Men and women are alike in many ways. However, there are important biological and behavioural differences between the two genders. They affect manifestation, epidemiology and pathophysiology of many widespread diseases and the approach to health care. Despite our knowledge of these crucial differences, there is little gender-specific health care; the prevention, management and therapeutic treatment of many common diseases does not reflect the most obvious and most important risk factors for the patient: sex and gender. This omission is holding back more efficient health care, as gender-based prevention measures or therapies are probably more effective than the usual ‘one-size-fits all’ approach and would benefit patients of both genders. Addressing gender in health and health care therefore requires new approaches at many levels, from training medical personal to clinical medicine, epidemiology and drug development.
…the prevention, management and therapeutic treatment of many common diseases does not reflect the most obvious and most important risk factors for the patient: sex and gender
To discuss and address properly the differences in health and health care between men and women, it is necessary to distinguish between sex and gender and their respective effects on health. Sex differences are based on biological factors. These include reproductive function, concentrations of sexual hormones, the expression of genes on X and Y chromosomes and their effects and the higher percentage of body fat in women. By contrast, gender is associated with behaviour, lifestyle and life experience. It determines access to health care, use of the health care system and the behavioural attitudes of medical personnel. Typical gender differences in health care include differences in the use of preventive measures, the prescription of drugs, health insurance reimbursement and referral for or acceptance of particular surgical therapies such as pacemaker implantation or heart transplantation.
Gender medicine must consider the needs of both sexes
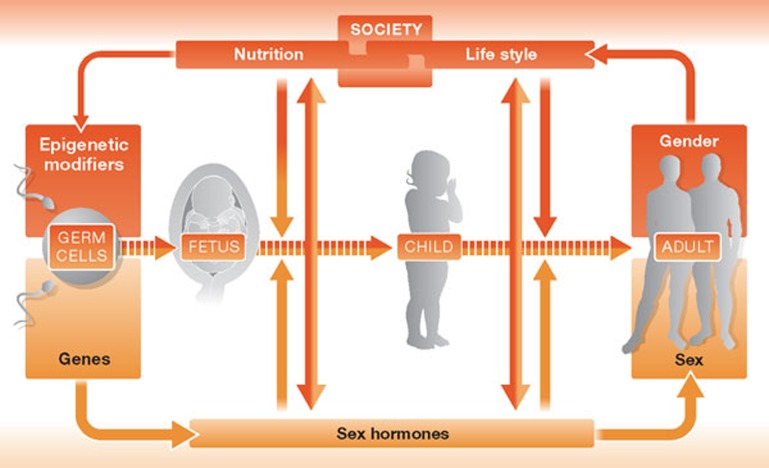
In practice, however, it is often not easy to separate the influence of sex and gender. On the one hand, sex influences health by modifying behaviour: testosterone, for instance, causes aggressive behaviour associated with risk-seeking and neglecting personal health. On the other hand, gender-behaviour can modify biological factors and thereby health: exposure to stress, environmental toxins, poor nutrition or lifestyle choices can induce genomic and epigenetic modifications in adults, children and even the developing fetus. These modifications and their physiological effects are different in women and men, as DNA repair and epigenetic mechanisms are modified by sex hormones (Fig 1). Thus, medical hypotheses need to take into account the effects of both sex and gender. Gender medicine therefore aims to include biological and socio-cultural dimensions, and their effects on women and men, to improve health and health care.
Figure 1. Complex interdependency of sex and gender in the human.
As such, gender-sensitive medicine is not the same as considering the specific needs of women in health care—such as during pregnancy or during menopause–and might even be contradictory. Gender medicine must consider the needs of both sexes. This might require giving greater attention to women where specific data on women are lacking, and greater attention to men where specific data on men are lacking. For example, more data on men are needed in regard to osteoporosis and depression, whilst more data on women are urgently needed in the cardiovascular area.
Indeed, because sex and gender affect a wide range of physiological functions, they have an impact on a wide range of diseases including those of the cardiovascular, pulmonary and autoimmune systems, as well as diseases involving gastroenterology, hepatology, nephrology, endocrinology, haematology and neurology; they also influence pharmacokinetics and pharmacodynamics [1]. These differences are reflected in the scientific literature: more than 10,000 articles deal with sex and gender differences in clinical medicine, epidemiology, pathophysiology, clinical manifestations, outcomes and management (Sidebar A, Table 1).
Sidebar A | Sex differences in disease management.
Women with myocardial infarction receive less guideline-based diagnosis and less-invasive treatment than men [3].
Women with heart failure receive fewer guideline-based diagnostic procedures and treatments, and fewer implantations and heart transplantations. Nevertheless women have a better outcome than men [54].
Women with atrial fibrillation receive less anticoagulation treatment with warfarin. Even so, they have a greater risk for stroke than men [51].
Women obtain dialysis later than men, and undergo fewer kidney transplants, both from living and deceased donors [52,53].
There is a significant delay in referral of female patients with rheumatoid arthritis to an early arthritis clinic in comparison with male patients [15].
Osteoporosis and depression are considered female diseases. Both might be under-diagnosed in men [16].
