Abstract
Background
Guidelines for cardiopulmonary resuscitation (CPR) recommend a chest compression rate of at least 100 compressions/min. Animaland human studies have reported that blood flow is greatest with chest compression rates near 120/min, but few have reported rates used during out-of-hospital (OOH) CPR, or the relationship between rate and outcome. The purpose of this study was to describe chest compression rates used by emergency medical services (EMS) providers to resuscitate patients with OOH cardiac arrest and to determine the relationship between chest compression rate and outcome.
Methods and Results
Included were patients ≥ 20 years old with OOH cardiac arrest treated by EMS providers participating in the Resuscitation Outcomes Consortium. Data were abstracted from monitor-defibrillator recordings during CPR. Multiple logistic regression assessed the association between chest compression rate and outcome. From December 2005 to May 2007, 3,098 patients with OOH cardiac arrest were included in this study. Mean age was 67±16 years and 8.6% survived to hospital discharge. Mean compression rate was 112±19/min. A curvilinear association between chest compression rate and return of spontaneous circulation (ROSC) was found in cubic spline models after multivariable adjustment (p = 0.012). ROSC rates peaked at a compression rate of about 125/min and then declined. Chest compression rate was not significantly associated with survival to hospital discharge in multivariable categorical or cubic spline models.
Conclusions
Chest compression rate was associated with ROSC but not with survival to hospital discharge in OOH cardiac arrest.
Keywords: cardiac arrest, cardiopulmonary resuscitation, guidelines, heart arrest, outcomes research
Introduction
The quality of cardiopulmonary resuscitation (CPR) and chest compressions is thought to be a major determinant of survival from cardiac arrest.1 Over the past 50 years, there has been a progressive increase in the recommended rate of chest compressions during CPR.2–4
The current 2010 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) recommend using a chest compression rate of at least 100 compressions/min.1 While the 2010 European Resuscitation Council CPR Guidelines5 recommend an upper rate limit of 120 chest compressions/minute, the AHA guidelines do not provide a similar recommendation, because of stated lack of evidence from human studies with return of spontaneous circulation (ROSC) or survival as outcomes.
In addition, few studies have reported the distribution of actual chest compression rates used to resuscitate patients with OOH cardiac arrest.6 –8 Whenever compression rates of emergency medical services (EMS) providers have been measured in the OOH setting, most often the rates have been faster than 100 compressions/minute, usually averaging between 100 to 120 compressions/minute.
The objectives of this North American multicenter observational study are: (1) to describe the mean rate of chest compressions and range used by EMS providers, including firefighters and paramedics, to resuscitate patients with OOH cardiac arrest and (2) to determine the relationships between chest compression rate and ROSC, and rate and survival to hospital discharge.
Methods
Setting and Design
The Resuscitation Outcomes Consortium (ROC) is a network of regional research centers in the US and Canada and a data coordinating center (DCC) in the US that conducts research focused on cardiac arrest and severe traumatic injury. The ROC established a registry for OOH cardiac arrest in December 2005. An important component of the registry is the collection of defibrillator-monitor electronic files that record the quality of CPR given by EMS providers during treatment of cardiac arrest.
This prospectively acquired, retrospectively analyzed, multicenter, EMS-based observational study was approved by institutional review boards of the University of Washington (location of the DCC), and the participating U.S. and Canadian study sites including Ottawa, Ontario; Toronto, Ontario; and Vancouver, British Columbia in Canada and Birmingham, Alabama; Dallas, Texas; Des Moines, Iowa; Pittsburgh, Pennsylvania; Milwaukee, Wisconsin; Portland, Oregon; Seattle/King County, Washington; and San Diego, California in the United States. Each board waived the requirement for informed consent for this study because it was considered to meet criteria for minimal risk.
ROC was established to evaluate strategies for treatment of patients with cardiac arrest or life-threatening traumatic injury with the primary focus on the OOH emergency setting. It includes over 260 separate emergency medical service (EMS) agencies serving a population of approximately 24 million.9 Since December 2005, the ROC Epidemiologic Cardiac Arrest Registry (Epistry)10, a population-based EMS registry, has prospectively collected data on OOH cardiac arrest cases attended by participating EMS agencies. The data are collected across all ROC sites using standardized data element forms and uniform definitions developed by ROC investigators. Data collected on each subject included information related to OOH treatments and outcomes, including initial cardiac rhythms, response times, descriptions of the types of professional responders on scene, timing of cardiopulmonary resuscitation and defibrillation, response to interventions, return of spontaneous circulation (ROSC), survival to hospital discharge, and collection of digital, electronic recordings of rhythm and chest compressions. All data were collected by trained personnel who followed standardized procedures to ensure the validity and reproducibility of the data. Data were managed by the DCC and included error, logic, and cross-form checks. In addition, the DCC audited a proportion of cases to compare data entry with the original source documents to ensure uniformity and quality of data entry across sites. Two of eleven sites were excluded from this study because they contributed fewer than two cases.
Patient Population
Included were patients 20 years of age or older with completed case status who had OOH cardiac arrest treated by EMS providers participating in the ROC. Age was entered into the database in years, months, or days. If that information was unavailable, then age was indicated as one of the following categories: infant < 1 year, child 1–11 years, adolescent 12–19 years, adult 20–39 years, middle age 40–60, older 61–75 years, elderly >75 years. In addition, the cohort included in this analysis had electronic recordings of chest compressions available. Patients with traumatic cardiac arrest or other obvious non-cardiac causes of arrest were excluded.
