of illicit or nonmedical drugs—is not screened routinely; SUDs are reported to be underdetected or undertreated.3,7,8 A state-wide survey in Tennessee estimated that 27% of ED patients needed substance abuse treatment, but only 3.3% of those in need received treatment.8 Patients with unmet treatment needs have elevated odds for hospital admission during ED visits, thus generating higher costs than those receiving SUD treatment.9 While substance use is considered prevalent in the ED, no representative data exist that describe the extent of use or the disorders for various drugs among ED users. Furthermore, little is known about whether universal screening for all drugs is a reasonable approach and whether certain demographic groups should receive more attention than others. Because results of hospital cases of substance users do not consider the denominator (at-risk population), they provide inadequate information about the prevalences or burdens of substance use and SUDs for diverse drugs and demographic groups.5 To identify substance classes that warrant research to evaluate screening strategies, substance use prevalences in the population of ED users and comparative likelihood of having a SUD among users of the substance (conditional prevalence of a SUD) must be determined systematically to allow valid comparison across substances.10
To date, screening and intervention efforts have focused primarily on alcohol problems, despite the fact that illicit or nonmedical drugs are often combined with alcohol and involved in the majority of drug-related ED visits.11–13 Due to scarcity of data, the U.S. Preventive Services Task Force has not recommended routine screening for drug problems. To achieve the goal of increasing substance abuse treatment under health care reform (e.g., routine screening for substance use, early intervention) and respond to an epidemic of nonmedical prescription opioid use in the United States (to which significant increases in drug-related ED admissions may be attributed),14–17 systematic data on the extent of different SUDs and at-risk groups found in the ED are needed to inform research on screening of substance use and assessments of SUDs among substance users (the design of clinical trials to evaluate screening foci and resources).18,19
The lack of research on routine screening and intervention for drug-related problems to guide the development of screening guidelines partly relates to the fact that such research must consider 9 major illicit or prescription drug classes (marijuana, inhalants, cocaine, hallucinogens, heroin, prescription opioids, stimulants, sedatives, tranquilizers). These drug classes differ in availability and sources (licit, illicit), abuse liability, and user demographic characteristics.10,20 The prevalence and demographic correlates of drug use have yet to be comprehensively examined in a large representative sample to specify common illicit and nonmedical drugs of use in the ED population and to identify demographic groups of ED users disproportionally affected by drug-related disorders. Such information will be useful to ED clinicians for prioritization of screening foci and identification of at-risk substance users. To this end, complete population-based data about use of all available substances and SUDs in a national sample of ED users will need to be compared with ED non-users to establish the reported elevated rate of substance use in the ED. The diversity in substance classes also requires comparative analysis to consider different substance use status (at-risk population) for making valid comparisons when evaluating SUDs across substances for heterogeneous groups of users. This is accomplished by examining conditional rates of SUDs for all substances (probability of having a SUD given use of the substance) to identify subgroups showing elevated rates of SUDs.
Here, we examined adult data from the 2007–2009 National Surveys on Drug Use and Health (NSDUH) to elucidate variations in substance use and SUDs by ED use and evaluate 10 SUDs (alcohol and nine drugs) among substance users for age, sex, and race/ethnicity. We focused on adults as they presently are the primary population of interest for screening.11–13 NSDUH is the largest survey of SUDs in the United States; the selected years used designs permitting use of pooled data to examine all SUDs assessed by the same instrument by ED use status, and to compare conditional probabilities of SUDs among substance users. The pooled data also identify the extent of overlooked illicit and prescription drug disorders for understudied demographic groups (Asians, Native Americans, multiple-race adults, older adults).4
To guide the current practice of a staged approach to screening (an initial question about substance use status, followed by questions of substance-related problems) and elucidate the extent of assessments for substance problems for various drugs, we examined the frequency of substance use and conditional probabilities of SUDs to characterize use patterns and identify subsets of users showing elevated odds of having a SUD. Conditional rates of SUDs consider substance-specific variations in use and disorders by restricting the denominator for each SUD to users of the corresponding substance, thereby allowing comparisons across substances. We also examined comorbid alcohol–drug disorders to fill the gap left by studies that have focused exclusively on alcohol use.
Study aims were to: 1) determine whether past-year rates of substance use and SUDs among ED users were higher than rates among ED non-users to gauge substance use-related burdens; 2) among ED users, examine conditional rates of SUDs by age, sex, and race/ethnicity to specify substances warranting research on targeted assessments for SUDs; and 3) determine key demographic correlates of SUDs to elucidate health disparities, which have implications for facilitating identification of subsets of ED users with a SUD and informing health policy-making.
METHODS
Data Source
Data were from the public-use data file of the 2007–2009 NSDUH, the only survey designed to provide ongoing national estimates of substance use and SUDs in the United States.20,21 From 2007–2009, approximately 67,500 unique persons aged ≥12 years were interviewed annually (weighted interviewing response rates: 74–76%). Three years of data from adults aged ≥18 years (n=37,708 38,067/year) were pooled to allow for the detection of differences in SUDs by age or race/ethnicity (N=113,672). The use of data for this research was approved by the Duke University Institutional Review Board.
Sample
The survey covers residents of households from the 50 states and the District of Columbia (persons living in houses, apartments, condominiums, or non-institutional group quarters, such as shelters, rooming houses, group homes; civilians residing on military bases).22 Participants are selected by multistage area probability methods to ensure that each independent cross-sectional sample is representative of persons aged ≥12 years. The design oversampled people aged 12–25 years; because of a large sample size, there was no need to oversample racial/ethnic groups as was done prior to 1999.