Table 1. Publications with sex and gender differences in the most frequent clinical entities.
| Cardiology | Rheumatology/Immunology | Pneumology | Nephrology | Gastroenterology/ Hepatology | Neurology | Endocrinology | Oncology | Haematology |
|---|---|---|---|---|---|---|---|---|
| Hypertension (414) | Lupus erythematosus (68) | Asthma (140) | Renal failure (27) | Hepatitis B (22) | Multiple sclerosis (65) | Diabetes mellitus (447) | Skin carcinoma (45) | Anaemia (44) |
| Myocardial infarction (275) | Rheumatoid arthritis (41) | Lung cancer (116) | Diabetic nephropathy (11) | Hepatitis C (26) | Stroke (129) | Obesity (349) | Gastric cancer (25) | Leukaemia (49) |
| Heart failure (153) | Systemic sclerosis (3) | Chronic obstructive pulmonary disease (36) | Glomerulone-nephritis (9) | Hepato-cellular carcinoma (37) | Alzheimer's disease (104) | Osteo-porosis (123) | Renal cell carcinoma (17) | Lymphoma (34) |
| Atrial fibrillation (38) | Fibromyalgia (15) | Pulmonary hypertension (12) | Polycystic kidney disease (12) | Inflammatory bowel disease (13) | Epilepsy (56) | Hypo-thyreoidsm (33) | Bladder cancer (22) | Thrombo-cytopoenia (6) |
| Coronary heart disease (207) | Sjögren's syndrome | Pulmonary embolism (110) | Renal artery stenosis (0) | Colorectoral cancer (24) | Parkinson's disease (69) | Hyper-thyreoidsm (16) | Thyroid carcinoma (16) | Purpura (2) |
| Cardiomyopathy (41) | Ankylosing sponylitis (11) | Sarcoidosis (6) | IgA Nephropathy (2) | Autoimmune Hepatitis (2) | Muscular dystrophy (11) | Morbus Addison/Cushing disease (5) | Pancreatic carcinoma (10) | Agranulo-cytosis (0) |
Numbers in brackets refer to the number of publications.
Science & Society Series on Sex and Science.
Sex is the greatest invention of all time: not only has sexual reproduction facilitated the evolution of higher life forms, it has had a profound influence on human history, culture and society. This series explores our attempts to understand the influence of sex in the natural world, and the biological, medical and cultural aspects of sexual reproduction, gender and sexual pleasure.
Sex and gender differences in cardiovascular diseases are particularly well-investigated because there is strong epidemiological evidence that men and women face different risks and have different outcomes. As such, it is useful to explore some of the differences between men and women and how they experience cardiovascular disease.
The overall incidence of myocardial infarction is in decline worldwide in all population groups except young women [2]. This group has probably not been reached by prevention programmes, and also faces increased cardiovascular risk owing to lifestyle changes—such as smoking or experiencing increasing job stress. In addition, young women have a higher rate of mortality after the first myocardial infarction and coronary bypass graft surgery than do men in the same age group. Conversely, men in all age groups have a higher risk of ischaemic sudden death. Women and men also differ in regard to the causes of myocardial infarction: psychological factors are more important in women; heavy exercise is a more common cause in men. Social stress is another main determinant of re-infarction after a first myocardial infarction in women [3]. Women also seem to experience a greater variety of symptoms, so-called ‘atypical syndromes’, and more vagal activation signs than men [4]. In terms of diagnosis and treatment, women receive less guideline-based diagnosis and less-invasive treatment for myocardial infarction than men, not as a result of evidence-based strategies, but simply owing to the habits of physicians.
For coronary artery disease, the average age of female sufferers is about ten years older than that of male sufferers. Women also present more frequently with single vessel disease and disturbances of the microcirculation. Although exercise echocardiography is frequently misleading in women for reasons not fully understood, exercise echocardiography, scintigraphy or magnetic resonance imaging are generally of greater diagnostic value for women.
Women more frequently experience heart failure with normal systolic function or diastolic heart failure, whereas men present more often with heart failure with reduced ejection fraction. The main causes for these differences include calcium signalling, nitric oxide synthesis and profibrotic mechanisms, which depend partly on the action of oestrogens and androgens. Survival is comparably poor for both sexes, but women have a better outcome than men [5]. Hypertension is more frequent in young men than in young women, but the incidence among women increases steeply after the menopause. Hypertension and myocardial hypertrophy are also relatively greater risk factors for heart failure in women than in men [3].
Cardiomyopathies occur slightly more frequently in men than in women with a ratio of 1.5:1 or 2:1; however, takotsubo cardiomyopathy, a largely understudied condition, affects almost only women. It is associated with psychological stress and mimics the features of acute myocardial infarction with open coronary arteries, accompanied by severe left ventricular dysfunction. Similar to heart failure, women with cardiomyopathies and systolic failure receive less-invasive treatment devices or organ transplants than men. Women have more bleeding complications when undergoing invasive therapies in the coronary arteries, receive less anticoagulation with warfarin and have a higher risk of bleeding with different forms of anticoagulant.
Women also experience more strokes than men, yet this is mostly owing to greater incidence of stroke with increasing age. In addition, an increasing number of younger women are affected by stroke each year. Atrial fibrillation is a greater risk for stroke in women than in men [6,7].
Of course, cardiovascular diseases are by no means the only area in which men and women differ in their susceptibility to and survival of disease. Generally, women are more frequently affected by all forms of anaemia; iron deficiency is a frequent cause of anaemia among women [8].