Measurement
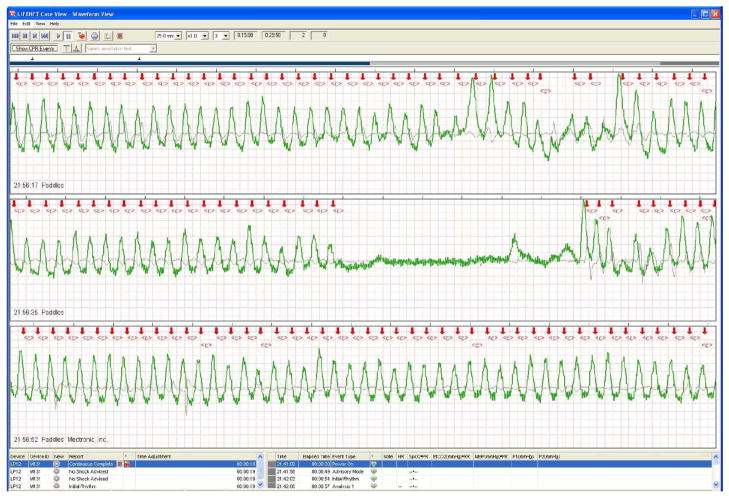
Monitor-defibrillators recorded chest compression rates during CPR. The electronic recordings (Figure 1) were reviewed for accuracy and data from the first five minutes of CPR are included in the analysis. The ROC DCC audited a proportion of original recordings from each site to ensure consistency of review and annotation methods. Selected recordings that had very high chest compression rates were reviewed by a panel with reviewers from other ROC sites and, additionally, by engineers from the defibrillator manufacturers.
Figure 1.
An example of an electronic recording from a monitor-defibrillator showing the electrical channel (black line), the bioimpedance channel (green line), and red arrows marking each chest compression.
The presence and frequency of chest compressions were measured indirectly either by changes in thoracic impedance recorded from external defibrillation electrodes11 or directly via an accelerometer interface between the rescuer and the patient’s chest using commercially available defibrillators. The electronic recordings were reviewed, annotated by trained personnel, and then analyzed with special software, which automatically calculated average chest compression rates for each minute of CPR. Chest compression rate is defined as the rate at which chest compressions were performed during an uninterrupted series of chest compressions, where interruptions in chest compressions (time without chest compressions) are defined as a pause ≥ 3 seconds (Medtronic devices [Minneapolis, Minn]) or ≥ 2 seconds (Philips devices [Andover, Mass] and ZOLL devices [Chelmsford, Mass]). Chest compression rate was defined as the actual rate used during each set of chest compressions within a one-minute interval independent of pauses within the one-minute interval. Thus, rate is the same whether chest compressions are given during the entire one-minute interval or during only 10 seconds of the one-minute interval.
On the other hand, delivered chest compressions was defined as the actual number of chest compressions delivered during a one-minute interval, which is illustrated by the formula: average chest compression rate multiplied by the chest compression fraction equals the number of delivered chest compressions/minute, where chest compression fraction is the proportion of time/minute that chest compressions are given. Interruptions in chest compression are inversely proportional to the chest compression fraction (e.g., no interruptions in chest compression would result in a chest compression fraction of 1). Thus, delivered chest compressions is dependent on both chest compression rate and chest compression fraction. The monitor-defibrillator software counted the actual number of chest compressions delivered each minute rather than estimate it with a formula.
Outcomes
The prospectively selected primary outcome measure was survival to hospital discharge; ROSC was a secondary outcome.
Statistical Analysis
All statistical analyses were performed with commercially available statistical packages (SAS, version 9.1.3, Cary, NC; R, version 2.5.1, Vienna, Austria; Stata, version 11, College Station, TX). Descriptive statistics were calculated for average chest compression rate and within subject variability of chest compression rate over the first five minutes of CPR for the overall sample population as well as for each site. Analysis of variance was used to determine if there was a difference in average chest compression rate between the different sites. Summary results are presented as mean (±SD) or median (IQR). Those with available data were categorized into three groups of chest compression rates based on the average chest compression rate over the first five minutes: <80, 80 – 140, and >140 compressions/minute. These intervals were selected a priori because animal and human physiological studies suggested that blood flow was maximized in the reference range (80 – 140/min).12 –18 Delivered chest compressions were also categorized into three groups based on the average number of chest compressions administered each minute over the first five minutes: <75, 75 – 100, and >100 compressions delivered each minute. These intervals were selected a priori because human studies suggested that ROSC19 and survival7 were maximized in the reference range (75 – 100/min). Potential confounding variables identified a priori included age, gender, bystander-witnessed cardiac arrest, EMS-witnessed cardiac arrest, attempted bystander CPR, public location, ROC site, first known EMS rhythm, and chest compression fraction. Logistic regression with robust standard errors was used to calculate unadjusted and adjusted odds ratios of the association between chest compression rate and number of delivered chest compressions with both survival and ROSC. As a post hoc exploratory analysis, we fit an adjusted natural cubic spline curve, adjusted for the confounding variables noted above (y-axis), to further characterize the nature of the relationship between chest compression rate and survival and chest compression rate and ROSC.20 The basis of the curve was a piecewise cubic polynomial with multiple knots. Four knots were chosen because it produced a curve that appeared adequately smooth. The knots are located at the 5th, 35th, 65th, and 95th percentiles of average chest compression rate. For the adjusted cubic spline graphs, we used a global test, which tested the null hypothesis that the spline curve is a horizontal line.