Data Collection
Prospective respondents are assured that their names will not be recorded and their responses will be kept strictly confidential. All study procedures and protections are carefully explained. Demographic questions are administered by interviewers using computer-assisted personal interviewing. Other questions of a sensitive nature (substance use, SUDs, treatment use) are administered with audio computer-assisted self-interviewing, which provides respondents with a highly confidential means of responding to questions to increase honest reporting of sensitive behaviors.20,21 Respondents read questions on the computer screen, or questions are read to them through headphones, and they enter responses directly into a computer provided by the interviewer. Each respondent who completed the interview was given a $30 payment to compensate for his/her time and effort.
Study Variables
Respondents’ age, sex, race/ethnicity, education, total family income, marital status, and population density of residence were examined. Population density of residence—a proxy for community location and a potential confounder for influencing the rate of substance use by ED—was included as a control variable.4
ED use was defined as having 1 or more hospital emergency department visits in the previous 12 months. ED use (“During the past 12 months, that is, since [DATEFILL], how many different times have you been treated in an emergency room for any reason?”). Research shows that self-reported ED use data are generally accurate; however, because underreporting of the number of ED visits may occur, the analysis focused on a dichotomized ED status.23,24 Exploratory analyses were conducted to determine whether more frequent ED users (≥3 times) had higher prevalences of substance use and SUDs than infrequent ED users (1–2 times).
The survey asked each respondent about his/her use of alcohol and 9 drug classes (illicit use of marijuana/hashish, cocaine/crack, heroin, or hallucinogens; inhalant use; nonmedical use of prescription analgesic opioids, stimulants, tranquilizers, sedatives). Nonmedical use was defined as use without a prescription or for the experience or feeling the drug caused; use of over-the-counter drugs and legitimate use of prescription drugs were not included.20,25 Alcohol and drug classes were assessed by discrete questions in 10 different sections. Each included a detailed description of the substance class and a list of substances belonging to the class. For nonmedical use, respondents were provided with pill cards showing color pictures of tablets for analgesic opioids, tranquilizers, stimulants, and sedatives. To determine the extent of co-usage of alcohol and drugs, users of both alcohol and a drug were categorized. Past-year substance use variables were examined as they are better indicators of recent or active use than lifetime measures and are the focus of screening.26
Respondents who reported alcohol or drug use in the past year were asked a set of structured, substance-specific questions designed to operationalize Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV criteria for past-year SUDs (abuse or dependence) (eTable 1 available online).20,27,28 Dependence on a given substance class included users who met ≥3 dependence criteria for that class in the past year; abuse applied to users who met ≥1 abuse criterion but did not meet criteria for dependence on that substance class.
Lifetime substance abuse treatment use was defined as any use of treatment services specifically related to alcohol or drug use in the prior year (“Have you ever you received treatment or counseling for your use of alcohol or any drug, not counting cigarettes?”). History of injection drug use (IDU) was ascertained by assessing whether respondents had ever injected heroin, cocaine, methamphetamine, or any other drug that was not prescribed for the respondents or that the respondents took solely for the experience or feeling it caused. Both were included as control variables.
Data Quality
NSDUH uses audio computer-assisted self-interviewing to increase privacy and the accuracy of self-reports and includes detailed probes and color pictures of prescription drugs to augment assessments for substance use; these practices have improved the quality of data.29,30 A reliability study showed substantial (for abuse/dependence questions) to nearly perfect (for alcohol and marijuana use questions) response agreement for NSDUH measures.29 Validity data revealed high agreement (marijuana, 89.8%; cocaine, 95.5%) between self-reported use and urine drug test results.31 NSDUH also incorporates consistency checks, statistical computation, and analysis weights to minimize response inconsistency and adjust for nonresponse bias.20,32 A prior follow-up study of survey nonrespondents showed no significant nonresponse bias.33
Data Analysis
The distributions of study variables by ED use were determined by χ2. Prevalences of past-year substance use and SUDs in the total sample were compared by ED use to determine whether ED users had higher prevalences of substance use and SUDs than ED non-users. Prevalences of SUDs among past-year users of the corresponding substance then were calculated to evaluate conditional rates of SUDs. To inform identification of substance users and research on screening, we report conditional rates of SUDs among ED users by age group, sex, and race/ethnicity, respectively. Logistic regression analyses were conducted among alcohol users to estimate associations between sociodemographic variables (age, sex, race/ethnicity, educational level, marital status, family income, and population density of residence) and alcohol use disorders; similar analyses were conducted among drug users for drug use disorders. History of substance abuse treatment, IDU, and survey year were adjusted in these analyses to mitigate for their confounding effects on associations. Data were analyzed by SUDAAN—the software designed for analyzing data from a complex national survey like NSDUH.34 All results are weighted figures except for sample sizes (unweighted).
RESULTS
Overall, 27.8% of adults used EDs for a medical reason in the past year. Table 1 presents demographics, substance abuse treatment, and injection drug use variables by ED status. All variables differed significantly by ED status (P< 0.001).
Table 1.
