Abstract
Background
Multimorbidity is now acknowledged as a research priority in primary care. The identification of risk factors and people most at risk is an important step in guiding prevention and intervention strategies. The aim of this study was to examine the relationship between literacy and multimorbidity while controlling for potential confounders.
Methods
Participants were adult patients attending the family medicine clinic of a regional health centre in Saguenay (Quebec), Canada. Literacy was measured with the Newest Vital Sign (NVS). Multimorbidity was measured with the Disease Burden Morbidity Assessment (DBMA) by self-report. Information on potential confounders (age, sex, education and family income) was also collected. The association between literacy (independent variable) and multimorbidity was examined in bivariate and multivariate analyses. Two operational definitions of multimorbidity were used successively as the dependent variable; confounding variables were introduced into the model as potential predictors.
Results
One hundred three patients (36 men) 19–83 years old were recruited; 41.8% had completed 12 years of school or less. Forty-seven percent of patients provided fewer than four correct answers on the NVS (possible low literacy) whereas 53% had four correct responses or more. Literacy and multimorbidity were associated in bivariate analyses (p < 0.01) but not in multivariate analyses, including age and family income.
Conclusion
This study suggests that there is no relationship between literacy and multimorbidity when controlling for age and family income.
Background
Multimorbidity, the coexistence of two or more chronic diseases in the same patient, has received growing interest in the primary care literature over the past few years and is now acknowledged by many as a research priority [1-6]. Patients with multimorbidity seen in family practice represent the rule rather than the exception [7-9]. These patients are more likely to present poor health outcomes such as a decrease in quality of life [10], increased psychological distress [11], more postsurgical complications [12], longer hospitalisations [13,14], and higher rates of mortality [15,16].
In the wake of prevention and intervention strategies to address this issue, the identification of risk factors and of people most at risk is an important aspect. Aging [7,9] and low socioeconomic status [8,9,17,18] are already clearly associated with an increased incidence of multimorbidity. Without directly measuring multimorbidity, many studies have also assessed a relationship between low literacy and poorer health status using global health measures [19-26] which raises the possibility of an independent association between literacy or health literacy and multimorbidity.
The Institute of Medicine defines health literacy as “the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions” [27]. This definition presents health literacy as a set of individual capacities that allow the person to acquire and use new information [28]. Others have argued that health literacy is the ability to function in the health care environment and depends on characteristics of both the individual and the health care system [28]. In both cases, individual capacity, including reading fluency and prior knowledge, have an influence on health literacy [28]. Reading fluency, or literacy [29], is the ability to mentally process written materials and form new knowledge. The first National Adult Literacy Study [30] divided literacy into three skill sets: 1) the ability to read and understand text; 2) the ability to locate and use information in documents; and 3) the ability to apply arithmetic operations and use numerical information in printed materials.
Notwithstanding the interest in looking into a potential association between health literacy and different health outcomes such as multimorbidity, health literacy is easier to conceptualize than to measure. Even if valid measures of literacy exist, a measure that accurately depicts the multiple dimensions of health literacy is still needed [28,31]. Most studies measuring an association with outcomes used a measure of literacy.
A low level of literacy has been linked to several negative health outcomes in patients: poorer knowledge of their health problems [32-35], poorer health status, and higher hospitalization rates [36,37], than those having an adequate level of literacy. Inadequate literacy has also been associated with problems with the use of preventive services [38], delayed diagnoses [39], and all-cause mortality among community dwelling older aged people [40,41].
The aim of this study was to evaluate the relationship between literacy and multimorbidity while controlling for potential confounders.
Methods
Study design and setting
A descriptive study was conducted among patients attending a family medicine clinic of a regional health centre in Saguenay (Québec), Canada. The Saguenay region’s population is approximately 150,000 living in one major city and several smaller boroughs. The Saguenay region has about 130 general practitioners, nearly 80% of whom have a general practice and work in a private office or a public institution. The present study was carried out in an institutional practice (Centre de santé et de services sociaux de Chicoutimi) where 12 family doctors and four nurses provide their services to 9,000 registered patients.
