Abstract
OBJECTIVES
To examine the change in use of “High Risk Medications for the Elderly,” as defined by the National Committee on Quality Assurance's Healthcare Effectiveness Data and Information Set (HEDIS) quality measure (HEDIS HRME), by older outpatient veterans over a three year time period. We also sought to identify risk factors for HEDIS HRME exposure overall, and among the most commonly used drug classes.
DESIGN
Longitudinal retrospective database analysis.
SETTING
Outpatient clinics within the Department of Veterans Affairs (VA).
PARTICIPANTS
Veterans aged 65 by October 1, 2003 and who received VA care at least once each year until September 30, 2006.
MEASUREMENTS
Rates of use of HEDIS HRME overall and by specific drug classes each year FY04-06.
RESULTS
In our cohort of 1,567,467, high risk medication exposure was reduced from 13.1% to 12.3% between FY04-06 (p<0.01). High risk antihistamines (e.g., diphenhydramine), opioid analgesics (e.g., propoxyphene), skeletal muscle relaxants (e.g., cyclobenzaprine), psychotropics (e.g., long half-life benzodiazepines), endocrine (e.g., estrogen), and cardiac medications (e.g., short-acting nifedipine) had modest but statistically significant (p<0.01) reductions (range -3.8% to -16.0%); nitrofurantoin demonstrated a statistically significant increase (+36.5%; p<0.01). Overall HEDIS HRME exposure was more likely for men, Hispanics, those receiving more medications, psychiatric comorbidity, and those without prior geriatric care. Exposure was lower for individuals exempt from copayment. Similar associations were seen between ethnicity, polypharmacy, psychiatric comorbidity, access to care factors and use of individual HEDIS HRME classes.
CONCLUSION
HEDIS HRME drug exposure decreased slightly in an integrated health care system. Risk factors for exposure were not consistent across drug groups.Future studies should examine whether interventions to further reduce HEDIS HRME use results in an improvement in health outcomes.
Keywords: Inappropriate prescribing, quality of care, aged, pharmacoepidemiology
INTRODUCTION
Explicit criteria for Potentially Inappropriate Prescribing in the Elderly (PIPE) defined as those medications rated by an expert panel whose risks outweigh their potential benefit in older adults were first developed by Dr. Mark Beers in 1991 and subsequently updated in 1997 and 2003. Numerous studies have shown the rates of PIPE based on the Beers criteria over the past decade to be between 20-30% in elderly outpatients.1-8 Several recent studies have identified small but significant reductions in PIPE as defined by different versions of the Beers criteria.9,10 For example, Carey and colleagues found a 3.9% reduction in PIPE (2003 Beers Criteria) between 1996 and 2005 in the United Kingdom despite a trend for an increase in the number of prescriptions overall during this time.11
In 2006 the National Committee on Quality Assurance (NCQA) developed a Healthcare Effectiveness Data and Information Set (HEDIS) quality measure to examine use of High Risk Medications in the Elderly (HRME) developed by an expert panel and based in part on the most recent version of the Beers Criteria.12,13 The HEDIS HRME measure included some, but not all of the drugs included on the Beers criteria, retaining only those for which there was consensus that 1) they should be avoided and 2) outcomes were considered high severity. This more refined measure is now used to benchmark the quality of medication management among older patients enrolled in Medicare and other managed care plans, and thus is of interest to the Department of Veterans Affairs, Veterans Health Administration (VA).
We previously reported using VA data from October 1, 1999-Spetmeber 30, 2000, that the overall one-year prevalence of HEDIS HRME exposure in older veteran outpatients was19.6%.14 To the best of our knowledge, the only published studies examining longitudinal use of HEDIS HRME as defined by this HEDIS quality measure have been reports by the NCQA.15
The objective of the current study was to examine the change in HEDIS HRME exposure among older veteran outpatients between 2004 and 2006, and to examine risk factors for HEDIS HRME exposure. Given that the foundation for the HEDIS HRME measure existed for over a decade before the refinement of the measure itself, we hypothesized that reductions in the rates of HEDIS HRME drug use overall and within specific drug classes should have been evident by the mid 2000s. Moreover, we hypothesized that risk factors for HEDIS HRME would be similar to those reported in previous studies using the Beers criteria and that they would be consistent across the major drug groups that comprise the HEDIS HRME measure.
METHODS
Study Design, Setting, and Sample
A longitudinal retrospective data analysis study was conducted using data from all Department of Veterans Affairs outpatient clinics. The sample consisted of Veterans aged 65 by October 1, 2003 (beginning Fiscal Year 2004 [FY04]) and who received VA care at least once each year between FY03-FY06. In order to examine change in a consistent sample over time, individuals who received sporadic VA care or who died during this period were not included in the analysis. This study was approved by Institutional Review Boards at three sites (University of Texas Health Science Center at San Antonio, Hines VA, and Bedford VA).
Data Sources
We obtained national VA inpatient, outpatient and pharmacy data from fiscal year 2003 (FY03; October 1, 2002 to September 30, 2003) through FY06 (October 1, 2005-September 30, 2006) for individuals who were 65 or older at the beginning of FY04. We created a merged database using information from the VA National Patient Care Database (NPCD) records and all outpatient pharmacy prescription data from the VA Pharmacy Benefits Management database. Records were merged using an encrypted identifier that is consistent for each person across VA data sets.
Measures
Exposure: High Risk Medications for the Elderly
We identified use of any of the HEDIS HRME drugs using VA pharmacy data each year between FY04-06. We then created a measure of exposure for overarching groups of drugs based on the VA Medication class system (Table 1) (http://www.pbm.va.gov/natform/vaclass.xls).
Table 1.
