Abstract
AIM
To study the success and outcome of trabeculectomy in Hospital Melaka.
METHODS
Medical records of all patients who underwent trabeculectomy between January 1, 2007 and October 31, 2010 whom were followed up for at least 6 months postoperatively in Hospital Melaka were retrospectively reviewed.
RESULTS
A total number of 117 eyes of 91 patients with the age range between 12 to 84 years underwent primary trabeculectomy (n=20, 17.1%), combine trabeculectomy with cataract surgery (n=90, 76.9%), repeat trabeculectomy (n=5, 4.3%), and combine repeat trabeculectomy with cataract surgery (n=2, 1.7%). The disease spectrum includes primary open-angle glaucoma (POAG) (54 patients, 59.3%), priamry angle-closure glaucoma (PACG) (14 patients, 15.4%), secondary glaucomas (19 patients, 20.9%) and juvenile glaucomas (4 patients, 4.4%). Preoperative mean intraocular pressure (IOP) was (24.69±8.67)mmHg as compared to postoperative mean IOP of (15.81±6.66)mmHg, (15.07±4.72)mmHg and (15.68 ±3.65)mmHg at 6-month, 12-month and 24-month respectively. Eighty-two point one percent of eyes (n=96) achieved complete success (CS), 12.8% (n=15) with qualified success (QS) and only 5.1% (n=6) failed at 6 month with two of them warrant other filtering surgery. At twelve months, trabeculectomy with CS was 71.6% (n=63), QS in 22.7% (n=20) and failure in 5.7% (n=5). Sixty-seven point five percent (n=27) attained CS, 20.0% (n=8) with QS while 12.5% (n=5) failed at 24 month postoperative.
CONCLUSION
As the understanding of the lower the IOP, the better the patients retaining the visual function, trabeculectomy is significantly a choice of treatment in uncontrolled glaucoma. This study concluded that trabeculectomy performed in Hospital Melaka has produced significant success as compared to other studies.
Keywords: trabeculectomy, glaucoma, success rate
INTRODUCTION
Glaucoma is one of the leading causes of irreversible blindness worldwide. It is estimated that the number of people affected approximating 79.6 million worldwide by 2020, and Asian accounts for almost half of them; with 10% of them develop bilateral blindness[1],[2].
It is defined as a progressive optic neuropathy with characteristics of optic disc changes with corresponding visual field defects, with or without raised intraocular pressure (IOP). Nevertheless, currently, IOP is the only modifiable risk factors as demonstrated in studies reporting reduced visual field progression when IOP has been lowered. Therefore, the management of glaucoma is often emphasized on optimal IOP reduction in order to prevent or delay the disease progression[2],[3].
Lowering of IOP in this group of patients could be achieved with medical, laser or surgical treatment. Trabeculectomy is always labelled as the “gold standard” of surgical management of uncontrolled glaucoma since its first introduction by Cairns about 4 decades ago. With the advance of surgical instruments, modification of surgical techniques and adjunctive use of anti-metabolites, trabeculectomy has been producing high success rate with low complications incidence. Nevertheless, the final outcome of this surgical therapy is variable in different age group, different types of glaucoma and different ethnicity[3].
This study is to analyze the outcome of fornix-based trabeculectomy adjunctive with mitomycin C (MMC) in Hospital Melaka.
MATERIALS AND METHODS
Subjects
This is a retrospective study reviewing records of all glaucoma patients who underwent trabeculectomy between July 1, 2007 and October 31, 2010 at Hospital Melaka. Patients who had a postoperative follow up period less than 6 months were excluded.
All the patients were diagnosed to have glaucoma based on the clinical evidence of glaucomatous optic disc changes, gonioscopic grading, associated raised in IOP (greater than 21mmHg) and glaucomatous visual filed defects. The main indications for trabeculectomy were uncontrolled IOP with maximal medical therapy, or progression in visual field loss with corresponding optic disc damages.