Participants and sampling
The sampling process took place during 10 four-hour sessions over a two-week period. Patients solicited were asked to complete a short questionnaire to determine eligibility. To be included in the study, participants had to be aged 18 years or older and regular patients of the family medicine clinic.
Patients were excluded if they presented an unstable acute or psychiatric condition, or if they were pregnant or unable to provide informed consent. Non eligible patients were thanked for completing the short questionnaire for eligibility and no further action was taken with them.
Instruments
Literacy was measured with the Newest Vital Sign (NVS) [42]. The NVS consists of a nutrition label from an ice cream container. The label is given to the patient, who is then asked six questions about it. The first four questions require document and quantitative skills, including the ability to calculate percentages. It takes approximately three minutes to administer. The NVS is reliable (Cronbach alpha > 0.76) and correlated with the Test of Functional Health Literacy in Adults (TOFHLA), another instrument measuring literacy [42]. The NVS is a markedly better predictor of patients with low literacy than education or age alone. Patients with four correct responses or more are considered as having adequate literacy whereas fewer than four correct answers indicate low literacy. The NVS was treated as a dichotomous variable: 1) low literacy (NVS < 4), and 2) adequate literacy (NVS ≥ 4) [42].
Multimorbidity was measured with a simplified version of the Disease Burden Morbidity Assessment (DBMA) by self-report described by Bayliss and colleagues [43]. The original instrument includes 21 diseases. For this study, only 11 diseases with a high prevalence in our setting were kept in order to reduce the time needed to complete the questionnaire: hypertension, hyperlipidemia, asthma, chronic obstructive pulmonary disease, diabetes, osteoarthritis, back pain, other musculoskeletal conditions, overweight, angina/coronary artery disease, and congestive heart failure. To assess their disease burden, patients identified in the list of 11 conditions those that they had, and rated the interference of each condition with daily activities on a five-point scale from 1 (“not at all”) to 5 (“a lot”). The total multimorbidity score is the sum of conditions weighed by the level of interference assigned to each. The original DBMA was found to be strongly associated with subjective health status [43].
Two operational definitions of multimorbidity were used: 1) the DBMA score while considering all 11 conditions (DBMA 11); 2) the DBMA score while taking into account only six conditions, which were considered to be associated with lifestyle habits or that have been reported as independently associated with inadequate literacy [44,45]: hypertension, hyperlipidemia, diabetes mellitus, overweight, angina/coronary artery disease, and congestive heart failure (DBMA 6). The latter operational definition of multimorbidity was computed to have a multimorbidity measure that, at least theoretically, could be associated with literacy.
Data collection
The patients were recruited in the waiting room of a family medicine clinic. A research assistant approached each patient to explain the project. All subjects who refused to participate did it at this point, and no data were collected from them. Patients who agreed to participate and met all eligibility criteria were brought to a small separate room where the research assistant obtained their written consent, collected sociodemographic data (sex, age, education and family income), and administered both the NVS and the DBMA. The responses to the NVS were collected by the research assistant while the DBMA questionnaire was completed by the patient in the presence of the research assistant who helped them, if needed (for example, reading the questionnaire to patients who did not have their glasses). Filling out the questionnaires took no more than 10 min. Participants did not receive any payment for participating in the study.
The study was approved by the research ethics board of the Centre de santé et de services sociaux de Chicoutimi.
Data analysis
The associations between multimorbidity (dependent variable) and the other variables (age, sex, education, family income and NVS) were first examined in bivariate analyses. In a multivariate general linear modeling analysis, both operational definitions of multimorbidity were used successively as dependent variable, and the variables with a significant relationship with multimorbidity in the bivariate analysis were used as potential predictors in the model. Correlations between predictor variables were examined to determine the presence of collinearity.
All analyses were performed with PASW Statistics 18 (SPSS Inc.). The α significance level was set at 0.05.
