Abstract
Introduction
Sudden cardiac arrest is one of the most frequent causes of death in the world. In highly qualified emergency medical service (EMS) systems, including well-trained emergency physicians, spontaneous circulation may be restored in up to 53% of patients at least until admission to hospital. Compared with these highly qualified EMS systems, markedly lower success rates are observed in other systems. These data clearly show that there are considerable differences between EMS systems concerning treatment success following cardiac arrest and resuscitation, although in all systems international guidelines for resuscitation are used. In this study, we investigated the impact of response time reliability (RTR) on cardiopulmonary resuscitation (CPR) incidence and resuscitation success by using the return of spontaneous circulation (ROSC) after cardiac arrest (RACA) scores and data from seven German EMS systems participating in the German Resuscitation Registry.
Methods
Anonymised patient data after out-of-hospital cardiac arrest gathered from seven EMS systems in Germany from 2006 to 2009 were analysed with regard to socioeconomic factors (population, area and EMS unit-hours), process quality (RTR, CPR incidence, special CPR measures and prehospital cooling), patient factors (age, gender, cause of cardiac arrest and bystander CPR). End points were defined as ROSC, admission to hospital, 24-hour survival and hospital discharge rate. χ2 tests, odds ratios and the Bonferroni correction were used for statistical analyses.
Results
Our present study comprised 2,330 prehospital CPR patients at seven centres. The incidence of sudden cardiac arrest ranged from 36.0 to 65.1/100,000 inhabitants/year. We identified two EMS systems (RTR < 70%) that reached patients within 8 minutes of the call to the dispatch centre 62.0% and 65.6% of the time, respectively. The other five EMS systems (RTR > 70%) reached patients within 8 minutes of the call to the dispatch centre 70.4% up to 95.5% of the time. EMS systems arriving relatively later at the patients side (RTR < 70%) initiate CPR less frequently and admit fewer patients alive to hospital (calculated per 100,000 inhabitants/year) (CPR incidence (1/100,000 inhabitants/year) RTR > 70% = 57.2 vs RTR < 70% = 36.1, OR = 1.586 (99% CI = 1.383 to 1.819); P < 0.01) (admitted to hospital with ROSC (1/100,000 inhabitants/year) RTR > 70% = 24.4 vs RTR < 70% = 15.6, OR = 1.57 (99% CI = 1.274 to 1.935); P < 0.01). Using ROSC rate and the multivariate RACA score to predict outcomes, we found that the two groups did not differ, but ROSC rates were higher than predicted in both groups (ROSC RTR > 70% = 46.6% vs RTR < 70% = 47.3%, OR = 0.971 (95% CI = 0.787 to 1.196); P = n.s.) (ROSC RACA RTR > 70% = 42.4% vs RTR < 70% = 39.5%, OR = 1.127 (95% CI = 0.911 to 1.395); P = n.s.)
Conclusion
This study demonstrates that, on the level of EMS systems, faster ones more often initiate CPR and increase the number of patients admitted to hospital alive. Furthermore, we show that, with very different approaches, all centres that adhere to and are intensely trained according to the 2005 European Resuscitation Council guidelines are superior and, on the basis of international comparisons, achieve excellent success rates following CPR.
Introduction
Sudden cardiac arrest is one of the most frequent causes of death in the world. In the United States and Europe, about 300,000 and 450,000 people, respectively, meet this fate [1,2]. Males are affected markedly more frequently than females: The ratio is 4.1:2.7 [3]. In Germany, data derived from the World Health Organisation's MONICA registry (Multinational Monitoring of Trends and Determinants of Cardiovascular Disease) show a predicted incidence 123/100,000 inhabitants/year in the 35- to 64-year-old age group [4,5], whereas in the European Union (EU), per 100,000 inhabitants, resuscitation attempts are performed to treat only about 55 patients [1,6-9]. Thus, in the EU, with about 500 million inhabitants, more than 275,000 resuscitation attempts are made annually. However, more than half of the patients in sudden cardiac arrest die without any resuscitation attempt because the event occurs unwitnessed or the emergency medical service (EMS) team, owing to statutory requirements, arrives too late at the patient's site and only can declare the patient's death. Out-of-hospital cardiopulmonary resuscitation (CPR) poses a huge challenge to emergency medical services because sudden cardiac death is a particularly time-critical event. Additionally, successful management requires a complex and target-oriented response of all acting persons and the entire chain of survival, from dispatch centre personnel to the hospital team.
To improve treatment, the International Liaison Committee on Resuscitation (ILCOR), or rather the European Resuscitation Council (ERC), publishes new resuscitation guidelines regularly every 5 years, with the latest one being released in October 2010 [10-17]. To develop these guidelines, experts in various scientific fields screen and evaluate current studies, amongst which are studies concerning 'telephone-guided CPR' [18-20], therapeutic hypothermia [21-24] or vasopressin treatment [25-27]. Following publication of the guidelines, it is essential to teach and subsequently implement them into EMS systems.
In highly qualified EMS systems, including well-trained emergency physicians, spontaneous circulation may be restored in up to 53% of patients at least until admission to hospital [1,9,28]. Discharge rates in these EMS systems are reported to be 14% to 20%, and 1-year survival rates can reach up to 12%. The 10-year survival rates of patients discharged from hospital may reach 46% [1,9,28,29]. Compared with these highly qualified EMS systems, markedly lower success rates are observed in other EMS systems, with only 9% to 12% of patients being admitted to hospital and only 1% to 3% being discharged from hospital with good neurological outcomes [1,8,9,28-30].
These data clearly show that there are considerable differences between EMS systems concerning treatment success following cardiac arrest and resuscitation, although in all systems the current international guidelines for resuscitation are used [1,6,8,9,28]. It is therefore essential to analyse the reasons for these differences. However, few studies have been published correlating resuscitation results with known influencing factors such as response times, qualifications of team members, actions taken during resuscitation and quality management procedures.
Not least for this purpose, the German Society for Anaesthesiology and Intensive Care Medicine (Deutsche Gesellschaft für Anästhesiologie und Intensivmedizin (DGAI)) has set up the German Resuscitation Registry (GRR), which was officially implemented in 2007 [31,32]. In this study, we investigated the impact of response time reliability (RTR) on CPR incidence and resuscitation success using return of spontaneous circulation (ROSC) after cardiac arrest (RACA) score and data from seven German EMS systems participating in the GRR.
Materials and methods
Participating centres
The following are the participating EMS systems studied: (1) the city of Bonn, (2) the county hospital 'Klinik am Eichert', Göppingen, (3) the county of Gütersloh, (4) the city of Münster, (5) the county of Tübingen, (6) the county of Rendsburg-Eckernförde and (7) the region of Marburg. In all of these seven EMS systems, well-trained emergency physicians are responsible for the resuscitation procedures performed at the emergency site. The EMS systems named and the scientific advisory board of the resuscitation registry of the DGAI approved the participation in and the performance of this comparison (trial no. 02/2011 ReaReg).
The German Resuscitation Registry
The nationwide interdisciplinary GRR run by the DGAI, based on national and international recommendations (MIND2, Utstein-style guidelines and reporting templates, European Registry of Cardiac Arrest (EuReCa) and ILCOR Guidelines), is described in detail elsewhere [2,31,32]. It centrally collects data from 84 participating centres. We analysed the quality reports of the seven centres that participated in our study.
Inclusion criteria for the resuscitation registry
Patients in whom out-of-hospital cardiac arrest (OHCA) had been diagnosed and a resuscitation attempt had been performed were included independently of the reason for OHCA. Great value was set upon all EMS treatment details and all corresponding data being completely transferred into the resuscitation registry, making it possible to calculate the resuscitation incidence.
Study period
The study period comprises the years 2006 to 2009. However, the single EMS systems reported periods of various lengths. The centres provided complete data sets for at least one entire calendar year.
Structural process and quality of results
According to requirements of the resuscitation registry, the following structural quality data of the EMS systems were recorded: the population served; the service area; population density; unit-hours of advanced cardiac life support (ALS) or basic life support (BLS), unit hours/100,000 inhabitants/year and unit-hours per service area. A 'unit-hour' is defined as a fully equipped response unit's being on a response or waiting for a response for 1 hour.
The following data regarding process quality were recorded: RTR (rate (%) of first vehicles' arriving at the scene within 8 minutes of the call to the dispatch centre); response time interval defined as the time from the call's being received in the dispatch centre until the arrival of the first ambulance at the scene, calculated using the time stamps available with dispatch technology; rate (%) of EMS CPR started within 8 minutes of the call to the dispatch centre; rate of dispatch under triage (no ALS unit (emergency physician-staffed) for the first alert); rate of special CPR measures (active compression decompression (ACD) CPR, load-distributing band (LDB) CPR, and CPR feedback); medical director and quality assurance programme; and rate of prehospital cooling to achieve therapeutic prehospital hypothermia.
According to the Utstein-style recommendations and requirements of the resuscitation registry, the following data regarding patients and the circumstances of their cardiac arrest were collected: cause of cardiac arrest, age, gender, witnessed by a bystander or EMS personnel, CPR performed by a bystander, location of cardiac arrest and first electrocardiogram (ECG) rhythm.