High Risk Medications in the Elderly
| Drug Group | Drugs Included | Concerns Regarding Use |
|---|---|---|
| Amphetamines | Amphetamine/dextroamphetamine, benzphetamine, dexmethylphenidate, pemoline, dextroamphetamine diethylpropion, methamphetamine, methylphenidate, phendimetrazine, phentermine | Dependence, hypertension, angina and myocardial infarction. |
| Antibiotics | nitrofurantoin | Potential for renal impairment. Safer alternatives available. |
| Antihistamines | diphenhydramine hydroxyzine, promethazine, cyproheptadine, dexchlorpheniramine, tripelennamine | Confusion and sedation. Potent anticholinergic properties. |
| Cardiac Medications/ Vasodilators | dipyridamole (short acting) | May cause orthostatic hypotension. |
| nifedipine (short acting) | Potential for hypotension and constipation. | |
| isoxsuprine, ergot mesyloids | Lack of efficacy. | |
| Endocrine Drugs | estrogens chlorpropamide | Carcinogenic potential. Syndrome of inappropriate antidiuretic hormone secretion; hypoglycemia. |
| desiccated thyroid | Concerns about cardiac effects. Safer alternatives available. | |
| Gastrointestinal Antispasmodics | dicyclomine, hyoscyamine, propantheline, atropine belladonna, scopalamine trimethobenzamide | Highly anticholinergic with uncertain effectiveness. Poor efficacy; can cause extrapyramidal effects. |
| Non-steroidal Anti-inflammatory Drugs | ketorolac | Commonly causes asymptomatic GI pathologic conditions. |
| Opioid Pain Relievers | propoxyphene | Lack of efficacy; more adverse effects. |
| meperidine | Lack of efficacy. Confusion, falls, fractures, dependency. |
|
| pentazocine | Falls, fractures, confusion, dependency, withdrawal. | |
| Psychotropic Drugs | diazepam, chlordiazepoxide, flurazepam | Prolonged sedation and increase the risk of falls. |
| thioridazine, meprobamate | More CNS and extra-pyramidal adverse effects than others. | |
| barbiturates | Highly addictive; more adverse effects than others. | |
| Skeletal Muscle | methocarbamol, cyclobenzaprine, | Anticholinergic adverse |
| Relaxants | carisoprodol, chlorzoxazone, metaxalone, orphenadrine | effects, sedation, and weakness. Effectiveness at doses tolerated by the elderly is questionable. |
Independent Variables
We identified patient demographic characteristics (age, sex, race/ ethnicity) using data fields from VA administrative databases between FY03-FY06. With the exception of race, these demographic characteristics are well documented and complete in the medical record. Because the process of recording race changed in 2002, race data are more likely to be missing than other aspects of VA administrative data. Findings from our prior studies indicate that those with missing data were most often white and had low healthcare utilization and disease burden. For these demographic variables, we used a process in which we looked back in VA data for previous years and forward in the data in subsequent years to minimize missing data.
Health Status Variables
Health status variables in the analyses predicting HEDIS HRME exposure in FY06 include several measures of disease burden. As prior studies indicate that individuals with greater disease burden as defined by more medications, more physical comorbidities and psychiatric conditions are at increased risk for potentially inappropriate prescribing,7,16-18 we controlled for these variables. We first counted the number of unique medication classes each individual received during FY05. We also used ICD-9-CM codes (two outpatient or one inpatient) found in VA inpatient and outpatient data (FY03-05) to identify individuals with physical and psychiatric conditions using the Selim comorbidity indices that were developed to control for disease burden in research studies involving veterans.19,20 For physical conditions we counted the number of chronic disease states from 30 possible conditions included in the Selim Physical Comorbidity index. We also identified the following psychiatric conditions included in the Selim Psychiatric Comorbidity Index: schizophrenia, bipolar disorder, depressive disorder, post-traumatic stress disorder, substance use disorder, and anxiety disorders. Due to the highly skewed distribution we identified individuals with zero, one or two or more psychiatric conditions. These measures of comorbidity have been previously associated with mortality, measures of health status, and PIPE.14,21,22
Access to Care Variables
Access to care variables in our analyses included a measure of copayment exemption, measures of geriatric care and primary care utilization in FY05. Copayment exemption was measured using the VA priority group. VA priority groups are associated with physical or mental health status and illness severity as well as socioeconomic status. Veterans with a service-connected disability ≥50%, or individuals who were catastrophically disabled, very low income, or had specific war-related experiences generally receive a waiver for copayments associated with VA care.21,23
Because our prior work found that geriatric care at some point the year prior to assessment was associated with lower risk of exposure to drugs included in the Beers criteria, individuals who received care in geriatric outpatient clinics or inpatient geriatric evaluation and management in FY05 were identified as having prior geriatric care.24 Finally, because prior literature found that patients with many primary care visits the previous year were more likely to have an exposure to potentially inappropriate medications as measured by the Beers criteria, those with more frequent visits to primary care (5+ in a year) may be sicker, and thus at higher risk of HEDIS HRME exposure.16,17 Based on prior studies and the empirical distribution we classified patients as having 0-1, 2-4 or 5+ primary care visits.
Analysis
We first describe demographic and health status characteristics of the cohort. We then identified changes in exposure to HEDIS HRME overall and individual medication classes among older VA outpatients over the three year study period (FY04-06). We used Generalized Estimating Equations (GEE) analyses with a logit link (exchangeable working correlation) and applied it to five unique samples of 100,000 randomly selected patients to determine if changes over time in HEDIS HRME overall and drug classes were statistically significant. We used the averaged parameter estimates (change over time only) obtained from the five random samples and approximated standard errors for the entire population using the pooled standard errors.25 Statistical significance of these pooled estimates was examined using the Z-score threshold: ± 2.33 (-2.33 and 2.33 are 0.005 and 0.995 quantiles of the standard normal distribution). We then used logistic regression analyses to identify demographic, health status, and access to care factors associated with risk of HEDIS HRME exposure overall in 2006, and for the four most commonly used HEDIS HRME drug classes. All statistical analyses were performed using SAS® software (version 9; Cary, NC).