Results
A total of 103 patients (36 men) between 19 and 83 years of age participated in the study; 41.8% had a 12-year or less school education and 30.1% had completed university studies (Table 1). Forty-eight percent of patients had a NVS score within the range of limited literacy (NVS < 4), and 52% had adequate health literacy. The number of subjects with and without multimorbidity was well distributed across the sample (Table 1).
Table 1.
Characteristics of the sample
| Characteristic | Participants n = 103 |
|---|---|
| Mean (SD) age, years |
49.9 (7.1) |
| Male, % |
35.0 |
| NVS < 4, % |
47.6 |
| NVS ≥ 4, % |
52.4 |
| DBMA 11. Mean (SD) |
5.8 (6.5) |
| DBMA 6, Mean (SD) |
2.5 (3.2) |
| 0 or 1 disease, % |
42.7 |
| 2 or more diseases, % |
57.3 |
| Education, % |
|
| ≤ 12 years |
41.8 |
| College |
27.2 |
| University |
30.1 |
| Missing data |
1.0 |
| Household income in Canadian dollars, % |
|
| < $10,000 |
5.8 |
| $10,000-$29,999 |
18.4 |
| $30,000-$49,999 |
31.0 |
| ≥ $50,000 |
41.7 |
| Missing data | 2.9 |
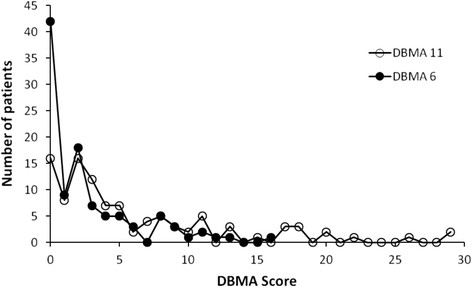
The scores of both operational definitions of multimorbidity showed a wide distribution across the sample. Figure 1 shows the distribution of each definition of multimorbidity score. As expected, the DBMA 11 had the widest variation, with a range of 0–29 and a median of three; the DBMA 6 varied from 0–13 with a median of two. The distribution of both operational definitions of multimorbidity followed a similar trend, the most striking difference being that 16 patients (15.5%) had a DBMA 11 score of zero whereas the number of patients with a DBMA 6 score of zero was 42 (40.8). This was also an expected finding due to the smaller number of chronic conditions considered in the DBMA 6.
Figure 1.
Distribution of scores on operational definitions of multimorbidity. DBMA = Disease Burden Morbidity Assessment (see text for description of chronic conditions considered in DBMA 11 and DBMA 6).
In bivariate analyses, age, family income, and literacy were linked to both operational definitions of multimorbidity. There was no association between sex or education and multimorbidity (Table 2).
Table 2.
Results of bivariate analyses
| Multimorbidity measure | ||||
|---|---|---|---|---|
|
Variable |
DBMA 11 |
DBMA 6 |
||
| |
β† |
p value |
β† |
p value |
| Age |
0.439 |
< 0.01 |
0.490 |
< 0.01 |
| Sex |
−0.004 |
0.97 |
0.061 |
0.55 |
| Education |
−0.185 |
0.06 |
−0.039 |
0.70 |
| Income |
−0.394 |
< 0.01 |
−0.286 |
< 0.01 |
| NVS | −0.334 | < 0.01 | −0.214 | 0.04 |
† β = regression coefficient.
In multivariate analyses, only age and family income were associated with both operational definitions of multimorbidity (Table 3). Literacy was no longer related to multimorbidity when age and family income were introduced into the model. No collinearity was found among the predictor variables.
Table 3.
Results of multivariate analyses
| Multimorbidity measure | ||||
|---|---|---|---|---|
| |
DBMA 11 |
DBMA 6 |
||
|
Variable |
β† |
p value |
β† |
p value |
| Age |
0.40 |
< 0.01 |
0.47 |
< 0.01 |
| Sex |
−0.02 |
0.82 |
0.02 |
0.83 |
| Education |
−0.07 |
0.46 |
0.03 |
0.76 |
| Income |
−0.31 |
< 0.01 |
−0.21 |
0.02 |
| NVS | −0.08 | 0.41 | −0.02 | 0.87 |
† β = regression coefficient.