There are also clear gender differences in regard to pulmonary diseases. There is a higher incidence of asthma among young boys, but this reverses over time such that, in young adulthood, women seem predominantly affected [9,10] and experience more severe symptoms. Lung cancer and chronic obstructive pulmonary artery disease remain a serious problem for both women and men. Owing to increased smoking prevalence among women and a greater sensitivity of women to tobacco toxicity [11], their prevalence in women is rising and will soon reach the same level as in men [12].
Another clear sex difference is the fact that women have a lower number of nephrons in their kidney and less capacity to concentrate urine than men. In terms of disease, more women have stage 3 chronic kidney diseases [13] and they experience more complications of kidney failure. Conversely, lupus nephritis is more common in men and displays a more aggressive progression. Polycystic kidney disease is also more prevalent in men and has a worse outcome than in women [14].
Most autoimmune diseases are more frequent in women than in men [15]. Systemic lupus erythematosus is more frequent in women of reproductive age, as its severity is affected by serum oestrogen concentration. Sjögren syndrome is also more frequent in women; again, it seems that sex hormones are involved in the pathophysiology. Fibromyalgia, a poorly understood disease, is more frequent in women than in men, as is rheumatoid arthritis. In addition, there is a significant diagnostic delay for rheumatic diseases in women in comparison to men.
Sex and gender differences in the incidence and prevalence of diabetes mellitus are small and in part controversial [16]. However, diabetes increases the risk for coronary artery disease to a higher degree in women than in men and is associated with a greater risk of death after myocardial infarction in women. Thyroid diseases and anti-thyroid antibodies are more common in women, whilst male sex is a risk factor for thyroid cancer. Osteoporosis is more frequent in women, but it is frequently under-diagnosed in men and is a hidden cause of hip fracture. Alzheimer disease is more frequent in women and more frequently associated with depression.
Despite the wealth of data on differences, medical practice does not sufficiently take gender into account in diagnosis, treatment or disease management
In summary, there is a significant number of sex and gender differences for many common diseases and disorders that need to be considered in health care, public health strategies, regulations and training of medical personnel. Unfortunately, they are largely neglected. In Europe, and in particular in Germany, relatively few public health organizations or health politics promote gender-sensitive health care.
Despite the wealth of data on differences, medical practice does not sufficiently take gender into account in diagnosis, treatment or disease management. This is further compounded by the fact that there are almost no systematic analyses of treatment differences between women and men, at least in German public health. Studies that have analysed the use of drugs in heart failure in Germany [17] or coronary artery disease [18,19] have found that women are less frequently treated with evidence-based therapies. This is most pronounced when the physician is male and is dealing with cardiovascular diseases [17,20] and diabetes [21]. In Europe, women receive less echocardiography, less angiography to diagnose coronary artery disease and less percutaneous coronary intervention or bypass surgery if needed [22]. Usually, the lack of treatment of women is justified by their higher age, but this argument neglects the significant fact that women on average live longer than men, and that elderly women and men 6–8 years younger are similar in regard to biological age and life expectancy.
Similarly, rehabilitation and disease management programmes are not always adjusted to the specific needs of each gender. In particular, they do not consider the limited mobility of women—elderly women less often own a car than elderly men—the constraints on their time that result from being the primary care giver in a family and their specific preferences for exercise. Even in areas in which sex and gender differences are obvious—such as for ischaemic heart disease, symptoms of myocardial infarction, sensitivity to some cardiovascular drugs, or different forms of pre-diabetes in women and men—these are not adequately considered in disease management guidelines.
Of course, there are some positive examples of guidelines and treatments that take gender into account, but these are few and far between in our experience. One such example is the guideline for the management of atrial fibrillation, which includes female sex as an additional risk factor for stroke to be taken into account by physicians [23]. Similarly, the guidelines for cardiovascular diseases during pregnancy issued by the German Cardiac Society (DGK)and the European Cardiac Society (ESC) are examples of best practice as they focus on risks and treatments specific to women [4,24]. Nonetheless, the fact that most of the recommendations in the guidelines derive from expert opinions, rather than evidence-based treatments, demonstrates the lack of standards in addressing pregnancy-related diseases. There is still a huge need for research on pharmacotherapy in pregnancy and mechanisms of pregnancy-related cardiovascular, metabolic and other diseases [25].
In general, however, few efforts have been made to consider both genders in health care. Even so, some progress has been made in Germany. In December 2000, the parliament of the German state of North Rhine-Westphalia established an Enquete-Kommission to look at the future of female health care and suggest solutions for the deficiencies identified. In 2004, this commission suggested strategies for a gender-sensitive health policy and recommended action to be taken by the government and public health stakeholders (Sidebar B; [26]). However, it took until 2010 for gender to be included as a research focus for state funding from North Rhine-Westphalia.
Sidebar B | Groups responsible for the major recommendations of the Enquete Commission in North Rhine–Westphalia in 2004.