Characteristics of adults aged 18 years or older by ED status: 2007–2009 (N=113,672)
| Characteristics % (SE) | ED users | ED non-users |
|---|---|---|
|
| ||
| Sample size | N=35,604 | N=78,068 |
| Age in years | ||
| 18–25 | 17.4 (0.24) | 13.7 (0.17) |
| 26–34 | 16.2 (0.31) | 15.8 (0.20) |
| 35–49 | 26.2 (0.54) | 29.7 (0.24) |
| 50–64 | 22.1 (0.49) | 25.0 (0.36) |
| 65+ | 18.1 (0.60) | 15.9 (0.35) |
|
| ||
| Sex | ||
| Male | 44.6 (0.53) | 49.7 (0.30) |
| Female | 55.4 (0.53) | 50.3 (0.30) |
|
| ||
| Race/ethnicity1 | ||
| White, non-Hispanic | 66.4 (0.45) | 69.7 (0.35) |
| Black, non-Hispanic | 15.5 (0.38) | 10.0 (0.22) |
| Native American/Alaska Native | 0.5 (0.06) | 0.4 (0.04) |
| Asian/Pacific Islander | 3.0 (0.23) | 5.3 (0.18) |
| Multiple race | 1.3 (0.08) | 1.0 (0.05) |
| Hispanic | 13.3 (0.32) | 13.6 (0.27) |
|
| ||
| Education | ||
| < High school | 20.3 (0.34) | 13.8 (0.26) |
| High school | 33.5 (0.48) | 30.1 (0.33) |
| College+ | 46.2 (0.45) | 56.2 (0.33) |
|
| ||
| Family income | ||
| < $40,000 | 48.5 (0.45) | 35.8 (0.34) |
| $40,000 – $74,999 | 27.3 (0.39) | 29.8 (0.27) |
| $75,000+ | 24.2 (0.44) | 34.4 (0.38) |
|
| ||
| Marital status | ||
| Married | 48.8 (0.53) | 57.4 (0.33) |
| Separate/divorced/widowed | 22.8 (0.47) | 17.5 (0.25) |
| Single | 28.4 (0.37) | 25.1 (0.25) |
|
| ||
| Population density2 | ||
| Large metropolitan | 49.9 (0.55) | 52.5 (0.48) |
| Small metropolitan | 43.2 (0.62) | 41.5 (0.47) |
| Non-metropolitan | 7.0 (0.29) | 6.1 (0.24) |
|
| ||
| History of substance abuse treatment | ||
| Yes | 8.0 (0.24) | 5.6 (0.13) |
| No | 92.0 (0.24) | 94.4 (0.13) |
|
| ||
| History of injection drug use | ||
| Yes | 2.4 (0.12) | 1.5 (0.07) |
| No | 97.6 (0.12) | 98.5 (0.07) |
SE: standard error.
Mutually exclusive groups.
Population density was based on 2000 census data and the June 2003 Core-based Statistical Area (CBSA) classifications, and was categorized as large-metro (≥1 million population), small-metro (<1 million population), and non-metro (not in a CBSA).
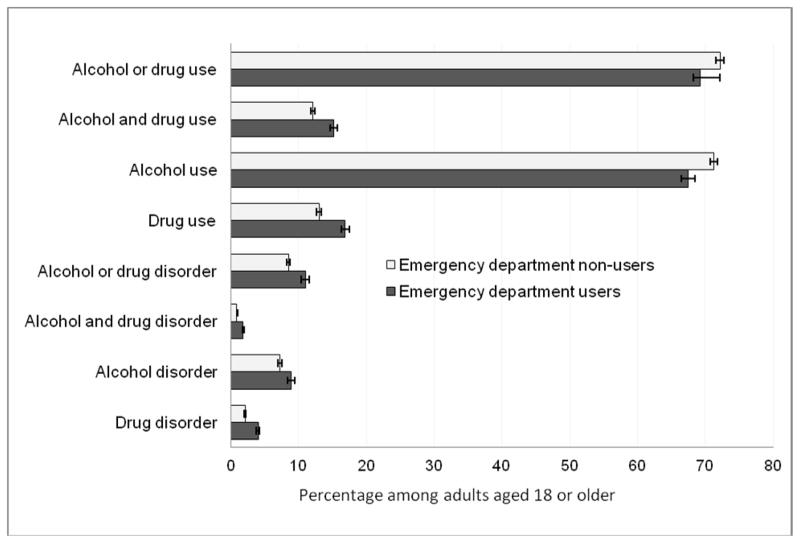
Fig. 1 shows that ED users had higher prevalences than ED non-users of coexisting alcohol–drug use, drug use, and SUDs (eTable 2).
Fig 1.
One-year prevalence of substance use and disorders (abuse or dependence) among adults aged 18 years or older by emergency department use (N=113,672). Lines extending from bars indicate 95% confidence intervals of the estimates.
Adjusted logistic regression analyses (controlling for the variables in the first column of Table 1) showed that ED users had higher odds than ED non-users in use of alcohol–drugs (adjusted odds ratio, AOR 1.19; 95% CI 1.13–1.25), any drug (AOR 1.23; 95% CI 1.16–1.29), marijuana (AOR 1.14; 95% CI 1.03–1.21), inhalants (AOR 1.41; 95% CI 1.10–1.80), cocaine (AOR 1.28; 95% CI 1.16–1.42), hallucinogens (AOR 1.21; 95% CI 1.09–1.36), opioids (AOR 1.48; 95% CI 1.37–1.59), stimulants (AOR 1.14; 95% CI 1.01–1.29), sedatives (AOR 1.85; 95% CI 1.36–2.52), and tranquilizers (AOR 1.32; 95% CI 1.20–1.49). Frequent ED users had higher prevalences than infrequent ED users in use of most substances and almost all SUDs (eTable 3).
