Abstract
Background
This study examined the association between social, demographic, and psychologic factors and smoking status among Appalachian Ohio women. A secondary aim examined whether specific factors could be identified and segmented for future tailored treatment of tobacco dependence.
Methods
A cross-sectional survey (n=570) obtained information about social, demographic, and psychologic factors and smoking. Logistic regression described associations between these characteristics and smoking status. Chi-square automatic interaction detection (CHAID) analyses identified subgroups at risk for smoking.
Results
Fifty-two percent never smoked, with 20.5% and 27.5% categorized as former and current smokers, respectively. Women with low adult socioeconomic position (SEP) were more likely to smoke (odds ratio [OR] 3.05, 95% confidence interval [CI] 1.74-5.34) compared to high SEP women. Other factors associated with current smoking included age 31–50 (OR 2.30, 95% CI 1.22-4.33), age 18–30 (OR 3.29, 95% CI 1.72-5.34), Center for Epidemiologic Studies Depression scale (CES-D) score≥16 (OR 1.99, 95% CI 1.31-3.05), and first pregnancy at age<20 (OR 1.74, 95% CI 1.14-2.66). The prevalence of smoking was 50% among those with four or more risk factors compared to 10% for those reporting no risk factors. CHAID analyses identified low adult SEP and depressive symptoms as the combination of risk factors most strongly associated with smoking; 49.3% of women in this subgroup currently smoked.
Conclusions
Low SEP in adulthood, maternal circumstances, and depressive symptoms are associated with current smoking. Tailored cessation interventions that address these risk factors should be developed and further evaluated in an attempt to reduce disparities in smoking prevalence among this vulnerable group of women.
Introduction
The incidence of disability and disease caused by smoking is well documented.1,2 Among women, 178,000 die every year because of a smoking-attributable disease, with chronic lung disease, lung cancer, and heart disease representing the top three causes.3 It has also been established that social inequalities are partially responsible for specific behaviors and disease conditions.4 With regard to a smoking behavior, socioeconomic disadvantage in childhood increases progression to regular smoking among youth, and poverty is related to persistent smoking as an adult.5 Currently, 18% of adult American women are smokers, and there is compelling evidence to support a positive relationship between disadvantage and smoking.6 U.S. women living below the poverty level are more likely to smoke (26.9%) compared to their advantaged counterparts (17.6%).7 In concert with this disparity, less education and lower employment are related to decreased success in quitting smoking, especially among women.8 Among young women who are mothers, smoking in the home has the potential to expose children to second-hand smoke. It has been estimated that 26.4% of children in poor families live with at least one person who smoked in the home compared to 15.5% among children living in more advantaged families.9 Protecting children from passive smoke exposure while maintaining a smoking behavior may be a challenge in circumstances that involve child care responsibilities, for example, single motherhood. As scholars have noted,6,10 the disproportionate prevalence in smoking among poorer women, with subsequent disparity in rates of morbidity and mortality, quitting success, and exposure to second-hand smoke, represents a critical topic of investigation in the field of women's health.
It is well established that social factors, including less education, lower income, and blue collar occupations, are directly related to smoking.11 However, less is known about specific life experiences and circumstances that may be associated with lower socioeconomic status (SES) and smoking, especially among women. It has been noted by Shi et al.12 that vulnerable groups may experience clusters of factors that operate simultaneously or cumulatively and increase the likelihood of poorer health outcomes. These authors12 and other investigators13 have also suggested that risk profiles should be constructed to better understand how clusters of specific factors influence certain individuals. For example, it has been separately reported that the odds of smoking are high among women who became mothers at an early age10,14 and that persistent smoking is linked with depression,15 which also correlates with economic disadvantage.16–18 Thus, social and maternal factors, as well as psychologic characteristics, together as a cluster of factors, may partially explain the maintenance of a smoking behavior. The timing and trajectory of these experiences and circumstances, such as disadvantage, as well as being a single woman often in the context of early parenthood, deserve further examination as risk factors for smoking. Characterizing the combination of individual factors may assist in the identification and treatment of risky behaviors, such as cigarette smoking.
The Social Determinants of Health model4 emphasizes SES, life experiences and circumstances, and psychologic variables (e.g., depression) as factors related to behaviors (i.e., smoking) that subsequently influence morbidity and mortality. Incidence and mortality rates from heart disease and cancer, and especially tobacco-attributable cancers, are higher in the Appalachian region of the United States.19,20 Rural and Appalachian women experience more poverty and have less education and a higher proportion of unskilled workers compared to other groups.21 Women in Appalachia earn less money than men; in addition, changing life circumstances (e.g., job loss, divorce) put Appalachian women at higher risk for poverty compared to men.22 Appalachian women demonstrate a higher prevalence of tobacco consumption compared to the American population in general.23,24 There is information about smoking behavior, quitting patterns, and overall lifestyle behaviors in urban and rural Appalachian women,25–32 but less is known about smoking behavior and its association with SES during vulnerable periods of childhood, motherhood, and psychologic states, such as depression. Understanding these factors may assist in shaping tobacco control efforts that subsequently reduce health disparities and improve health outcomes among this vulnerable population. This article uses data collected from women enrolled in a National Cancer Institute (NCI)-funded Appalachian Center for Population Health and Health Disparities cervical health study to answer the question: What is the association between social, demographic, and psychologic factors and smoking status among Appalachian Ohio women? A secondary aim examined whether specific factors, or profiles, could be identified, segmented, and combined for future tailored treatment of tobacco dependence.