According to the Utstein-style recommendations and requirements of the resuscitation registry, the following data regarding resuscitation outcomes were recorded: ROSC, admitted to hospital with spontaneous circulation, 24-hour survival rate and hospital discharge rate.
Resuscitation procedures were performed according to the 2005 ILCOR guidelines. If not already initiated by bystanders or first responders, the resuscitation attempt was started or continued by the first team that arrived at the site (BLS or ALS unit).
Incidence of CPR attempts and resuscitation success
For the calculation of incidence, the number of patients in whom CPR was attempted and/or ROSC status and/or were admitted to hospital were counted. The incidence data refer to cases per 100,000 inhabitants of the respective EMS system areas per year.
Quality of CPR performance
To compare the quality of CPR performance between EMS systems, we used the percentage survival rates of all patients andespecially the subgroup of patients found in ventricular fibrillation (VF) and/or ventricular tachycardia (VT) (cardiac origin), according to the Utstein-style recommendations. To compare EMS systems, we used hospital admission rates and not discharge rates, because postresuscitation care has a significant impact on discharge rate.
The second method we used to compare the quality of CPR performance within the centres was the calculation of the RACA scores [33], which predict the ROSC rate (%), including the following factors: age, gender, cause of cardiac arrest, location of cardiac arrest, first ECG rhythm, CPR performed by a bystander and time of EMS arrival.
Statistics and analysis
Data were processed using Excel XP software (Microsoft Corp, Redmond, WA, USA). Distributions are reported as absolute numbers and percentages. Statistical analyses were performed using χ2 and t-tests, respectively, with a difference of P < 0.05 considered statistically significant. The Bonferroni correction was used to neutralise the α error in connection with multiple paired comparisons. For analysis of the influence of the RTR on CPR incidence and success, we grouped the EMS systems by RTR using a cut-off level of 70%. Odds ratios and confidence intervals were calculated to compare the two groups of EMS systems. The analysis of numeric variables is specified with means and standard deviations using the SPSS version 14.0 statistical software package (SPSS Inc, Chicago, IL, USA).
Ethics committee vote
The design and publication of this study were approved by the scientific committee of the GRR in compliance with current publication guidelines. Patients' informed consent was waived by the ethics committee of the University of Cologne Faculty of Medicine (Kerpener Strasse 62, D-50937 Cologne, Germany), due to the fact thatanalysis of anonymous data collection for quality management was not considered necessary to be approved.
Results
Sociodemographic characteristics
The EMS systems of Bonn and Münster serve big-city population structures with a high population density, whereas the EMS systems in Rendsburg-Eckernförde, Marburg and Tübingen cover rural areas with a low population density (Table 1). Göppingen and Gütersloh have both urban and rural areas within their EMS regions. Time periods ranging from 12 months (Marburg) and 44 months (Göppingen) were analysed. The entire study period was from 1 May 2006 to 31 December 2009, and during that time 2,330 resuscitation attempts were started.
Table 1.
Sociodemographic characteristics of the centres
| Sociodemographic characteristics | Bonn | Göppingen | Gütersloh | Marburg | Münster | Rendsburg-Eckernförde | Tübingen | P-value | Totals or averages |
|---|---|---|---|---|---|---|---|---|---|
| Served population, (n) | 315,000 | 192,000 | 319,732 | 251,800 | 280,199 | 272,488 | 218,692 | 1,849,911 | |
| Service area (km2) | 141.0 | 354.0 | 864.0 | 1,262.6 | 302.9 | 2,185.9 | 519.2 | 5,629.6 | |
| Population density (1/km2) | 2,234.0 | 542.4 | 370.1 | 199.4 | 925.0 | 124.7 | 421.2 | 328.6 | |
| Time frame | 1 Jan 2007 to 31 Dec 2009 | 1 May 2006 to 31 Dec 2009 | 1 Nov 2007 to 31 Dec 2009 | 1 Jan 2008 to 31 Dec 2008 | 1 Jun 2007 to 31 Dec 2009 | 1 Jan 2006 31 Dec 2007 | 1 Jan 2007 to 31 Dec 2009 | ||
| Person-years | 945,000 | 704,000 | 692,753 | 251,800 | 723,847 | 544,976 | 656,076 | 4,518,452 | |
| CPR attempted (n) | 533 | 399 | 410 | 164 | 391 | 196 | 237 | 2,330 | |
| CPR incidence (1/year/100,000 inhabitants) | 56.4 | 56.7 | 59.2 | 65.1 | 54.0 | 36.0 | 36.1 | < 0.001 | 50.6 |
| Rate of first vehicle's reaching emergency patient within 8 minutes (%) | 95.5 | 70.4 | 77.9 | 79.8 | 90.0 | 65.6 | 62.0 | < 0.001 | 80.0 |
| Rate of CPR started within 8 minutes (%) | 67.9 | 60.6 | 57.6 | 57.9 | 64.2 | 56.0 | 53.0 | < 0.001 | 60.3 |
| Witnessed (%) | 64.2 | 58.1 | 58.3 | 67.7 | 59.6 | 65.8 | 49.4 | < 0.001 | 60.2 |
| Witnessed by bystander (%) | 53.8 | 45.6 | 47.1 | 58.5 | 53.2 | 59.7 | 38.4 | < 0.001 | 50.4 |
| CPR performed by bystander (%) | 23.3 | 10.0 | 20.2 | 17.1 | 28.6 | 24.0 | 1.3 | < 0.001 | 18.8 |
| Witnessed and CPR performed by EMS (%) | 10.3 | 12.5 | 11.2 | 9.1 | 6.4 | 6.1 | 11.0 | 0.09 | 9.8 |
| Males (%) | 64.4 | 66.9 | 66.1 | 68.3 | 68.0 | 71.9 | 66.7 | 0.64 | 66.9 |
| Mean age (years) | 66.9 | 68.9 | 67.9 | 65.9 | 67.4 | 65.2 | 65.3 | 67.1 | |
| Median age (years) | 70.6 | 73.0 | 70.9 | 69.4 | 70.2 | 68.6 | 70.0 | 70.2 | |
| Age (SD) | 17.7 | 16.1 | 16.6 | 16.6 | 17.0 | 16.5 | 19.8 | 17.2 | |
| > 65 years old (%) | 65.5 | 71.4 | 67.3 | 57.9 | 63.4 | 62.2 | 66.2 | < 0.05 | |
| Location of cardiac arrest (%) | |||||||||
| Home | 70.5 | 68.2 | 77.6 | 71.3 | 68.0 | 69.4 | 69.2 | 0.05 | 70.8 |
| Public | 17.4 | 17.3 | 16.6 | 15.9 | 22.0 | 20.9 | 18.1 | 0.37 | 18.3 |
| Other | 12.0 | 14.5 | 5.9 | 12.8 | 10.0 | 9.7 | 12.7 | < 0.01 | 10.9 |
CPR = cardiopulmonary resuscitation; EMS = emergency medical service. Data are for service areas and populations served by the EMS systems. Unit hours = fully equipped response unit on a response or waiting for a response for 1 hour. P-values were calculated by t-test or χ2 test, with significance set at P < 0.05.
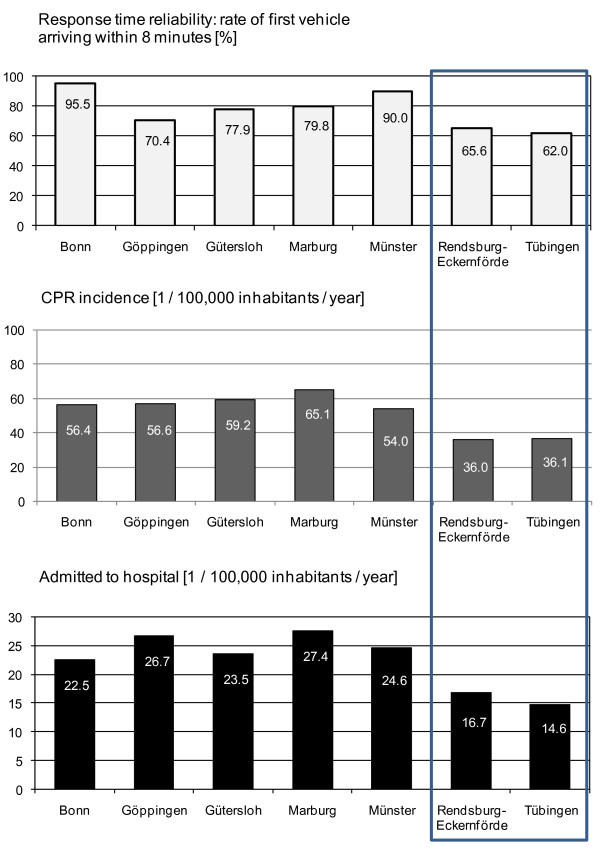
Response time reliability
In Tübingen and Rendsburg-Eckernförde, only 62.0% and 65.6%, respectively, of patients were reached by the EMS within 8 minutes after being alerted (Table 1 and Figure 1). In the other centres, 70.4% to 95.5% of the patients were treated by the EMS within this period of time. In the big-city areas of Bonn and Münster, about 90% of the patients were reached by the first ambulance within 8 minutes after the EMS was alerted. This performance is much faster than that in the other five EMS systems (P < 0.001). Accordingly, in Bonn and Münster, resuscitation attempts were started the earliest (67.9% and 64.2%, respectively, within 8 minutes after being alerted; P < 0.001).
