Abstract
Malignant lymphoma encompasses a wide variety of distinct disease entities. It is generally more common in developed countries and less common in developing countries. The East Asia region has one of the lowest incidence rates of malignant lymphoma. The incidence of malignant lymphoma around the world has been increasing at a rate of 3-4% over the last 4 decades, while some stabilization has been observed in developed countries in recent years. The reasons behind this lymphoma epidemic are poorly understood, although improving diagnostic accuracy, the recent AIDS epidemic, an aging world population and the increasing adoption of cancer-causing behaviors are suggested as contributing factors. Etiologies of malignant lymphoma include infectious agents, immunodeficiency, autoimmune disease, exposure to certain organic chemicals, and pharmaceuticals. The distribution of many subtypes exhibit marked geographic variations. Compared to the West, T/natural killer (NK) cell lymphomas (T/NK-cell lymphoma) and extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) are relatively more common, whereas other B-cell lymphomas, particularly follicular lymphoma and chronic lymphocytic leukemia/small lymphocytic lymphoma, are less common in Asia. Some subtypes of T/NK-cell lymphomas defined by Epstein-Barr virus association are predominantly Asian diseases, if not exclusively so. Both ethnic and environmental factors play roles in such diversity. In this review, we discuss the geographic distribution and etiology of malignant lymphoma, as well as the trend.
Keywords: Malignant lymphoma, Epidemiology, Asia
INTRODUCTION
Lymphoid neoplasms are a group of distinct entities with widely varying clinical features, histology, immunophenotypes, and genetic abnormalities. The WHO classification of lymphoid neoplasm encompasses not only Hodgkin lymphoma and non-Hodgkin lymphoma (NHL), but also plasma cell neoplasm and lymphoid leukemia, with the underlying tenet that lymphoma and lymphoid leukemia represent solid and circulating phases, respectively, of the same disease [1-3]. In this review, however, the discussion will focus on the epidemiologic characteristics of malignant lymphoma, that is, Hodgkin lymphoma and NHL.
Epidemiologic study of malignant lymphoma has been hampered by the lack of uniform classification and coding, which has precluded meaningful comparative analysis [4, 5]. As the understanding of the biology of lymphoid cells and their malignant counterparts has evolved rapidly during the past decades, lymphoma classification has changed extensively. Many competing classifications had been used until a consensus classification, the Revised European-American classification (1994), and subsequently, the WHO classification (2001, with a revision in 2008) were proposed and accepted as the global standard [1-3]. To aid epidemiologic research, the Pathology Working Group of the International Lymphoma Epidemiology Consortium (InterLymph) published the hierarchical classification that enables systematic categorization of the entities into epidemiologically meaningful groups and reclassification of cases that had been coded using previous classifications [5, 6]. However, even in the era of the WHO classification, the quality and accuracy of the diagnosis and coding of lymphoma continue to challenge both pathologists and epidemiologists due to the need for elaborate immunophenotyping, cytogenetic and molecular studies, clinical information, and histopathologic expertise in the interpretation [4, 7].
In Korea, the first analysis of the population-based disease-specific statistics on hematologic malignancies was published in 2012 through the joint effort of the Korea Central Cancer Registry and the Korean Society of Hematology [8]; the incidence rates, prevalence rates, and annual percentage change of NHL, Hodgkin lymphoma, multiple myeloma, and lymphoid leukemia from 1993 to 2008 are now available.