Materials and Methods
This study was part of a larger NCI-funded cervical health project entitled, Community Awareness, Resources and Education (CARE) (P50 CA105632), and has been described elsewhere.33 Briefly, Ohio Appalachian-designated counties (n=29)21 were selected using probability proportional to size sampling, with county cervical cancer incident cases in 1998–200034 as the size measure. After county selection, all primary care and obstetrics/gynecology clinics listed in county telephone books or named by key informants were identified (n=171). Clinics were contacted to determine if cervical screenings were performed (n=160). Clinics reporting≥200 unique cervical screenings annually (n=22) were invited to participate; a total of 14 clinics, or 63.6%, agreed.
Following clinic agreement, a random sample was selected from a complete list of female patients. First, medical records were reviewed to determine eligibility, which included (1) documented clinic visit within 2 years, (2) age 18+, (3) nonpregnant, (4) no history of invasive cervical cancer or hysterectomy, and (5) Ohio Appalachian county resident. Second, potentially eligible women were contacted (by mail and phone) and invited to participate in a baseline interview. Next, if a woman was determined as eligible and agreed to participate, a baseline survey was scheduled and conducted in private, usually at the participant's home. All respondents were paid $25 as reimbursement for their time and participation. The study was approved by the Institutional Review Boards at The Ohio State University, the University of Michigan, and the Centers for Disease Control and Prevention (CDC).
The baseline survey was verbally administered by a trained research staff interviewer. The interview averaged about 1 hour in length. All survey questions were presented visually on a laptop screen and simultaneously read to the participant by the interviewer. Responses were entered by the interviewer via a Computer Assisted Personal Interview (CAPI) system. Specific variables for this analysis included the following.
Social and demographic characteristics
Variables included age (18–30, 31–50, and≥51 years), education (<high school, high school/General Educational Development (GED), and>high school), race (white vs. other), marital status at time of interview (never married, married/member of couple, and divorced/widowed/separated), employment (full-time, part-time, unemployed/disabled, other), occupation (professional as defined by a degree, skilled labor, unskilled labor, other), annual household income, and health insurance (private, government-assisted, none).
Life course socioeconomic position (SEP)
Previous approaches to childhood and adult SES were used to create variables that categorized the individual's SEP as high or low during childhood and at present.5,35–39 A woman's childhood SEP was defined as high if (1) she lived with both parents at age 14 years, and (2) both parents had≥high school education. Otherwise, her childhood SEP was defined as low. A woman's adult SEP was defined as high if she had (1)>high school education, (2) private insurance, and (3) a poverty income ratio (PIR) above the sample's median cutoff point. PIR was defined as the ratio of midpoint of observed family income category to official poverty threshold of a family of the same size for the same calendar year.40 If the participant did not report these three characteristics, her adult SEP was defined as low.
Age at first pregnancy
Women who were pregnant for the first time when<20 were grouped together, and women who reported never being pregnant or reported a first pregnancy when≥20 comprised the second group.14
Single mother status
Single mothers included only those women who reported children aged≤18 living in the household and no current husband, partner, or other adult household resident. All other women were coded as not being a single mother.14
Psychologic characteristic
Depressive symptoms
Depressive symptomatology was measured by the Center for Epidemiologic Studies Depression scale (CES-D).41 The CES-D is a 20-item self-report instrument used with the general population and asks the respondent to rate the frequency of feelings and behaviors experienced in the past week related to depressive symptoms. Scores range from 0 to 60, with a higher score indicating the presence of more depressive symptoms. CES-D scores≥16 are considered the cutoff point for further investigation of a depressive condition.
Smoking status
Smoking status was based on questions from the National Health Interview Survey (NHIS).42 First, participants were asked if they had ever smoked 100 cigarettes in their entire life. Those who responded no were categorized as never smokers. Those who answered yes were then asked if they smoke now. Those who answered yes were subsequently asked whether they smoked everyday or most days. Former smokers were categorized as those who had smoked 100 cigarettes in their entire life but did not smoke now. Current smokers were classified as those who answered that they had smoked 100 cigarettes in their lifetime and smoked now (everyday or most days).
Statistical analyses
Participants were categorized according to smoking status (i.e., never, former, current), and descriptive statistics were calculated for each independent variable. Analyses were conducted to determine the association between smoking status and social, demographic, and psychologic characteristics after combining information obtained from never smokers and former smokers to create a nonsmoker category. To answer the main research question of the study, a multivariable logistic regression model was fit with the binary outcome of smoking status (1=current smokers; 0=former and never smokers). This analysis allowed for examination of the independent effect of each variable. Because participant-level data were clustered within 14 Appalachian clinics, the model was fit using a mixed model approach (GLIMMIX procedure in SAS, version 9.13). Variables that were significant in univariate analyses were considered in the multivariable model. Backward elimination was performed to select factors significantly associated with smoking status. Interactions between life course SEP and other variables in the final model were examined. The model fit was examined using the Hosmer-Lemeshow test43; the area under the receiver operating characteristic (ROC) curve was assessed.
To address the secondary aim of the analysis, that is, whether specific factors or profiles could be identified and segmented for tailored treatment of tobacco dependence, a chi-squared automatic interaction detection (CHAID) method was used.44 The CHAID approach involved the construction of a decision tree that splits the sample into progressively smaller subsets based on which factor is most strongly related to the outcome at each split. This method was used to identify the combination of factors or profiles (i.e., child SEP, adult SEP, age at first pregnancy, single mother status, and depressive symptoms) that were most strongly associated with the dependent variable, which in this case was smoking status.