Figure 1.
Response time reliability rate of first vehicle stop within 8 minutes of dispatch, cardiopulmonary resuscitation (CPR) incidence (1/100,000 inhabitants/year) and patients admitted to the hospital (1/100,000 inhabitants/year).
CPR incidence
The calculated incidence of sudden cardiac death followed by resuscitation attempt was between 36.0 and 65.1/100,000 inhabitants/year (Table 1 and Figure 1). In two regions (Rendsburg-Eckernförde and Tübingen), the CPR incidence amounted to 36.0 and 36.1/100,000 inhabitants/year, respectively. In the other regions with shorter response intervals, a minimum of 54 and up to 65.1 resuscitation attempts/100,000 inhabitants/year were registered (P < 0.001).
Circumstances of cardiac arrest
Cardiac arrest was witnessed in about 60% of patients, most rarely in Tübingen (49.4%) and most often in Marburg (67.7%) (P < 0.001) (Table 1). In most cases, the witnesses were laypeople or bystanders (38.4% in Tübingen and up to 59.7% in Rendsburg-Eckernförde; P < 0.001). EMS personnel were present at the scene when the cardiac arrest occurred less often (6.1% in Rendsburg-Eckernförde and up to 12.5% in Göppingen; P = 0.09). In contrast, the rate of bystander CPR attempts was low. Only in a few cases did laypeople start CPR before EMS arrival, even when they had witnessed the person's collapse. The rate of bystander CPR attempts was 1.3% in Tübingen and 28.6% in Münster (P < 0.001).
Men more frequently have cardiac arrests than women. A mean of 66.9% of the patients were male, and there were only minor differences between the centres (64.4% to 71.9%; P = 0.64). The mean age of patients collected from the different centres was comparable (67.1 ± 17.2 years), with patients being slightly younger in Rendsburg-Eckernförde (65.2 ± 16.5 years) and slightly older in Göppingen (68.9 ± 16.1 years). There were small differences between the centres regarding patients older than 65 years of age (P < 0.05). Regarding the site of cardiac arrest, there were small differences between centres. Most collapses occurred in domestic environments (68.0% to 77.6%; P = 0.05), in public places (15.9% to 22.0%; P = 0.37) and at other sites (5.9% to 14.5%; P < 0.01).
EMS systems, medical treatments and special measures
In all participating centres, the two-tiered system of BLS and ALS units has been established (emergency physician-staffed), meeting at the site of the emergency (Table 2). The availability of EMS teams results from the time during which units are held available. The highest amount of unit-hours/100,000 inhabitants/year was reported by Marburg (54,314 unit-hours) and the lowest was reported by Münster (22,603.2 unit-hours). The lowest amount of unit-hours/service area/year was reported by Rendsburg-Eckernförde (48.1 unit-hours) and the highest was reported by Bonn (723.1 unit-hours).
Table 2.
EMS systems data
| Description of the EMS systems | Bonn | Göppingen | Gütersloh | Marburg | Münster | Rendsburg-Eckernförde | Tübingen | P-value | Average | |
|---|---|---|---|---|---|---|---|---|---|---|
| Providers | City of Bonn/fire department | EMS, district of Göppingen, Klinik am Eichert Göppingen | EMS district of Gütersloh | EMS, district of Marburg | City of Münster/fire department | EMS, district of Rendsburg-Eckernförde | EMS, DRK and ASB Tübingen | All | ||
| Vehicles | Two-tiered system | Yes | Yes | Yes | Yes | Yes | Yes | Yes | ||
| ALS unit (emergency physician) | Unit-hours (1/year/100,000 inhabitants) | 5,561.9 | 6,463.5 | 10,959.2 | 10,436.9 | 6,252.7 | 6,429.6 | 8,011.3 | < 0.001 | 7,773.9 |
| BLS unit | Unit-hours (1/year/100,000 inhabitants) | 26,807.6 | 18,250.0 | 25,923.0 | 43,876.9 | 16,350.5 | 32,148.2 | 24,033.8 | < 0.001 | 26,964.8 |
| ALS + BLS unit | Unit-hours (1/year/100,000 inhabitants) | 32,369.5 | 24,713.5 | 36,882.1 | 54,313.7 | 22,603.2 | 38,577.8 | 32,045.1 | < 0.001 | 34,738.6 |
| ALS + BLS unit | Unit-hours/year/area (hours/km2) | 723.1 | 134.0 | 136.5 | 108.3 | 209.1 | 48.1 | 135.0 | < 0.001 | 114.2 |
| Quality assurance | Training programme | RA + RS: 30 hours/year | RA + RS: 30 hours/year NA: 12 hours/year |
RA + RS: 30 hours/year NA: 8 hours/year |
RA + RS: 38 hours/year NA: 8 hours/year |
RA + RS: 30 hours/year NA: 4 hours/year |
RA + RS: 30 hours/year | RA + RS: 30 hours/year NA: 12 hours/year |
||
| Additional emergency physician requested by ambulance crew | 9.0 | 11.5 | 8.8 | 11.6 | 17.9 | 8.7 | 3.8 | < 0.001 | 10.5 | |
| Equipment | LDB CPR (%) | 15.4 | 0.0 | 0.0 | 0.0 | 0.3 | 0.0 | 0.0 | < 0.001 | 3.6 |
| ACD CPR (%) | 4.5 | 42.6 | 0.0 | 5.5 | 7.2 | 0.0 | 6.8 | < 0.001 | 10.6 | |
| Feedback system (%) | 0.0 | 0.0 | 0.0 | 1.8 | 90.3 | 0.0 | 0.0 | < 0.001 | 15.3 | |
| Prehospital cooling | Cooling of ROSC patients (%) | 72.0 | 50.3 | 40.2 | 33.3 | 64.0 | 1.0 | 7.9 | < 0.001 | 46.2 |
ACD = active compression decompression; ALS unit = NEF (Notarzteinsatzfahrzeug): emergency vehicle providing advanced life support, including an emergency physician; ASB = Arbeiter Samariter Bund; BLS unit = RTW (Rettungswagen): emergency vehicle providing basic life support and defibrillation, without an emergency physician; CPR = cardiopulmonary resuscitation; DRK = Deutsches Rotes Kruez (German Red Cross); EMS = emergency medical service; LDB = load-distributing band; NA: Notarzt = emergency physician; RA: Rettungsassistent = PM: paramedic; ROSC = return of spontaneous circulation; RS: Rettungssanitäter = EMT: emergency medical technician. P-values were calculated by t-test or χ2 test, with significance set at P < 0.05.
It is essential that the staff of dispatch centres identify cardiac arrest victims correctly so that BLS and ALS units are sent out immediately. If an ALS unit has to be requested later by the BLS unit after the BLS unit's arrival at the scene, a deficit in identifying cardiac arrest results (under triage by the dispatch centre). The rate of under triage was different between Münster (17.9%) and Tübingen (3.8%) (P < 0.001).
In some centres, additional CPR devices are used besides the normal equipment. In Bonn, for example, in 15.4% of all cases, mechanical resuscitation was performed with a LDB CPR device. In Münster, a CPR feedback system was used for 90.3% of the patients. ACD CPR was not available in Gütersloh and Rendsburg-Eckernförde, whereas the other centres, most frequently in Göppingen (42.6%), used this system.
All centres have implemented regular CPR training, but with differences concerning intervals and intensity. For emergency physicians, the training is done partly on a voluntary basis. The recommended induction of mild hypothermia following resuscitation and ROSC was performed most frequently in Bonn (72.0%) and Münster (64.0%) and markedly less often in Tübingen (7.9%) and Rendsburg-Eckernförde (only 1.0%) (P < 0.001).
CPR success and clinical outcomes
Table 3 shows the survival rates following sudden cardiac arrest and resuscitation at the seven EMS systems (see also Figure 1). The survival rates were calculated by two different methods: (1) The survival rates were calculated as percentages for all patients and the respective Utstein subgroups, and (2) the absolute number of survivors/100,000 inhabitants/year are reported. The frequency of ROSC and hospital admissions with ROSC could be determined for all centres. The entire 24-hour survival data could be determined for Bonn, Göppingen, Gütersloh, Marburg, Münster and Tübingen, but not for Rendsburg-Eckernförde. Discharge rates were completely recorded only for Göppingen, Gütersloh and Marburg. Overall, 2,330 patients were resuscitated in the seven EMS systems. In 46.7%, spontaneous circulation could be restored, 42.8% of the patients were admitted to a hospital with ROSC, 30.7% survived for 24 hours, and 15.4% were discharged alive.
Table 3.