Fig. 2 shows that ED users had higher conditional rates of SUDs than ED non-users in most substances (except for inhalants, hallucinogens, and heroin).
Fig 2.
One-year conditional prevalence of substance use disorders (abuse or dependence) among adults aged 18 years or older who used the corresponding substance by emergency department use status (N=86,682). Lines extending from bars indicate 95% confidence intervals of the estimates.
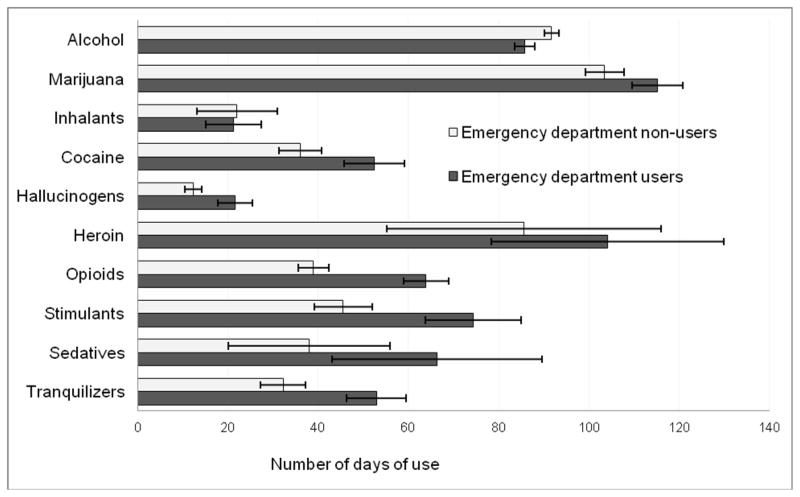
Fig. 3 indicates that substance-using ED users on average spent a greater number of days using most drugs (except for inhalants, heroin, and sedatives) than substance-using ED non-users, but ED non-users had more days of alcohol use than ED users.
Fig 3.
Average number of days of substance use among past-year adult users of the corresponding substance by emergency department use (N=86,682). Lines extending from bars indicate 95% confidence intervals of the estimates.
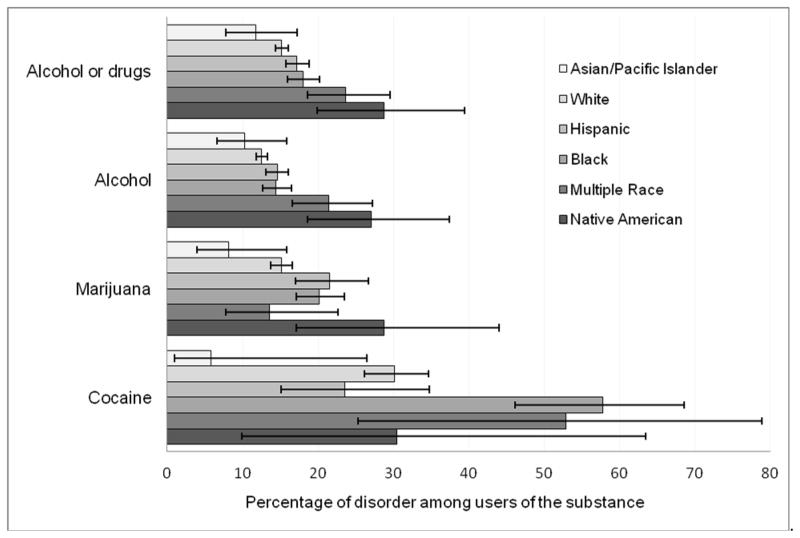
Conditional SUDs among ED users who used alcohol or drugs in the past year (n=86,682) by key demographics are summarized in eTables 4–6. There were age-related decreases in conditional rates of any SUD. Male substance users had higher conditional rates than female substance users of any SUD, alcohol–drug, alcohol, any drug, and marijuana disorders. Fig. 4 presents racial/ethnic differences in conditional rates of SUDs. Native Americans and multiple-race adults exhibited higher conditional rates of any SUD than whites and Asians/Pacific Islanders.
Fig 4.
One-year conditional prevalence of substance use disorders (abuse or dependence) among emergency department patients aged 18 years or older by race/ethnicity group (N=86,682). Lines extending from bars indicate 95% confidence intervals of the estimates.
Finally, adjusted logistic regression analyses of conditional rates of SUDs showed that, regardless of ED status, younger age, being male, having less education, being single, and history of substance abuse treatment or IDU increased odds of having a SUD (Table 2). A similar finding was found after each model also was controlled for past-year frequency of alcohol use (for alcohol disorders) and of marijuana use (for drug disorders) (eTable 7).
Table 2.