Results
A total of 2903 women were determined to be potentially eligible and invited (via mail or phone) to be screened; 801 women were able to be contacted and determined to be fully eligible. Of these, 570 completed the interview, yielding a cooperation rate of 71%.45
Sample characteristics
The sample included never smokers (52.1%), former smokers (20.5%), and current smokers (27.4%). Social, demographic, and psychologic characteristics are presented in Table 1, according to smoking status. The sample (n=570) was relatively young, with approximately three fourths being aged≤50. The majority had greater than a high school education (55.9%) and were white (94.7%). Most were married or partnered, and about 65% worked outside the home either full-time or part-time. One third of women had an annual household income of $20,000; 57.5% were classified as low child SEP and 67.5% as low adult SEP. Approximately 38% reported their first pregnancy occurring before age 20, and 9% were now classified as single mothers. Almost 31% of the sample scored≥16 on the CES-D instrument (Cronbach α for sample=0.74).
Table 1.
Percentage Distributions of Sample Characteristics for 570 Community Awareness, Resources and Education Participants Who Completed the Baseline Survey
| Characteristic | Never smokers (n=297) | Former smokers (n=117) | Current smokers (n=156) | Total (n=570) |
|---|---|---|---|---|
| Demographics and income | ||||
| Age | ||||
| 18–30 | 26.9 | 28.2 | 45.5 | 32.3 |
| 31–50 | 48.2 | 42.7 | 44.2 | 46.0 |
| ≥ 51 | 24.9 | 29.1 | 10.3 | 21.7 |
| Education | ||||
| Less than high school | 4.0 | 12.0 | 12.8 | 8.1 |
| High school diploma or GED | 28.6 | 42.7 | 44.9 | 36.0 |
| > High school diploma | 67.4 | 45.3 | 42.3 | 55.9 |
| Race | ||||
| White | 95.6 | 95.7 | 92.3 | 94.7 |
| Other | 4.4 | 4.3 | 7.7 | 5.3 |
| Marital status (n=569) | ||||
| Never married | 13.5 | 22.2 | 21.8 | 17.6 |
| Married/member of couple | 67.2 | 53.0 | 55.8 | 61.1 |
| Divorced/widowed/separated | 19.3 | 24.8 | 22.4 | 21.3 |
| No other smokers in household (n=565) | 79.6 | 76.5 | 41.7 | 68.5 |
| Employment (n=569) | ||||
| Works full-time or part-time | 68.7 | 57.8 | 62.2 | 64.7 |
| Unemployed/disabled | 10.4 | 14.6 | 19.2 | 13.7 |
| Other | 20.9 | 27.6 | 18.6 | 21.6 |
| Occupation (n=568) | ||||
| Professional (has a degree) | 33.8 | 19.8 | 11.5 | 24.8 |
| Skilled labor | 24.6 | 28.5 | 25.0 | 25.5 |
| Unskilled labor | 31.1 | 34.5 | 49.4 | 36.8 |
| Other | 10.5 | 17.2 | 14.1 | 12.9 |
| Insurance type (n=566) | ||||
| Private (job or purchased) | 73.7 | 62.3 | 39.1 | 61.9 |
| Medicaid/Medicare | 15.2 | 25.4 | 36.5 | 23.1 |
| No coverage | 11.1 | 12.3 | 24.4 | 15.0 |
| Poverty income ratio (n=542) | ||||
| High (advantaged) | 59.4 | 48.2 | 35.8 | 50.4 |
| Low (disadvantaged0 | 40.6 | 51.8 | 64.2 | 49.6 |
| Household income (n=542) | ||||
| < $20,000 | 26.0 | 40.0 | 45.0 | 34.1 |
| $20,000–$50,000 | 41.3 | 30.9 | 39.8 | 38.8 |
| > 50,000 | 32.7 | 29.1 | 15.2 | 27.1 |
| Life course socioeconomic position (SEP) (n=542) | ||||
| Low childhood SEP | 48.8 | 64.7 | 68.6 | 57.5 |
| Low adult SEP | 54.5 | 73.6 | 87.4 | 67.5 |
| Depressive symptoms | ||||
| CES-D score≥16 (n=569) | 24.2 | 23.3 | 48.7 | 30.8 |
| Maternal factors | ||||
| Pregnancy before age 20 years (n=567) | 29.0 | 40.0 | 52.3 | 37.6 |
| Currently a single mother (n=564) | 6.1 | 12.9 | 11.9 | 9.0 |
CES-D, Center for Epidemiologic Studies Depression Scale; GED, General Educational Development.
Logistic regression analyses
A univariate logistic regression model was first fit with each covariate, and significance was assessed (Table 2). The final adjusted main effects model (Table 3) contained the variables adult SEP, CES-D, age at first pregnancy, and age. The model had good fit and discrimination (Hosmer-Lemeshow Goodness of Fit test chi-square statistic=4.95, p=0.67, area under ROC curve=0.75). There were no significant two-way interactions at the α=0.05 level of significance.
Table 2.