RESULTS
Of the 1,933,291 individuals who met age criteria in FY04, 1,567,467 received care between FY03-06 and were included in this study. The mean age of individuals in this cohort in 2004 was 74.4 (SD=5.8). Similar to other studies of older veterans, this cohort was primarily male (1,539,324; 98.2%) and white (1,060,366; 67.7%). Table 2 provides additional descriptive statistics for this cohort.
Table 2.
Characteristics of Longitudinal Cohort
| Characteristic | Overall (N=1,567,467) | No HEDIS HRME Exposure (N=1,374,016) | HEDIS HRME Exposure (N=193,451) | |
|---|---|---|---|---|
| Age (Mean SD) | 74.4 (5.8) | 76.5 (5.8) | 75.9 (5.8) | |
| Sex | Men | 1,539,324 (98.2) | 1,352,233 (98.4) | 187,091 (96.71) |
| Women | 28,143 (1.8) | 21,783 (1.6) | 6,360 (3.3) | |
| Race | White | 1,060,366 (67.7) | 919,575 (66.9) | 140,791 (72.8) |
| African American | 103,818 (6.6) | 87,261 (6.4) | 16,557 (8.6) | |
| Hispanic | 52,925 (3.4) | 43,913 (3.2) | 9,012 (4.7) | |
| Other | 19,719 (1.3) | 16,988 (1.2) | 2,731 (1.4) | |
| Missing | 330,639 (21.09) | 306,279 (22.3) | 24,360 (12.6) | |
| Unique Medications (Mean SD) | 6.4 (4.4) | 6.1 (4.1) | 9.2 (5.1) | |
| Selim Physical† (Mean, SD) | 2.5 (1.7) | 2.4 (1.6) | 3.1 (1.9) | |
| Selim Psychiatric‡ | 0 | 1,362,490 (86.9) | 1,212,466 (88.2) | 150,024(77.5) |
| 1 | 159,426 (10.2) | 127,866 (9.3) | 31,560 (16.3) | |
| ≥2 | 45,551 (2.9) | 33,684 (2.5) | 11,867 (6.1) | |
| Copay Status* | ||||
| Exempt | 953,467(60.8) | 805,186 (58.6) | 148,281 (76.7) | |
| Not Exempt | 613,810 (39.2) | 568,662 (41.4) | 45,148 (23.3) | |
| Geriatric Care in 2003 | 33,046 (2.11) | 29,020 (2.1)) | 4,026 (2.1) | |
| Yes | ||||
| No | 1,534,421 (97.9) | 1,344,996 (97.9) | X189,425 (97.9) | |
| Primary Care | ||||
| Utilization | ||||
| 0-1 Visits | 382,741 (24.4) | 352,852 (25.7) | 29,889 (15.5) | |
| 2-4 Visits | 892,662 (57.0) | 787,111 (57.3) | 105,551 (54.7) | |
| ≥5 Visits | 292,064 (18.6) | 234,053 (17.0) | 58,011 (30.0) | |
190 individuals had missing data for copayment status
HEDIS HRME: High Risk Medications for the Elderly defined by the Healthcare Effectiveness Data and Information Set quality measure.
Selim Physical Comorbidity Index
Selim Psychiatric Comorbidity Index
Longitudinal Change in HEDIS HRME Exposure
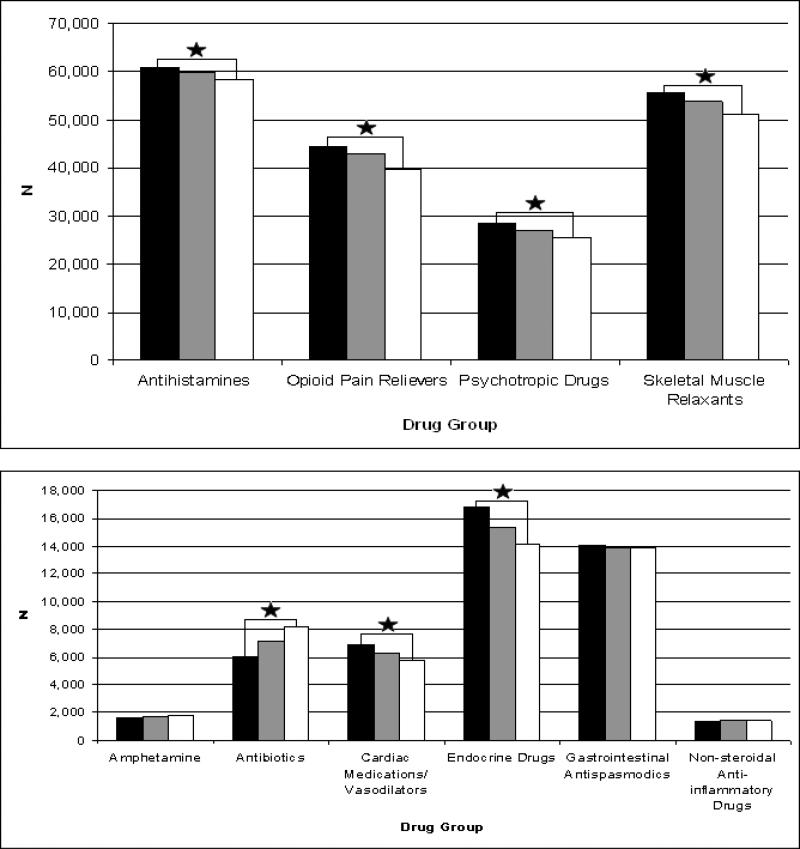
Overall, the rates of HEDIS HRME exposure decreased over the study period: FY04 (205,179; 13.1%), FY05 (200,326; 12.8%), FY06 (193,456; 12.3%). This represents an absolute difference of 0.8 and a relative difference of 6.1% between FY04 and FY06. Figure 1 shows changes in HEDIS HRME exposure by drug category over the study period. Most categories experienced small reductions in use between FY04 and FY06; however, antibiotics, amphetamines, and ketorolac, a nonsteroidal anti-inflammatory drug (NSAID), saw relative increases of 36.5%, 10.3%, and 8.0% respectively. Table 3 shows results of GEE analyses examining the statistical significance of HEDIS HRME over time in the 5 random samples of the population. Overall, exposure to HEDIS HRME was significantly lower in FY06 than FY04 (estimate -.07, standard error (SE) .004, Z score -15.59). There was no significant change in exposure for gastrointestinal antispasmodics, amphetamines or ketorolac, but there were statistically significant reductions in high risk opioid pain relievers (primarily propoxyphene), skeletal muscle relaxants, psychotropic drugs, endocrine drugs and cardiac/vasodilator medications. There was also a statistically significant increase in exposure to nitrofurantoin. Table 4 shows results of logistic regression models predicting HEDIS HRME exposure in FY06. Similar to our previous report using data from FY00, older individuals, African Americans (vs. whites), those required to make copayments, and those with previous geriatric care were significantly less likely to have HEDIS HRME exposure. Women, Hispanics, those with higher numbers of medications the prior year, psychiatric comorbidity or higher primary care utilization were significantly more likely to have HEDIS HRME exposure.