North Rhine–Westphalia government
Establish a register for myocardial infarction on gender-sensitive principles
Increased efforts in education of children and adolescents, particularly covering risk factors and preventive aspects
Increased funding of gender-sensitive research questions in the area of cardiovascular diseases
Health insurances
Support of company-based prevention
Increased offer of long-term prevention programmes, specifically adapted for women
Support for the development of physical fitness programmes that improve cardiovascular function, adapted to female needs
Chambers of doctors
Consider sex-specific differences in diagnostics and therapy in the information and training given to doctors
Support of programmes in primary and secondary prevention of cardiovascular diseases considering gender-specific aspects
Realizing gender-sensitive optimized treatment strategies in life-threatening cardiovascular diseases in women and men in their area of responsibility
Physician's association in Germany
Support for more cooperation as prerequisite for emergency care in cardiovascular diseases in a gender-sensitive manner
Support of projects in disease management of cardiovascular diseases
Media
Contribution to dispersing information on prevention and treatment programmes in cardiovascular disease
Researcher
Include possible sex and gender differences in research questions and research design, as well as planning of cohorts
Obtain a gender-sensitive data set
Describe research results in a gender-sensitive manner
At the federal level, the Frauengesundheitsbericht report (Report on Women's Health) provided data on the health status of women in Germany. Its original release was in 2001, but it has not been updated since. The most recent study, still awaiting publication, is the Deutsche Gesundheits studie bei Erwachsenen (DGESA; German study on the health of adults). In order to assess the extent to which gender is considered in this report, one can search the DGESA outline for ‘women’ to find that it yields only a few hits, mainly in the chapter about sexual diseases. Searching for ‘Geschlecht’, meaning sex or gender, is slightly better and leads to hits in most chapters, but only four references among the several hundred in the DGESA outline have sex or gender in their title. Thus, the report recognizes the role of gender in health, but does not adequately cover the research into sex, gender and health [27,28,29,30].
To address these shortcomings in Germany and in order to improve the treatment of common diseases by considering sex and gender, the Charité University Hospital in Berlin began in 2008 to integrate sex and gender medicine into educational programmes. The unique Charité Institute Gender in Medicine (GiM) has established a curriculum on gender medicine that is implemented in the medical student's regular curriculum, and is integrated into specific disciplines wherever possible. In addition, GiM has established an elective course that gives interested students the opportunity to learn more about sex and gender medicine and get an overview on this evolving area.
Sex and gender differences in common diseases must be considered to improve health and health care for women and for men; this is a quality issue in medical care
GiM has also developed two teaching modules that can be integrated in master's degree programmes: one is being used at the Berlin School of Public Health and another one for a Health and Society programme for students who will eventually work in health care management, health insurance companies or political organizations. The elective modules are well-accepted and are now being taught for the second time in 2012. In order to reach as many professionals as possible, GiM has also established an e-learning course on gender medicine to communicate the most important messages of this field to students in biomedicine and the scientific community generally. So far, it consists of two days of personal tuition and a personal exam in a combined learning programme. After the first course in 2011, the 2012 course for 25 students and professionals completely sold out, with a considerable waiting list.
The GiM also coordinated a European project known as the European Curriculum Gender in Medicine (EUGIM) from 2009 to 2011, which defined a curriculum and study regulations for gender medicine. Following the principles of the Bologna process that aims at harmonizing study structures between European universities, it has established learning goals, skills and required time investments in such a way that this curriculum can be taught throughout Europe. So far it is packed into two modules that can be integrated into diverse biomedicalor social sciences master's programmes.
Similar efforts are being made on a national scale. To improve awareness among the medical profession of gender and sex in health, the German Society of Gender Medicine (DGesGM e.V.) has set up a qualification as a ‘gender physician’. The qualification Gendermediziner® indicates that physicians understand the goals, principles and knowledge of gender medicine in a way that enables them to treat women and men in a gender-sensitive manner. Documented activities in the field of gender medicine as well as participation in training courses are required to obtain this additional qualification. Last year, ten physicians acquired this qualification and there is now growing interest from physicians and patients.
Yet, despite this progress, gender medicine is still a new medical discipline. Sex and gender differences in common diseases must be considered to improve health and health care for women and for men; this is a quality issue in medical care. GiM has edited and partly written a textbook in this vein that focuses on clinical questions. More than 10,000 references have been included and categorized according to epidemiology, pathophysiology, clinical manifestations of disease, management and outcome. This might contribute to further developing gender medicine and to defining available knowledge and the scope of knowledge in this field. A second book in the well-renowned series Handbook in Experimental Pharmacology is on its way and will appear in Autumn 2012.
Some experts argue that gender-based medicine will eventually become irrelevant with the advent of personalized medicine. However, the analysis of large databases reveals that gender remains an independent and important risk factor after controlling for age, comorbidities, scored risk factors and ethnicity because some genetic variants convey a different risk in women and men [31,32]. Moreover, the socio-cultural dimension of gender, integrating lifestyle, environment, stress and other variables, cannot easily be replaced by a sum of biological parameters. Given this prominent role of gender, individualized clinical-care algorithms based on individual risk profiles would have to include gender-based assessments.
Efficient gender- and sex-based health care ultimately requires a more holistic strategy, which needs to include all aspects of health and health care. As such, research programmes need to be far more aware and take more serious account of gender- and sex-based differences. For example, adequate animal models for menopause transition are lacking. Usually, ovarectomy in young female mice is used to model menopause, but this eliminates all ovarian tissues and ovarian hormones, including testosterone-synthesizing stroma cells. On the upside, a new model has been developed that uses chronic vinylcyclohexene administration in female mice, which slowly destroys ovarian follicles and creates a pathophysiological state that mimics natural menopause [33,34].