Univariate Odds Ratios and 95% Confidence Intervals from Logistic Regression Model
| Characteristic | OR (95% CI) of being a current smoker | p value |
|---|---|---|
| Demographics and income | ||
| Age | <0.0001 | |
| 18–30 | 1.0 | |
| 31–50 | 0.58 (0.38-0.88) | |
| ≥ 51 | 0.23 (0.13-0.44) | |
| Education | 0.001 | |
| Less than high school | 1.0 | |
| High school diploma or GED | 0.38 (0.20-0.74) | |
| > High school diploma | 0.73 (0.38-1.40) | |
| Race | 0.25 | |
| White | 1.0 | |
| Other | 1.58 (0.73-3.42) | |
| Marital status (n=569) | 0.45 | |
| Never married | 1.0 | |
| Married/member of couple | 0.74 (0.45-1.22) | |
| Divorced/widowed/separated | 0.87 (0.48-1.58) | |
| Employment (n=569) | 0.14 | |
| Works full-time or part-time | 1.0 | |
| Unemployed/disabled | 0.80 (0.49-1.29) | |
| Other | 1.49 (0.88-2.53) | |
| Occupation (n=568) | 0.0001 | |
| Professional (has a degree) | 1.0 | |
| Skilled labor | 2.46 (1.32-4.57) | |
| Unskilled labor | 3.84 (2.16-6.83) | |
| Other | 2.90 (1.43-5.87) | |
| Insurance type (n=566) | <0.0001 | |
| Private (job or purchased) | 1.0 | |
| Medicaid/Medicare | 3.65 (2.34-5.69) | |
| No coverage | 3.83 (2.30-6.38) | |
| Poverty income ratio (n=542) | 0.0002 | |
| High (advantaged) | 1.0 | |
| Low (disadvantaged) | 2.14 (1.43-3.20) | |
| Socioeconomic position (SEP) (n=539) | ||
| Childhood SEP | 0.0032 | |
| High | 1.0 | |
| Low | 1.82 (1.22-2.70) | |
| Adult SEP | <0.0001 | |
| High | 1.0 | |
| Low | 4.50 (2.66-7.63) | |
| Depressive symptoms | ||
| CES-D score (n=569) | < 0.0001 | |
| < 16 | 1.0 | |
| ≥ 16 | 2.86 (1.93-4.24) | |
| Maternal factors | ||
| First pregnancy | < 0.0001 | |
| ≥ age 20 years | 1.0 | |
| < age 20 years | 2.21 (1.50-3.24) | |
| Currently a single mother | 0.22 | |
| No | 1.0 | |
| Yes | 1.47 (0.79-2.73) | |
Table 3.
Adjusted Odds Ratios and 95% Confidence Intervals from Multivariable Logistic Regression Model (n=537)
| Characteristic | OR (95% CI) of being a current smoker vs. nonsmoker | p value |
|---|---|---|
| Age | 0.002 | |
| ≥ 51 | 1.0 | |
| 31–50 | 2.30 (1.22-4.33) | |
| 18–30 | 3.29 (1.72-5.34) | |
| Adult SEP | 0.0001 | |
| High | 1.0 | |
| Low | 3.05 (1.74-5.34) | |
| CES-D score | 0.002 | |
| < 16 | 1.0 | |
| ≥ 16 | 1.99 (1.31-3.05) | |
| First pregnancy | 0.010 | |
| ≥ age 20 years | 1.0 | |
| < age 20 years | 1.74 (1.14-2.66) |
Area under the receiver operating characteristic (ROC) curve: 0.74.
Hosmer-Lemeshow goodness-of-fit test: chi-square statistic=4.95, p=0.67.
Associations in the final model indicated that women aged 31–50 (odds ratio [OR] 2.30, 95% confidence interval [CI] 1.22-4.33) and 18–30 (OR 3.29, 95% CI 1.72-5.34) were significantly more likely to currently smoke compared to those aged≥51. Disadvantage as an adult (low adult SEP) was significantly related to current smoking. These women were more than three times as likely to smoke compared to those with high adult SEP (OR 3.05, 95% CI 1.74-5.34). Those reporting a CES-D score≥16 were almost twice as likely to currently smoke (OR 1.99, 95% CI 1.31-3.05) compared to those with a score <16. Women who became pregnant with a first child before age 20 were significantly more likely to smoke (OR 1.74, CI 1.14-2.66) than women who first experienced a pregnancy after age 20.
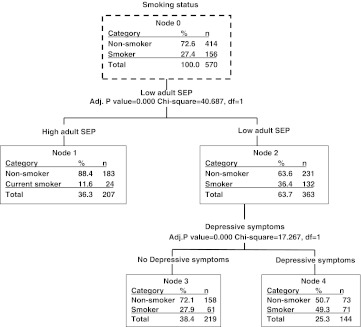
CHAID analyses
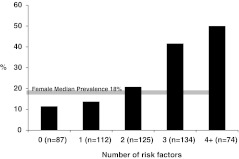
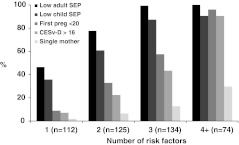
Figure 1 presents the current smoking prevalence, according to the number of risk factor variables for smoking. It was apparent that significant disparity in prevalence existed based on the number of risk factors reported by each female respondent. Specifically, about 10% of women with no risk factors currently smoked, as compared to 50% of women who reported four or more risk factors. Figure 2 presents the distribution of risk factors according to number reported. Low adult SEP represented the most prevalent factor for each number category, and single motherhood factor was the least prevalent in each number category.
FIG. 1.
Prevalence of current smoking by number of risk factors (n=532). Number of risk factors for smoking is displayed on the horizontal axis and corresponds to the prevalence of current smoking. A shaded line at 18% indicates the U.S. female median smoking prevalence.6
FIG. 2.