Clinical outcomes
| Clinical outcome | Bonn | Göppingen | Gütersloh | Marburg | Münster | Rendsburg-Eckernförde | Tübingen | p value (1/Y/100.000 I) |
p value (%) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [n] | [1/Y/100, 000 I | % | [n] | [1/Y/100, 000 I | % | [n] | [1/Y/100, 000 I | % | [n] | [1/Y/100, 000 I | % | [n] | [1/Y/100, 000 I | % | [n] | [1/Y/100, 000 I | % | [n] | [1/Y/100, 000 I | % | |||
| All (cardiac and non-cardiac) | 533 | 56,4 | 100,0 | 399 | 56,6 | 100,0 | 410 | 59,2 | 100,0 | 164 | 65,1 | 100,0 | 391 | 54,0 | 100,0 | 196 | 36,0 | 100,0 | 237 | 36,1 | 100,0 | < 0.001 | |
| any ROSC | 250 | 26,5 | 46,9 | 191 | 27,1 | 47,9 | 179 | 25,8 | 43,7 | 75 | 29,8 | 45,7 | 189 | 26,1 | 48,3 | 104 | 19,1 | 53,1 | 101 | 15,4 | 42,6 | < 0.001 | 0,32 |
| any ROSC CI 95% | 41,9/51,5 | 43,5/55,2 | 38,7/52,1 | 41,4/61,4 | 44,0/56,4 | 45,7/63,8 | 37,4/54,3 | ||||||||||||||||
| RACA Score | 41,8 | 39,7 | 42,4 | 45,5 | 44,7 | 42,4 | 37,1 | ||||||||||||||||
| difference significant | y | y | n | n | n | y | y | ||||||||||||||||
| admitted to hospital | 213 | 22,5 | 40,0 | 188 | 26,7 | 47,1 | 163 | 23,5 | 39,8 | 69 | 27,4 | 42,1 | 178 | 24,6 | 45,5 | 91 | 16,7 | 46,4 | 96 | 14,6 | 40,5 | < 0.001 | 0,17 |
| 24 hours survival | 141 | 14,9 | 26,5 | 121 | 17,2 | 30,3 | 109 | 15,7 | 26,6 | 40 | 15,9 | 24,4 | 59 | 8,1 | 15,1 | n.d. | 56 | 8,5 | 23,6 | < 0.001 | < 0.001 | ||
| discharged alive | n.d. | 56 | 8,0 | 13,8 | 68 | 9,8 | 16,6 | 27 | 10,7 | 16,5 | n.d. | n.d. | n.d. | 0,30 | 0,50 | ||||||||
| First rhythm VF/VT (all) | 141 | 14,9 | 26,5 | 105 | 14,9 | 26,3 | 99 | 14,3 | 24,1 | 55 | 21,8 | 33,5 | 119 | 16,4 | 30,4 | 78 | 14,3 | 39,8 | 64 | 9,8 | 27,0 | < 0.01 | < 0.01 |
| VF/VT (cardiac) | 125 | 13,2 | 23,5 | 94 | 13,3 | 23,6 | 79 | 11,4 | 19,3 | 44 | 17,5 | 26,8 | 95 | 13,1 | 24,3 | 63 | 11,6 | 32,1 | 57 | 8,7 | 24,1 | < 0.05 | < 0.05 |
| any ROSC | 88 | 9,3 | 70,4 | 68 | 9,6 | 72,3 | 53 | 7,6 | 67,1 | 33 | 13,1 | 75,0 | 70 | 9,7 | 73,7 | 47 | 8,6 | 74,6 | 34 | 5,2 | 59,6 | < 0.01 | 0,51 |
| admitted to hospital | 77 | 8,1 | 61,6 | 68 | 9,6 | 72,3 | 47 | 6,8 | 59,5 | 32 | 12,7 | 72,7 | 66 | 9,1 | 69,5 | 43 | 7,9 | 68,3 | 33 | 5,0 | 57,9 | < 0.01 | 0,28 |
| 24 hours survival | 58 | 6,1 | 46,4 | 52 | 7,4 | 55,3 | 38 | 5,5 | 48,1 | n.d. | 25 | 3,4 | 26,3 | 5 | 3,4 | 26,3 | 23 | 3,5 | 40,4 | < 0.001 | < 0.001 | ||
| Asystoly (cardiac) | 133 | 14,1 | 25,0 | 128 | 18,2 | 32,1 | 94 | 13,6 | 22,9 | 33 | 13,1 | 20,1 | 91 | 12,6 | 23,3 | 52 | 9,6 | 26,5 | 62 | 9,5 | 26,2 | < 0.001 | < 0.05 |
| any ROSC | 43 | 4,6 | 32,3 | 42 | 6,0 | 32,8 | 24 | 3,5 | 25,5 | 9 | 3,6 | 27,3 | 26 | 3,6 | 28,6 | 16 | 2,9 | 30,8 | 15 | 2,3 | 24,2 | < 0.05 | 0,82 |
| admitted to hospital | 31 | 3,3 | 23,3 | 42 | 6,0 | 32,8 | 22 | 3,2 | 23,4 | 8 | 3,2 | 24,2 | 23 | 3,2 | 25,3 | 11 | 2,0 | 21,2 | 13 | 2,0 | 21,0 | < 0.01 | 0,49 |
| 24 hours survival | 18 | 1,9 | 13,5 | 23 | 3,3 | 18,0 | 12 | 1,7 | 12,8 | n.d. | 9 | 1,2 | 9,9 | 1 | 0,2 | 1,9 | 6 | 0,9 | 9,7 | < 0.01 | 0,07 | ||
| PEA (cardiac) | 73 | 7,7 | 13,7 | 49 | 7,0 | 12,3 | 30 | 4,3 | 7,3 | 12 | 4,8 | 7,3 | 15 | 2,1 | 3,8 | 3 | 0,6 | 1,5 | 21 | 3,2 | 8,9 | < 0.001 | < 0.001 |
| any ROSC | 32 | 3,4 | 43,8 | 23 | 3,3 | 46,9 | 11 | 1,6 | 36,7 | 5 | 2,0 | 41,7 | 7 | 1,0 | 46,7 | 3 | 0,6 | 100,0 | 11 | 1,7 | 52,4 | < 0.001 | 0,92 |
| admitted to hospital | 26 | 2,8 | 35,6 | 22 | 3,1 | 44,9 | 11 | 1,6 | 36,7 | 3 | 1,2 | 25,0 | 6 | 0,8 | 40,0 | 3 | 0,6 | 100,0 | 11 | 1,7 | 52,4 | < 0.01 | 0,60 |
| 24 hours survival | 18 | 1,9 | 24,7 | 6 | 0,9 | 12,2 | 6 | 0,9 | 20,0 | n.d. | 2 | 0,3 | 13,3 | n.d. | 5 | 0,8 | 23,8 | < 0.05 | 0,48 | ||||
p-value (1/Y/100,000 I): Comparison of the number of patients in one year per 100,000 Inhabitants of the centre; p-value (%): Comparison of the number of grouped patients regarding to the number of all treated patients;RACA Score: predicted
value of ROSC; VF = ventricular heart flutter; VT = ventricular tachycardia; PEA = pulseless electrical activity; p-value calculated by t-test or chi square test (significant = p < 0.05)
Survival rate differences between the centres were minor. Any ROSC was achieved in 42.6% of patients (Tübingen) and 53.1% of patients (Rendsburg-Eckernförde) (P = 0.32). Between 39.8% (Gütersloh) and 47.1% (Göppingen) of patients were admitted to hospital with ROSC (P = 0.17). Survival after 24 hours varied from 15.1% (Münster) to 30.3% (Göppingen) (P < 0.001). Discharge rates were between 13.8% and 16.6% (P = 0.50).
Quality of EMS care should not be measured only by using the 'percentage admission to hospital rate', because a selection bias might influence this rate in both directions. Therefore, in this study, the quality of preclinical care was additionally assessed according to the 'admission rate relative to the population served'.
Regarding CPR incidence, the EMS systems differed significantly. In two of the seven systems, the CPR incidence was below 38/100,000 population/year, and in these two systems, the rate of patients admitted to hospital was significantly lower than in the other centres (P < 0.001). In Tübingen and Rendsburg-Eckernförde, only 14.6 and 16.7 patients/100,000 population/year, respectively, were admitted to hospital following cardiac arrest. In the other five systems, between 22.5 (Bonn) and 27.4 (Marburg) patients/100,000 population/year survived the event to hospital admission (P < 0.001).
The quality of EMS care may further be assessed on the basis of the real ROSC rate and the predicted ROSC rate (RACA score [33]). The predicted ROSC rate was, on average, 41.9%, with a minimum of 37.1% in Tübingen and a maximum of 45.5% in Marburg. In all seven centres, the ROSC rate was higher than predicted by the RACA score. In four centres (Bonn, Göppingen, Rendsburg-Eckernförde and Tübingen), the ROSC rate was significantly higher than predicted.
An outcome analysis of subgroups according to the initially recorded cardiac rhythm may further specify the comparison of the centres, eliminating an important influencing factor. For example, among the subgroup of patients with a collapse of cardiac origin found in a shockable initial rhythm (23.9% of all patients), the admission rate was 65.7% and thus considerably higher than that of patients with asystole (25.3%) or pulseless electrical activity (40.4%) (incidence = 7.9 vs 3.3 vs 1.8/100,000 inhabitants/year, respectively). Differences between EMS systems can generally also be found in the subgroup analysis. Following collapse of cardiac origin and shockable rhythm, 72.7% were admitted in Marburg, but only 57.9% were admitted in Tübingen (P = 0.28). In Göppingen, 55.3% of the patients were alive 24 hours after the event, but only 26.3% were still alive in Münster and Rendsburg-Eckernförde each (P < 0.001).