INCIDENCE OF MALIGNANT LYMPHOMA
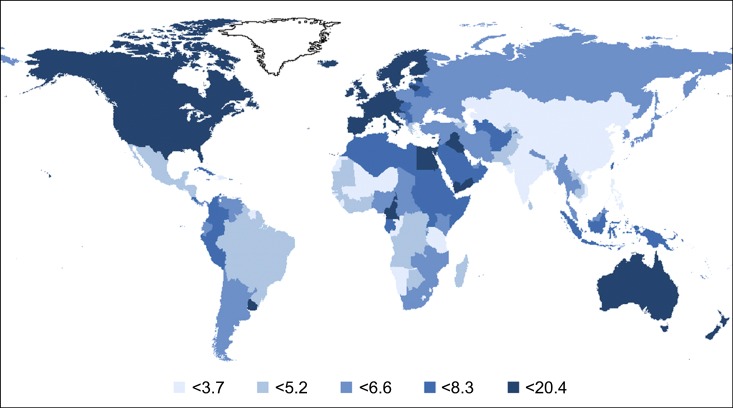
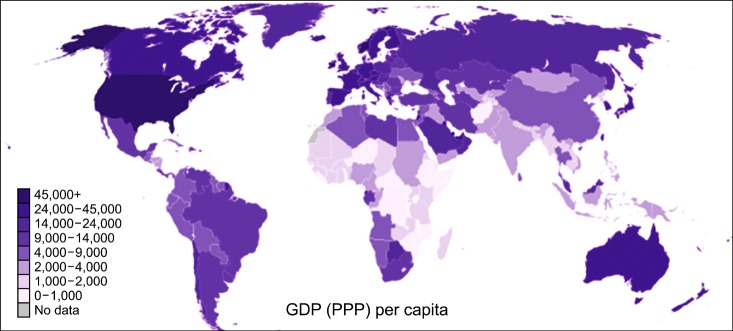
Malignant lymphoma comprises 3.37% of all malignancy worldwide [9]. In Korea, malignant lymphoma accounted for 3.69% of all malignancies in 2008 [8]. The incidence of malignant lymphoma exhibits a marked geographic variation; higher in North America, Australia/New Zealand, and Europe, and lower throughout Asia and Africa, except where Burkitt lymphoma (BL) is endemic (Fig. 1) [9-11]. The age-standardized incidence rates for East Asia are summarized in Table 1, which reveals lower incidences of NHL and Hodgkin lymphoma in East Asia compared with Western countries. It also shows that the incidences in ethnic Koreans and Chinese vary markedly depending on the country of residence. While the disparity between East and West suggests the influence of ethnicity, the disparity between identical or similar ethnic populations residing in different regions indicates an environmental influence [12]. In Fig. 2, the striking similarity of the world lymphoma map to the world GDP per capita map, with a few exceptions, demonstrates the association of malignant lymphoma with economic development. Factors associated with economic improvement include change in the diet/over-nutrition, increase in anthropometric measurement/metabolic syndrome, better hygiene and smaller family size, adoption of a sedentary lifestyle, better medical access and care, increase in lifespan, exposure to environmental carcinogens associated with industrialization, etc.
Fig. 1.
World map of the estimated age-standardized incidence rates (per 100,000 WHO world standard population) of non-Hodgkin lymphoma and Hodgkin lymphoma combined. Source: GLOBOCAN (http://globocan.iarc.fr/) from CANCERMondial (http://www-dep.iarc.fr/).
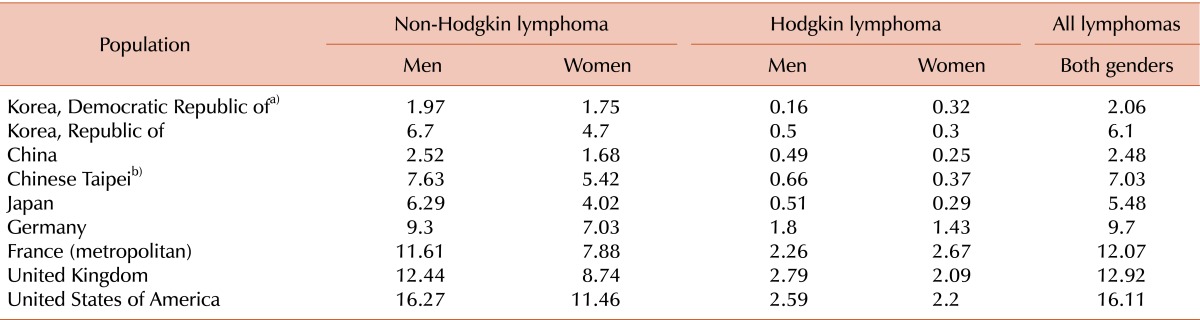
Table 1.
Incidence rates of malignant lymphoma in East Asia in 2008.
a)North Korea, b)Taiwan.
Age-standardized incidence rates/100,000 (WHO world standard population). GLOBOCAN 2008.
For Korea, data are from the Korea National Cancer Incidence Database.
Fig. 2.
Nominal gross domestic product (GDP) per capita world map 2008. Source: CIA World Factbook 2008. Abbreviation: PPP, purchasing power parity.