… research programmes need to be far more aware and take more serious account of gender- and sex-based differences
Similarly, models for drug development and testing are not ideal. Although significant differences exist in the outcomes of male and female mice in models of myocardial infarction and genetic cardiovascular diseases [3,35,36], most cardiovascular researchers use only male mice [37]. Female mice tend to have better outcomes in most models of pressure overload, in transgenic models for heart failure and in myocardial infarction, whereas males have severe phenotypes. Because of this, more therapeutic effects observed in males are probably greater than those seen in female mice. In the extreme, a drug might have a major effect in males and yet be totally ineffective in females. Moreover, even a single gene mutation or an element of the animal's nutrition, such as phyto-oestrogens supplied in the animal chow, can have varied drug effects in male and female mice [38,39].
Personalized medicine cannot replace gender-based medicine
These differences are borne out in humans and the effects of many pharmacological interventions differ between women and men. Lower body surface in women, differences in kidney function, drug resorption and metabolism by hepatic enzymes and excretion cause significant differences in pharmacokinetics. Many drugs therefore require different dosing to achieve optimal effects. In addition, differences in pharmacodynamics are also evident. Ion channels in kidney and heart tissue differ between women and men, which might cause sex-specific effects of drugs that are used to modify kidney function or heart rhythm. Major sex and gender differences have been reported for the efficiency and adverse effects of heart failure drugs, such as digitalis, angiotensin-converting enzyme inhibitors and anti-arrhythmics. Similar effects have also been found in analgesic, neuropsychiatric, anticancer and cardiovascular drugs, as well as in the effects of anti-tumour necrosis factor-α and antiviral drugs. These differences are related to the efficacy of the drugs and to their appropriate dosage and administration for each gender. Nonetheless, there is some progress being made, as the first drugs for use in only one gender have been developed, as well as gender-specific recommendations for drug dosing in the treatment of depression and inflammatory bowel disease [40,41].
The effects of non-pharmaceutical therapeutic interventions also differ in women and men. Coronary bypass surgery has a greater early mortality in women, and aggressive early revascularization strategies seem to be less effective in women with unstable angina than in men. By contrast, the use of resynchronization therapy in heart failure seems to be more effective in women. Therefore, different strategies are needed to optimize therapeutic procedures.
In terms of clinical testing, major efforts have been made to increase the participation of women in all types of clinical trial. However, various studies concluded that women were still not sufficiently included in mixed-sex cardiovascular trials to reflect the disease prevalence among the general population [42,43]. A 2005 analysis of 300 new drug applications between 1995 and 2000 found that even drugs showing substantial differences in how they were absorbed, metabolized and excreted by men and women had no sex-specific dosage recommendations on their labels [44]. This might be one reason why women are 1.5–2-fold more likely to develop an adverse reaction to prescription drugs than men [45,46]. Even the most recent investigations have found that female-specific effects are still overlooked in research into cardiovascular diseases and in early studies [47,48,49].
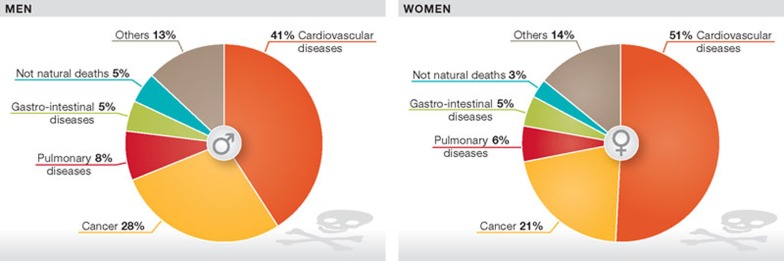
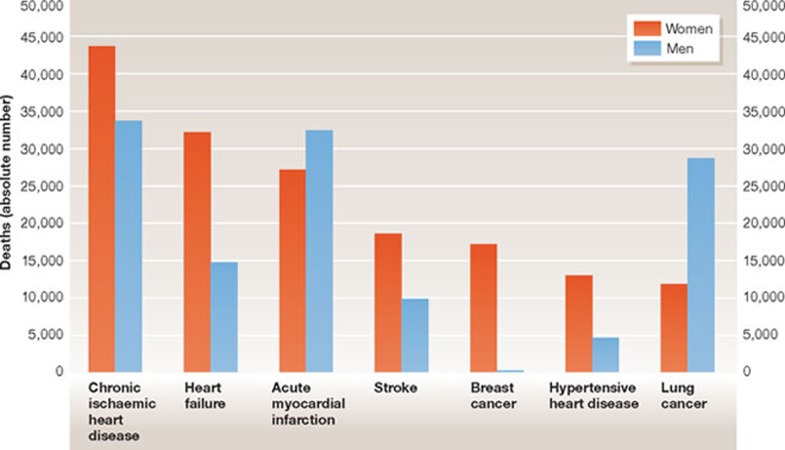
In fact, owing to the standard inclusion of sex in epidemiological studies, descriptive data are available that confirm that the incidence and mortality of the most common diseases differ in women and men (Figs 2,3). However, we have no studies specifically designed to understand variations in disease mechanisms across both genders. These are sorely needed to inform public campaigns aimed at improving prevention and early diagnosis, thereby reducing mortality. As some campaigns have shown, integrating the role of gender in this way can lead to successful outcomes, such as increasing breast cancer awareness and early diagnosis, anti-smoking campaigns targeted at men and the ‘Go Red for Women’ campaign of the American Heart Association.