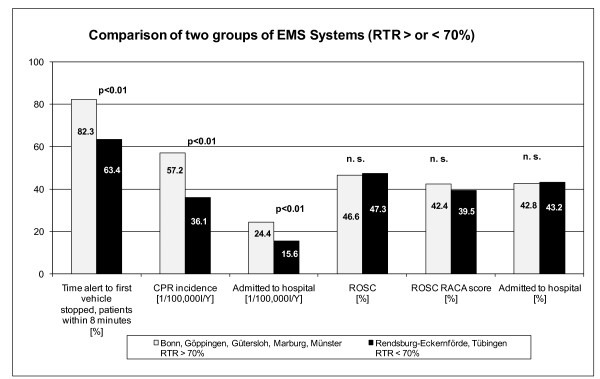
Impact of response time reliability on CPR incidence and CPR success
To analyse the impact of RTR on CPR incidence and success, we contrasted the performance of the EMS systems of Bonn, Göppingen, Gütersloh, Marburg and Münster (group 1; RTR > 70%), where > 70% of patients are reached by the first unit within 8 minutes, with the EMS systems of Tübingen and Rendsburg-Eckernförde (group 2; RTR < 70%), where < 70% of the patients are reached within 8 minutes (RTR > 70% = 82.3% vs RTR < 70% = 63.4%, OR = 2.676 (99% CI = 1.93 to 3.711); P < 0.01) (Table 4 and Figure 2).
Table 4.
Comparison of two groups of EMS systems grouped by response time reliability achieved or not achieved in 70% of dispatches
| Provider | Bonn, Göppingen, Gütersloh, Marburg and Münster RTR > 70% | Rendsburg-Eckernförde and Tübingen RTR < 70% | P-values, ORs and 95% CIs | All seven providers | All other centres in the German Resuscitation Registry |
|---|---|---|---|---|---|
| Person-years | 3,317,400 | 1,201,052 | 4,518,452 | 1 Jan 2006 to 31 Dec 2009 | |
| All patients (cardiac + noncardiac) (n) | 1,897 | 433 | 2,330 | 4,624 | |
| Time from alert until first vehicle stopped (n) | |||||
| Patients with time | 1,860 | 347 | |||
| Patients within 8 minutes | 1,530 | 220 | |||
| Statistics | 82.3% | 63.4% | P < 0.01 | 79.3% | 73.6% |
| OR = 2.676 | |||||
| 99% CI = 1.93 to 3.711 | |||||
| CPR incidence (1/100,000 inhabitants/year) | 57.2% | 36.1% | P < 0.01 | 51.6% | n.d. |
| OR = 1.586 | |||||
| 99% CI = 1.383 to 1.819 | |||||
| ROSC (n) | 884 | 205 | |||
| ROSC (1/100,000 inhabitants/year) | 26.6% | 17.1% | P < 0.01 | 24.1% | n.d. |
| OR = 1.561 | |||||
| 99% CI = 1.279 to 1.906 | |||||
| Admitted to hospital (n) | 811 | 187 | |||
| Admitted to hospital (1/100,000 inhabitants/year) | 24.4% | 15.6% | P < 0.01 | 22.1% | n.d. |
| OR = 1.57 | |||||
| 99% CI = 1.274 to 1.935 | |||||
| ROSC RACA (n) | 804 | 171 | |||
| ROSC RACA | 42.4% | 39.5% | P = n.s. | 41.9% | n.d. |
| OR = 1.127 | |||||
| 95% CI = 0.911 to 1.395 | |||||
| ROSC | 46.6% | 47.3% | P = n.s. | 46.7% | 37.9% |
| OR = 0.971 | |||||
| 95% CI = 0.787 to 1.196 | |||||
| Admitted to hospital | 42.75% | 43.19% | P = n.s. | 42.83% | 32.7% |
| OR = 0.982 | |||||
| 95% CI = 0.878 to 1.116 | |||||
| RTR > 70%: ROSC vs RACA ROSC | 884/1,897 vs 804/1,897 | P < 0.01 | |||
| OR = 1.186 | |||||
| 99% CI = 1.002 to 1.404 | |||||
| RTR < 70%: ROSC vs RACA ROSC | 205/433 vs 171/433 | P < 0.05 | |||
| OR = 1.378 | |||||
| 95% CI = 1.052 to 1.804 |
CPR = cardiopulmonary resuscitation; n.d. = not determined; n.s. = not significant; RACA = return of spontaneous circulation after cardiac arrest; ROSC = return of spontaneous circulation; RTR = response time reliability. RTR is the rate of the first vehicle's arriving at the scene within 8 minutes (%). The response time interval was defined as the time from when a call was received in the dispatch centre until the arrival of the first ambulance at the scene. It was calculated using the time stamps of dispatch technology. Odds ratios, confidence intervals and χ2 tests were used for statistical analysis.
Figure 2.
Comparison of two groups of emergency medical service (EMS) systems grouped by response time reliability (RTR) achieved or not achieved in 70% of dispatches. RTR calculates the rate of first vehicle arriving within 8 minutes (%). Response time interval was defined from call reception in the dispatch centre until arrival of the first ambulance on scene and was calculated using the time stamps of dispatch technology. Odds ratios, confidence intervals and χ2 tests were used for statistical analysis. n.s. = not significant; CPR = cardiopulmonary resuscitation; RACA = return of spontaneous circulation after cardiac arrest; ROSC = return of spontaneous circulation.
In faster EMS systems with RTR > 70% (group 1), CPR incidence was significantly higher than in group 2 (CPR incidence (1/100,000 inhabitants/year) RTR > 70% = 57.2 vs RTR < 70% = 36.1, OR = 1.586 (99% CI = 1.383 to 1.819); P < 0.01) and more patients with ROSC were admitted to hospital (admitted to hospital (1/100,000 inhabitants/year) RTR > 70% = 24.4 vs RTR < 70% = 15.6, OR = 1.57 (99% CI = 1.274 to 1.935); P < 0.01). However, these two groups did not differ in 'percentage CPR success rates' (ROSC RTR > 70% = 46.6% vs RTR < 70% = 47.3%, OR = 0.971 (95% CI = 0.787 to 1.196); P = n.s.) (admitted to hospital RTR > 70% = 42.8% vs RTR < 70% = 43.2%, OR = 0.982 (95% CI = 0.878 to 1.116); P = n.s.). On the basis of using the multivariate RACA score to predict outcome, the two groups did not differ, but ROSC rates were higher than predicted in both groups (ROSC RACA RTR > 70% = 42.4% vs RTR < 70% = 39.5%, OR = 1.127 (95% CI = 0.911 to 1.395); P = n.s.).
Discussion
This study demonstrates for the first time a relation between the RTR, CPR incidence and resuscitation success rate for sudden cardiac arrest in Germany (Tables 3 and 4 and Figures 1 and 2). Our study clearly shows that the EMS systems with the longest response intervals have the lowest CPR incidence and CPR success rates, calculated per 1/100,000 inhabitants/year.
It is noteworthy that the 'percentage ROSC rate' and the 'admission to hospital rate', which are usually used to compare EMS systems, did not differ between both groups and thus seem to be weak indicators of the performance of EMS systems (Figure 2). In addition, the RTR seems to be a particularly important influencing factor. On the one hand, it affects the frequency of resuscitation attempts by an EMS system; on the other hand, it affects the resuscitation success related to the population served. In this study, the time interval from when the call is received until the arrival of the first ambulance at the scene was used to calculate, consistently for all centres, the RTR in resuscitation missions. The rate of patients reached within 8 minutes of the call was determined. This time interval corresponds largely to the national standard for response times in the United Kingdom, whereas in Germany, owing to different state laws regarding EMS, there is no nationwide standard. According to the heterogeneous legal requirements, the best RTRs were found in the most densely populated areas (Bonn and Münster), with 90% of the patients reached by the first ambulance within 8 minutes after the call. It is remarkable that in the very rural EMS system of Marburg, which has the second lowest population density, 79.8% of the patients were reached within 8 minutes after the call. This success is explained by high number of EMS vehicles and unit-hours in Marburg. In contrast to the EMS system of Rendsburg-Eckernförde, which also provides service in a rural area, Marburg reached 108.3 unit-hours/km2 service area, which is more than twice the provided unit-hours in Rendsburg-Eckernförde.
A high RTR regularly shortens the interval without treatment, so professional resuscitation attempts may be initiated earlier. In other regions, this leads to improved admission and survival rates as described by Hollenberg et al. [34], who compared the resuscitation success rates of Gothenburg and Stockholm (admission rates 30% vs 16%). Vukmir et al. [35] showed that more patients survive when it is possible to initiate resuscitation attempts within 8 minutes of the call or not (56 vs 32 patients). Our study supports the demand for a standardised response time interval for the arriving first vehicle and RTR > 70%, meaning that > 70% of the patients should regularly be reached within 8 minutes after the call.