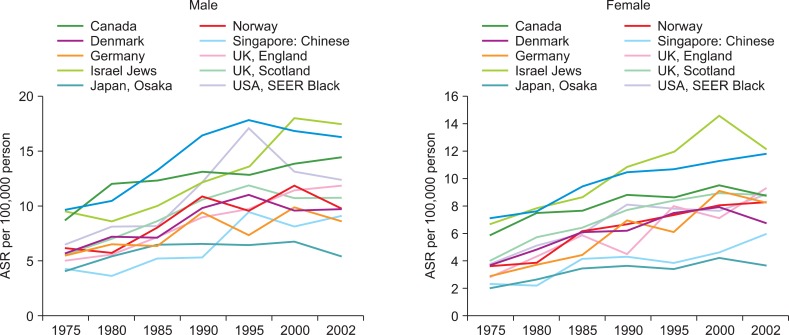
As depicted in Fig. 3, the incidence of NHL has been increasing since the 1970s across all regions and races [9-16]. In the USA, for instance, NHL has steadily increased by 3-4% each year in both whites and blacks, both sexes, and all ages except the very young from 1973 until the mid-1990s, when the increasing trend slowed down somewhat to 1-2% per year [12-14]. A similarly high rate of increase was consistently observed in Korea in 1999-2008 for NHL in both men and women, with no sign of stabilization [8]. While the improvement in diagnosis and reporting, the AIDS epidemic, and the change in lymphoma classification were found to be responsible for approximately 50% of the increase, an increase of such epidemic proportions is unprecedented and remains largely unexplained [13-15].
Fig. 3.
Trends in estimated age-standardized (world) incidence rates of non-Hodgkin lymphoma. Source: CI5plus in CANCERMondial.
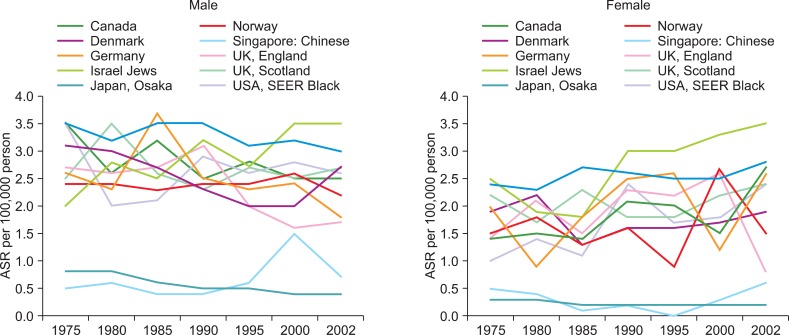
The incidence of Hodgkin lymphoma is consistently lower than that of NHL throughout the world. In contrast to NHL, the incidence of Hodgkin lymphoma worldwide is either decreasing or stationary (Fig. 4) [16]. In the USA, the incidence of Hodgkin lymphoma decreased by approximately 16% in the 1970s through to 1997. The reasons for the decrease are unclear, with only a small proportion of the decrease attributed to the shift in classification and the problem of misdiagnosis [13, 17]. On the other hand, an increase in Hodgkin lymphoma incidence was observed in many female populations, including white and black women in the USA [16, 17]. In Korea, Hodgkin lymphoma increased by 4.5% per year in 1999-2008, with a 2.8% increase in men and 7.2% increase in women [8]. The upward trend in women has been associated with decreasing parity in developed countries, implicating childbearing as a protective factor against Hodgkin lymphoma [17, 18]. With the increasingly higher age of motherhood and decreasing parity in Korea, we may expect a further rise of Hodgkin lymphoma incidence in women.
Fig. 4.
Trends in estimated age-standardized (world) incidence rates of Hodgkin lymphoma. Source: CI5plus in CANCERMondial (http://www-dep.iarc.fr/).
Age and sex are important factors in the epidemiology of lymphoma. In NHL, incidence increases with advancing age, with a median age of diagnosis in the seventh decade [4, 8, 15]. NHL incidence continues to increase with age in men. In women, NHL also increases with age, but at a lower rate, and then decreases at ages 80 years or older. Fig. 5 shows the age-specific incidence arates of NHL and Hodkgin lymphoma in Korea (2008 data) [8]. As depicted in Fig. 5A, the age-specific incidence rate of NHL in Korea in 2008 exhibits a typical pattern. NHL is basically a disease of older adults, with a median age of most NHL subtypes in the sixth to seventh decade, except BL, precursor NHL (acute lymphoblastic lymphoma/leukemia, ALL/LBL), and mediastinal large B-cell lymphoma. Fig. 6 depicts the age distribution of the major lymphoma subtypes in Korea using previously reported data from Asan Medical Center, Seoul (1989-2008) [7]. It shows that follicular lymphoma, MALT lymphoma, and extranodal nasal-type natural killer (NK)/T cell lymphoma affect younger individuals compared with other mature NHL.