Risk factor type distribution according to number of factors, including low adult socioeconomic position (SEP), low child SEP, first pregnancy at less than age 20, Center for Epidemiologic Studies Depression scale score (CES-D)>16), single mother: n=445.
According to the CHAID analyses (Fig. 3), adult SEP (p=0.0000) was most strongly related to smoking status, as this risk factor was the first split in the decision tree. A total of 132 women were segmented into the low adult SEP category. Of these, 36.4% were current smokers compared to 11.6% of high adult SEP women. Further, among the low adult SEP subset, depressive symptoms were significantly associated with smoking status (p=0.000). For low adult SEP women with an elevated CES-D score, the prevalence of current smoking was 49.3%.
FIG. 3.
Chi-square automatic interaction detection (CHAID) analysis for significant risk factors, indicating that low adult SEP and depressive symptoms are associated with smoker category.
Discussion
This investigation was designed to expand our conceptualization of persistent smoking by including a life course perspective of risk factors, including SEP in childhood and as an adult, early pregnancy, and single motherhood, as well as depression. The disparity in smoking prevalence that was noted among women in this study was striking and points to the disproportionate future burden of disease that faces disadvantaged women. Fifty percent of women with four or more risk factors were current smokers and at increased risk for future tobacco-attributable disease and death. Of concern, this prevalence estimate is significantly higher than the current 18% in the U.S. female population and the 10% estimate that was observed among women in this study who reported no social, demographic, or psychologic risk factors.
The overwhelming majority (95%) of women enrolled in this study were white, which is consistent with the racial makeup of the Appalachian region of Ohio. The sample was younger than the general population of Appalachian women, with>95%<age 65 compared to 84.2% in the 2000 Census estimates within the region.46 Recruiting women from primary care and women's health clinics, where reproductive services are provided, may partially explain the overrepresentation of women aged≤50. Other demographic characteristics that differed between the sample and the general population (for women aged≥25) included a higher percentage of study participants with≥high school education (92.5%) compared to 78.5% in Appalachian Ohio counties.46 In addition, more study participants were employed (68.7% vs. 49.5% of Appalachian Ohio women).46 Despite these differences, the sample resembled the Appalachian population in that one third of women reported an annual household income of≤$20,000, and a similar proportion (37%) were employed in unskilled labor occupations. With regard to smoking status, approximately 27% of study participants were classified as current smokers, which was comparable to other population-based estimates for women residents of Appalachian Ohio counties at the time of data collection.47,48 Overall, social and demographic characteristics of smoking participants indicated more disadvantage as a child and at present, in contrast to never smokers and former smokers.
The final logistic regression model allowed for assessment of the independent effect of each variable and supported the relationship between factors that comprise the Social Determinants of Health framework.4 SEP in adulthood was associated with current smoking. Disadvantage, as measured by material and social factors, increased the odds of smoking among women enrolled in this study. Having less education, less income, and no health insurance as an adult (i.e., low adult SEP) was associated with smoking. The circumstance of early parenthood (i.e., first pregnancy before age 20) was also related to whether a woman currently smoked. This finding is consistent with studies of English10 and Australian14 women, where mothers, often living as the lone adult in the home, are surrounded by disadvantage. Other circumstances associated with pregnancy deserve consideration in future studies. For example, Bailey and Daugherty27 observed that pregnant women who experienced intimate partner violence were more likely to smoke. Also, depressive symptoms were reported by approximately half of the women who smoked, and the presence of these symptoms significantly increased the likelihood of smoking.
The CHAID, or decision tree analysis, identified subsets (or nodes) that were categorized by different risk factors. The final subsets significantly associated with current smoking included low adult SEP and depressive symptoms. Given the cycle of poverty described among women who smoke,6,10 it is not surprising these nodes were identified. Depression is related to current smoking,15 and using nicotine as a way to self-medicate for depression has been described.49 Further, a CES-D score≥16 was noted in 13.9% of those with a high childhood and high adult SEP, 11.5% with a low childhood and high adult SEP, 31.4% with a high childhood and low adult SEP, and 43.9% with a low childhood and low adult SEP (results not presented). The CHAID analysis confirmed that depressive symptoms not only were more common among low-income adult SEP women but also were significantly associated with smoking prevalence. The results of the current study may be used to inform tobacco dependence treatment efforts. Future clinical trials should investigate the combined risk factors of depression among low SEP women as it relates to treatment outcome or abstinence from smoking. Treating depression should be considered a priority for healthcare providers who manage the care of low SEP women who smoke. In future studies, the role of depression should be addressed, especially in clinic-based tobacco dependence treatment trials, where the disorder can be appropriately managed by a healthcare provider.
The statistical analyses conducted in this study were partially based on the work of Ho et al.13 comparing logistic regression and CHAID in an analysis of risk factors for cervical cancer. More recently, Nickelson et al.49 compared the two analytic techniques in a study that characterized social and demographic factors among adolescents enrolled in a physical activity intervention. CHAID has also been conducted for audience segmentation analysis among subgroups of women screened for breast cancer50 and adolescents at risk for obesity.51 In the current study, both analytic approaches provided important information about the role of variables associated with current smoking. However, the methodologic assumptions of each test differed. Logistic regression modeling allowed for examination of the independent effect of each variable and assumed that variables of interest were uniform for all participants. Conversely, the CHAID analysis assumed that this effect was not identical across participants but specific to identified subsets of participants. As an example, the logistic regression analysis identified depressive symptoms as an independent risk factor for smoking across all participants, after controlling for other risk factors. However, the CHAID analysis specified that depressive symptoms were particularly important for women with low adult SEP. Although the tests held different assumptions, they both contributed to an understanding of smoking prevalence. Overall, the findings from both analyses were consistent with regard to the relationship between low adult SEP and depressive symptoms and current smoking.