Because regional state laws in Germany differ, response intervals are defined differently and healthcare funds provide financial means to reach only the respective standards. Thus, a German EMS system can realise a response interval standard only within a given legislative and financial framework. To compare the quality of EMS care under these conditions, further indicators must be considered. The survival rates following cardiac arrest are, in addition to other factors, influenced by techniques and quality of BLS [36,37], ALS [38-41] and postresuscitation care [30,42-44]. Therefore, in our study, the quality of EMS care was analysed by additionally assessing 'percentage survival rates', that is, ROSC and admission to hospital, of the total population and subgroups defined beforehand, as well as in comparison to a predictive value (RACA score) [33]. Table 4 shows that both groups of EMS systems could achieve higher ROSC rates than predicted by the RACA score, but did not differ regarding the 'percentage survival rates'. This means that (1) all seven EMS centres studies belong to the the best performing systems in the GRR, and (2) a lower CPR incidence does not lead to a positive selection of 'good risks'. The first statement is additionally supported by a comparison with the admission rates from the GRR, because all seven centres performed better than the other centres participating in the GRR, with, on average, 42.8% vs 32.7% of patients being admitted to hospital.
There might be various reasons for the superior resuscitation results of the seven participating EMS systems that we studied. It is well-known that both a collapse in public and a witnessed collapse improve the chances of surviving an OHCA [9]. However, in this respect, there were no differences between the seven centres participating in our study and the total GRR participants (witnessed = 60.2% vs 61.6%, collapse in public = 18.3% vs 18.2%). The results cannot be explained by the rates of bystander CPR, which were 18.8% in the seven participating centres in our study and 18.5% in the total GRR. It is remarkable that in Germany bystanders too rarely initiate CPR before EMS arrival, even when they witness the collapse. The positive influence of bystander CPR on survival rate has been demonstrated frequently [45-47]. Previous studies have shown similar setups in German and European systems [9,48]. One reason for the low rate of bystander CPR in Germany may be that > 70% of the events occur at home and that it is usually elderly people who are affected and live alone or with an elderly partner who is unable to perform BLS spontaneously. As a consequence, the approach of telephone-guided CPR should urgently be intensified in the EMS systems that we studied and in Germany generally.
The comparatively high survival rates in the seven analysed centres in our study may be explained by the higher rate of patients found in a shockable rhythm (rate of VF/VT = 28.4% vs 23.1% in the entire GRR; P < 0.001). Therapeutic hypothermia following ROSC was induced in 46.2% of the patients in the seven centres in our study, but only in 13.7% of all patients in the GRR (P < 0.001).
Special efforts are made in all seven centres studied regarding CPR training in general, particularly BLS CPR. This is reflected by the fact that, in three centres, intensive training is provided in the use of special supportive devices, which are used extensively. Bonn has established LDB CPR use [37,49], ACD-CPR is applied in connection with an impedance valve in Göppingen [50] and, after intensive training and continuous scientific evaluation, a CPR feedback system is regularly used in Münster [51,52]. In this study, we found no evidence that using these mechanical or feedback devices increases CPR success. However, as the data derived from the remaining participating centres show, excellent results are possible by applying only committed manual CPR.
Limitations
The relationship between RTR, CPR incidence and hospital admission rate in this study including seven EMS systems is obvious, but needs to be examined in more detail on the basis of a greater number of included EMS systems.
Conclusions
The results of this study demonstrate that, with regard to the level of EMS systems, the faster ones more often initiate CPR and increase the number of patients admitted to hospital alive. Furthermore, we have shown that with the use of very different approaches, all EMS systems that adhere to and provide intensive training based on the 2005 ERC guidelines, superior and, on the basis of international comparisons, excellent success rates following resuscitation can be achieved. The data derived from the three EMS systems in our study (Göppingen, Gütersloh and Marburg) in which the discharge rates based on 1/100,000 inhabitants/year could be calculated, with results between 8.0 and 10.7/100,000 inhabitants/year, take a top position in Europe (Table 3). Despite these internationally compared excellent results, some potential improvements could be identified for the centres. (1) Change of location of ambulance and emergency physician's stations, implementation of global positioning systems (GPSs) and computer-aided dispatch systems should be used to improve the rate of calls reached within the standardised response time interval. (2) The time interval between EMS arrival and onset of CPR should be shortened. (3) Intensive, required training in BLS should be implemented, especially when mechanical devices are used. (4) Special CPR training for elderly citizens should be required. (5) Awareness should be raised among, and training should be provided to, the general population regarding the importance of bystander CPR. (6) A structured interview of emergency calls and telephone-guided CPR instructions by the dispatch centre should be implemented. (7) Consistent use of a standard operating procedure concerning treatment of hypothermia, starting in the preclinical phase, should be implemented.
Key messages
• Later arrival of the first EMS unit at the scene decreases the incidence of CPR, the number of patients who reach ROSC and who can be admitted to hospital with ROSC. Therefore, the RTR, that is, the rate of the first vehicle's arriving within 8 minutes after the call is received at the dispatch centre, should be > 70%.
• Changes in the location of ambulance and emergency physician stations, as well as the use of GPS devices and computer-aided dispatching systems, should be implemented to improve the rate of OHCA victims reached within the standardised response time interval.
• Telephone-guided CPR should be introduced to increase the rate of bystander CPR.
• BLS training should be required for use among the general public and special groups of elderly people to reduce no-flow time until EMS arrives to take over CPR.
• For comparison and benchmarking of EMS systems, not only 'percentage survival rates' but also the number of patients with CPR attempted and/or ROSC and/or admitted to hospital, referring to 1/100,000 inhabitants/year of the respective EMS systems, should be calculated.
Abbreviations
ACD: active compression decompression; ALS: advanced cardiac life support; BLS: basic life support; CPR: cardiopulmonary resuscitation; DGAI: German Society for Anaesthesiology and Intensive Care Medicine (Deutsche Gesellschaft für Anästhesiologie und Intensivmedizin); ECG: electrocardiogram; EMS: emergency medical service; ERC: European Resuscitation Council; EU: European Union; EuReCa: European Registry of Cardiac Arrest; GRR: German Resuscitation Registry; ILCOR: International Liaison Committee on Resuscitation; LDB: load-distributing band; NA: Notarzt (emergency physician); NEF: Notarzteinsatzfahrzeug (emergency vehicle staffed with emergency physicians); OHCA: out-of-hospital cardiac arrest; RA: Rettungsassistent (paramedic); RACA: return of spontaneous circulation after cardiac arrest; ROSC: return of spontaneous circulation; RS: Rettungssanitäter (emergency medical technician); RTR: response time reliability; RTW: Rettungswagen (emergency vehicle staffed with paramedics but no doctors); VF: ventricular heart flutter; VT: ventricular tachycardia.
Competing interests
JTG, JW, MM and MF are members of the steering committee of the German Resuscitation Registry. All authors declare that they have no competing interests.
Authors' contributions
JN and JTG made substantial contributions to the study's conception and design and drafted the manuscript. MF conceived the study, participated in its design and coordination and helped to draft the manuscript. JCS, MB, UH, JW, AB, GH, BS, HF, CK, RL and MM were responsible for data collection and quality control in the participating centres and helped to revise the manuscript. JB, BB, PM, JS and MF were involved in the final critical revision of the manuscript. All authors read and approved the final manuscript.
Contributor Information
Jürgen Neukamm, Email: juergen.neukamm@gmx.de.
Jan-Thorsten Gräsner, Email: graesner@anaesthesie.uni-kiel.de.
Jens-Christian Schewe, Email: jens-christian.schewe@ukb.uni-bonn.de.
Martin Breil, Email: Martin.Breil@ukb.uni-bonn.de.
Jan Bahr, Email: jan.bahr@med.uni-goettingen.de.
Ulrich Heister, Email: Ulli.Heister@Bonn.de.
Jan Wnent, Email: wnent@reanimationsregister.de.
Andreas Bohn, Email: BohnA@stadt-muenster.de.
Gilbert Heller, Email: heller@anaesthesie.uni-kiel.de.
Bernd Strickmann, Email: AELRD@gt-net.de.
Hans Fischer, Email: hans.fischer@med.uni-tuebingen.de.
Clemens Kill, Email: killc@staff.uni-marburg.de.
Martin Messelken, Email: M.Messelken@kae.de.
Berthold Bein, Email: bein@anaesthesie.uni-kiel.de.
Roman Lukas, Email: lukasr@lukasr.de.
Patrick Meybohm, Email: meybohm@anaesthesie.uni-kiel.de.
Jens Scholz, Email: jens.scholz@uksh.de.
Matthias Fischer, Email: Matthias.Fischer@kae.de.
Acknowledgements
The authors are indebted to all active participants of the GRR who registered patients. Furthermore, the authors thank all professional emergency physicians and emergency medical technicians involved in prehospital emergency medical care and intensive care at the emergency physician-staffed EMS systems.