Figure 1.
Exposure to High Risk Medications in the Elderly (HRME) by Drug Group
Table 3.
Results of Pooled General Estimating Equations Assessing Change in Proportion of Exposure to Healthcare Effectiveness Data and Information Set (HEDIS) High Risk Medications in the Elderly (HRME) by Drug Category FY06 (vs. FY04)
| Drug Group | Estimate | Standard Error | Z Score |
|---|---|---|---|
| Any HEDIS HRME | -0.07 | 0.004 | -15.59 |
| Amphetamine | 0.10 | 0.045 | 2.09 |
| Antibiotics | 0.30 | 0.026 | 11.55 |
| Antihistamines | -0.04 | 0.008 | -4.40 |
| Cardiac Medications/ Vasodilators | -0.16 | 0.018 | -8.84 |
| Endocrine Drugs | -0.18 | 0.013 | -14.05 |
| Gastrointestinal Antispasmodics | -0.026 | 0.016 | -1.60 |
| Non-steroidal Anti-inflammatory Drugs | 0.03 | 0.064 | 0.49 |
| Opioid Pain Relievers | -0.13 | 0.009 | -13.92 |
| Psychotropic Drugs | -0.11 | 0.009 | -12.47 |
| Skeletal Muscle Relaxants | -0.08 | 0.009 | -9.19 |
Bold indicates significance at p < .01
Table 4.
Logistic Regression Analysis Predicting Exposure to High Risk Medications for the Elderly
| Variables | Overall HEDIS HRME OR (99% CI) | Antihistamines OR (99% CI) | Opioids OR (99% CI) | Psychotropics OR (99% CI) | Skeletal Muscle Relaxants OR (99% CI) |
|---|---|---|---|---|---|
| Demographic Characteristics | |||||
| Age | 0.98 (0.98-0.98) | 0.99 (0.99-0.99) | 1.00 (1.00-1.00) | 0.98 (0.98-0.98) | 0.94 (0.94-0.94) |
| Women (vs. Men) | 1.95 (1.87-2.02) | 1.16 (1.11-1.20) | 1.29 (1.17-1.41) | 1.23 (1.10-1.36) | 1.44 (1.33-1.56) |
| Race: (vs. White) | |||||
| African American | 0.96 (0.93-0.98) | 1.16 (1.11-1.20) | 0.73 (0.69-0.77) | 0.75 (0.70-0.80) | 1.13 (1.09-1.18) |
| Hispanic | 1.08 (1.05-1.12) | 1.34 (1.28-1.41) | 0.32 (0.28-0.35) | 1.10 (1.02-1.19) | 1.41 (1.34-1.48) |
| Other | 0.97 (0.92-1.03) | 1.18 (1.08-1.28) | 0.69 (0.60-0.78) | 0.97 (0.85-1.12) | 0.98 (0.89-1.08) |
| Missing | 0.77 (0.75-0.78) | 0.67 (0.65-0.70) | 0.66 (0.64-0.69) | 0.88 (0.84-0.93) | 0.78 (0.75-0.81) |
| Not Married (vs. Married) | 1.00 (0.99-1.02) | 1.14 (1.12-1.17) | 0.92 (0.90-0.95) | 0.88 (0.85-0.91) | 0.97 (0.95-1.00) |
| Health Status Factors | |||||
| Unique Medications | 1.13 (1.12-1.13) | 1.12 (1.11-1.12) | 1.10 (1.09-1.10) | 1.12 (1.12-1.13) | 1.10 (1.10-1.10) |
| Selim Physical† | 0.99 (0.98-0.99) | 0.96 (0.95-0.97) | 1.07 (1.06-1.08) | 0.89 (0.88-0.90) | 1.01 (1.00-1.02) |
| Selim Mental‡ (vs.0) | |||||
| 1 | 1.38 (1.35-1.40) | 1.35 (1.31-1.40) | 1.03 (0.99-1.08) | 2.79 (2.68-2.91) | 1.06 (1.03-1.10) |
| 2 or more | 1.51 (1.47-1.56) | 1.53 (1.46-1.60) | 0.92 (0.86-0.99) | 3.75 (3.54-3.96) | 1.06 (1.00-1.12) |
| Access to Care Factors | |||||
| Copay Status: Not | 0.61 (0.60-0.62) | 0.49 (0.47-0.50) | 0.61 (0.59-0.63) | 0.56 (0.54-0.59) | 0.55 (0.53-0.56) |
| Exempt | |||||
| Geriatric Care: Yes | 0.73 (0.70-0.77) | 0.71 (0.66-0.77) | 0.689(0.63-0.76) | 0.65 (0.57-0.73) | 0.65 (0.59-0.71) |
| Primary Care (vs. 0-1 Visits) | |||||
| 2-4 Visits | 1.10 (1.08-1.12) | 1.10 (1.07-1.14) | 1.20 (1.16-1.25) | 1.00 (0.96-1.05) | 1.24 (1.20-1.29) |
| 5+ Visits | 1.12 (1.09-1.15) | 1.20 (1.15-1.25) | 0.99 (0.95-1.04) | 0.87 (0.82-0.92) | 1.35 (1.30-1.41) |
HEDIS HRME: High Risk Medications for the Elderly defined by the Healthcare Effectiveness Data and Information Set (HEDIS) quality measure.