Results
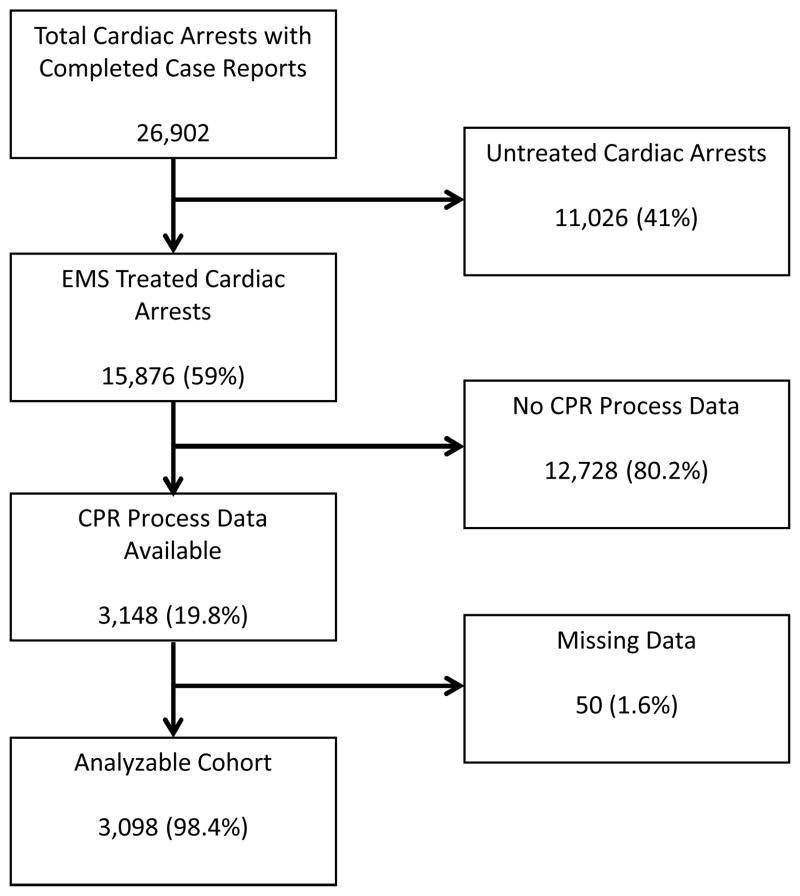
There were a total of 26,902 OOH cardiac arrest cases available, 15,876 received CPR, CPR process data were available for 3,148 cases (19.8% of those treated), and 3,098 cases (19.5% of treated patients) formed the analyzable cohort (Figure 2). The CPR process data were derived from electronic files downloaded from monitor-defibrillators on-board emergency response vehicles. During this study period, December 2005 to May 2007, many ROC sites were in the process of developing the EMS infrastructure necessary to collect these files; this accounts for the relatively low proportion of treated cardiac arrest cases with CPR process data. Across all ROC sites, the distribution of defibrillators was 82% Medtronic, 10% Philips, 7% ZOLL, and 1% Laerdal and missing defibrillator assignment.
Figure 2.
Study cohort and exclusions. EMS indicates emergency medical services.
Patient demographic information is summarized in Table 1. Mean age (±SD) was 67 years ± 16 years, 1,082 had ROSC (35%), and 265 (8.6%) survived to hospital discharge; the distribution of patient characteristics and other key data between three chest compression rate categories also is presented in Table 1. As well, patient characteristics and key data for the analyzed cohort and patients excluded from the study are compared in Table 2. Important differences between the analyzed cohort and the excluded group, respectively, include EMS witnessed arrest (5% vs 10%), bystander CPR (39% vs 30%), VT/VF rhythm (29% vs 23%) and ROSC (35% vs 25%).
Table 1.
Demographic characteristics of patients; if the event was witnessed; if bystander CPR was administered; and the location of the event. The table also indicates the presenting rhythm, return of spontaneous circulation (ROSC), survival to hospital discharge, and the distribution of characteristics and variables between the three chest compression rate categories.
| Patient Characteristics | Chest Compression Rate Categories | |||
|---|---|---|---|---|
| All Patients N=3098 |
<80 N=122 |
80–140 N=2763 |
>140 N=213 |
|
| Age, mean (SD) | 66.6 (16) | 62.8 (17) | 66.9 (16) | 65.8 (17) |
| Male, N(%) | 2071 (67) | 88 (72) | 1844 (67) | 139 (65) |
| EMS witnessed arrest, N(%) | 154 (5) | 8 (7) | 130 (5) | 16 (8) |
| Bystander witnessed arrest, N(%) | 1267 (41) | 47 (39) | 1142 (41) | 78 (37) |
| Bystander CPR, N(%) | 1201 (39) | 50 (41) | 1080 (39) | 71 (33) |
| Public Location, N(%) | 534 (17) | 21 (17) | 480 (17) | 33 (15) |
| Presenting Rhythm, N(%) | ||||
| VT/VF | 884 (29) | 39 (32) | 794 (29) | 51 (24) |
| PEA | 690 (22) | 32 (26) | 620 (22) | 38 (18) |
| Asystole | 1381 (45) | 45 (37) | 1234 (45) | 102 (48) |
| AED no shock | 100 (3) | 2 (2) | 81 (3) | 17 (8) |
| Can’t determine/missing | 43 (1) | 4 (3) | 34 (1) | 5 (2) |
| ROSC, N(%) | 1082 (35) | 46 (38) | 972 (35) | 64 (30) |
| Survival to Discharge, N(%) | 265 (9) | 13 (11) | 242 (9) | 10 (5) |
EMS, Emergency Medical Services; CPR, Cardiopulmonary Resuscitation; VT, Ventricular Tachycardia; VF, Ventricular Fibrillation; PEA, Pulseless Electrical Activity; AED, Automatic External Defibrillator; ROSC, return of spontaneous circulation.
Table 2.
Comparison of analyzed cohort with patients excluded from the study.
| Analyzed Cohort N=3098 (%) |
Excluded Patients N=12428 (%) |
P-value (Chi-squared or t-test) | |
|---|---|---|---|
| Age, mean (SD) | 66.6 (± 16) | 67.4 (± 16) | 0.031 |
| Male, N (%) | 2071 (67) | 7771 (63) | <0.001 |
| EMS witnessed arrest, N (%) | 154 (5) | 1203 (10) | <0.001 |
| Bystander witnessed arrest, N (%) | 1267 (41) | 4729 (38) | 0.004 |
| Bystander CPR, N (%) | 1201 (39) | 3711 (30) | <0.001 |
| Public Location, N (%) | 534 (17) | 1875 (15) | 0.003 |
| Presenting Rhythm, N(%) | <0.001 | ||
| VT/VF | 884 (29) | 2889 (23) | |
| PEA | 690 (22) | 2315 (19) | |
| Asystole | 1383 (45) | 4819 (39) | |
| AED no shock | 100 (3) | 1300 (10) | |
| Can’t determine/missing | 43 (1) | 1105 (9) | |
| ROSC, N (%) | 1082 (35) | 3100 (25) | <0.001 |
| Survival to Discharge, N (%) | 265 (8.6) | 975 (7.8) | 0.197 |
EMS, Emergency Medical Services; CPR, Cardiopulmonary Resuscitation; VT, Ventricular Tachycardia; VF, Ventricular Fibrillation; PEA Pulseless Electrical Activity; AED, Automatic External Defibrillator; ROSC, return of spontaneous circulation
Mean chest compression rate was 112 ± 19 compressions/minute (range: 45 – 202) and median was 111 (IQR 100 – 123) during the first five minutes of CPR with rates between sites significantly different (p <0.0001) (Table 3). Mean within subject variability of compression rate from minute to minute was 7 ± 8 compressions/minute (median 5, IQR 3 – 9, N=2,974). In addition, chest compression rates at each of five chest compression fraction quintiles (0 – 20%, 20 – 40%, 40 – 60%, 60 – 80%, and 80 – 100%) were not significantly different (mean range 111 – 113, p = 0.40). Furthermore, there was little correlation between chest compression fraction and chest compression rate (correlation coefficient −0.025, p = 0.16)
Table 3.