Fig. 5.
Age-specific incidence rates (ASR) of non-Hodgkin lymphoma and Hodgkin lymphoma in Korea in 2008. Source: Park et al. [8].
Fig. 6.
Age distribution of malignant lymphoma at diagnosis for 1989-2008 at Asan Medical Center. Source: Yoon et al. [7]. Abbreviations: CLL/SLL, chronic lymphocytic leukemia/small lymphocytic lymphoma; MCL, mantle cell lymphoma; FL, follicular lymphoma; MALT, mucosa-associated lymphoid tissue; DLBCL, diffuse large B-cell lymphoma; NK, natural killer; PTCL, peripheral T-cell lymphoma, not otherwise specified; NHL, non-Hodgkin lymphoma.
In contrast to NHL, Hodgkin lymphoma exhibits several specific patterns of age-incidence curves, depending on the socioeconomic status of the population [19-23]. In underdeveloped countries, a peak in early childhood with a predominance of mixed cellularity subtype is followed by an older adult peak (>50 years of age). In developed countries, a peak in young adulthood with a predominance of nodular sclerosis subtype is followed by an older adult peak. These subtypes are currently viewed as distinct diseases with different epidemiologies [22, 23]. The mixed cellularity subtype is primarily a disease of economically disadvantaged children who are exposed to early childhood infection, and of older individuals who are immunosuppressed due to old age or human immunodeficiency virus (HIV) infection. In contrast, nodular sclerosis is a disease of young adults whose higher social class has delayed their exposure to common childhood infections [19-23]. The age-specific incidence pattern of Hodgkin lymphoma in Korea in 2008 reveals a peak in young adulthood, with equal contribution from male and female cases, and a second old-age peak with greater male predominance (Fig. 5B).
NHL is more common in men than in women. In 2008, the sex ratio of NHL incidence in Korea was 1.42 [8]. Notable exceptions to male predominance are MALT lymphoma, mediastinal large B-cell lymphoma, and nodular sclerosis-type Hodgkin lymphoma, which are more common in women [1, 3]. Although the overall incidence of Hodgkin lymphoma is higher in men, the sex ratio differs among different age group. In developed countries, the sex ratio in the young adult peak of Hodgkin lymphoma is often reversed, being associated with female predominance of nodular sclerosis that comprises the bulk of cases in that age group. In developing countries, the childhood peak reveals a high sex ratio due to marked male predominance of the mixed cellularity subtype that comprises the bulk of childhood cases [20, 21].
SUBTYPE DISTRIBUTION
The subtype distribution of malignant lymphoma reveals striking geographic variations. Asians typically have relatively higher proportions of mature T/NK cell lymphomas and MALT lymphoma and lower proportions of follicular lymphoma and chronic lymphocytic lymphoma/small lymphocytic lymphoma (CLL/SLL) than Western populations [1, 3, 7, 24-26]. The higher proportions of MALT lymphoma in Asia and mature T/NK-cell neoplasms in the southeastern parts of Japan are attributed to the high prevalence of Helicobacter pylori (H. pylori) and human T-lymphotropic virus 1 (HTLV-1), respectively [1, 2, 25]. However, the lower proportions of the other subtypes are largely unexplained. Before examining the ethnic and environmental risk factors, one should first rule out bias in the statistical data [27]. Bias may result from incomplete diagnostic work-up, miscoding or incomplete coding, inequity in the access to medical care, etc. Non-technical bias may include a population's significantly shorter life expectancy, as seen in extremely resource-poor populations in which age-associated diseases would be rare. Therefore, direct comparison of South and North Korean statistics will be limited.
A comparative analysis of the genetically homogenous populations living in different environments (e.g., resident Koreans and migrant Koreans in the USA) is an excellent tool to identify the risks associated with particular geographic locations [27]. In such analysis, the influence of the cancer-causing behavior of a particular ethnic group (culturally determined exposure) should be considered by incorporating age at migration, duration of residence, and residential neighborhood measures of acculturation [27-29]. In a study of NHL in US Asians using SEER data between 1988-2004, Clarke et al. reported that the incidence rates of follicular lymphoma, CLL/SLL, and nodular sclerosis Hodgkin lymphoma were significantly higher in US-born Asians (second-generation immigrants or beyond) compared with foreign-born Asians (first-generation immigrants), which supports the role of environmental factors in lymphomagenesis [28]. A similar trend was observed in studies of resident Koreans [7, 26].