Selim Physical Comorbidity Index
Selim Psychiatric Comorbidity Index
Examination of the four types of most commonly used HEDIS HRME suggested some consistency across medication types, but also some variation with regard to predictors of HEDIS HRME exposure (Table 4). The effect of age, gender, number of medications, copayment requirement, and prior geriatric care were consistent across all drug groups. For race, African Americans and Hispanics were less likely than whites to have opioid HEDIS HRME exposure and more likely to have antihistamine and skeletal muscle relaxant HEDIS HRME exposure. African Americans were also significantly less likely than whites to have psychotropic HEDIS HRME exposure; while Hispanics were significantly more likely to have such exposure. Individuals who were not married were more likely to have antihistamine and opioid HEDIS HRME exposure and less likely to have psychotropic or skeletal muscle relaxant HEDIS HRME exposure. The effect of high primary care utilization was associated with increased likelihood of HEDIS HRME exposure with the exception of psychotropics, where the effect was non-significant for those with two to four visits and significantly increased for those with five or more visits. Finally, psychiatric comorbidity was not significantly associated with exposure to opioids or musculoskeletal relaxants.
DISCUSSION
Findings from this study suggest that small, but statistically significant reductions in exposure to HRME overall defined by the HEDIS criteria occurred between 2004 and 2006 for older VA patients. While the reductions in overall exposure were relatively small during this time period (13.1% in FY04 to 12.3% in FY06), exposure is markedly reduced compared to our previous assessment of 19.6% in FY00. This is quite similar to the rate of 12.9% reported by Albert and colleagues from a previous national sample of retirees from one company in 2003-2005.26 The rates of exposure in this current study were considerably lower than those reported by the National Committee on Quality Assurance for 2006 among Medicare enrollees, where 23.1% of individuals meeting criteria for the denominator in 2006 had one or more HEDIS HRME exposure.15 VA's leadership in geriatric care, the active role of pharmacists in VA, and VA formulary management may have contributed to the reduction. VA created its One-National Formulary in 2002 by freezing formularies at the facility and regional level, then creating a uniform formulary which resulted in excluding drugs that had previously been on a number of regional formularies such as propoxyphene.
Examination of change over time by individual drugs/classes revealed some reduction in most drug classes, stability in some others, and increases in nitrofurantoin. Reductions in use of skeletal muscle relaxants, psychotropic drugs, and opioid pain relievers is notable as recent studies have demonstrated that the use of these medications increase the risk of falls and fractures in older adults.27-29
One possible explanation for the increase in nitrofurantoin use is related to increasing resistance to common urinary tract pathogens such as e-coli with common antibiotics (e.g., ciprofloxacin trimethoprim/sulfamethoxazole). One invitro study found that nitrofurantoin was effective in killing e-coli isolates in 98.1% of those with trimethoprim/sulfamethoxazole resistance and 89.6% of those with ciprofloxacin resistance.30 Unfortunately, invitro testing does not translate to nitrofurantoin being effective in older adults. The use nitrofurantoin, a primarily renally cleared medication, should be avoided in those with estimated creatinine clearances less than 60ml/min as insufficient concentrations reach the bladder to be capable to kill bacteria such as e-coli.31,32 A recent study of veterans residing in a VA community living center found that this agent was in the top four suboptimally prescribed medications.33 Of concern is an increased risk for serious adverse drug events with nitrofurantoin that include chronic, sub-acute, or acute pulmonary hypersensitivity reactions and peripheral neuropathy.
This study also adds to our understanding of risk factors for potentially inappropriate prescribing. Prior studies have either examined a single drug such as propoxyphene or potentially inappropriate drugs in the Beers or HEDIS criteria as a single entity.7,14-18,34,35 Neither the aforementioned Albert nor the NCQA studies examined risk factors for the use of high risk medications.15,26 Consistent with our prior report and other studies examining exposure to potentially inappropriate medications, we found that Whites, women, and those with more medications were more likely to be exposed. Examination of the four most commonly prescribed HEDIS HRME groups suggests that findings from studies of HEDIS HRME as a whole provide insufficient insight into this problem. In particular, the effects of race and psychiatric comorbidity and primary care utilization depend upon the type of potentially inappropriate medication.