Methods
All trabeculectomies were performed by experienced surgeons mainly under local anesthesia. Fornix-based conjunctival flap approach was used in all cases, followed by the creation of partial triangular or rectangular thickness scleral flap (scleral flap thickness created was individualized). A number of small cellulose sponges, soaked with antimetabolites, MMC 0.04mg/mL, were applied beneath the tenon capsule and scleral flap for 3 minutes. At the end of the 3 minutes, the sponges were removed and the area was cleaned with copious of normal saline.
If the patient was for phacoemulsification, the anterior chamber was entered at the base of the scleral flap after a paracenthesis. After completion of cataract extraction with intraocular lens implantation, the sclerostomy was performed with a Kelly Descemet punch followed by peripheral iridectomy.
The scleral flap was then sutured with 10/0 nylon sutures and one to two of these sutures were anchored to the cornea as releasable sutures. The suture tension was adjusted to allow adequate flow of aqueous and at the same time maintain anterior chamber depth. The flow of the aqueous via scleral flap was checked with cellulose sponge. Superficial scrapping over the superior cornea near limbus was performed to assist adhesion of conjunctiva. The fornix-based conjunctival flap was then anchored to the limbus with nylon 10/0 sutures.
Postoperatively, all the systemic and topical anti-glaucomas were withheld and the patients were started on a combination of topical antibiotic and steroid eyedrop, which was tailed down over a period of 3 to 4 months. Other additional procedures were instituted as needed depending on the postoperative condition.
All the patients were examined at day 1, day 4, day 7, week 2 and then monthly depending on the patient's recovery response or any additional post-operative procedure such as released of sutures and needling. For each post-operative session, visual acuity, full eye examination, IOP, bleb condition and post-operative complications such as wound leak, hyphema, hypotony, choroidal detachment and endophthalmitis were looked into.
The data collected for this study include: name, age, race, gender, diagnosis, nature of operation and anesthesia, preoperative and postoperative IOP, preoperative and postoperative number of antiglaucoma medications, postoperative complications and additional postoperative procedures.
The outcomes of the surgeries were graded as: (1) Complete success (CS): IOP below 21mmHg without medication; (2) Qualified success (QS): IOP below 21mmHg with medication; (3) Complete failure (CF): IOP at or above 21mmHg despite maximum medications.
RESULTS
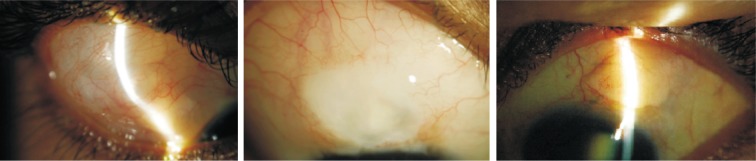
From the review of the records, it was noted that 65 patients had trabeculectomies in one eye while the remaining 26 patients had bilateral surgery. Sixty-five (55.6%) right eyes and 52 (44.4%) left eyes were operated during the studied period(Figure 1).
Figure 1. Successful trabeculectomy with functioning bleb.
Table 1 illustrates the demography of the patients. The mean age at operation was 64 years (range of age: 12-84years). Trabeculectomies were performed for 54 male patients (59.3%) and 37 female patients (40.7%). The patients were constituted by 40 Malays (44.0%), 38 Chinese (41.8%) and 11 Indian (12.1%). The disease spectrum includes primary open angle glaucoma (POAG) (54 patients, 59.3%), primary angle-closure glaucoma (PACG) (14 patients, 15.4%), secondary glaucomas (19 patients, 20.9%) and juvenile glaucomas (4 patients, 4.4%).
Table 1. Patient characteristics.