Adjusted odds ratio (AOR) of the conditional prevalence of past-year substance use disorder in past-year substance users among ED patients aged 18 years or older
| Adjusted logistic regression model1 | AOR (95% CI) of alcohol use disorder1 (N=85,008) | AOR (95% CI) of drug use disorder1 (N=26,585) | ||
|---|---|---|---|---|
|
| ||||
| ED status | ED users | ED non-users | ED users | ED non-users |
| Age (vs. 18–25 years) | ||||
| 26–34 | 0.76 (0.63–0.91) | 0.69 (0.61–0.78) | 0.81 (0.65–1.00) | 0.86 (0.72–1.03) |
| 35–49 | 0.53 (0.46–0.62) | 0.50 (0.44–0.57) | 0.65 (0.49–0.85) | 0.65 (0.52–0.79) |
| 50–64 | 0.35 (0.27–0.47) | 0.35 (0.31–0.40) | 0.44 (0.26–0.76) | 0.38 (0.25–0.57) |
| 65+ | 0.12 (0.07–0.19) | 0.16 (0.11–0.24) | 0.70 (0.21–2.28) | 0.85 (0.40–1.84) |
|
| ||||
| Sex (vs. female) | ||||
| Male | 1.99 (1.78–2.22) | 1.98 (1.82–2.16) | 1.38 (1.17–1.63) | 1.38 (1.17–1.63) |
|
| ||||
| Race/ethnicity (vs. white) | ||||
| Black | 0.95 (0.80–1.13) | 0.79 (0.66–0.96) | 1.13 (0.88–1.44) | 1.03 (0.80–1.32) |
| Native American | 1.56 (0.95–2.56) | 1.20 (0.81–1.78) | 0.91 (0.48–1.72) | 0.68 (0.32–1.45) |
| Asian/Pacific Islander | 0.80 (0.48–1.33) | 0.55 (0.43–0.71) | 0.61 (0.30–1.21) | 1.20 (0.66–2.19) |
| Multiple race | 1.47 (1.06–2.03) | 0.85 (0.61–1.19) | 1.03 (0.55–1.93) | 0.97 (0.56–1.66) |
| Hispanic | 0.97 (0.83–1.12) | 0.96 (0.86–1.08) | 1.04 (0.79–1.36) | 1.17 (0.96–1.42) |
|
| ||||
| Education (vs. ≥ college) | ||||
| < High school | 1.24 (1.07–1.44) | 1.17 (1.01–1.37) | 1.44 (1.19–1.74) | 2.02 (1.68–2.44) |
| High school | 1.06 (0.92–1.22) | 0.98 (0.89–1.08) | 1.40 (1.18–1.65) | 1.41 (1.62–1.62) |
|
| ||||
| Family income (vs. $75,000+) | ||||
| < $40,000 | 1.07 (0.89–1.28) | 1.04 (0.92–1.18) | 1.31 (1.02–1.68) | 1.12 (0.94–1.35) |
| $40,000 – 74,999 | 1.02 (0.87–1.19) | 0.95 (0.85–1.06) | 1.23 (0.96–1.58) | 1.23 (0.94–1.61) |
|
| ||||
| Marital status (vs. married) | ||||
| Separate/divorced/wid. | 1.68 (1.33–2.12) | 1.51 (1.28–1.78) | 1.32 (0.96–1.82) | 1.33 (0.97–1.82) |
| Single | 1.91 (1.64–2.22) | 1.69 (1.50–1.90) | 1.52 (1.18–1.95) | 1.56 (1.28–1.92) |
|
| ||||
| Population density (vs. large metropolitan) | ||||
| Small metropolitan | 1.06 (0.93–1.21) | 1.01 (0.92–1.11) | 0.91 (0.78–1.07) | 0.96 (0.81–1.13) |
| Non-metropolitan | 1.11 (0.84–1.48) | 0.80 (0.66–0.97) | 0.86 (0.66–1.14) | 0.79 (0.56–1.13) |
|
| ||||
| History of substance abuse treatment (vs. no) | ||||
| Yes | 4.65 (4.01–5.39) | 4.56 (3.99–5.20) | 3.24 (2.65–3.96) | 2.78 (2.28–3.38) |
| History of injection drug use (vs. no) | ||||
| Yes | 1.50 (1.13–2.01) | 1.40 (1.01–1.91) | 2.44 (1.80–3.29) | 1.89 (1.38–2.59) |
|
| ||||
| Survey year (vs. 2007) | ||||
| 2008 | 1.12 (0.96–1.30) | 0.94 (0.86–1.04) | 1.19 (0.96–1.49) | 0.96 (0.81–1.14) |
| 2009 | 1.06 (0.92–1.22) | 0.95 (0.86–1.06) | 1.04 (0.84–1.29) | 0.93 (0.78–1.10) |
ED: emergency department. CI: confidence interval.
Each separate model included all independent variables listed in the first column; results were adjusted for the complex survey design of the data (weighting, clustering, and stratification) and model covariates.
Limitations
The data source relies on self-reports, which can be influenced by memory error and under-reporting. Like other surveys, NSDUH uses standardized questions designed to operationalize DSM-IV criteria for SUDs; SUDs are self-reported estimates, not clinical diagnoses. Of note, the NSDUH-based prevalence of SUDs among adults in 2000 (6.7%) resembled the prevalence of SUDs (7.4%) among adults in the National Longitudinal Alcohol Epidemiologic Survey.28 Additionally, SUD estimates in the ED are expected to be greater than our findings have suggested because nicotine dependence was not based on DSM-IV criteria and not included. NSDUH also does not distinguish between drug-related vs. non–drug-related ED visits, and findings do not apply to institutionalized or homeless adults (about 2%) who were not included in the survey. Nonetheless, research shows that the inclusion of institutionalized and homeless individuals in large-scale surveys does not change substantially the overall population estimates of drug dependence because of the very small sample size of these individuals relative to that of the noninstitutionalized population.35
DISCUSSION
This study presents the most recent and comprehensive national estimates of past-year substance use and SUDs among adults who used EDs in the past year; findings have implications for screening, intervention efforts, and designs of clinical trials to evaluate the effectiveness of such efforts. First, ED users had higher prevalences than ED non-users of past-year drug use (12.1% vs. 9.7%), alcohol–drug use (15.2% vs. 12.1%), and alcohol (8.9% vs. 7.3%) and drug (4.0% vs. 2.1%) disorders. Second, among substance users, ED users had higher conditional rates than ED non-users of alcohol (13.1 % vs. 10.3%) or drug (23.5% vs. 16.0%) disorders, including marijuana (16.6%), cocaine (33.2%), opioid (20.6%), stimulant (18.6%), sedative (35.0%), and tranquilizer (12.4%) disorders. Third, regardless of ED status, substance users who were male, single, younger than 35 years, or less educated demonstrated elevated rates of SUD.