Average chest compression rate by site (indicated by letter) for the first five minutes of CPR.
| Overall Average Compression Rate for the First Five Minutes
| ||||||||
|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | Minimum | 25 % tile | Median | 75% tile | Maximum | |
| 3098 | 112 | 19 | 45 | 100 | 111 | 123 | 202 | |
|
| ||||||||
| Average Compression Rate by Site for the First Five Minutes | ||||||||
| Site | N | Mean | SD | Minimum | 25 % tile | Median | 75% tile | Maximum |
| A | 205 | 106 | 22 | 60 | 91 | 105 | 119 | 187 |
| B | 265 | 113 | 20 | 59 | 100 | 110 | 122 | 200 |
| C | 81 | 112 | 23 | 58 | 99 | 111 | 124 | 186 |
| D | 61 | 100 | 17 | 62 | 91 | 98 | 105 | 159 |
| E | 302 | 115 | 22 | 53 | 101 | 114 | 128 | 202 |
| F | 68 | 113 | 23 | 53 | 96 | 114 | 128 | 175 |
| G | 712 | 111 | 16 | 45 | 102 | 110 | 121 | 167 |
| H | 1169 | 112 | 17 | 56 | 102 | 113 | 123 | 175 |
| I | 235 | 113 | 22 | 60 | 98 | 112 | 128 | 192 |
N = number of patients.
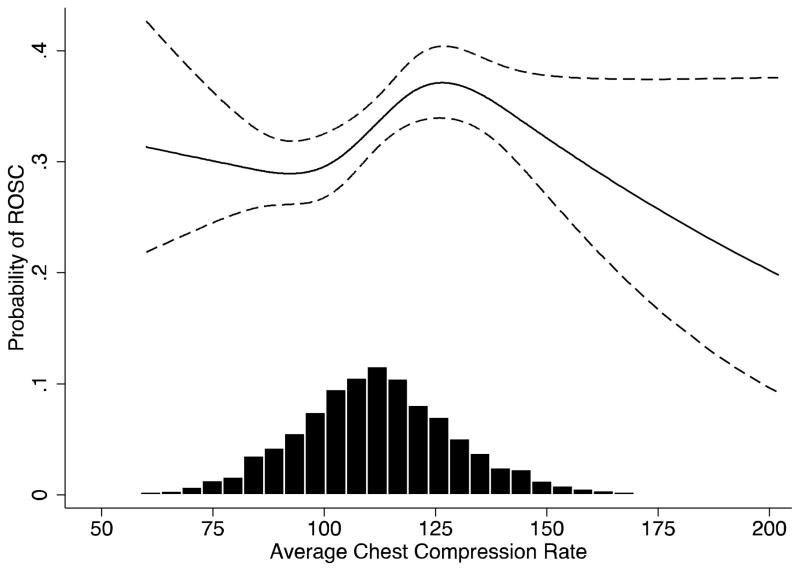
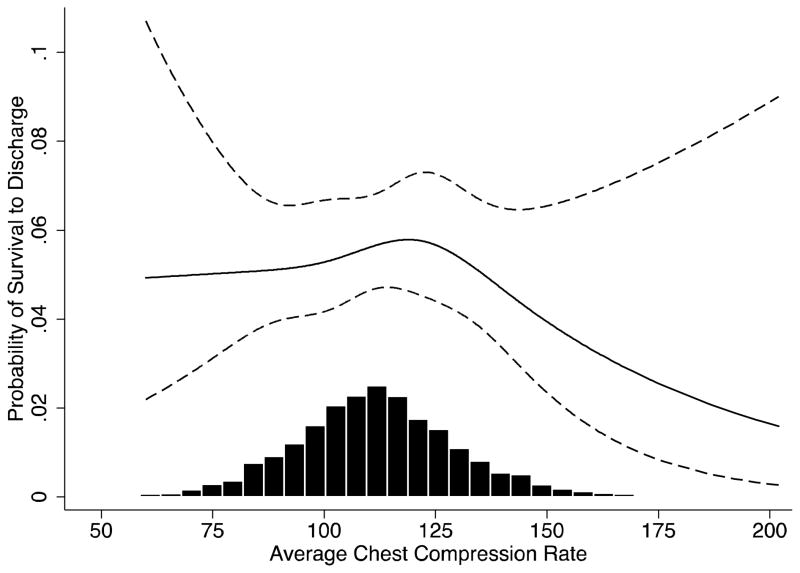
The categorical model showed that patients receiving compression rates >140/minute had an unadjusted odds ratio for survival of 0.51 [95% confidence interval (CI) 0.27 – 0.98, p = 0.04] compared with the reference rate of 80 – 140 compressions/minute, and an adjusted odds ratio of 0.61 (95% CI 0.29 – 1.25, p = 0.18) (Table 4). As well, patients receiving compression rates >140/minute had an unadjusted odds ratio of 0.79 (95% CI 0.58 – 1.07, p = 0.13) for ROSC compared with the reference rate and an adjusted odds ratio of 1.01 (95% CI 0.72 – 1.41, p = 0.96) (Table 4). One-third of cases had a rate of chest compressions >120/minute and 7% of cases had a rate >140/minute. Bystander-witnessed cardiac arrest, EMS-witnessed cardiac arrest, first known EMS rhythm, age, and public location had odds ratios suggesting these variables had important effects on ROSC and survival in the model, while attempted bystander CPR did not (Table 4). A sensitivity analysis that included chest compression fraction in the model did not change the estimated relationship between rate and survival. An adjusted natural cubic spline curve described graphically the relationship between chest compression rate and ROSC over the range of chest compression rates (Figure 3). The curve shows that ROSC peaks at a chest compression rate of about 125/minute and then declines sharply (p = 0.012). Another adjusted cubic spline curve (Figure 4) showed the relationship between chest compression rate and survival to hospital discharge (p = 0.63). The curves were adjusted for bystander-witnessed cardiac arrest, EMS-witnessed cardiac arrest, first known EMS rhythm, attempted bystander CPR, age, and public location (y-axis).