These findings add to a growing body of literature that emphasizes the social and contextual factors that partially explain smoking behavior.4–6,10,14,52 This perspective deserves equal consideration in explaining the persistence of smoking in disadvantaged groups. Understanding the combination of social and material factors and life course circumstances associated with smoking helps to determine the mechanisms responsible for the behavior and can guide tobacco control efforts. The current findings indicated that low SEP as an adult woman, depressive symptomatology, and early age at first pregnancy are associated with persistent smoking. As Graham et al.6,10 and others53 have observed, social policies may be necessary precursors to changing tobacco-related behaviors among vulnerable groups, and in fact, social policies may act as tobacco control policies.
For women living in poverty, evidenced by early parenthood, a lower income, and a lack of private health insurance, smoking behavior may persist if social conditions are not modified. An uninsured woman who lacks access to tobacco dependence therapy and treatment for depression is highly likely to continue smoking. Modifying social policies by promoting participation in the educational system or reducing the risks of early motherhood may improve subsequent employment opportunities that help women accumulate material resources, including health insurance. Another tobacco control policy might involve an employed woman accessing her worksite smoking cessation program, which may provide a pathway to quitting smoking. Other organizational policies might include bundling tobacco dependence treatment with other social services accessed by women. Armour et al.54 recommend combining food assistance and tobacco control programs, as food-insecure families often smoke. As low income women are especially responsive to messages about cigarette prices,8 these types of initiatives may be worthwhile.
Past tobacco control efforts have focused primarily on initiatives aimed at designing educational or behavioral interventions to assist individual smokers in quitting.55 The most recent update to a U.S. clinical practice guideline with recommendations to healthcare providers to assist their patients to quit includes information tailored to smokers with low SES.56 Here again, the focus has been primarily on educational and clinical interventions without addressing social factors, such as low income and early age at time of pregnancy, as well as other policy-related variables that may explain persistent smoking.
Several limitations were evident in the present study. First, 22 clinics were identified for inclusion in the sampling plan, but only 14 clinics agreed to participate. Although this number was sufficient, women recruited from the participating clinics may differ from women in nonparticipating clinics or women from Appalachia in general. Reasons for clinic refusal were unable to be ascertained, other than staff was too busy or not interested. Second, the clinic lists contained names of many women seen in the past 2 years who were unable to be reached by mail or phone at the time of invitation, limiting generalizability. Once contact was made with a potential participant, however, the cooperation rate was 71%. In addition, women enrolled in this study were younger, more likely to be employed, and better educated compared to the general Ohio Appalachian population, which may restrict generalizability. The cross-sectional design also limits the ability to characterize the order of selected events in relation to smoking status. Finally, the childhood life course SEP required the participant to recall parents' educational level and whether both parents lived with the participant at age 14. However, the reliability and validity of this measure have been demonstrated previously.39
Conclusions
This report documented that women in this region experience a variety of social, demographic, and maternal risk factors that increase the risk of current smoking as an adult. Because of their high prevalence of cigarette smoking and high rates of poverty, Appalachian women could be at increased risk for future life-threatening diseases. As health and health behaviors are influenced by the social environment, further research is warranted to expand the characterization of these underlying mechanisms. Their role in explaining health disparities among Appalachian women must be addressed. This information can be used to develop and test tailored social services that accompany organizational tobacco policies that focus primarily on reducing smoking prevalence in uniquely disadvantaged populations similar to women in the Appalachian Ohio region.
Acknowledgments
This study was funded by the National Cancer Institute (P50 CA105632), the Behavioral Measurement Shared Resource at The Ohio State University Comprehensive Cancer Center (P30 CA016058) from the National Cancer Institute; and the General Clinical Research Center at The Ohio State University from the National Center for Research Resources (M01 RR00034).
We thank the women who participated in this research and the field staff who implemented this study.
Disclosure Statement
No competing financial interests exist.