| POAG (n=74) | PACG (n=18) | Secondary glaucoma (n=21) | Juvenile glaucoma (n=4) | |
| Age(a) | ||||
| Mean (SD) | 64.49 (10.538) | 62.06 (10.435) | 65.00 (9.834) | 24.00 (10.231) |
| Median(range) | 64.00 (33-81) | 61 (49-83) | 68 (47-84) | 25.5 (12-33) |
| Gender | ||||
| Male | 44 (59.5%) | 4 (22.2%) | 14 (66.7%) | 4 (100%) |
| Female | 30 (40.5%) | 14 (77.8%) | 7 (33.3%) | |
| Race | ||||
| Malay | 28 (37.8%) | 8 (44.4%) | 13 (61.9%) | 4 (100%) |
| Chinese | 35 (47.3%) | 8 (44.4%) | 3 (14.3%) | - |
| Indian | 9 (12.2%) | 2 (11.1%) | 5 (23.8%) | - |
| Others | 2 (2.7%) | - | - | - |
Surgeries performed were primary trabeculectomy (n=20, 17.1%), repeat trabeculectomy (n=5, 4.3%), combine procedure of primary trabeculectomy with cataract extraction and intraocular lens implantation (n=90, 76.9%) and combine procedure of repeat trabeculectomy with cataract surgery and intraocular lens implantation (n=2, 1.7%).
Majority of eyes with POAG (n=55, 74.3%) underwent primary trabeculectomy combine with cataract extraction and intraocular lens implantation, 17.6% (n=13) had primary trabeculectomy, 5.4% (n=4) had repeat trabeculectomy, while the remaining 2.7% (n=2) had repeat trabeculectomy combine with phacoemulsification and intraocular lens implantation (PEA/IOL).
For PACG eyes (n=18), all surgeries performed were combine procedures, in which 94.4% (n=17) were combined with PEA/IOL and only one eye was combined with conventional extracapsular cataract extraction with IOL implantation (ECCE/IOL).
Fifteen eyes with secondary glaucoma (71.4%) underwent trabeculectomy combine with PEA/IOL, 3 eyes (14.3%) had primary trabeculectomy, 2 eyes (9.5%) had trabeculectomy combine with ECCE/IOL and only 1 eye (4.5%) had repeat trabeculectomy. Primary trabeculectomy was performed in all cases of juvenile glaucoma.
Majority of the surgeries were performed under local anesthesia (n=110, 94.0%), with a much smaller number (n=7, 6.0%) were performed under general anesthesia for very young patients.
Preoperatively, the mean IOP for all groups of patients was (24.69±8.67)mmHg as compared to postoperative mean IOP of (15.81±6.66)mmHg, (15.07±4.72)mmHg and (15.68±3.65)mmHg at 6-month, 12-month and 24-month respectively. For POAG group, the mean preoperative IOP dropped from (22.61±6.31)mmHg to (15.66±5.82)mmHg, (15.07±4.21)mmHg and (15.96±3.41)mmHg postoperatively at 6-month, 12-month and 24-month respectively. Mean preoperative IOP for PACG was (31.00±12.26)mmHg as compared to mean postoperative IOP of (16.44±4.61)mmHg, (14.75±4.22)mmHg and 16.78±3.93mmHg at 6-month, 12-month and 24-month respectively. For secondary glaucoma, the mean preoperative IOP dropped from (26.00±10.03)mmHg to mean postoperative IOP of (17.10±10.18)mmHg, (15.73±6.91)mmHg and (11.50±2.52)mmHg at month-6, month-12 and month-24 respectively. Four eyes of juvenile glaucoma showed drop of mean preoperative IOP from (28.00±6.73)mmHg to (9.00±2.0)mmHg, (12.00±2.83)mmHg and (16±0)mmHg at postoperative month-6, month-12 and month-24 respectively.
Eighty-two point one percent of the cases (n=96) achieved complete success (CS), 12.8% (n=15) with qualified success (QS) and only 5.1% (n=6) failed at 6 month with two of them warrant Ahmed valve filtering surgery. At twelve month, trabeculectomy with CS was 71.6% (n=63), QS was 22.7% (n=20) and failure was 5.7% (n=5). Sixty-seven point five percent (n=27) attained CS, 20.0% (n=8) with QS while 12.5% (n=5) failed at 24 month postoperatively. For each different group of glaucoma, the success rate is between 66.7% and 100% as shown in Table 2.