Discussion
To our knowledge, this is the first publication addressing the relationship between literacy and multimorbidity. The results of the study suggest that low literacy is associated with the presence of multimorbidity in adults consulting in primary care in bivariate analysis, but this association is no longer present when controlling for age and family income.
Many previous studies have indicated that patients with low literacy were more likely to report poorer health than patients with adequate literacy [19-26], while other studies found no relationship between literacy and health status when controlling for education [46,47]. Many studies were conducted in older aged patients [21,23-25,46,47] making generalization of results to other age groups difficult. One study did not adjust for confounding variables [21]. In another study [20], literacy was not evaluated with a validated tool but by the staff of the institution where the study was carried out. In all studies, health status was evaluated globally using self-rated health status categories. In this research, we used a more detailed instrument to measure patients’ disease burden than the studies supporting the existence of a relationship between health literacy and global health measures.
Other research has addressed the relationship between literacy and specific diseases with inconsistent results. One study reported that inadequate literacy (measured with the short form of the Test of Functional Health Literacy in Adults) was an independent predictor of diabetes mellitus and heart failure but not hypertension, arthritis or pulmonary disease, while adjusting for sociodemographic variables (age, sex, race/ethnicity, education and annual income), health risk behaviours (smoking habit and alcohol use), and body mass index [45]. Another study using the same measure of literacy found that heart attack, stroke, hypertension, diabetes, arthritis and depression were all associated with the literacy level [48]. A study accounting for hypertension, diabetes, obesity and depression concluded that only depression remained significantly associated with literacy after adjusting for confounders [46]. Another study reported that individuals with low literacy had significantly higher rates of arthritis and hypertension, but no statistical differences were found in the prevalence of diabetes, pulmonary, or heart disease [25].
A low level of literacy may be linked to certain health issues and not others. As our measure of multimorbidity evaluated chronic diseases as a whole as well as their severity, we may not have detected a link because of the presence of specific health issues not associated with literacy. An association between literacy and multimorbidity may exist when two or more specific diseases individually related to health literacy coexist in one person. The conceptualization and measure of multimorbidity could therefore have an impact on this association. That is why we conducted analysis using two distinctive conceptualizations and measures, in order to verify if results were different. It was not the case.
We found that multimorbidity was associated with age and family income in the multivariate models. The association of multimorbidity with age is well recognized [7-9,49]. The relationship between socioeconomic status and multimorbidity has also been extensively documented [8,9,17,18].
Our results do not allow us to rule on a potential association between health literacy, a more global concept than literacy [28,31], and multimorbidity. A comprehensive measure of health literacy that considers other dimensions of the concept still needs to be developed. We could then verify if there is a link between health literacy and multimorbidity. Although we did not observe a direct association between literacy and multimorbidity, it is still important to continue taking this variable into account in patient care in order to tailor health information to patient needs and in a format they can understand [42].
A limitation of this study is that participants were not randomly selected from the general population. We recruited patients from the waiting room of a single primary care setting. This method may over sample complex patients with several diseases or frequent attendees. However, we were able to recruit a group of patients with a good distribution of multimorbidity and literacy. Another limitation is the lack of statistical power to carry out multivariate analysis by individual disease. Although the study was conducted in one family practice, we expect the same results from similar primary care settings.
In conclusion, this study suggests that there is no relationship between literacy and multimorbidity when controlling for age and family income. Patients with multimorbidity may have specific diseases that are associated with low literacy. Further studies are needed to identify individual diseases and combinations of diseases linked to literacy while controlling for potential confounding variables. A possible association between health literacy and multimorbidity still needs to be explored when a comprehensive measure of health literacy is available.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
CH, MF and M-EP conceived and designed the study. MF supervised the data collection, participated in the data analysis and helped draft the manuscript. M-EP participated in the data collection and analysis and critically reviewed the manuscript. JA and CH analyzed the data and drafted the manuscript. All authors read and gave their final approval of the version of the manuscript submitted for publication. CH takes responsibility for the integrity of the work as a whole.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Catherine Hudon, Email: Catherine.Hudon@USherbrooke.ca.