References
- 1.U.S. Department of Health and Human Services. Atlanta, CA: U.S. Department of Health and Human Services. Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. The health consequences of smoking: A report of the Surgeon General. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Hyattsville, MD: U. S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2010. Health, United States, 2009. [Google Scholar]
- 3.Centers for Disease Control and Prevention. Cigarette smoking among adults—United States, 2004. MMWR. 2005;54:1121–1124. [PubMed] [Google Scholar]
- 4.Brunner E. Marmot M. Social organization, stress and health. In: Marmot M, editor; Wilkinson RG, editor. Social determinants of health. Oxford, UK: Oxford University Press; 2001. pp. 17–43. [Google Scholar]
- 5.Gilman SE. Abrams DB. Buka SL. Socioeconomic status over the life course and stages of cigarette use: Initiation, regular use, and cessation. J Epidemiol Community Health. 2003;57:802–808. doi: 10.1136/jech.57.10.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graham H. Inskip HM. Francis B. Harman J. Pathways of disadvantage and smoking careers: Evidence and policy implications. J Epidemiol Community Health. 2006;60(Suppl III):ii7–ii12. doi: 10.1136/jech.2005.045583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Tobacco use among adults—United States, 2005. MMWR. 2006;55:1145–1148. [Google Scholar]
- 8.Levy DT. Mumford EA. Compton C. Tobacco control policies and smoking in a population of low education women, 1992–2002. J Epidemiol Community Health. 2006;60:ii20–ii26. doi: 10.1136/jech.2005.045542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marano C. Schober SE. Brody DJ. Zhang C. Secondhand tobacco smoke exposure among children and adolescents: United States, 2003–2006. Pediatrics. 2009;124:1299–1305. doi: 10.1542/peds.2009-0880. [DOI] [PubMed] [Google Scholar]
- 10.Graham H. Francis B. Inskip HM. Harman J SWS Study Team. Socioeconomic life course influences on women's smoking status in early adulthood. J Epidemiol Community Health. 2006;60:228–233. doi: 10.1136/jech.2005.039784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Cigarette smoking among adults and trends in smoking cessation—United States, 2008. MMWR. 2009;58:1227–1232. [PubMed] [Google Scholar]
- 12.Shi L. Stevens GD. Lebrun LA. Faed P. Tsai J. Enhancing the measurement of health disparities for vulnerable populations. J Public Health Management Pract. 2008:S45–52. doi: 10.1097/01.PHH.0000338386.59565.dc. [DOI] [PubMed] [Google Scholar]
- 13.Ho SH. Jee SH. Lee JE. Park JS. Analysis on risk factors for cervical cancer using induction technique. Expert Syst Appl. 2004;27:97–105. [Google Scholar]
- 14.Siahpush M. Why is lone motherhood so strongly associated with smoking in Australia? Austral NZ J Public Health. 2004;28:37–42. doi: 10.1111/j.1467-842x.2004.tb00630.x. [DOI] [PubMed] [Google Scholar]
- 15.Hughes JR. Comorbidity and smoking. Nicotine Tobacco Res. 1999;1(Suppl 2):S149–152. doi: 10.1080/14622299050011981. [DOI] [PubMed] [Google Scholar]
- 16.Adler NE. Boyce WT. Chesney MA. Folkman S. Syme SL. Socioeconomic inequalities in health. No easy solution. JAMA. 1993;269:3140–3145. [PubMed] [Google Scholar]
- 17.Lynch JW. Kaplan GA. Shema SJ. Cumulative impact of sustained economic hardship on physical, cognitive, psychological, and social functioning. N Engl J Med. 1997;337:1889–1895. doi: 10.1056/NEJM199712253372606. [DOI] [PubMed] [Google Scholar]
- 18.Stimpson JP. Hyunsu J. Raji MA. Eschbach K. Neighborhood deprivation and health risk behaviors in NHANES III. Am J Health Behav. 2007;31:215–222. doi: 10.5555/ajhb.2007.31.2.215. [DOI] [PubMed] [Google Scholar]
- 19.Winger PA. Tucker TA. Jamison PM, et al. Cancer in Appalachia, 2001–2003. Cancer. 2008;112:181–192. doi: 10.1002/cncr.23132. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Atlanta, GA: U.S. Department of Health and Human Services, National Center for Chronic Disease Prevention and Health Promotion; 2010. Division for Heart Disease and Stroke Prevention. Data trends & maps web site. [Google Scholar]
- 21.Appalachian Regional Commission. Data reports. Socioeconomic data. 2007. www.arc.gov/data. [Apr 6;2009 ]. www.arc.gov/data
- 22.Thorne D. Tickamyer A. Thorne M. Poverty and income in Appalachia. J Appalachian Stud. 2005;10:341–358. [Google Scholar]
- 23.Ohio Department of Health. Columbus, OH: The Ohio Health Monograph Series; 2007. Tobacco use: An Ohio profile. [Google Scholar]
- 24.State of Ohio. Columbus: Ohio State University, Ohio Colleges of Medicine Government Resource Center; 2009. Department of Insurance, Department of Job and Family Services, Department of Health, and Department of Mental Health. Ohio Family Health Survey, 2008–2009 [Computer file] [Google Scholar]
- 25.Centers for Disease Control and Prevention. Coronary heart disease mortality trends among whites and blacks—Appalachia and the United States, 1980–1993. MMWR. 1998;47:1005–1015. [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Cancer death rates—Appalachia, 1994–1998. MMWR. 2002;51:527–529. [PubMed] [Google Scholar]
- 27.Bailey BA. Daugherty RA. Intimate partner violence: Incidence and associated health behaviors in a rural population. Matern Child Health J. 2007;11:495–503. doi: 10.1007/s10995-007-0191-6. [DOI] [PubMed] [Google Scholar]
- 28.Campbell MK. Tessaro I. Devellis B, et al. Effects of tailored health promotion program for female blue-collar workers: Health works for women. Prev Med. 2002;34:313–323. doi: 10.1006/pmed.2001.0988. [DOI] [PubMed] [Google Scholar]