Table 2. Type of surgery, mean change in IOP and success outcome of different types of glaucoma.
| POAG | PACG | Secondary glaucoma | Juvenile glaucoma | |
| Surgical procedures | n=74 | n=18 | n=21 | n=4 |
| Primary trabeculectomy | 13(17.6%) | - | 3(14.3%) | 4(100%) |
| Primary trabeculectomy combine with cataract surgery | 55(74.3%) | 18(100%) | 17(80.9%) | - |
| Repeat trabeculectomy | 4(5.4%) | - | 1(4.5%) | - |
| Repeat trabeculectomy combine with cataract surgery | 2(2.7%) | - | - | - |
| Preoperative mean IOP (SD), mmHg | 22.61(6.307) | 31.00(12.257) | 26.00(10.025) | 28.00(6.733) |
| Postoperative mean IOP (SD), mmHg | ||||
| 6 months | 15.66(5.820) | 16.44(4.605) | 17.10(10.183) | 9.00(2.000) |
| 12 months | 15.07(4.213) | 14.75(4.224) | 15.73(6.912) | 12.00(2.828) |
| 24 months | 15.96(3.407) | 16.78(3.930) | 11.50(2.517) | 16.00(0) |
| Postoperative 6 months | ||||
| Complete success | 85.1% (n=63) | 72.2% (n=13) | 76.2% (n=16) | 100% (n=4) |
| Qualified success | 12.2% (n=9) | 22.2% (n=4) | 9.5% (n=2) | - |
| Complete failure | 2.7% (n=2) | 5.6% (n=1) | 14.3% (n=3) | - |
| Postoperative 12 months | ||||
| Complete success | 77.6% (n=45) | 75.0% (n=9) | 43.8% (n=7) | 100% (n=2) |
| Qualified success | 20.7% (n=12) | 16.7% (n=2) | 37.5% (n=6) | - |
| Complete failure | 1.7% (n=1) | 8.3% (n=1) | 18.7% (n=3) | - |
| Postoperative 24 months | ||||
| Complete success | 72.0% (n=18) | 55.6% (n=5) | 60.0% (n=3) | 100% (n=1) |
| Qualified success | 24.0% (n=6) | 11.1% (n=1) | 20.0% (n=1) | - |
| Complete failure | 4.0% (n=1) | 33.3% (n=3) | 20.0% (n=1) | - |
Table 3 showed the summary of the postoperative complications. Sixty-eight point four percent of the surgeries (n=80) had no complications. The commonest complication observed was wound leak in 11.1% (n=13) in which majority resolved with conservative management and the remaining require secondary suturing. Only 7.7% (n=9) developed postoperative hyphema which resolve spontaneously. Nine eyes (7.6%) developed postoperative hypotony secondary to overfiltration, with 7 of the eyes complicated with choroidal detachment. Three eyes (2.6%) developed severe uveitis in which all of them were from secondary glaucoma group. Cataract progression was only observed in three eyes, which was much lower compared to other studies because majority of the surgeries performed in the studied eyes were combine procedure.
Table 3. Postoperative complications.
| Complications | Frequency(%) |
| None | 80 (68.4) |
| Wound leak | 13 (11.1) |
| Hyphema | 9 (7.7) |
| Choroidal detachment | 7 (6.0) |
| Cataract progression | 3 (2.6) |
| Severe uveitis | 3 (2.6) |
| Hypotony | 2 (1.6) |
DISCUSSION
Glaucoma, a serious sight-threatening condition, is defined as progressive loss of retinal ganglion cells and their axons, and this process is believed to be slowed down by lowering the IOP at all stages of the disease. Hence, early treatment offers a potential benefit in all newly diagnosed glaucoma patients which eventually reduces the possibility of loss of functional vision[4].
Multiple large studies which had demonstrated the effects of lowering IOP in reducing disease progression, has guided the ophthalmologist to focus on IOP reduction in glaucoma management[3],[5]. Some even reported that for each millimeter of mercury of IOP reduction, the risk of progression decreased by approximately 10 percent[6].
With the advent of powerful medical treatment, IOP has dramatically decreased to the targeted level in the hope to prevent or delay the glaucoma progression and eventually the blindness. Surgical treatment such as trabeculectomy is only indicated when the target IOP is not achievable medically, when there is evidence of disease progression, or if the patient is unable to comply or tolerate the medical treatment[7].