Martin Fortin, Email: Martin.Fortin@USherbrooke.ca.
Marie-Eve Poitras, Email: Marie-Eve.Poitras@USherbrooke.ca.
José Almirall, Email: Jose.Almirall@USherbrooke.ca.
Acknowledgements
Martin Fortin is funded by the Canadian Institutes of Health Research and partners (Applied CIHR Chair on Health Services and Policy Research on chronic diseases in primary care/CIHR-IHSPR-CHSRF-CSSSC).
References
- Fortin M, Stewart M, Poitras M-E, Almirall J, Maddocks H. A Systematic Review of Prevalence Studies on Multimorbidity: Toward a More Uniform Methodology. Ann Fam Med. 2012;10:142–151. doi: 10.1370/afm.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starfield B. Global health, equity, and primary care. J Am Board Fam Med. 2007;20:511–513. doi: 10.3122/jabfm.2007.06.070176. [DOI] [PubMed] [Google Scholar]
- Listening for Direction. A National Consultation on Health Services and Policy Issues. , ; [http://www.cihr-irsc.gc.ca/e/20461.html] [Google Scholar]
- Valderas JM, Starfield B, Roland M. Multimorbidity's many challenges: A research priority in the UK. BMJ. 2007;334:1128. doi: 10.1136/bmj.39226.427095.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortin M, Soubhi H, Hudon C, Bayliss EA, van den Akker M. Multimorbidity's many challenges. BMJ. 2007;334:1016–1017. doi: 10.1136/bmj.39201.463819.2C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenberg NE, Kim H, Edwards W, Fleming ST. Burden of common multiple-morbidity constellations on out-of-pocket medical expenditures among older adults. Gerontologist. 2007;47:423–437. doi: 10.1093/geront/47.4.423. [DOI] [PubMed] [Google Scholar]
- Fortin M, Bravo G, Hudon C, Vanasse A, Lapointe L. Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med. 2005;3:223–228. doi: 10.1370/afm.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Akker M, Buntinx F, Metsemakers JF, Roos S, Knottnerus JA. Multimorbidity in general practice: prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. J Clin Epidemiol. 1998;51:367–375. doi: 10.1016/S0895-4356(97)00306-5. [DOI] [PubMed] [Google Scholar]
- Uijen AA, van de Lisdonk EH. Multimorbidity in primary care: prevalence and trend over the last 20 years. Eur J Gen Pract. 2008;1:28–32. doi: 10.1080/13814780802436093. [DOI] [PubMed] [Google Scholar]
- Fortin M, Bravo G, Hudon C, Lapointe L, Almirall J, Dubois MF, Vanasse A. Relationship between multimorbidity and health-related quality of life of patients in primary care. Qual Life Res. 2006;15:83–91. doi: 10.1007/s11136-005-8661-z. [DOI] [PubMed] [Google Scholar]
- Fortin M, Bravo G, Hudon C, Lapointe L, Dubois MF, Almirall J. Relationship between psychological distress and multimorbidity of patients in family practice. Ann Fam Med. 2006;4:417–422. doi: 10.1370/afm.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield S, Apolone G, McNeil BJ, Cleary PD. The importance of co-existent disease in the occurrence of postoperative complications and one-year recovery in patients undergoing total hip replacement. Comorbidity and outcomes after hip replacement. Med Care. 1993;31:141–154. doi: 10.1097/00005650-199302000-00005. [DOI] [PubMed] [Google Scholar]
- Librero J, Peiro S, Ordinana R. Chronic comorbidity and outcomes of hospital care: length of stay, mortality, and readmission at 30 and 365 days. J Clin Epidemiol. 1999;52:171–179. doi: 10.1016/S0895-4356(98)00160-7. [DOI] [PubMed] [Google Scholar]
- Rochon PA, Katz JN, Morrow LA, McGlinchey-Berroth R, Ahlquist MM, Sarkarati M, Minaker KL. Comorbid illness is associated with survival and length of hospital stay in patients with chronic disability. A prospective comparison of three comorbidity indices. Med Care. 1996;34:1093–1101. doi: 10.1097/00005650-199611000-00004. [DOI] [PubMed] [Google Scholar]