What This Study Adds to Our Knowledge
Research has shown that alcohol or drug use increases ED use, but community-based rates of illicit/nonmedical drug use and disorders in the population of ED users are lacking.36,37 DAWN estimates are based on retrospective reviews of medical records of ED visits, focus on drugs identified as the primary causes for ED visits, exclude ED visits involving alcohol only for patients aged 21+ years, and do not address conditional probabilities or the size of the population at risk for experiencing substance problems.5,38 Thus, they are inadequate in elucidating comparative probabilities of substance use or demographic profiles to aid in prioritizing substances and population subgroups for screening and better management. Additionally, DAWN’s hospital participation rates in non-metropolitan areas have been low (20–30%) and may have identified severe subsets of substance users whose substance use resulted in emergent medical visits; for instance, 73% of drug-related ED visits for substance abuse treatment involved multiple drugs.39 Thus, these data are incomplete for delineating profiles of less-problematic substance users to inform identification efforts.
Using the NSDUH’s national probability sample, our results suggest that at least two-thirds (68%) of adults aged 18+ years in the ED used alcohol; 1 in 6 (17%) were recent or active illicit/nonmedical drug users (mainly marijuana, prescription opioids), and 90% of drug users also used alcohol in the past year. This high rate of past-year drug use supports the need for research to explore the feasibility of routine screening of drug use in the ED with a focus on marijuana and opioids, as well as additional assessments of alcohol problems among drug users. Of note, marijuana and prescription opioids were the most prevalent drug disorders in this national sample of ED users; however, DAWN data showed that cocaine and heroin were the most commonly reported drugs among adults.38,39 The discrepancy might relate to the severe nature of DAWN cases identified from ED visits or assessment bias (illicit use or injection of cocaine or heroin are more salient to medical staff than use of marijuana or prescription drugs). These results, nonetheless, support increasing concerns about nonmedical marijuana and opioid use and their associated morbidity or mortality.16,40,41
Additionally, substance abuse is considered common in the ED due to substance-related injuries. Using a broad definition for substance problems (lifetime SUD/current use, past treatment/current substance use, wanting treating, current substance use, current dependence), Rockett et al.8 estimated that 27% of ED users in a sample from a statewide survey needed substance abuse treatment. Our findings demonstrate that about 1 in 10 (11%) adults aged 18+ years in the ED have had a self-reported alcohol (9%) or drug (4%) disorder in the past year. Comparison of our estimates with others is complicated, however, by differences in study samples and criteria for defining substance problems. If our results had included subthreshold substance users (individuals who met some DSM-IV dependence criteria but had no disorder),42,43 the estimate would increase substantially and be closer to that of Rockett et al.8
Another clinically relevant finding concerns our inclusive survey-based estimates of conditional SUDs to inform clinical strategies for targeted screening. Close to 1 in 4 (24%) past-year drug users in the ED sample had a drug disorder compared with 1 in 8 (13%) of past-year alcohol users with an alcohol disorder. Drugs with notable conditional rates of disorders include heroin (66%), sedatives (35%), cocaine (33%), prescription opioids (21%), stimulants (19%), and marijuana (17%). The low use rate of several drugs in the total sample and the high conditional rate of drug disorders suggest that universal screening for drug disorders may not be efficient. The feasibility of a staged approach, however, should be studied to identify strategies that can improve detection of adults with a drug disorder and facilitate integration of SUD treatment with medical care.17,26
In conclusion, 28% of adults nationally used ED treatment in the past year. ED users include higher proportions of socioeconomically disadvantaged groups (young, female, black, less-educated adults) than ED non-users. Among substance users, the ED group used drugs more frequently and had higher conditional rates of SUDs than the non-ED group. The ED setting thus provides a window of opportunity for improving detection for substance use problems and linking SUD care with other medical services.44 Taking into account the number of affected adults and available resources, marijuana and prescription opioids should be the primary focus for screening efforts.
Acknowledgments
Funding support: This work was supported primarily by research grants from the U.S. National Institute on Drug Abuse of the National Institutes of Health (R21DA027503, R33DA027503, R01DA019623, R01DA019901; PI, Li-Tzy Wu) and in part by HSN271200522071C (PI, Dan G. Blazer). The National Institutes of Health had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
The Substance Abuse and Mental Health Data Archive provided the public-use data files for the National Survey on Drug Use and Health, which was sponsored by the Center for Behavioral Health Statistics and Quality of the Substance Abuse and Mental Health Services Administration. We thank Amanda McMillan, MPH, MA, for her editorial assistance.