Figure 2. Percentage breakdown of causes of death for men and women in Germany.
Cardiovascular diseases are the main cause of death for men and women in western industrial nations. (Totals might not be 100 owing to rounding up or down of data.) Statistics taken from Statistisches Bundesamt Robert Koch Institut Berlin, 2005.
Figure 3. Percentage breakdown of cardiovascular causes of deaths for men and women in Germany.
Chronic ischaemic heart diseases are the main cause of death for women. In absolute numbers more men than women die of acute myocardial infarction. Statistics taken from Statistisches Bundesamt Robert Koch Institut Berlin, 2007.
In the area of cardiovascular diseases, for instance, campaigns should create awareness of positive lifestyle changes that can be made, including exercise, nutrition and stress reduction [50]. Such campaigns are probably only successful if they are targeted to specific female or male audiences. A good example is the ‘Hör auf dein Herz’ or ‘Listen to your Heart’ campaign to raise awareness of cardiovascular health among German women. This campaign will include the Berlin Women Risk Evaluation study, which is investigating how 1,000 women living in Berlin estimate their own cardiovascular risk and then comparing their estimates with objective data. Additionally, it will analyse risk factors that are typical for women—rheumatic diseases, depression or complications during pregnancy—but have not yet been specifically studied, with the aim to include these in better risk prediction algorithms in the near future.
Ultimately, the role of sex and gender must be taken into account in research and health care practices. Not doing so is adversely affecting the health of citizens and the survival of patients. The preferential use of male animals in drug development, and the under-representation of women in early and clinical cardiovascular trials must come to an end. Sex and gender aspects must be considered in drug use—taking into account pharmacokinetic and pharmacodynamic aspects—in health care and in public health. They must be included in guidelines and disease management.
The implementation of gender-equitable diagnostics and treatment requires time, commitment and institutional and political support
Personalized medicine cannot replace gender-based medicine. The socio-cultural dimension of gender, integrating lifestyle, environment, stress and other variables, is a valuable component of clinical medicine and gains rather than loses acceptance. The inclusion of gender-specific analysis in medical trials and the development of gender-sensitive diagnostic and therapeutic indications can have a long-term effect on the bulging costs of medical care. From a cost–benefit perspective, inadequate and inappropriate therapy might even be more costly than the complete absence of therapy.
The implementation of gender-equitable diagnostics and treatment requires time, commitment and institutional and political support. Translating the available research results into practice might take between 5 and 15 years, especially if the development of new drugs has to be taken into account. This calls for immediate action as we cannot ethically afford to ignore these research-backed results. Several steps to further this integration are being taken, as described in this article, by us and colleagues around the world. However, the growing support of the scientific community in this matter is essential to achieve productive and lasting results that will benefit all patients, regardless of their gender.
There are obviously obstacles against the promotion of gender medicine. It has been mistaken for feminism, attacked as ‘biologistic’ and assumed to generate higher costs by doubling the amount of animal work and increasing the number of patients needed for clinical studies without adequate payback. None of these arguments is true—gender medicine aims to improve the health of women and men; it considers sociological aspects and biological facts.

Vera Regitz-Zagrosek
Acknowledgments
I thank Sabine Oertelt Prigione for adding valuable comments to the text, Stefanie Schmidt for secretarial assistance and the German Center of Cardiovascular Research for institutional support.
Footnotes
The author declares that she has no conflict of interest.
References
- Oertelt-Prigione S, Regitz-Zagrosek V (eds) (2012) Sex and Gender Aspects in Clinical Medicine. London, UK: Springer [Google Scholar]
- Lloyd-Jones D et al. (2010) Heart disease and stroke statistics—2010 update. Circulation 121: e46–e215 [DOI] [PubMed] [Google Scholar]
- Regitz-Zagrosek V (2006) Therapeutic implications of the gender-specific aspects of cardiovascular disease. Nat Rev Drug Discov 5: 425–438 [DOI] [PubMed] [Google Scholar]
- Regitz-Zagrosek V (2011) Sex and gender differences in symptoms of myocardial ischaemia. Eur Heart J 32: 3064–3066 [DOI] [PubMed] [Google Scholar]
- Regitz-Zagrosek V, Oertelt-Prigione S, Seeland U, Hetzer R (2010) Sex and gender differences in myocardial hypertrophy and heart failure. Circ J 74: 1265–1273 [DOI] [PubMed] [Google Scholar]