With regard to race, African Americans were less likely to have exposure to suboptimal opioid and psychotropic medications than were whites, and Hispanics were also significantly less likely than whites to have exposure to opioid medications. The finding for African Americans is consistent with literature finding lower use of psychotropic medications and analgesics in blacks compared to whites.36-38 The finding for Hispanics is less clear, in part because many previous studies have not distinguished between blacks and Hispanics, but rather evaluated them as “nonwhites”.
It is interesting to note that those with multiple psychiatric comorbidities had a lower risk of being prescribed high risk opioids (e.g. propoxyphene). This finding may result from clinicians being less likely to prescribe opioids for pain in patients receiving psychotropic medications for psychiatric comorbidities due to concern of that total CNS medication burden (e.g., opioids, benzodiazepines, antidepressants, antipsychotics) increase the risk of falls in older adults.39
There are a number of potential limitations that should be noted
First, restriction of our assessment to individuals who received VA care between FY03-06 may lead to selection bias. Although this was necessary in order to understand change in a consistent population of patients, this may bias the results since individuals who are sicker and die during this 3 year period are not represented in the findings. However, examination of the entire population revealed similar rates of exposure and trends overall and for HEDIS HRME drug groups (range 14.1% in FY04 to 12.6% in FY06) and predictors of exposure. Second, our assessment was restricted to medications received within the VA. It is possible that some HEDIS HRME were purchased outside the VA and thus our assessment may be conservative. One potential problem is with medications that can be purchased over the counter (OTC) such as diphenhydramine. Substantial variation in the relationship of copayment status on HEDIS HRME exposure for antihistamines would support the idea that reduced risk for exposure among those with required copayments was differentially affected by OTC medications. While small variation did exist, the direction and magnitude of the copayment variable was similar across drug classes. A second issue regarding use of medications received from the VA is that our findings may be affected by implementation of Medicare Part D in January, 2006.40 Because we did not see a sudden, marked decrease in the average number of prescriptions per patient or marked decreases in exposure between 2005-2006 (Table 2), it is unlikely that our findings for FY06 were affected substantially. Moreover, our assessment occurred using data from a timeframe before the implementation of the HEDIS HRME measure. Because the Beers criteria from which the HEDIS HRME measure was derived has been in existence in various forms for nearly a decade, the time period examined for this assessment is not unreasonable. Moreover, this study provides a foundation for subsequent study of change in exposure by chronicling the years up to and including the first year of HEDIS HRME implementation. We cannot rule out residual confounding due to potential important factors for which information was not available (e.g., smoking) and HEDIS HRME. Because this study provides information on change in prescribing on a national sample of older primarily male VA patients, it does not reflect prescribing in non-VA settings. Finally, since propoxyphene was removed from the market, we expect that rates of HEDIS HRME exposure will be significantly reduced nationally. This would follow a consistent trend in the VA where rates were reduced considerably due to formulary restrictions. However, since opioids rank third among the most common high risk drug classes, high risk medication exposure continues to be of concern.
CONCLUSION
Our study found a small decrease in HEDIS HRME exposure between FY04 and FY06. These rates of exposure were lower in the VA than in 2006 Medicare data. Comparison of our findings between those of our earlier study14 suggests that exposure in the VA has been reduced substantially between 2000 and 2006, but that only small changes occurred between 2004-2006. Moreover we found variation in risk factors for different groups of HEDIS HRME drugs. Future studies should examine the impact of these reductions on overall health outcomes, as well as measure the effects by drug class as variation in outcomes may also be evident, depending on the medications and the conditions they treat.
Figure 1.
Trends in Use of High Risk Medication Classes in the Elderly: 2004-2006 Key
ACKNOWLEDGMENTS
This study was supported by a VA Health Services Research grant (IIR-06–062, Dr. Pugh PI). Dr Hanlon is supported by National Institute of Aging grants (R01AG027017, P30AG024827, T32 AG021885, K07AG033174, R01AG034056), a National Institute of Mental Health grant (R34 MH082682), a National Institute of Nursing Research grant (R01NR010135), and an Agency for Healthcare Research and Quality grant (R01HS017695). We acknowledge the contributions of Jeffrey Tabares and Ranjani Davalath in assisting with manuscript preparation. The authors acknowledge and appreciate support from the South Texas Veterans Healthcare System/Audie L. Murphy Division and the VERDICT research program. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Sponsor's Role: VA Health Services Research and Development played no role in the design, methods, subject recruitment, data collections, analysis and preparation of paper.
Footnotes
Author Contributions: Indicate authors’ role in study concept and design, acquisition of subjects and/or data, analysis and interpretation of data, and preparation of manuscript.
Mary Jo V. Pugh, PhD, concept and design, acquisition of data, analysis and interpretation of data and preparation of the manuscript.
Dan R. Berlowitz, MD, interpretation of data and preparation of the manuscript.
Todd Semla PharmD, interpretation of data and preparation of the manuscript.
Muriel Burk, PharmD, interpretation of data and preparation of the manuscript.
Megan E. Amuan, MPH, acquisition of data, analysis of data and preparation of the manuscript.
John R. Downs, interpretation of data and preparation of the manuscript.
Chen-Pin Wang, PhD, analytic design, analysis and interpretation of data and preparation of the manuscript.
Chester B. Good, MD interpretation of data and preparation of the manuscript.