Table 4.
Odds ratios of variables known to affect outcome from cardiac arrest, and the odds ratio of chest compression rate by category. The reference rate category is 80 to 140 compressions/minute.
| ROSC OR (95% CI)* | P-Value | Survival to Discharge OR (95% CI)* | P-Value | |
|---|---|---|---|---|
| Chest compression rate, categories | ||||
| Unadjusted Model | ||||
| 0–80 compressions/min | 1.12 (0.77,1.62) | 0.57 | 1.24 (0.69,2.24) | 0.47 |
| 80–140 compressions/min | Reference | Reference | ||
| 140+ compressions/min | 0.79 (0.58,1.072) | 0.13 | 0.51 (0.27,0.98) | 0.04 |
| Adjusted Model † | ||||
| 0–80 compressions/min | 1.18 (0.78,1.79) | 0.79 | 1.32 (0.67,2.62) | 0.42 |
| 80–140 compressions/min | Reference | Reference | ||
| 140+ compressions/min | 1.01 (0.72,1.41) | 0.96 | 0.61 (0.29,1.25) | 0.18 |
| Global test for chest compression rate categories | vs ROSC | 0.73 | vs Survival | 0.25 |
| Male sex | 0.72 (0.60,0.86) | <0.001 | 0.83 (0.60,1.17) | 0.29 |
| Age (10-year increase) | 0.96 (0.91,1.01) | 0.1 | 0.77 (0.71,0.84) | <0.001 |
| Bystander witnessed arrest | 2.05 (1.71,2.47) | <0.001 | 2.18 (1.54, 3.09) | <0.001 |
| EMS witnessed arrest | 2.04 (1.39, 2.98) | <0.001 | 3.18 (1.68, 6.02) | <0.001 |
| Bystander CPR | 0.93 (0.78, 1.11) | 0.41 | 1.15 (0.85, 1.56) | 0.36 |
| Public location | 1.25 (1.01, 1.55) | 0.04 | 1.83 (1.34, 2.50) | <0.001 |
| Rhythm | ||||
| VT/VF | Reference | Reference | ||
| PEA | 0.43 (0.34,0.54) | <0.001 | 0.22 (0.15,0.32) | <0.001 |
| Asystole | 0.22 (0.17, 0.27) | <0.001 | 0.04 (0.02, 0.07) | <0.001 |
| AED – no shock advised | 0.30 (0.17, 0.52) | <0.001 | 0.07 (0.01, 0.52) | 0.01 |
| Can’t Determine | 0.59 (0.31, 1.12) | 0.11 | 0.24 (0.07, 0.85) | 0.03 |
OR, odds ratio; CI, confidence interval; ROSC, return of spontaneous circulation; EMS, emergency medical services; CPR, cardiopulmonary resuscitation; VT, ventricular tachycardia; VF, ventricular fibrillation; PEA, pulseless electrical activity; AED, automated external defibrillator.
Model includes sex, age, bystander witnessed arrest, EMS witnessed arrest, first known EMS rhythm, attempted bystander CPR, public location, and site location. The number of patients in each category of compressions/min are: <80/min, n = 122 (3.9%); 80 – 140/min, n = 2,763 (89.2%; >140/min, n = 213 (6.9%).
Figure 3.
Adjusted cubic spline of the relationship between chest compression rates and the probability of return of spontaneous circulation (ROSC). The adjusted model includes sex, age, bystander witnessed arrest, EMS witnessed arrest, first known EMS rhythm, attempted bystander CPR, public location, and site location (y-axis). Probability of ROSC versus average chest compression rate when other covariates are equal to the population average. We used a global test, which tested the null hypothesis that the spline curve is a horizontal line (p = 0.012). A histogram of the compression rates and numbers of patients is included. Dashed lines show 95% confidence intervals.
Figure 4.
Adjusted cubic spline of the relationship between chest compression rates and the probability of survival to hospital discharge. The adjusted model includes sex, age, bystander witnessed arrest, EMS witnessed arrest, first known EMS rhythm, attempted bystander CPR, public location, and site location (y-axis). Probability of survival versus average chest compression rate when other covariates are equal to the population average. We used a global test, which tested the null hypothesis that the spline curve is a horizontal line (p = 0.63). A histogram of the compression rates and numbers of patients is included. Dashed lines show 95% confidence intervals.
The number of chest compressions actually delivered each minute combined the effects of chest compression rate and chest compression fraction. The mean number of delivered chest compressions was 74 ± 23 and the median was 75 (IQR 58 – 91) (Table 5). Delivered chest compressions was modeled categorically for <75, 75–100, and >100 compressions delivered each minute. Patients receiving less than 75 compressions each minute had adjusted odds ratios of 0.81 (95% CI 0.68 – 0.98, p = 0.03) for ROSC and 0.78 (95% CI 0.58 – 1.06, p = 0.11) for survival compared with the reference range of 75 – 100 compressions (Table 6). The global test for delivered chest compressions vs ROSC and vs survival, respectively, was p = 0.01 and p = 0.25. Proportionately more patients receiving <75 compressions delivered each minute also had a chest compression rate <80/min (Table 7).
Table 5.
Average number of delivered chest compressions per minute by site (indicated by letter) for the first five minutes of CPR.
| Overall Average Number of Delivered Chest Compressions/min for the First Five Minutes
| |||||
|---|---|---|---|---|---|
| N | Mean | SD | Minimum | Maximum | |
| 3098 | 74 | 23 | 6 | 167 | |
| Average Number of Delivered Chest Compressions by Site for the First Five Minutes | |||||
|
| |||||
| Site | N | Mean | SD | Minimum | Maximum |
| A | 205 | 65 | 22 | 12 | 136 |
| B | 265 | 64 | 21 | 9 | 127 |
| C | 81 | 64 | 24 | 9 | 113 |
| D | 61 | 65 | 21 | 9 | 116 |
| E | 302 | 68 | 21 | 10 | 126 |
| F | 68 | 64 | 28 | 11 | 162 |
| G | 712 | 85 | 20 | 19 | 167 |
| H | 1169 | 76 | 23 | 6 | 143 |
| I | 235 | 72 | 23 | 14 | 135 |
N = number of patients
Table 6.