Since its first introduction by Cairns in 1967, partial thickness trabeculectomy started to become a popular surgical option for glaucoma patients and until now it remains as the standard procedure for glaucoma patients with uncontrolled IOP[3],[8]. The refinement of surgical technique and adjunctive usage of antimetabolites such as 5-Fluorouracil (5-FU) and mitomycin C (MMC) further imporves the success rate and survival of trabeculectomy over the past decade; and it is believed that trabeculectomy has not only out-performed the medical treatment in lowering the magnitude of the IOP, but also the diurnal fluctuation of IOP[8]-[13].
Studies comparing limbal-based and fornix-based trabeculectomy found that there are no significant differences in the outcome of the surgeries[14]. On the other hand, limbus-based trabeculectomy appears to be more likely to develop bleb complications such as cystic bleb formation, hypotony and ocular infection[15].
In this retrospective study, all trabeculectomies were approached with fornix-based conjunctival flap and intraoperative adjunctive MMC was used. Fornix-based approach was commenced because it require less manipulation, easier to perform, better intraoperative wound exposure, and produce broader and more diffuse conjunctival flap. In addition, postoperative bleb manipulation such as ocular massage, removal of releasable suture and suturelysis has further enhanced the outcome of the surgery.
Majority of the surgeries performed was combine trabeculectomy with cataract surgery as most patients are above the age of 50 years and with significant cataract.
Majority of the patients in this study benefited from the surgery, with 94.8% (111 eyes) achieved success at postoperative 6 months, which subsequently reduced to 84.3% (83 eyes) at 12 months and 87.5% (35 eyes) at 24 months. Of these, only 12.8%-22.7% of them required additional topical medications. Of all, the mean IOP and the mean number of glaucoma medications were significantly reduced in the latest visit. The overall mean IOP decreased from preoperative (24.69±8.67)mmHg to postoperative (15.81±6.66)mmHg, (15.07±4.72)mmHg and (15.68 ±3.65)mmHg at 6-month, 12-month and 24-month respectively (P<0.01∼0.03).
We also found that the success rate in older age group in higher than the younger age group. However, the difference was not statistically significant. Whilst in comparing the success outcome in different disease spectrum, the POAG group has significantly higher success rate compared to secondary glaucoma and PACG, particularly at 24 months after the surgery.
In our study, the overall rate of postoperative complications was low and comparable with others[8],[15],[16]. Only 37 eyes (31.6%) developed some form of early postoperative complications. The most common complication was wound leak in 13 eyes (11.1%), in which 5 eyes required conjunctival resuturing and the remainder successfully treated conservatively with eye padding.
Over the past decade, in the search for a safer surgical procedures for glaucoma, many new surgical options such as non-penetrating filtering procedures (deep sclerotomy, viscocanalostomy, Ex-PRESS filtration device, Trabectome, etc.) were introduced and reported promising results. These procedures appear to have more advantages in terms of preserving conjunctiva and lesser postoperative complications. However, trabeculectomy still remains as the standard sugical care as these new procedures are limited by factors like higher cost, longer learning curve and the uncertain long term results.
In conclusion, the ideal strategy in managing glaucoma is to detect the disease as early as possible, to use as less the medication as possible to maintain optimal low and diurnally stable IOP and to reduce the risk of adverse effects of medication or surgery. In view of the great challenge in early detection and diagnosing glaucoma, early surgical intervention may be another option in delaying the rate of visual loss in this group of patients.
The modern trabeculectomy is a highly successful surgery with a relatively predictable outcome and very low risk of complication. In good hands, it could achieve low IOP from day 1, without medication, and maintained for years. Moreover, the failed trabeculectomy could be re-operated at different site with intact conjunctiva and also able to achieve a comparable outcome.
Despite the limitations in this retrospective study (no objective evaluation of the conjunctival bleb, patients between groups are not comparable, and 10-20% of patients defaulted the follow up), the information could still be extrapolated to managing patients at all stages of glaucoma.
Besides aiming for a targeted IOP in the hope of staving off disease progresaion long enough to preserve their sight throughout the remainder of their life, successful trabeculectomy also provide better quality of life, as many glaucoma patients may suffered from the side effects and high cost of multiple eyedrops.