- Incalzi RA, Capparella O, Gemma A, Landi F, Bruno E, Di Meo F, Carbonin P. The interaction between age and comorbidity contributes to predicting the mortality of geriatric patients in the acute-care hospital. J Intern Med. 1997;242:291–298. doi: 10.1046/j.1365-2796.1997.00132.x. [DOI] [PubMed] [Google Scholar]
- Poses RM, McClish DK, Smith WR, Bekes C, Scott WE. Prediction of survival of critically ill patients by admission comorbidity. J Clin Epidemiol. 1996;49:743–747. doi: 10.1016/0895-4356(96)00021-2. [DOI] [PubMed] [Google Scholar]
- Cheng YH, Chi I, Boey KW, Ko LS, Chou KL. Self-rated economic condition and the health of elderly persons in Hong Kong. Soc Sci Med. 2002;55:1415–1424. doi: 10.1016/S0277-9536(01)00271-4. [DOI] [PubMed] [Google Scholar]
- Macleod U, Mitchell E, Black M, Spence G. Comorbidity and socioeconomic deprivation: an observational study of the prevalence of comorbidity in general practice. Eur J Gen Pract. 2004;10:24–26. doi: 10.3109/13814780409094223. [DOI] [PubMed] [Google Scholar]
- Rootman I, Gordon-El-Bihbety D. A Vision for a Health Literate Canada: Report of the Expert Panel on Health Literacy. , ; 2008. available from www.cpha.ca. [Google Scholar]
- Weiss BD, Hart G, McGee DL, D’Estelle S. Health status of illiterate adults: relation between literacy and health status among persons with low literacy skills. J Am Board Fam Pract. 1992;5:257–264. [PubMed] [Google Scholar]
- Gazmararian JA, Baker DW, Williams MV, Parker RM, Scott TL, Green DC, Fehrenbach SN, Ren J, Koplan JP. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281:545–551. doi: 10.1001/jama.281.6.545. [DOI] [PubMed] [Google Scholar]
- Baker DW, Parker RM, Williams MV, Clark WS, Nurss J. The relationship of patient reading ability to self-reported health and use of health services. Am J Public Health. 1997;87:1027–1030. doi: 10.2105/AJPH.87.6.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho YI, Lee SY, Arozullah AM, Crittenden KS. Effects of health literacy on health status and health service utilization amongst the elderly. Soc Sci Med. 2008;66:1809–1816. doi: 10.1016/j.socscimed.2008.01.003. [DOI] [PubMed] [Google Scholar]
- Bennett IM, Chen J, Soroui JS, White S. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann Fam Med. 2009;7:204–211. doi: 10.1370/afm.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SH. Health literacy and functional health status in Korean older adults. J Clin Nurs. 2009;18:2337–2343. doi: 10.1111/j.1365-2702.2008.02739.x. [DOI] [PubMed] [Google Scholar]
- Lee SY, Arozullah AM, Cho YI, Crittenden K, Vicencio D. Health literacy, social support, and health status among older adults. Educ Gerontol. 2009;35:191–201. doi: 10.1080/03601270802466629. [DOI] [Google Scholar]
- Institute of Medicine. Health literacy: a prescription to end confusion. National Academies Press, Washington DC; 2004. [PubMed] [Google Scholar]
- Baker DW. The meaning and the measure of health literacy. J Gen Intern Med. 2006;21:878–883. doi: 10.1111/j.1525-1497.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutner M, Greenberg E, Jin Y, Boyle B, Hsu Y, Dunleavy E. Literacy in Everyday Life: Results From the 2003 National Assessment of Adult Literacy (NCES 2007–480). U.S.Department of Education. National Center for Education Statistics, Washington,DC; 2007. [Google Scholar]