- 29.Coker AL. DeSimone CP. Eggleston KS. Hopenhayn C. Nee J. Tucker T. Smoking and survival among Kentucky women diagnosed with invasive cervical cancer. Gynecol Oncol. 2009;112:365–369. doi: 10.1016/j.ygyno.2008.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hahn EJ. Rayens MK. Butler KM. Zhang M. Durbin E. Steinke D. Smoke-free laws and adult smoking prevalence. Prev Med. 2008;47:206–209. doi: 10.1016/j.ypmed.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 31.Northridge ME. Vallone D. Xiao H, et al. The importance of location for tobacco cessation: Rural-urban disparities in quit success in underserved West Virginia counties. J Rural Health. 2008;24:106–115. doi: 10.1111/j.1748-0361.2008.00146.x. [DOI] [PubMed] [Google Scholar]
- 32.Whalen U. Griffin MR. Shintani A, et al. Smoking rates among pregnant women in Tennessee, 1990–2001. Prev Med. 2006;43:196–199. doi: 10.1016/j.ypmed.2006.04.021. [DOI] [PubMed] [Google Scholar]
- 33.Paskett ED. McLaughlin JM. Reiter PL, et al. Psychosocial predictors of adherence to risk-appropriate cervical cancer screening guidelines: A cross-sectional study of women in Ohio Appalachia participating in the Community Awareness Resources and Education (CARE) project. Prev Med. 2010;50:74–80. doi: 10.1016/j.ypmed.2009.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ohio Department of Health. Columbus: Ohio Department of Health; 2002. Ohio Cancer Incidence Surveillance System. [Google Scholar]
- 35.Baumann M. Spitz E. Guillemen F, et al. Associations of social and material deprivation with tobacco, alcohol, and psychotropic drug use, and gender: A population-based study. Int J Health Geogr. 2007;6:50–62. doi: 10.1186/1476-072X-6-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krieger N. Williams DR. Moss NE. Measuring social class in U.S. public health research: Concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- 37.Loucks EB. Magnusson KT. Cook S, et al. Socioeconomic position and the metabolic syndrome in early, middle and late life: Evidence from NHANES 1999–2002. Ann Epidemiol. 2007;17:782–790. doi: 10.1016/j.annepidem.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 38.Salsberry PJ. Reagan PB. Comparing the influence of childhood and adult economic status on midlife obesity in Mexican American, white and African American women. Public Health Nurs. 2009;26:14–22. doi: 10.1111/j.1525-1446.2008.00751.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cohen S. Doyle WJ. Turner RB. Alper CM. Skoner DP. Childhood socioeconomic status and host resistance to infectious illness in adulthood. Psychosom Med. 2004;66:553–558. doi: 10.1097/01.psy.0000126200.05189.d3. [DOI] [PubMed] [Google Scholar]
- 40.U.S. Census Bureau. How the Census Bureau measures poverty. www.census.gov/hhes/www/poverty/about/overview/measure.html. [Sep 6;2009 ]. www.census.gov/hhes/www/poverty/about/overview/measure.html
- 41.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 42.Centers for Disease Control and Prevention. Cigarette smoking among adults—United States, 1992, and changes in the definition of current cigarette smoking [published erratum appears in MMWR 1994;43:801–803] MMWR. 1994;43:342–346. [PubMed] [Google Scholar]
- 43.Hosmer DW. Lemeshow S. Applied logistic regression. 2nd. New York: Wiley; 2000. pp. 116–167. [Google Scholar]
- 44.Michael JA. Gordon SL. Data mining technique: For marketing, sales and customer support. New York: Wiley; 1997. [Google Scholar]
- 45.The American Association for Public Opinion Research. Standard definitions: Final dispositions of case codes and outcome rates for surveys. 4th. 2006. www.aapor.org/Standard_Definitions/1818.htm. [Feb 1;2010 ]. www.aapor.org/Standard_Definitions/1818.htm
- 46.United States Census Bureau. U.S. Census Bureau datasets. www2.census.gov/census_2000/datasets. [May 22;2009 ]. www2.census.gov/census_2000/datasets
- 47.Ohio Department of Health. Columbus: Ohio Department of Health; 2005. Behavior Risk Factor Surveillance System. [Google Scholar]
- 48.Ohio Department of Health. Columbus: Ohio Department of Health; 2006. Ohio Adult Tobacco Survey. [Google Scholar]
- 49.Nickelson J. Alfonso ML. McDermott RJ, et al. Characteristics of “tween” participants and non-participants in the VERB™ summer scorecard physical activity promotion program. Health Educ Res. 2011;26:225–238. doi: 10.1093/her/cyq089. [DOI] [PubMed] [Google Scholar]
- 50.Forthofer MS. Bryant CA. Using audience-segmentation techniques to tailor health behavior change strategies. Am J Health Behav. 2000;24:36–43. [Google Scholar]
- 51.BeLue R. Francis LA. Rollins B. Colaco B. One size does not fit all: Identifying risk profiles for overweight in adolescent population subsets. J Adolesc Health. 2009;45:517–524. doi: 10.1016/j.jadohealth.2009.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jarvis MF. Wardle J. Social patterning of individual health behaviours: The case of cigarette smoking. In: Marmot M, editor; Wilkinson RG, editor. Social determinants of health. Oxford, UK: Oxford University Press; 2001. pp. 240–255. [Google Scholar]
- 53.Greaves L. Jategaonkar N. Tobacco policies and vulnerable girls and women: Toward a framework for gender sensitive policy development. J Epidemiol Community Health. 2006;60:ii57–ii65. doi: 10.1136/jech.2005.045393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Armour BS. Pitts M. Lee C-W. Cigarette smoking and food insecurity among low-income families in the United States, 2001. Am J Health Promotion. 2008;22:386–392. doi: 10.4278/ajhp.22.6.386. [DOI] [PubMed] [Google Scholar]
- 55.U.S. Department of Health and Human Services. Tobacco cessation. Office of the Surgeon General. www.surgeongeneral.gov/tobacco/ [Jul 1;2011 ]. www.surgeongeneral.gov/tobacco/
- 56.Fiore MC. Jaen C. Baker T, et al. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2008. Treating tobacco use and dependence: 2008 update. Clinical Practice Guideline; p. 151. [Google Scholar]