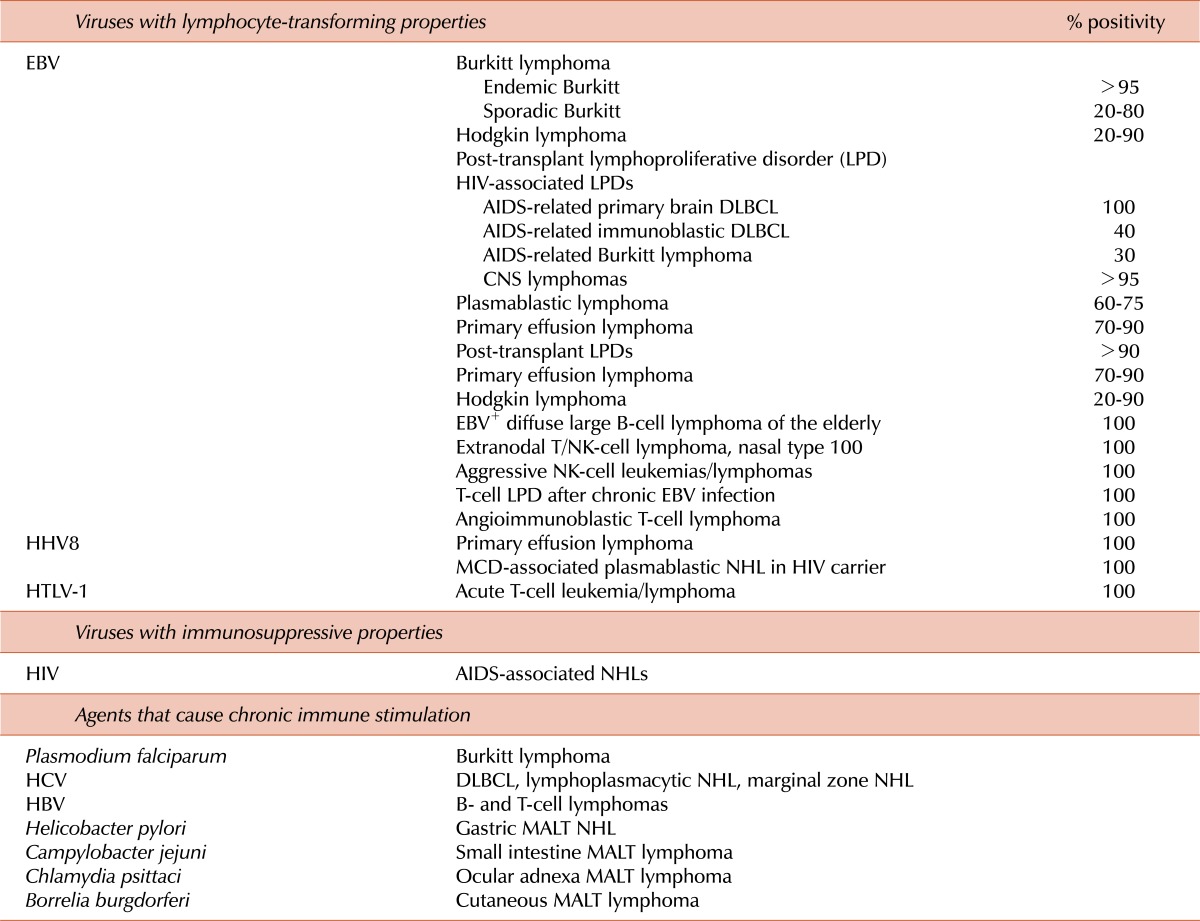
INFECTIOUS CAUSE
The infectious agents implicated in lymphomagenesis are listed in Table 2. Depending on the mode of action, the agents can be categorized into 3 groups [30]. Lymphocyte-transforming viruses directly infect lymphocytes, induce proliferation, and promote transformation. The genomes of the causative virus are detected in lymphoma cells [30, 31]. On the other hand, HIV induces immunosuppression by depleting CD4+ T cells, increasing the risk of "opportunistic" high-grade B-cell NHLs, many of which are in association with Epstein-Barr virus (EBV) or human herpesvirus 8 (HHV8). Other infectious agents promote lymphomagenesis by chronic antigenic stimulation, driving chronic persistent lymphocytic activation and proliferation, thus providing rich ground for malignant clones to arise.
Table 2.
Biologic agents implicated in malignant lymphomas [31].