Footnotes
Disclosures: M. Swartz has served as a consultant to Novartis Pharmaceuticals and has received research support from Eli Lilly and Co. P. Mannelli has received support from AstraZeneca, Bristol-Myers Squibb, Cephalon Inc., Forest, GlaxoSmithKline, Janssen, Jazz Pharmaceuticals, King Pharmaceutical, Lundbeck, McNeil Consumer and Specialty, Merck, Organon, Orphan Medical, Pfizer, Reckitt Benckiser, and Titan. The other authors have no conflicts of interest to disclose.
Contributors: LT Wu conceived the study and drafted the manuscript. LT Wu and DG Blazer obtained research funding. LT Wu and C Yang conducted the data analysis and are responsible for statistical analysis. All authors contributed to interpretation of the findings and critical revision to result in the final manuscript. LT Wu takes responsibility for the paper as a whole.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Office of National Drug Control Policy. National Drug Control Strategy 2011. Washington, DC: Office of National Drug Control Policy, Executive Office of the President; 2011. [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration. What you need to know about health reform? Substance Abuse and Mental Health Services Administration News. 2010 Sep-Oct;18(5) [Google Scholar]
- 3.D’Onofrio G, Becker B, Woolard RH. The impact of alcohol, tobacco, and other drug use and abuse in the emergency department. Emerg Med Clin North Am. 2006;24:925–967. doi: 10.1016/j.emc.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 4.Vitale S, van de Mheen D. Illicit drug use and injuries: a review of emergency room studies. Drug Alcohol Depend. 2006;82:1–9. doi: 10.1016/j.drugalcdep.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 5.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The DAWN Report: Highlights of the 2009 Drug Abuse Warning Network (DAWN) Findings on Drug-Related Emergency Department Visits. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; 2010. [Google Scholar]
- 6.Bogenschutz MP, Donovan DM, Adinoff B, et al. Design of NIDA CTN Protocol 0047: screening, motivational assessment, referral, and treatment in emergency departments (SMARTED) Am J Drug Alcohol Abuse. 2011;37:417–425. doi: 10.3109/00952990.2011.596971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D’Onofrio G, Degutis LC. Preventive care in the emergency department: screening and brief intervention for alcohol problems in the emergency department: a systematic review. Acad Emerg Med. 2002;9:627–638. doi: 10.1111/j.1553-2712.2002.tb02304.x. [DOI] [PubMed] [Google Scholar]
- 8.Rockett IR, Putnam SL, Jia H, et al. Assessing substance abuse treatment need: a statewide hospital emergency department study. Ann Emerg Med. 2003;41:802–813. doi: 10.1067/mem.2003.189. [DOI] [PubMed] [Google Scholar]
- 9.Rockett IR, Putnam SL, Jia H, et al. Unmet substance abuse treatment need, health services utilization, and cost: a population-based emergency department study. Ann Emerg Med. 2005;45:118–127. doi: 10.1016/j.annemergmed.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 10.Wu LT, Woody GE, Yang C, Pan JJ, Blazer DG. Racial/ethnic variations in substance-related disorders among adolescents in the United States. Arch Gen Psychiatry. 2011;68:1176–1185. doi: 10.1001/archgenpsychiatry.2011.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American College of Emergency Physicians. [Accessed September 1, 2011];Alcohol screening and brief intervention in the ED. Available at: http:/www.acep.org/content.aspx?id=34358.
- 12.Higgins-Biddle J, Hungerford D, Cates-Wessel K. Screening and Brief Interventions (SBI) for Unhealthy Alcohol Use: A Step-By-Step Implementation Guide for Trauma Centers. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2009. [Google Scholar]
- 13.U S. Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: recommendation statement. Ann Intern Med. 2004;140:554–556. doi: 10.7326/0003-4819-140-7-200404060-00016. [DOI] [PubMed] [Google Scholar]
- 14.Cai R, Crane E, Poneleit K, et al. Emergency department visits involving nonmedical use of selected prescription drugs in the United States, 2004–2008. J Pain Palliat Care Pharmacother. 2010;24:293–297. doi: 10.3109/15360288.2010.503730. [DOI] [PubMed] [Google Scholar]
- 15.Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006;15:618–627. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Emergency department visits involving nonmedical use of selected prescription drugs—United States, 2004–2008. MMWR Morb Mortal Wkly Rep. 2010;59:705–709. [PubMed] [Google Scholar]
- 17.Ghitza UE, Sparenborg S, Tai B. Improving drug abuse treatment delivery through adoption of harmonized electronic health record systems. Subst Abuse Rehabil. 2011;2:125–131. doi: 10.2147/SAR.S23030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bernstein E, Bernstein J, Levenson S. Project ASSERT: an ED-based intervention to increase access to primary care, preventive services, and the substance abuse treatment system. Ann Emerg Med. 1997;30:181–189. doi: 10.1016/s0196-0644(97)70140-9. [DOI] [PubMed] [Google Scholar]
- 19.D’Onofrio G, Degutis LC. Integrating Project ASSERT: a screening, intervention, and referral to treatment program for unhealthy alcohol and drug use into an urban emergency department. Acad Emerg Med. 2010;17:903–911. doi: 10.1111/j.1553-2712.2010.00824.x. [DOI] [PubMed] [Google Scholar]
- 20.Substance Abuse and Mental Health Services Administration. Summary of National Findings NSDUH Series H-38A, HHS Publication No SMA 10-4586. I. Rockville, MD: Office of Applied Studies; 2010. Results from the 2009 National Survey on Drug Use and Health. [Google Scholar]
- 21.Substance Abuse and Mental Health Services Administration, Office of Applied Studies. NSDUH Series H-36, DHHS Publication No SMA 09-4434. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2009. Results from the 2008 National Survey on Drug Use and Health: National Findings. [Google Scholar]
- 22.Morton KB, Martin PC, Chromy JR, Hirsch EL, Ridenhour JL. 2010 National Survey on Drug Use and Health: Methodological Resource Book. Research Triangle Park, NC: RTI International; 2011. Sample design report. [Google Scholar]
- 23.Dendukuri N, McCusker J, Bellavance F, et al. Comparing the validity of different sources of information on emergency department visits: a latent class analysis. Med Care. 2005;43:266–275. doi: 10.1097/00005650-200503000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Lubeck DP, Hubert HB. Self-report was a viable method for obtaining health care utilization data in community-dwelling seniors. J Clin Epidemiol. 2005;58:286–290. doi: 10.1016/j.jclinepi.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 25.Wu LT, Ringwalt CL, Mannelli P, et al. Prescription pain reliever abuse and dependence among adolescents: a nationally representative study. J Am Acad Child Adolesc Psychiatry. 2008;47:1020–1029. doi: 10.1097/CHI.0b013e31817eed4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Institutes of Health and The Society for Behavioral Medicine. [Accessed December 2, 2011];Identifying Core Behavioral and Psychosocial Data Elements for the Electronic Health Record: Executive Summary. Available from: http://ebookbrowse.com/ehr-meeting-may-executive-summary-pdf-d146218496.