Odds ratios of delivered chest compressions/min by category.
| ROSC OR (95% CI)* | P-Value | Survival to Discharge OR (95% CI)* | P-Value | |
|---|---|---|---|---|
| Delivered chest compressions, categories | ||||
| Unadjusted Model | ||||
| 0–75 compressions/min | 0.78 (0.66, 0.92) | 0.003 | 0.82 (0.63, 1.07) | 0.14 |
| 75–100 compressions/min | Reference | Reference | ||
| 100+ compressions/min | 0.99 (0.79, 1.26) | 0.96 | 0.64 (0.42, 0.99) | 0.05 |
| Adjusted Model† | ||||
| 0–75 compressions/min | 0.81 (0.68, 0.98) | 0.03 | 0.78 (0.58, 1.06) | 0.11 |
| 75–100 compressions/min | Reference | Reference | ||
| 100+ compressions/min | 1.15 (0.89, 1.49) | 0.28 | 0.77 (0.47, 1.28) | 0.32 |
| Global test for delivered chest compressions | vs ROSC | 0.01 | vs Survival | 0.25 |
OR, odds ratio; CI, confidence interval; ROSC, return of spontaneous circulation; EMS, emergency medical services.
Model includes sex, age, bystander witnessed arrest, EMS witnessed arrest, first known EMS rhythm, attempted bystander CPR, public location, and site location. The number of patients in each category of delivered compression/min are: <75/min, n = 1,555 (50.2%); 75 – 100/min, n = 1,131 (36.5%); >100/min, n = 412 (13.3%).
Table 7.
Average chest compression rates vs. number of delivered chest compressions
| Average Compression Rate/min, N (%) | |||||
|---|---|---|---|---|---|
|
| |||||
| <80 rate | 80–140 | >140 | Total | ||
|
|
|||||
| Average | <75 delivered | 122 (100%) | 1380 (50%) | 53 (25%) | 1555 (50%) |
| Delivered | 75–100 | 0 | 1056 (38%) | 75 (35%) | 1131 (37%) |
| Compressions/min | >100 | 0 | 327 (12%) | 85 (40%) | 412 (13%) |
| Total | 122 (100%) | 2763 (100%) | 213 (100%) | 3098 (100%) | |
Chi squared p<0.001; N = number of patients
Chest compression depth was measured in 362 of 3,098 patients (11.7%). There was a significant relationship between chest compression rate and depth (p = 0.03) (Table 8).21 Depth declined with increasing chest compression rates. However, a sensitivity analysis that included depth in the model did not change the estimated relationship between rate and ROSC or between rate and survival.
Table 8.
Average chest compression depth vs. chest compression rate/min.
| Average Compression Rate, N (%) | |||||
|---|---|---|---|---|---|
|
| |||||
| <80 rate | 81–140 | >140 | Total | ||
|
|
|||||
| Average | <38 | 8 (42%) | 171 (52%) | 14 (82%) | 193 (53%) |
| Compression | 38–51 | 6 (32%) | 122 (38%) | 3 (18%) | 131 (36%) |
| Depth (mm) | >51 | 5 (26%) | 33 (10%) | 0 (0%) | 38 (11%) |
| Total | 19 (100%) | 326 (100%) | 17 (5%) | 362 (100%) | |
Fisher’s Exact Test (for association): p=0.03
N = number of patients
Discussion
This large, observational, multi-center study showed that the likelihood of ROSC peaks at a chest compression rate of about 125/minute during the first five minutes of OOH CPR. However, we were unable to confirm a significant relationship between chest compression rate and survival to hospital discharge. The study also demonstrates that EMS rescuers frequently apply rates greater than 100/minute with rates greater than 120/minute occurring in one-third of cases. Faster than recommended chest compression rates have been reported previously and likely occur frequently.6,8 Animal studies showed chest compression rates of 120/minute were associated with improved blood flow and survival, while rates faster than that were associated with decreased
blood flow.12 –14 Similarly, human studies also showed improved blood flow and end-tidal CO2 levels (a surrogate for blood flow) with a chest compression rate of 120/minute.17,18,22 In contrast to rate studies, a CPR study of humans with in-hospital cardiac arrest measured and reported the actual number of compressions delivered each minute, which is a product of chest compression rate and chest compression fraction (the proportion of each minute spent doing chest compressions).19 This study found that patients who received 90 delivered chest compressions each minute had a significantly greater rate of ROSC compared with those who received only 79 compressions.19
The current study found that patients receiving less than 75 chest compressions each minute had a decreased likelihood of ROSC, possibly because it reflected lower chest compression rates and more interruptions in chest compressions (Table 7). Interruptions in chest compressions are commonly observed, even in a high-performance EMS system6 and an average chest compression fraction of 0.70 to 0.80 may be the best that can be achieved during conventional CPR. A study of OOH CPR found that the proportion of time that chest compression is given during each minute is associated with survival to hospital discharge and that survival was greatest when chest compressions were given 60% to 80% of the time.7 While analysis of the number of delivered chest compressions per minute provides important insight into overall quality of CPR, this measurement is not displayed on most defibrillators and, therefore, use of chest compression rate for feedback and monitoring is more applicable to clinical practice.
The use of metronomes as well as real-time feedback during CPR has been shown to be useful and effective in helping rescuers maintain a desired chest compression rate.8,18
Limitations
There are factors regarding the quality of CPR that are known to affect ROSC and survival that were not available for analysis in the current study including chest compression depth and incomplete recoil (leaning). The amount of leaning was not abstracted in our database and chest compression depth could not be analyzed completely because of insufficient numbers of electronic files captured from devices capable of recording compression depth. However, in the subset of patients in which depth was measured, depth was found to decrease significantly with increasing chest compression rates (Table 8).21 Measurement of depth was available for only 12% of cases in the analysis group, which is an important limitation that could affect results in this study.