Joseph T. Hanlon PharmD, MS8, study design, interpretation of data and preparation of the manuscript.
| Elements of Financial/Personal Conflicts | MJP | JTH | CPW | AL | TS | MB | MEA | CBG | DRB | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | X | X | X | X | X | X | X | X | X | |||||||||
| Grants/Funds | X | x | X | X | X | X | X | X | X | |||||||||
| Honoraria | X | X | X | X | X | X | X | X | X | |||||||||
| Speaker Forum | X | X | X | X | X | X | X | X | X | |||||||||
| Consultant | X | X | X | X | X | X | X | X | X | |||||||||
| Stocks | X | X | X | X | X | X | X | X | X | |||||||||
| Royalties | X | X | X | X | X | X | X | X | X | |||||||||
| Expert Testimony | X | X | X | X | X | X | X | X | X | |||||||||
| Board Member | X | X | X | X | X | X | X | X | X | |||||||||
| Patents | X | X | X | X | X | X | X | X | X | |||||||||
| Personal Relationship | X | X | X | X | X | X | X | X | X | |||||||||
REFERENCES
- 1.Fick DM, Waller JL, Maclean JR, et al. Potentially inappropriate medication use in a Medicare managed care population with higher costs and utilization. J Manag Care Pharm. 2001;7:407–413. [Google Scholar]
- 2.Zhan C, Correa-de-Araujo R, Bierman AS, et al. Suboptimal prescribing in elderly outpatients: potentially harmful drug-drug and drug-disease combinations. J Am Geriatr Soc. 2005;53:262–267. doi: 10.1111/j.1532-5415.2005.53112.x. [DOI] [PubMed] [Google Scholar]
- 3.Blalock SJ, Byrd JE, Hansen RA, et al. Factors associated with potentially inappropriate drug utilization in a sample of rural community-dwelling older adults. Am J Geriatr Pharmacother. 2005;3:168–179. doi: 10.1016/s1543-5946(05)80023-6. [DOI] [PubMed] [Google Scholar]
- 4.Cannon KT, Choi MM, Zuniga MA. Potentially inappropriate medication use in elderly patients receiving home health care: a retrospective data analysis. Am J Geriatr Pharmacother. 2006;4:134–143. doi: 10.1016/j.amjopharm.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Barnett MJ, Perry PJ, Langstaff JD, et al. Comparison of rates of potentially inappropriate medication use according to the Zhan criteria for VA versus private sector medicare HMOs. J Manag Care Pharm. 2006;12:362–370. doi: 10.18553/jmcp.2006.12.5.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roughead EE, Anderson B, Gilbert AL. Potentially inappropriate prescribing among Australian veterans and war widows/widowers. Intern Med J. 2007;37:402–405. doi: 10.1111/j.1445-5994.2007.01316.x. [DOI] [PubMed] [Google Scholar]
- 7.Pugh MJ, Fincke BG, Bierman A, et al. Potentially inappropriate prescribing in elderly veterans: are we using the wrong drug, wrong dose, or wrong duration? J Am Geriatr Soc. 2005;53:1282–1289. doi: 10.1111/j.1532-5415.2005.53402.x. [DOI] [PubMed] [Google Scholar]
- 8.Shrout PE, Yager TJ. Reliability and validity of screening scales: effect of reducing scale length. J Clin Epidemiol. 1989;42:69–78. doi: 10.1016/0895-4356(89)90027-9. [DOI] [PubMed] [Google Scholar]
- 9.Stuart BC, Kamal-Bahl SJ, Briesacher BA, et al. Trends in prescribing inappropriate drugs for the elderly between 1995 and 1999. Am J Geriatr Pharmacother. 2003;1:61–74. doi: 10.1016/s1543-5946(03)90002-x. [DOI] [PubMed] [Google Scholar]
- 10.Bongue B, Naudin F, Laroche ML, et al. Trends of the potentially inappropriate medication consumption over 10 years in older adults in the East of France. Pharmacoepidemiol Drug Saf. 2009;18:1125–1133. doi: 10.1002/pds.1762. [DOI] [PubMed] [Google Scholar]
- 11.Carey IM, De Wilde S, Harris T, et al. What factors predict potentially inappropriate primary care prescribing in older people? Analysis of UK Primary Care Patient Record database. Drugs Aging. 2008;25:693–706. doi: 10.2165/00002512-200825080-00006. [DOI] [PubMed] [Google Scholar]
- 12. [October 24, 2005];Use of High Risk Medications in the Elderly. National Committee on Quality Assurance (online) Available at http://www.ncqa.org/portals/0/hedisqm/HEDIS2008/Vol2/NDC/Table%20DAEA.doc.
- 13.Fick DM, Cooper JW, Wade WE, et al. Updating the Beers Criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. 2003;163:2716–2724. doi: 10.1001/archinte.163.22.2716. [DOI] [PubMed] [Google Scholar]
- 14.Pugh MJ, Hanlon JT, Zeber JE, et al. Assessing potentially inappropriate prescribing in the elderly Veterans Affairs population using the HEDIS 2006 quality measure. J Manag Care Pharm. 2006;12:537–545. doi: 10.18553/jmcp.2006.12.7.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. [August 6, 2010];The state of health care quality: value, variation and vulnerable populations 2009 . National Committee for Quality Assurance (online) Available at http://www.ncqa.org/Portals/0/Newsroom/SOHC/SOHC_2009.pdf.