References
- Berdowski J, Berg RA, Tijssen JGP, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81:1479–1487. doi: 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- Gräsner JT, Herlitz J, Koster RW, Rosell-Ortiz F, Stamatakis L, Bossaert L. Quality management in resuscitation: towards a European Cardiac Arrest Registry (EuReCa) Resuscitation. 2011;82:989–994. doi: 10.1016/j.resuscitation.2011.02.047. [DOI] [PubMed] [Google Scholar]
- Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104:2158–2163. doi: 10.1161/hc4301.098254. [DOI] [PubMed] [Google Scholar]
- Löwel H, Meisinger C, Heier M, Hörmann A, Kuch B, Gostomzyk J, Koenig W. [Sex specific trends of sudden cardiac death and acute myocardial infarction: results of the population-based KORA/MONICA-Augsburg Register 1985 to 1998] [in German] Dtsch Med Wochenschr. 2002;127:2311–2316. doi: 10.1055/s-2002-35181. [DOI] [PubMed] [Google Scholar]
- Willich SN, Löwel H, Lewis M, Hörmann A, Arntz HR, Keil U. Weekly variation of acute myocardial infarction: increased Monday risk in the working population. Circulation. 1994;90:87–93. doi: 10.1161/01.cir.90.1.87. [DOI] [PubMed] [Google Scholar]
- Atwood C, Eisenberg MS, Herlitz J, Rea TD. Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation. 2005;67:75–80. doi: 10.1016/j.resuscitation.2005.03.021. [DOI] [PubMed] [Google Scholar]
- Messelken M, Kehrberger E, Dirks B, Fischer M. The quality of emergency medical care in Baden-Württemberg (Germany): four years in focus. Dtsch Arztebl Int. 2010;107:523–530. doi: 10.3238/arztebl.2010.0523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer M, Krep H, Wierich D, Heister U, Hoeft A, Edwards S, Castrillo-Riesgo LG, Krafft T. Comparison of the emergency medical services systems of Birmingham and Bonn: process efficacy and cost effectiveness. Anasthesiol Intensivmed Notfallmed Schmerzther. 2003;38:630–642. doi: 10.1055/s-2003-42507. [DOI] [PubMed] [Google Scholar]
- Fischer M, Fischer NJ, Schüttler J. One-year survival after out-of-hospital cardiac arrest in Bonn city: outcome report according to the 'Utstein style'. Resuscitation. 1997;33:233–243. doi: 10.1016/S0300-9572(96)01022-2. [DOI] [PubMed] [Google Scholar]
- Lippert FK, Raffay V, Georgiou M, Steen PA, Bossaert L. European Resuscitation Council Guidelines for Resuscitation 2010 Section 10. The ethics of resuscitation and end-of-life decisions. Resuscitation. 2010;81:1445–1451. doi: 10.1016/j.resuscitation.2010.08.013. [DOI] [PubMed] [Google Scholar]
- Soar J, Monsieurs KG, Ballance JH, Barelli A, Biarent D, Greif R, Handley AJ, Lockey AS, Richmond S, Ringsted C, Wyllie JP, Nolan JP, Perkins GD. European Resuscitation Council Guidelines for Resuscitation 2010 Section 9. Principles of education in resuscitation. Resuscitation. 2010;81:1434–1444. doi: 10.1016/j.resuscitation.2010.08.014. [DOI] [PubMed] [Google Scholar]
- Richmond S, Wyllie J. European Resuscitation Council Guidelines for Resuscitation 2010 Section 7. Resuscitation of babies at birth. Resuscitation. 2010;81:1389–1399. doi: 10.1016/j.resuscitation.2010.08.018. [DOI] [PubMed] [Google Scholar]
- Biarent D, Bingham R, Eich C, López-Herce J, Maconochie I, Rodríguez-Nuñez A, Rajka T, Zideman D. European Resuscitation Council Guidelines for Resuscitation 2010 Section 6. Paediatric life support. Resuscitation. 2010;81:1364–1388. doi: 10.1016/j.resuscitation.2010.08.012. [DOI] [PubMed] [Google Scholar]
- Arntz HR, Bossaert LL, Danchin N, Nikolaou NI. European Resuscitation Council Guidelines for Resuscitation 2010 Section 5. Initial management of acute coronary syndromes. Resuscitation. 2010;81:1353–1363. doi: 10.1016/j.resuscitation.2010.08.016. [DOI] [PubMed] [Google Scholar]
- Deakin CD, Nolan JP, Soar J, Sunde K, Koster RW, Smith GB, Perkins GD. European Resuscitation Council Guidelines for Resuscitation 2010 Section 4. Adult advanced life support. Resuscitation. 2010;81:1305–1352. doi: 10.1016/j.resuscitation.2010.08.017. [DOI] [PubMed] [Google Scholar]
- Deakin CD, Nolan JP, Sunde K, Koster RW. European Resuscitation Council Guidelines for Resuscitation 2010 Section 3. Electrical therapies: automated external defibrillators, defibrillation, cardioversion and pacing. Resuscitation. 2010;81:1293–1304. doi: 10.1016/j.resuscitation.2010.08.008. [DOI] [PubMed] [Google Scholar]
- Nolan JP, Soar J, Zideman DA, Biarent D, Bossaert LL, Deakin C, Koster RW, Wyllie J, Böttiger B. the ERC Guidelines Writing Group. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation. 2010;81:1219–1276. doi: 10.1016/j.resuscitation.2010.08.021. [DOI] [PubMed] [Google Scholar]
- Ghuysen A, Collas D, Stipulante S, Donneau AF, Hartstein G, Hosmans T, Vantroyen B, D'Orio V. Dispatcher-assisted telephone cardiopulmonary resuscitation using a French-language compression-only protocol in volunteers with or without prior life support training: a randomized trial. Resuscitation. 2011;82:57–63. doi: 10.1016/j.resuscitation.2010.09.014. [DOI] [PubMed] [Google Scholar]
- Hüpfl M, Selig HF, Nagele P. Chest-compression-only versus standard cardiopulmonary resuscitation: a meta-analysis. Lancet. 2010;376:1552–1557. doi: 10.1016/S0140-6736(10)61454-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobrow BJ, Spaite DW, Berg RA, Stolz U, Sanders AB, Kern KB, Vadeboncoeur TF, Clark LL, Gallagher JV, Stapczynski JS, LoVecchio F, Mullins TJ, Humble WO, Ewy GA. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA. 2010;304:1447–1454. doi: 10.1001/jama.2010.1392. [DOI] [PubMed] [Google Scholar]
- Szumita PM, Baroletti S, Avery KR, Massaro AF, Hou PC, Pierce CD, Henderson GV, Stone PH, Scirica BM. Implementation of a Hospital-wide Protocol for Induced Hypothermia Following Successfully Resuscitated Cardiac Arrest. Crit Pathw Cardiol. 2010;9:216–220. doi: 10.1097/HPC.0b013e3181f8228d. [DOI] [PubMed] [Google Scholar]
- Gaieski DF, Band RA, Abella BS, Neumar RW, Fuchs BD, Kolansky DM, Merchant RM, Carr BG, Becker LB, Maguire C, Klair A, Hylton J, Goyal M. Early goal-directed hemodynamic optimization combined with therapeutic hypothermia in comatose survivors of out-of-hospital cardiac arrest. Resuscitation. 2009;80:418–424. doi: 10.1016/j.resuscitation.2008.12.015. [DOI] [PubMed] [Google Scholar]
- Friberg H, Nielsen N. Hypothermia after cardiac arrest: lessons learned from national registries. J Neurotrauma. 2009;26:365–369. doi: 10.1089/neu.2008.0637. [DOI] [PubMed] [Google Scholar]
- Nolan JP, Neumar RW, Adrie C, Aibiki M, Berg RA, Böttiger BW, Callaway C, Clark RS, Geocadin RG, Jauch EC, Kern KB, Laurent I, Longstreth WT, Merchant RM, Morley P, Morrison LJ, Nadkarni V, Peberdy MA, Rivers EP, Rodríguez-Nuñez A, Sellke FW, Spaulding C, Sunde K, Hoek TV. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A scientific statement from the International Liaison Committee on Resuscitation; the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; the Council on Stroke (Part 1) Int Emerg Nurs. 2009;17:203–225. doi: 10.1016/j.ienj.2009.01.001. [DOI] [PubMed] [Google Scholar]
- Duncan JM, Meaney P, Simpson P, Berg RA, Nadkarni V, Schexnayder S. Vasopressin for in-hospital pediatric cardiac arrest: results from the American Heart Association National Registry of Cardiopulmonary Resuscitation. Pediatr Crit Care Med. 2009;10:191–195. doi: 10.1097/PCC.0b013e31819a36f2. [DOI] [PubMed] [Google Scholar]
- Mentzelopoulos SD, Zakynthinos SG, Tzoufi M, Katsios N, Papastylianou A, Gkisioti S, Stathopoulos A, Kollintza A, Stamataki E, Roussos C. Vasopressin, epinephrine, and corticosteroids for in-hospital cardiac arrest. Arch Intern Med. 2009;169:15–24. doi: 10.1001/archinternmed.2008.509. [DOI] [PubMed] [Google Scholar]