The percentage of eligible patients who had electronic CPR process files was only about 20% of all treated cases, which may produce a selection bias. We compared the cohort in the analysis with those who had CPR, but were not included and found differences in proportions whose cardiac arrest was witnessed, received bystander CPR, or occurred in a public location, and differences in presenting rhythm and ROSC rate, but not survival (Table 2). A larger percentage of patients in the analyzed cohort had ROSC, however we did not find a significant relationship between ROSC and chest compression rate in the categorical multivariate analysis. If the association between compression rate and outcome is different in the excluded cases than in those included in the analysis, the bias produced by this exclusion would be large.
Furthermore, a mandatory condition for participation in the ROC Epistry was that agencies had to use devices capable of recording chest compressions and interruptions in chest compressions. It is possible that non-ROC communities in North America using devices incapable of recording chest compressions could have different results related to differences in socioeconomic status.
While our study suggests a positive association of ROSC with chest compression rates within a relatively defined range, a larger study with fewer excluded patients would help to confirm these findings.
Certain monitor-defibrillators are capable of providing feedback with respect to chest compression rate and depth and seven of nine ROC sites had such monitors. The feedback feature was turned on during CPR in 12% of all patients included in this study. A trial of real-time feedback in a similar group of patients showed that average chest compression rates were 104/minute with and 109/minute without feedback turned on, respectively, a difference that is probably not clinically important.23
Another limitation was that only the first five minutes of CPR were analyzed, but some patients had substantially longer periods of CPR, which could be an effect modifying variable. A prior study, however, showed that chest compressions during the first five minutes of CPR was similar to subsequent minutes of CPR.24
Conclusions
The likelihood of return of spontaneous circulation during CPR for out-of-hospital cardiac arrest was greatest with use of a chest compression rate of about 125 compressions/minute and then declined at higher rates. The association between chest compression rate and survival was not significant after adjusting for confounding variables.
Clinical Summary.
Guidelines for cardiopulmonary resuscitation (CPR) recommend a chest compression rate of at least 100 compressions/min, but do not provide an upper limit for rate because of lack of evidence from human studies with return of spontaneous circulation (ROSC) or survival as outcomes. In this study we describe chest compression rates used by emergency medical services (EMS) providers to resuscitate patients with OOH cardiac arrest and we sought to determine the relationship between chest compression rate and return of spontaneous circulation and survival. This study used data from the Resuscitation Outcomes Consortium (ROC) Epidemiologic Cardiac Arrest Registry database. The study included over 3,000 patients who had OOH cardiac arrest and CPR. The investigators found that 75% of rescuers used chest compression rates that exceeded 100/min and one-third used rates >120/min. Depth of chest compressions is an important factor related to CPR quality and survival. We found that chest compression depth decreases when chest compression rate exceeds 140/minute. This study found that the likelihood of ROSC from out-of-hospital cardiac arrest was greatest with use of a chest compression rate of about 125 compressions/min and then declines sharply with faster rates. By using chest compression rates of at least 100/minute but no faster than 125/minute, we can further improve ROSC.
Acknowledgments
We are indebted to the firefighters and paramedics participating in the ROC for their hard work and dedication. We would also like to thank the data coordinators at each ROC site for their extraordinary diligence and focus in abstracting the data for this study.
Funding Sources: This study was supported by a series of cooperative agreements to 10 regional clinical centers and one Data Coordinating Center (5U01 HL077863-University of Washington Data Coordinating Center, HL077865-University of Iowa, HL077866-Medical College of Wisconsin, HL077867 University of Washington, HL077871-University of Pittsburgh, HL077872-St. Michael’s Hospital, HL077873-Oregon Health and Science University, HL077881-University of Alabama at Birmingham, HL077885-Ottawa Health Research Institute, HL077887-University of Texas Southwestern Medical Center at Dallas, HL077908-University of California San Diego) from the National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, the American Heart Association, U.S. Army Medical Research & Materiel Command, the Canadian Institutes of Health Research (CIHR) - Institute of Circulatory and Respiratory Health, the Heart, Stroke Foundation of Canada, and Defence Research and Development Canada.
Footnotes
Conflict of Interest Disclosures: Drs. Idris, Aufderheide, Brown, Daya, Morrison, Davis, Stiell, and Nichol, as well as Danielle Guffey and Judy Powell, receive ROC grant funding. Dr. Aufderheide receives grant funding from NHLBI and NINDS; he is a consultant for Jolife and Medtronics and is a board member for Take Heart America and for the Citizen CPR Foundation. Drs. Idris, Aufderheide, Daya, Morrison, Atkins, and Nichol are volunteers for the American Heart Association National Emergency Cardiovascular Care Committee. Drs. Daya and Idris are unpaid consultants for Philips Medical Systems. Dr. Nichol has research grant funding from the Asmund S. Laerdal Foundation for Acute Medicine, and Medtronic, Inc.