- 27.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. text revision. [Google Scholar]
- 28.Epstein JF. DHHS Publication No SMA 02-3642, Analytic Series A-16. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2002. Substance Dependence, Abuse, and Treatment: Findings from the 2000 National Household Survey on Drug Abuse. [Google Scholar]
- 29.Chromy JR, Feder M, Gfroerer J, et al. DHHS Publication No SMA 09-4425, Methodology Series M-8. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2009. Reliability of Key Measures in the National Survey on Drug Use and Health. [PubMed] [Google Scholar]
- 30.Gfroerer J, Eyerman J, Chromy J, editors. DHHS Publication No SMA 03–3768. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2002. Redesigning an Ongoing National Household Survey: Methodological Issues. [Google Scholar]
- 31.Harrison LD, Martin SS, Enev T, et al. DHHS Publication No SMA 07-4249, Methodology Series M-7, RTI/0209009186002. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2007. Comparing Drug Testing and Self-report of Drug Use among Youths and Young Adults in the General Population. [Google Scholar]
- 32.Substance Abuse and Mental Health Services Administration. NSDUH Series H-41, HHS Publication No (SMA) 11-4658. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2011. Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. [Google Scholar]
- 33.Caspar R. Follow-up of nonrespondents in 1990. In: Turner CF, Lessler JT, Gfroerer JC, editors. Survey Measurement of Drug Use: Methodological Studies. DHHS Publication No. ADM 92-1929. Rockville, MD: National Institute on Drug Abuse; 1992. [Google Scholar]
- 34.Research Triangle Institute. SUDAAN User’s Manual, Release 9.0. Research Triangle Park, NC: Research Triangle Institute; 2006. [Google Scholar]
- 35.Anthony JC, Helzer JE. Syndromes of drug abuse and dependence. In: Robins LN, Regier DA, editors. Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York: The Free Press; 1991. pp. 116–154. [Google Scholar]
- 36.Balsa AI, French MT, Maclean JC, et al. From pubs to scrubs: alcohol misuse and health care use. Health Serv Res. 2009;44(5 Pt 1):1480–1503. doi: 10.1111/j.1475-6773.2009.00987.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McGeary KA, French MT. Illicit drug use and emergency room utilization. Health Serv Res. 2000;35(1 Pt 1):153–169. [PMC free article] [PubMed] [Google Scholar]
- 38.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. HHS Publication No SMA 11-4618. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; 2011. Drug Abuse Warning Network, 2008: National Estimates of Drug-related Emergency Department Visits. [Google Scholar]
- 39.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The DAWN Report: Emergency Department Visits Involving Patients Seeking Detoxification or Substance Abuse Treatment Services. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; 2011. [Google Scholar]
- 40.Kuepper R, van Os J, Lieb R, et al. Continued cannabis use and risk of incidence and persistence of psychotic symptoms: 10-year follow-up cohort study. BMJ. 2011;342:d738. doi: 10.1136/bmj.d738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McGrath J, Welham J, Scott J, et al. Association between cannabis use and psychosis-related outcomes using sibling pair analysis in a cohort of young adults. Arch Gen Psychiatry. 2010;67:440–447. doi: 10.1001/archgenpsychiatry.2010.6. [DOI] [PubMed] [Google Scholar]
- 42.Blazer DG, Wu LT. The epidemiology of alcohol use disorders and subthreshold dependence in a middle-aged and elderly community sample. Am J Geriatr Psychiatry. 2011;19:685–694. doi: 10.1097/JGP.0b013e3182006a96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wu LT, Ringwalt CL, Mannelli P, et al. Hallucinogen use disorders among adult users of MDMA and other hallucinogens. Am J Addict. 2008;17:354–363. doi: 10.1080/10550490802269064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Academic ED SBIRT Research Collaborative. The impact of screening, brief intervention and referral for treatment in emergency department patients’ alcohol use: a 3-, 6- and 12-month follow-up. Alcohol Alcohol. 2010;45:514–519. doi: 10.1093/alcalc/agq058. [DOI] [PMC free article] [PubMed] [Google Scholar]