- Gueugniaud PY, David JS, Chanzy E, Hubert H, Dubien PY, Mauriaucourt P, Bragança C, Billères X, Clotteau-Lambert MP, Fuster P, Thiercelin D, Debaty G, Ricard-Hibon A, Roux P, Espesson C, Querellou E, Ducros L, Ecollan P, Halbout L, Savary D, Guillaumée F, Maupoint R, Capelle P, Bracq C, Dreyfus P, Nouguier P, Gache A, Meurisse C, Boulanger B, Lae C. et al. Vasopressin and epinephrine vs epinephrine alone in cardiopulmonary resuscitation. N Engl J Med. 2008;359:21–30. doi: 10.1056/NEJMoa0706873. [DOI] [PubMed] [Google Scholar]
- Herlitz J, Bahr J, Fischer M, Kuisma M, Lexow K, Thorgeirsson G. Resuscitation in Europe: a tale of five European regions. Resuscitation. 1999;41:121–131. doi: 10.1016/S0300-9572(99)00045-3. [DOI] [PubMed] [Google Scholar]
- Holler NG, Mantoni T, Nielsen SL, Lippert F, Rasmussen LS. Long-term survival after out-of-hospital cardiac arrest. Resuscitation. 2007;75:23–28. doi: 10.1016/j.resuscitation.2007.03.015. [DOI] [PubMed] [Google Scholar]
- Gräsner JT, Meybohm P, Caliebe A, Böttiger BW, Wnent J, Messelken M, Jantzen T, Zeng T, Strickmann B, Bohn A, Fischer H, Scholz J, Fischer M. German Resuscitation Registry Study Group. Postresuscitation care with mild therapeutic hypothermia and coronary intervention after out-of-hospital cardiopulmonary resuscitation: a prospective registry analysis. Crit Care. 2011;15:R61. doi: 10.1186/cc10035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gräsner JT, Meybohm P, Fischer M, Bein B, Wnent J, Franz R, Zander J, Lemke H, Bahr J, Jantzen T, Messelken M, Dörges V, Böttiger BW, Scholz J. A national resuscitation registry of out-of-hospital cardiac arrest in Germany: a pilot study. Resuscitation. 2009;80:199–203. doi: 10.1016/j.resuscitation.2008.10.008. [DOI] [PubMed] [Google Scholar]
- Gräsner JT, Messelken M, Fischer M, Jantzen T, Bahr J, Böttiger BW, Dörges V, Franz R, Gries A, Krieter H, Schüttler J, Wnent J, Zander JF, Scholz J. [The DGAI CPR registry: the datasets "hospital care" and "long-term process"] [in German] Anasthesiol Intensivmed Notfallmed Schmerzther. 2008;43:706–709. doi: 10.1055/s-0028-1102989. [DOI] [PubMed] [Google Scholar]
- Gräsner JT, Meybohm P, Lefering R, Wnent J, Bahr J, Messelken M, Jantzen T, Franz R, Scholz J, Schleppers A, Böttiger BW, Bein B, Fischer M. German Resuscitation Registry Study Group. ROSC after cardiac arrest: the RACA score to predict outcome after out-of-hospital cardiac arrest. Eur Heart J. 2011;32:1649–1656. doi: 10.1093/eurheartj/ehr107. [DOI] [PubMed] [Google Scholar]
- Hollenberg J, Bång A, Lindqvist J, Herlitz J, Nordlander R, Svensson L, Rosenqvist M. Difference in survival after out-of-hospital cardiac arrest between the two largest cities in Sweden: a matter of time? J Intern Med. 2005;257:247–254. doi: 10.1111/j.1365-2796.2004.01447.x. [DOI] [PubMed] [Google Scholar]
- Vukmir RB. Survival from prehospital cardiac arrest is critically dependent upon response time. Resuscitation. 2006;69:229–234. doi: 10.1016/j.resuscitation.2005.08.014. [DOI] [PubMed] [Google Scholar]
- Kramer-Johansen J, Myklebust H, Wik L, Fellows B, Svensson L, Sørebø H, Steen PA. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: a prospective interventional study. Resuscitation. 2006;71:283–292. doi: 10.1016/j.resuscitation.2006.05.011. [DOI] [PubMed] [Google Scholar]
- Ong ME, Ornato JP, Edwards DP, Dhindsa HS, Best AM, Ines CS, Hickey S, Clark B, Williams DC, Powell RG, Overton JL, Peberdy MA. Use of an automated, load-distributing band chest compression device for out-of-hospital cardiac arrest resuscitation. JAMA. 2006;295:2629–2637. doi: 10.1001/jama.295.22.2629. [DOI] [PubMed] [Google Scholar]
- Fischer M, Kamp J, Garcia-Castrillo Riesgo L, Robertson-Steel I, Overton J, Ziemann A, Krafft T. the EED Group. Comparing emergency medical service systems: a project of the European Emergency Data (EED) Project. Resuscitation. 2011;82:285–293. doi: 10.1016/j.resuscitation.2010.11.001. [DOI] [PubMed] [Google Scholar]
- Olasveengen TM, Sunde K, Brunborg C, Thowsen J, Steen PA, Wik L. Intravenous drug administration during out-of-hospital cardiac arrest: a randomized trial. JAMA. 2009;302:2222–2229. doi: 10.1001/jama.2009.1729. [DOI] [PubMed] [Google Scholar]
- Lund-Kordahl I, Olasveengen TM, Lorem T, Samdal M, Wik L, Sunde K. Improving outcome after out-of-hospital cardiac arrest by strengthening weak links of the local Chain of Survival: quality of advanced life support and post-resuscitation care. Resuscitation. 2010;81:422–426. doi: 10.1016/j.resuscitation.2009.12.020. [DOI] [PubMed] [Google Scholar]
- Dickinson ET, Schneider RM, Verdile VP. The impact of prehospital physicians on out-of-hospital nonasystolic cardiac arrest. Prehosp Emerg Care. 1997;1:132–135. doi: 10.1080/10903129708958805. [DOI] [PubMed] [Google Scholar]
- Sunde K, Pytte M, Jacobsen D, Mangschau A, Jensen LP, Smedsrud C, Draegni T, Steen PA. Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation. 2007;73:29–39. doi: 10.1016/j.resuscitation.2006.08.016. [DOI] [PubMed] [Google Scholar]
- Holzer M, Müllner M, Sterz F, Robak O, Kliegel A, Losert H, Sodeck G, Uray T, Zeiner A, Laggner AN. Efficacy and safety of endovascular cooling after cardiac arrest: cohort study and Bayesian approach. Stroke. 2006;37:1792–1797. doi: 10.1161/01.STR.0000227265.52763.16. [DOI] [PubMed] [Google Scholar]
- Holzer M, Bernard SA, Hachimi-Idrissi S, Roine RO, Sterz F, Müllner M. Collaborative Group on Induced Hypothermia for Neuroprotection After Cardiac Arrest. Hypothermia for neuroprotection after cardiac arrest: systematic review and individual patient data meta-analysis. Crit Care Med. 2005;33:414–418. doi: 10.1097/01.CCM.0000153410.87750.53. [DOI] [PubMed] [Google Scholar]
- Kitamura T, Iwami T, Kawamura T, Nagao K, Tanaka H, Hiraide A. Bystander-initiated rescue breathing for out-of-hospital cardiac arrests of noncardiac origin. Circulation. 2010;122:293–299. doi: 10.1161/CIRCULATIONAHA.109.926816. [DOI] [PubMed] [Google Scholar]
- Nordberg P, Hollenberg J, Herlitz J, Rosenqvist M, Svensson L. Aspects on the increase in bystander CPR in Sweden and its association with outcome. Resuscitation. 2009;80:329–333. doi: 10.1016/j.resuscitation.2008.11.013. [DOI] [PubMed] [Google Scholar]
- Sekimoto M, Noguchi Y, Rahman M, Hira K, Fukui M, Enzan K, Inaba H, Fukui T. Estimating the effect of bystander-initiated cardiopulmonary resuscitation in Japan. Resuscitation. 2001;50:153–160. doi: 10.1016/S0300-9572(01)00330-6. [DOI] [PubMed] [Google Scholar]
- Steinmetz J, Barnung S, Nielsen SL, Risom M, Rasmussen LS. Improved survival after an out-of-hospital cardiac arrest using new guidelines. Acta Anaesthesiol Scand. 2008;52:908–913. doi: 10.1111/j.1399-6576.2008.01657.x. [DOI] [PubMed] [Google Scholar]
- Krep H, Mamier M, Breil M, Heister U, Fischer M, Hoeft A. Out-of-hospital cardiopulmonary resuscitation with the AutoPulse system: a prospective observational study with a new load-distributing band chest compression device. Resuscitation. 2007;73:86–95. doi: 10.1016/j.resuscitation.2006.08.027. [DOI] [PubMed] [Google Scholar]
- Wolcke BB, Mauer DK, Schoefmann MF, Teichmann H, Provo TA, Lindner KH, Dick WF, Aeppli D, Lurie KG. Comparison of standard cardiopulmonary resuscitation versus the combination of active compression-decompression cardiopulmonary resuscitation and an inspiratory impedance threshold device for out-of-hospital cardiac arrest. Circulation. 2003;108:2201–2205. doi: 10.1161/01.CIR.0000095787.99180.B5. [DOI] [PubMed] [Google Scholar]
- Yeung J, Meeks R, Edelson D, Gao F, Soar J, Perkins GD. The use of CPR feedback/prompt devices during training and CPR performance: a systematic review. Resuscitation. 2009;80:743–751. doi: 10.1016/j.resuscitation.2009.04.012. [DOI] [PubMed] [Google Scholar]
- Abella BS, Edelson DP, Kim S, Retzer E, Myklebust H, Barry AM, O'Hearn N, Hoek TL, Becker LB. CPR quality improvement during in-hospital cardiac arrest using a real-time audiovisual feedback system. Resuscitation. 2007;73:54–61. doi: 10.1016/j.resuscitation.2006.10.027. [DOI] [PubMed] [Google Scholar]