References
- 1.Berg RA, Hemphill R, Abella BS, Aufderheide TP, Cave DM, Hazinski MF, Lerner EB, Rea TD, Sayre MR, Swor RA. Part 5: Adult basic life support. 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:S685–S705. doi: 10.1161/CIRCULATIONAHA.110.970939. [DOI] [PubMed] [Google Scholar]
- 2.Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed-chest cardiac massage. JAMA. 1960;173:1064–1067. doi: 10.1001/jama.1960.03020280004002. [DOI] [PubMed] [Google Scholar]
- 3.Cardiopulmonary resuscitation: Statement by the Ad Hoc Committee on Cardiopulmonary Resuscitation of the Division of Medical Sciences, National Academy of Sciences – National Research Council. JAMA. 1966;198:138–145. [Google Scholar]
- 4.Standards and guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiac care (ECC) JAMA. 1986;255:2905–2984. [PubMed] [Google Scholar]
- 5.Koster RW, Baubin MA, Bossaert LL, Caballero A, Cassa P, Castrén M, Granja C, Handley AJ, Monsieurs KG, Perkins GD, Raffay V, Sandroni C. European Resuscitation Council guidelines for resuscitation 2010. Section 2: Adult basic life support and use of automated external defibrillators. Resuscitation. 2010;81:1277–1292. doi: 10.1016/j.resuscitation.2010.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wik L, Kramer-Johansen J, Myklebust H, Sorebo H, Svensson L, Fellows B, Steen PA. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. JAMA. 2005;293:299–304. doi: 10.1001/jama.293.3.299. [DOI] [PubMed] [Google Scholar]
- 7.Christenson J, Andrusiek D, Everson-Stewart S, Kudenchuk P, Hostler D, Powell J, Callaway CW, Bishop D, Vaillancourt C, Aufderheide TP, Idris A, Stoufer JA, Stiell I, Berg R Resuscitation Outcomes Consortium Investigators. Chest Compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009;120:1241–1247. doi: 10.1161/CIRCULATIONAHA.109.852202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fletcher D, Galloway R, Chamberlain D, Pateman J, Bryant G, Newcombe RG. Basics in advanced life support: A role for download audit and metronomes. Resuscitation. 2008;78:127–134. doi: 10.1016/j.resuscitation.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Davis DP, Garberson LA, Andrusiek DL, Hostler D, Daya M, Pirrallo R, Craig A, Stephens S, Larsen J, Drum AF, Fowler R. A descriptive analysis of Emergency Medical Service Systems participating in the Resuscitation Outcomes Consortium (ROC) network. Prehosp Emerg Care. 2007;11:369–382. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 10.Morrison LJ, Nichol G, Rea TD, Christenson J, Callaway CW, Stephens S, Pirrallo RG, Atkins DL, Davis DP, Idris AH, Newgard C. Rationale, development and implementation of the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Resuscitation. 2008;78:161–169. doi: 10.1016/j.resuscitation.2008.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stecher FS, Olsen JA, Stickney RE, Wik L. Transthoracic impedance used to evaluate performance of cardiopulmonary resuscitation during out of hospital cardiac arrest. Resuscitation. 2008;79:432–437. doi: 10.1016/j.resuscitation.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 12.Harris LC, Kirimli B, Safar P. Ventilation-cardiac compression rates and ratios in cardiopulmonary resusucitation. Anesthesiology. 1967;2:806–813. doi: 10.1097/00000542-196709000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Maier GW, Tyson GS, Jr, Olsen CO, Kernstein KH, Davis JW, Conn EH, Sabiston DC, Jr, Rankin JS. The physiology of external cardiac massage: high-impulse cardiopulmonary resuscitation. Circulation. 1984;70:86–101. doi: 10.1161/01.cir.70.1.86. [DOI] [PubMed] [Google Scholar]
- 14.Feneley MP, Maier GW, Kern KB, Gaynor JW, Gall SA, JR, Sanders AB, Raessler K, Muhlbaier LH, Rankin JS, Ewy GA. Influence of compression rate on initial success of resuscitation and 24 hour survival after prolonged manual cardiopulmonary resuscitation in dogs. Circulation. 1988;77:240–250. doi: 10.1161/01.cir.77.1.240. [DOI] [PubMed] [Google Scholar]
- 15.Fitzgerald KR, Babbs CF, Frissora HA, Davis RW, Silver DI. Cardiac output during cardiopulmonary resuscitation at various compression rates and durations. Am J Physiol. 1981;241:H442–448. doi: 10.1152/ajpheart.1981.241.3.H442. [DOI] [PubMed] [Google Scholar]
- 16.Wolfe JA, Maier GW, Newton JR, Glower DD, Tyson GS, Jr, Spratt JA, Rankin JS, Olsen CO. Physiologic determinants of coronary blood flow during external cardiac massage. J Thorac Cardiovasc Surg. 1988;95:523. [PubMed] [Google Scholar]
- 17.Swenson RD, Weaver WD, Niskanen RA, Martin J, Dahlberg S. Hemodynamics in humans during conventional and experimental methods of cardiopulmonary resuscitation. Circulation. 1988;78:630–639. doi: 10.1161/01.cir.78.3.630. [DOI] [PubMed] [Google Scholar]
- 18.Kern KB, Sanders AB, Raife J, Milander MM, Otto CW, Ewy GA. A study of chest compression rates during cardiopulmonary resuscitation in humans. The importance of rate-directed chest compressions. Arch Int Med. 1992;15:145–149. [PubMed] [Google Scholar]
- 19.Abella BS, Sandbo N, Vassilatos P, Alvarado JP, O’Hearn N, Wigder HN, Hoffman P, Tynus K, Vanden Hoek TL, Becker LB. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation. 2005;111:428–434. doi: 10.1161/01.CIR.0000153811.84257.59. [DOI] [PubMed] [Google Scholar]
- 20.Chambers JM, Hastie T. Statistical models in S. Pacific Grove, Calif: Wadsworth & Brooks/Cole Advanced Books & Software; 1992. [Google Scholar]
- 21.Stiell IG, Brown SP, Christenson J, Cheskes S, Nichol G, Powell J, Bigham B, Morrison LJ, Larsen J, Hess E, Vaillancourt C, Davis DP, Callaway CW the Resuscitation Outcomes Consortium (ROC) Investigators. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit Care Med. 2012;40 doi: 10.1097/CCM.0b013e31823bc8bb. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Idris AH, Staples E, O’Brien D, Melker RJ, Rush W, Del Duca KJ, Falk J. End-tidal carbon dioxide during extremely low cardiac output. Annals of Emergency Medicine. 1994;23:568–572. doi: 10.1016/s0196-0644(94)70080-x. [DOI] [PubMed] [Google Scholar]
- 23.Hostler D, Everson-Stewart S, Rea TD, Stiell G, Callaway CW, Kudenchuk PJ, Sears GK, Emerson SS, Nichol G Resuscitation Outcomes Consortium Investigators. Effect of real-time feedback during cardiopulmonary resuscitation outside hospital: prospective, cluster-randomised trial. BMJ. 2011;342:d512. doi: 10.1136/bmj.d512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Valenzuela TD, Kern KB, Clark LL, Berg RA, Berg MD, Berg DD, Hilwig RW, Otto CW, Newburn D, Ewy GA. Interruptions of chest compressions during emergency medical systems resuscitation. Circulation. 2005;112:1259–1265. doi: 10.1161/CIRCULATIONAHA.105.537282. [DOI] [PubMed] [Google Scholar]