- Kirsch I, Jungeblut A, Jenkins L, Kolstad A. Adult Literacy in America : A First Look at the Results of the National Adult Literacy Survey. U.S. Department of Education. National Center for Education Statistics, Washington, DC; 1993. [Google Scholar]
- Nutbeam D. The evolving concept of health literacy. Soc Sci Med. 2008;67:2072–2078. doi: 10.1016/j.socscimed.2008.09.050. [DOI] [PubMed] [Google Scholar]
- Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients' knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158:166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114:1008–1015. doi: 10.1378/chest.114.4.1008. [DOI] [PubMed] [Google Scholar]
- Arnold CL, Davis TC, Berkel HJ, Jackson RH, Nandy I, London S. Smoking status, reading level, and knowledge of tobacco effects among low-income pregnant women. Prev Med. 2001;32:313–320. doi: 10.1006/pmed.2000.0815. [DOI] [PubMed] [Google Scholar]
- Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51:267–275. doi: 10.1016/S0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. J Gen Intern Med. 1998;13:791–798. doi: 10.1046/j.1525-1497.1998.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, Ren J, Peel J. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health. 2002;92:1278–1283. doi: 10.2105/AJPH.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care. 2002;40:395–404. doi: 10.1097/00005650-200205000-00005. [DOI] [PubMed] [Google Scholar]
- Bennett CL, Ferreira MR, Davis TC, Kaplan J, Weinberger M, Kuzel T, Seday MA, Sartor O. Relation between literacy, race, and stage of presentation among low-income patients with prostate cancer. J Clin Oncol. 1998;16:3101–3104. doi: 10.1200/JCO.1998.16.9.3101. [DOI] [PubMed] [Google Scholar]
- Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly person. Arch Intern Med. 2007;167:1503–1509. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- Bostock S, Steptoe A. Association between low functional health literacy and mortality in older adults: longitudinal cohort study. BMJ. 2012;344:e1602. doi: 10.1136/bmj.e1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss BD, Maysm MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, Mockbee J, Hale FA. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3:514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayliss EA, Ellis JL, Steiner JF. Subjective assessments of comorbidity correlate with quality of life health outcomes: Initial validation of a comorbidity assessment instrument. Health Qual Life Outcomes. 2005;3:51. doi: 10.1186/1477-7525-3-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan GD, Bindman AB. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165:1946–1952. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- Sudore RL, Mehta KM, Simonsick EM, Harris TB, Newman AB, Satterfield S, Rosano C, Rooks RN, Rubin SM, Ayonayon HN, Yaffe K. Limited literacy in older people and disparities in health and healthcare access. J Am Geriatr Soc. 2006;54:770–776. doi: 10.1111/j.1532-5415.2006.00691.x. [DOI] [PubMed] [Google Scholar]
- Lee SY, Tsai TI, Tsai YW, Kuo KN. Health literacy, health status, and healthcare utilization of Taiwanese adults: results from a national survey. BMC Publ Health. 2010;10:614. doi: 10.1186/1471-2458-10-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard DH, Gazmararian J, Parker RM. The impact of low health literacy on the medical costs of Medicare managed care enrollees. Am J Med. 2005;118:371–377. doi: 10.1016/j.amjmed.2005.01.010. [DOI] [PubMed] [Google Scholar]
- Britt HC, Harrison CM, Miller GC, Knox SA. Prevalence and patterns of multimorbidity in Australia. Med J Aust. 2008;189:72–77. doi: 10.5694/j.1326-5377.2008.tb01919.x. [DOI] [PubMed] [Google Scholar]