- Dagres N et al. (2007) Gender-related differences in presentation, treatment, and outcome of patients with atrial fibrillation in Europe: a report from the Euro Heart Survey on Atrial Fibrillation. J Am Coll Cardiol 49: 572–577 [DOI] [PubMed] [Google Scholar]
- Nolte CH, Heuschmann PU, Endres M (2012) Sex and gender differences in neurology. In Sex and Gender Aspects in Clinical Medicine (eds Oertelt-Prigione S, Regitz-Zagrosek V), pp 169–182. London, UK: Springer [Google Scholar]
- Schmetzer O, Florcken A (2012) Sex and gender differences in hematology. In Sex and Gender Aspects in Clinical Medicine (eds Oertelt-Prigione S, Regitz-Zagrosek V), pp 151–168. London, UK: Springer [Google Scholar]
- Manfreda J et al. (2004) Geographic and gender variability in the prevalence of bronchial responsiveness in Canada. Chest 125: 1657–1664 [DOI] [PubMed] [Google Scholar]
- Grohe C (2012) Sex and gender differences in pulmonary diseases. In Sex and Gender Aspects in Clinical Medicine, (eds Oertelt-Prigione S, Regitz-Zagrosek V), pp 45–63. London, UK: Springer [Google Scholar]
- Dransfield MT, Davis JJ, Gerald LB, Bailey WC (2006) Racial and gender differences in susceptibility to tobacco smoke among patients with chronic obstructive pulmonary disease. Respir Med 100: 1110–1116 [DOI] [PubMed] [Google Scholar]
- Manton KG (2000) Gender differences in the cross-sectional and cohort age dependence of cause-specific mortality: the United States, 1962 to 1995. J Gend Specif Med 3: 47–54 [PubMed] [Google Scholar]
- Silbiger S, Neugarten J (2008) Gender and human chronic renal disease. Gend Med 5 (Suppl A): S3–S10 [DOI] [PubMed] [Google Scholar]
- Gallieni M, Mezzina N, Pinerolo C, Granata A (2012) Sex and gender differences in nephrology. In Sex and Gender Aspects in Clinical Medicine (eds Oertelt-Prigione S, Regitz-Zagrosek V), pp 83–100. London, UK: Springer [Google Scholar]
- Zandman-Goddard G et al. (2012) Sex and gender differences in autoimmune diseases. In Sex and Gender Aspects in Clinical Medicine (eds Oertelt-Prigione S, Regitz-Zagrosek V), pp 101–124. London, UK: Springer [Google Scholar]
- Kautzky-Willer A (2012) Sex and gender differences in endocrinology. In Sex and Gender Aspects in Clinical Medicine (eds Oertelt-Prigione S, Regitz-Zagrosek V), pp 125–149. London, UK: Springer [Google Scholar]
- Baumhakel M, Muller U, Bohm M (2009) Influence of gender of physicians and patients on guideline-recommended treatment of chronic heart failure in a cross-sectional study. Eur J Heart Fail 11: 299–303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bischoff B, Silber S, Richartz BM, Pieper L, Klotsche J, Wittchen HU (2006) Inadequate medical treatment of patients with coronary artery disease by primary care physicians in Germany. Clin Res Cardiol 95: 405–412 [DOI] [PubMed] [Google Scholar]
- Geller JC et al. (2007) Achievement of guideline-defined treatment goals in primary care: the German Coronary Risk Management (CoRiMa) study. Eur Heart J 28: 3051–3058 [DOI] [PubMed] [Google Scholar]
- Journath G, Hellenius ML, Manhem K, Kjellgren KI, Nilsson PM (2008) Association of physician's sex with risk factor control in treated hypertensive patients from Swedish primary healthcare. J Hypertens 26: 2050–2056 [DOI] [PubMed] [Google Scholar]
- Berthold HK, Gouni-Berthold I, Bestehorn KP, Bohm M, Krone W (2008) Physician gender is associated with the quality of type 2 diabetes care. J Intern Med 264: 340–350 [DOI] [PubMed] [Google Scholar]
- Daly C et al. (2006) Gender differences in the management and clinical outcome of stable angina. Circulation 113: 490–498 [DOI] [PubMed] [Google Scholar]
- Camm AJ et al. (2010) Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J 31: 2369–2429 [DOI] [PubMed] [Google Scholar]
- Regitz-Zagrosek V, Gohlke-Barwolf C, Geibel-Zehender A, Haass M, Kaemmerer H, Kruck I, Nienaber C (2008) Heart diseases in pregnancy. Clin Res Cardiol 97: 630–665 [DOI] [PubMed] [Google Scholar]
- Baylis F (2010) Pregnant women deserve better. Nature 465: 689–690 [DOI] [PubMed] [Google Scholar]
- Landtag NRW (ed) (2004) Zukunft einer frauengerechten Gesundheitsversorgung in NRW: Bericht der Enquetekommission des Landtags Nordrhein-Westfalen. Wiesbaden, Germany: VS Verlag für Sozialwissenschaften [Google Scholar]
- Kurth BM (2002) Die Gesundheit von Männern und Frauen—Möglichkeiten und Grenzen einer geschlechtsspezifischen Gesundheitsberichterstattung. In Dokumentation der Fachtagung “Frauen Gesundheit-Frauen Leben-Frauen Arbeit” im Oktober 2001. Bericht zur gesundheitlichen Situation von Frauen in Deutschland, Bundesministerium für Familie S, Frauen und Jugend (BMFSFJ) (ed). Berlin, Germany: Bundesministerium für Familie, Senioren, Frauen und Jugend (BMFSFJ) [Google Scholar]
- Hurrelmann K, Kolip P (eds) (2002) Geschlecht, Gesundheit und Krankheit: Männer und Frauen im Vergleich. Bern, Germany: Hans Huber [Google Scholar]
- Lange C, Lampert T (2004) Perspectives on gender sensitive health reporting. Gesundheitswesen 66: 158–163 [DOI] [PubMed] [Google Scholar]