REFERENCES
- 1.Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–267. doi: 10.1136/bjo.2005.081224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hussain R, Clarke JCK, Seah SKL, Khaw PT. A review of trabeculectomy in East Asian people-the influence of race. Eye. 2005;19:243–252. doi: 10.1038/sj.eye.6701477. [DOI] [PubMed] [Google Scholar]
- 3.Mahar PS, Laghari DA. Intraocular pressure Control and Post Operative Complications with Mitomycin C Augmented Trabeculectomy in Primary Open Angle and Primary Angle-Closure Glaucoma. Pak J Ophthalmol. 2011;27(1):35–39. [Google Scholar]
- 4.Kuldev S, Shrivastava A. Early Aggressive Intraocular Pressure Lowering, Target Intraocular Pressure, and a Novel Concept of Glaucoma Care. Surv Ophthalmol. 2008;53:33–38. doi: 10.1016/j.survophthal.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Ophthalmology, Glaucoma Panel . San Francisco: American Academy of Ophthalmology; 2000. Primary open-angle glaucoma. Preferred practice pattern; pp. 1–36. [Google Scholar]
- 6.Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L, Komaroff E. Factors for glaucoma progression and the effect of treatment: the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2003;121:48–56. doi: 10.1001/archopht.121.1.48. [DOI] [PubMed] [Google Scholar]
- 7.Keenan TDL, Salmon JF, Yeates D, Goldacre MJ. Trends in rates of trabeculectomy in England. Eye. 2009;23:1141–1149. doi: 10.1038/eye.2008.195. [DOI] [PubMed] [Google Scholar]
- 8.David R, Sachs U. Quantitative trabeculectomy. Br J Ophthalmol. 1981;65:457–459. doi: 10.1136/bjo.65.7.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stead RE, King AJ. Outcome of trabeculectomy with mitomycin C in patients with advanced glaucoma. Br J Ophthalmol. 2011;95:960–965. doi: 10.1136/bjo.2010.185272. [DOI] [PubMed] [Google Scholar]
- 10.Ramahrishnan R, Khurana M. Surgical management of glaucoma: An Indian perspective. Indian J Ophthalmol. 2011;59(Suppl. 1):118–122. doi: 10.4103/0301-4738.73697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lim LA, Chindasub P, Kitnarong N. The surgical outcome of Primary Trabeculectomy with Mitomycin C and A Fornix-based Conjunctival Flap Technique in Thailand. J Med Assoc Thai. 2008;91(10):1551–1557. [PubMed] [Google Scholar]
- 12.Jay JL, Murray SB. Early trabeculectomy versus conventional management in primary open angle glaucoma. Br J Ophthalmol. 1988;72:881–889. doi: 10.1136/bjo.72.12.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee PP, Walt JW, Rosenblatt LC, Siegartel LR, Stern LS, Glaucoma Care Study Group Am J Ophthalmol. 2007;144:901–907. doi: 10.1016/j.ajo.2007.07.040. [DOI] [PubMed] [Google Scholar]
- 14.Shingleton BJ, Chaudhry IM, O'Domghue MW, Baylus SL, King RJ, Chaudhry MB. Phacotrabeculectomy: limbus-based versus fornix-based conjunctival flap in fellow eyes. Ophthalmology. 1999;106:1152–1155. doi: 10.1016/S0161-6420(99)90252-X. [DOI] [PubMed] [Google Scholar]
- 15.Kohl DA, Cordeiro MF, Bunce C, Khaw PT. Cystic bleb formation and related complications in limbus-versus fornix-based conjunctival flap in pediatric and young adult trabeculectomy with mitomycin C. Ophthalmology. 2003;110:2192–2197. doi: 10.1016/S0161-6420(03)00800-5. [DOI] [PubMed] [Google Scholar]
- 16.Ng PW, Yeung BY, Yick DW, Yu CB, Lam DS. Fornix-based trabeculectomy with Wise's suture technique in Chinese patients. Ophthalmology. 2000;107:2310–2313. doi: 10.1016/s0161-6420(00)00460-7. [DOI] [PubMed] [Google Scholar]