- 16.Zhan C, Sangl J, Bierman AS, et al. Potentially inappropriate medication use in the community-dwelling elderly: findings from the 1996 Medical Expenditure Panel Survey. JAMA. 2001;286:2823–2829. doi: 10.1001/jama.286.22.2823. [DOI] [PubMed] [Google Scholar]
- 17.Hanlon JT, Fillenbaum GG, Schmader KE, et al. Inappropriate drug use among community dwelling elderly. Pharmacotherapy. 2000;20:575–582. doi: 10.1592/phco.20.6.575.35163. [DOI] [PubMed] [Google Scholar]
- 18.Goulding MR. Inappropriate medication prescribing for elderly ambulatory care patients. Arch Intern Med. 2004;164:305–312. doi: 10.1001/archinte.164.3.305. [DOI] [PubMed] [Google Scholar]
- 19.Selim AJ, Berlowitz DR, Ren XS, et al. The comorbidity index. In: Davies M, editor. Measuring and Managing Health Care Quality. Vol. 4. Aspen Publishers; New York: 2002. pp. 91–94. [Google Scholar]
- 20.Selim AJ, Fincke G, Ren XS, et al. Comorbidity assessments based on patient report: results from the Veterans Health Study. J Ambulatory Care Manage. 2004;27:281–295. doi: 10.1097/00004479-200407000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Pugh MJ, Copeland LA, Zeber JE, et al. The impact of epilepsy on health status among younger and older adults. Epilepsia. 2005;46:1820–1827. doi: 10.1111/j.1528-1167.2005.00291.x. [DOI] [PubMed] [Google Scholar]
- 22.Selim AJ, Kazis LE, Rogers W, et al. Risk-adjusted mortality as an indicator of outcomes: comparison of the medicare advantage program with the Veterans’ Health Administration. Med Care. 2006;44:359–365. doi: 10.1097/01.mlr.0000204119.27597.f1. [DOI] [PubMed] [Google Scholar]
- 23.Kazis LE, Miller DR, Clark J, et al. Health-related quality of life in patients served by the Department of Veterans Affairs. Arch Intern Med. 1998;158:626–632. doi: 10.1001/archinte.158.6.626. [DOI] [PubMed] [Google Scholar]
- 24.Pugh MJ, Rosen AK, Montez-Rath M, et al. Potentially inappropriate prescribing for the elderly: effects of geriatric care at the patient and health care system level. Med Care. 2008;46:167–173. doi: 10.1097/MLR.0b013e318158aec2. [DOI] [PubMed] [Google Scholar]
- 25.Hanley JA, Negassa A, Edwardes MD, et al. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157:364–375. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- 26.Albert SM, Colombi A, Hanlon J. Potentially inappropriate medications and risk of hospitalization in retirees: analysis of a US retiree health claims database. Drugs Aging. 2010;27:407–415. doi: 10.2165/11315990-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169:1952–1960. doi: 10.1001/archinternmed.2009.357. [DOI] [PubMed] [Google Scholar]
- 28.Hartikainen S, Lonnroos E, Louhivuori K. Medication as a risk factor for falls: critical systematic review. J Gerontol A Biol Sci Med Sci. 2007;62:1172–1181. doi: 10.1093/gerona/62.10.1172. [DOI] [PubMed] [Google Scholar]
- 29.Golden AG, Ma Q, Nair V, et al. Risk for fractures with centrally acting muscle relaxants: an analysis of a national Medicare Advantage claims database. Ann Pharmacother. 2010;44:1369–1375. doi: 10.1345/aph.1P210. [DOI] [PubMed] [Google Scholar]
- 30.Karlowsky JA, Thornsberry C, Jones ME, et al. Susceptibility of antimicrobial-resistant urinary Escherichia coli isolates to fluoroquinolones and nitrofurantoin. Clin Infect Dis. 2003;36:183–187. doi: 10.1086/345754. [DOI] [PubMed] [Google Scholar]
- 31.Sachs J, Geer T, Noell P, et al. Effect of renal function on urinary recovery of orally administered nitrofurantoin. N Engl J Med. 1968;278:1032–1035. doi: 10.1056/NEJM196805092781902. [DOI] [PubMed] [Google Scholar]
- 32.Covvey JR, Lewis DA. Glimepiride-induced hypoglycemia with ciprofloxacin, metronidazole, and acute Kidney injury. Hosp Pharm. 2010;45:934–938. [Google Scholar]
- 33.Hanlon JT, Wang X, Handler SM, Weisbord S, Pugh MJ, Semla T, Stone RA, Aspinall SL. Potentially inappropriate prescribing of primarily renally cleared medications for older Veterans Affairs nursing home patients. JAMDA. doi: 10.1016/j.jamda.2010.04.008. published online October 4, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kamal-Bahl S, Stuart BC, Beers MH. National trends in and predictors of propoxyphene use in community-dwelling older adults. Am J Geriatr Pharmacother. 2005;3:186–195. doi: 10.1016/s1543-5946(05)80025-x. [DOI] [PubMed] [Google Scholar]
- 35.Simon SR, Chan KA, Soumerai SB, et al. Potentially inappropriate medication use by elderly persons in U.S. Health Maintenance Organizations, 2000-2001. J Am Geriatr Soc. 2005;53:227–232. doi: 10.1111/j.1532-5415.2005.53107.x. [DOI] [PubMed] [Google Scholar]
- 36.Hanlon JT, Fillenbaum GG, Studenski SA, et al. Factors associated with suboptimal analgesic use in community-dwelling elderly. Ann Pharmacother. 1996;30:739–744. doi: 10.1177/106002809603000706. [DOI] [PubMed] [Google Scholar]
- 37.Blazer D, Hybels C, Simonsick E, et al. Sedative, hypnotic, and antianxiety medication use in an aging cohort over ten years: a racial comparison. J Am Geriatr Soc. 2000;48:1073–1079. doi: 10.1111/j.1532-5415.2000.tb04782.x. [DOI] [PubMed] [Google Scholar]
- 38.Hanlon JT, Boudreau RM, Roumani YF, et al. Number and dosage of central nervous system medications on recurrent falls in community elders: the Health, Aging and Body Composition study. J Gerontol A Biol Sci Med Sci. 2009;64:492–498. doi: 10.1093/gerona/gln043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. [October 16, 1909];Resources on the Medicare Prescription Drug Benefit. Kaiser Family Foundation (online) Available at http://www.kff.org/medicare/rxdrugbenefit.cfm.