- Kolip P, Koppelin F (2002) Geschlechtsspezifische Inanspruchnahme von Prävention und Krankheitsfrüherkennung. In Geschlecht, Gesundheit und Krankheit: Männer und Frauen im Vergleich [Gender, Health and Disease: Men and Women by Comparison] (eds Hurrelmann K, Kolip P), pp 491–504. Bern, Germany: Hans Huber [Google Scholar]
- Siddiqui RA et al. (2009) X chromosomal variation is associated with slow progression to AIDS in HIV-1-infected women. Am J Hum Genet 85: 228–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu LY, Schaub MA, Sirota M, Butte AJ (2012) Sex differences in disease risk from reported genome-wide association study findings. Hum Genet 131: 353–364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyer PB, Devine PJ, Hu X, Thompson KE, Sipes IG (2001) Ovarian toxicity of 4-vinylcyclohexene diepoxide: a mechanistic model. Toxicol Pathol 29: 91–99 [DOI] [PubMed] [Google Scholar]
- Lohff JC, Christian PJ, Marion SL, Arrandale A, Hoyer PB (2005) Characterization of cyclicity and hormonal profile with impending ovarian failure in a novel chemical-induced mouse model of perimenopause. Comp Med 55: 523–527 [PubMed] [Google Scholar]
- Czubryt MP, McAnally J, Fishman GI, Olson EN (2003) Regulation of peroxisome proliferator-activated receptor gamma coactivator 1 alpha (PGC-1 alpha) and mitochondrial function by MEF2 and HDAC5. Proc Natl Acad Sci USA 100: 1711–1716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fliegner D et al. (2010) Female sex and estrogen receptor-beta attenuate cardiac remodeling and apoptosis in pressure overload. Am J Physiol Regul Integr Comp Physiol 298: R1597–R1606 [DOI] [PubMed] [Google Scholar]
- Zucker I, Beery AK (2010) Males still dominate animal studies. Nature 465: 690. [DOI] [PubMed] [Google Scholar]
- Bhupathy P, Haines CD, Leinwand LA (2010) Influence of sex hormones and phytoestrogens on heart disease in men and women. Womens Health (Lond Engl) 6: 77–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luczak ED, Barthel KK, Stauffer BL, Konhilas JP, Cheung TH, Leinwand LA (2011) Remodeling the cardiac transcriptional landscape with diet. Physiological Genomics 43: 772–780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adeyemo MA, Chang L (2008) New treatments for irritable bowel syndrome in women. Womens Health (Lond Engl) 4: 605–622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shekhar C, Whorwell PJ (2009) Emerging drugs for irritable bowel syndrome. Expert Opin Emerg Drugs 14: 673–685 [DOI] [PubMed] [Google Scholar]
- Kim ES, Carrigan TP, Menon V (2008) Enrollment of women in National Heart, Lung, and Blood Institute-funded cardiovascular randomized controlled trials fails to meet current federal mandates for inclusion. J Am Coll Cardiol 52: 672–673 [DOI] [PubMed] [Google Scholar]
- Kim AM, Tingen CM, Woodruff TK (2010) Sex bias in trials and treatment must end. Nature 465: 688–689 [DOI] [PubMed] [Google Scholar]
- Anderson GD (2005) Sex and racial differences in pharmacological response: where is the evidence? Pharmacogenetics, pharmacokinetics, and pharmacodynamics. J Womens Health (Larchmt) 14: 19–29 [DOI] [PubMed] [Google Scholar]
- Zopf Y, Rabe C, Neubert A, Gassmann KG, Rascher W, Hahn EG, Brune K, Dormann H (2008) Women encounter ADRs more often than do men. Eur J Clin Pharmacol 64: 999–1004 [DOI] [PubMed] [Google Scholar]
- Martin RM, Biswas PN, Freemantle SN, Pearce GL, Mann RD (1998) Age and sex distribution of suspected adverse drug reactions to newly marketed drugs in general practice in England: analysis of 48 cohort studies. Br J Clin Pharmacol 46: 505–511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melloni C et al. (2010) Representation of women in randomized clinical trials of cardiovascular disease prevention. Circ Cardiovasc Qual Outcomes 3: 135–142 [DOI] [PubMed] [Google Scholar]
- O'Connor RE et al. (2010) Part 9: Acute coronary syndromes: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 122: S422–S465 [DOI] [PubMed] [Google Scholar]
- O'Connor RE et al. (2010) Part 10: acute coronary syndromes: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 122: S787–S817 [DOI] [PubMed] [Google Scholar]
- Seeland U, Regitz-Zagrosek V (2012) Geschlechtsspezifische Unterschiede in der Kardiologie—Schwerpunkt Prävention— Thieme XX 2: 100–106 [Google Scholar]
- Humphries KH et al. (2001) New-onset atrial fibrillation: sex differences in presentation, treatment, and outcome. Circulation 103: 2365–2370 [DOI] [PubMed] [Google Scholar]
- Jindal RM, Ryan JJ, Sajjad I, Murthy MH, Baines LS (2005) Kidney transplantation and gender disparity. Am J Nephrol 25: 474–483 [DOI] [PubMed] [Google Scholar]
- Kausz AT, Obrador GT, Arora P, Ruthazer R, Levey AS, Pereira BJ (2000) Late initiation of dialysis among women and ethnic minorities in the United States. J Am Soc Nephrol 11: 2351–2357 [DOI] [PubMed] [Google Scholar]
- Regitz-Zagrosek V et al. (2010) Heart transplantation in women with dilated cardiomyopathy. Transplantation 89: 236–244 [DOI] [PubMed] [Google Scholar]