Abbreviations: AIDS, acquired immunodeficiency syndrome; CNS, central nervous system; DLBCL, diffuse large B-cell lymphoma; EBV, Epstein-Barr virus; HBV, hepatitis B virus; HCV, hepatitis C virus; HHV8, human herpesvirus 8; HIV, human immunodeficiency virus; LPD, lymphoproliferative disorder; MALT, mucosa-associated lymphoid tissue; MCD, multicentric Castleman disease; NHL, non-Hodgkin lymphoma.
EPSTEIN-BARR VIRUS
There are 3 forms of BL, with distinct geographic and EBV associations. In endemic BL in sub-Saharan Africa and rainforest regions in Papua New Guinea [30-32], EBV is consistently detected in tumor cells in monoclonal form, which suggests that EBV infection is an early event. Tumor most commonly affects the jaws of these children, who frequently show evidence of active EBV replication prior to overt lymphoma, a sign of immunodysregulation induced by chronic infection of Plasmodium falciparum malaria. Both EBV and malaria induce B-cell hyperplasia. Malaria also reduces T-cell-mediated immunosurveillance of EBV-infected cells, and leads to an increased EBV viral load. Stimulation of Toll-like receptor 9 by malaria-associated agonists also induces activation-induced cytidine deaminase (AID), which mediates t(8;14) translocation [30-32]. The t(8;14) translocation results in constitutive overexpression of c-myc, the crucial event in Burkitt lymphomagenesis. EBV also prevents the apoptosis of translocation-containing cells on their journey through the germinal center to become memory cells. Sporadic BL occurs worldwide, affecting children and young adults primarily in the abdomen. EBV association is uncommonly observed.
EBV causes a significant proportion of Hodgkin lymphoma. The risk of Hodgkin lymphoma increases in patients with infectious mononucleosis (odds ratio, OR 1.0-8.2), especially of EBV-positive tumors in young patients [33]. EBV genomes are detected in the majority of tumor cells of Hodgkin lymphoma, and the virus is clonal. EBV demonstrates type 2 latency in Hodgkin lymphoma, with expression of EBNA-1, LMP-1, LMP-2, EBER, and BARTS. EBV positivity is seen in 26-50% of Hodgkin lymphoma in Western populations, but in a much higher percentage in Asia and Latin America (80% in India, Egypt, and Northeastern Brazil) [31]. EBV is associated with children and older adults, males, and mixed cellularity [30, 31, 34].
While the etiologic role of EBV in Hodgkin lymphoma is no longer disputed, the apparent contradiction of the higher incidence of EBV-negative Hodgkin lymphoma in populations with a higher incidence of Hodgkin lymphoma still puzzles many. The best explanation at present hypothesizes that there are 4 separate diseases in Hodgkin lymphoma, differing in the age at diagnosis, EBV association, and history of infectious mononucleosis. EBV-positive cases include a childhood group (cases occurring under the age of 10 years), a young adult group with previous infectious mononucleosis, and an older adult group with relative immunosuppression due to aging of the immune system. A single group of EBV-negative cases account for the young adult age-specific incidence peak [23]. The relative contribution of these 4 subtypes in a population will determine the age-specific incidence peak. While a study from Korea in 1996 reported EBV positivity of 68% and a predominance of the mixed cellularity subtype [34], a recent study reported EBV positivity of 34.5% and a predominance of the nodular sclerosis subtype using cases collected in 1990-2009 [35]. The same study also showed that EBV positivity was correlated with worsened survival in adults aged 25 years or older with advanced stage.
The Epstein-Barr virus is regularly involved in B cell lymphoproliferative disorder (LPD) in congenital or acquired immunodeficiency [3, 30, 31]. Post-transplant LPD (PTLD) is an EBV-driven, uncontrolled proliferation of latently infected B cells ranging from hyperplasia to overt lymphomas that occur as a result of the loss of cytotoxic T lymphocyte immunosurveillance induced by immunosuppressive medication [3, 31]. The overall incidence of PTLDs is between 1-4.6%; heart (1-2%), heart/lung (>5%), liver (1-2%), kidney (<1%), and is much lower in bone marrow recipients (<1%). In a single-center report of Korean patients, the frequency of PTLD was 0.81% of 4,545 solid organ transplants and 0.81% of 747 bone marrow transplants [36].
Age-related EBV-associated diffuse large B-cell lymphoma (DLBCL) affects individuals aged over 50 years without prior lymphoma or other known immunodeficiency [3, 37]. They account for 8-10% of DLBCL in Japan, but are rarer in other parts of the world [1, 38]. They may be monomorphic (two-thirds) or polymorphic (one-third), and are associated with poor performance status, elevated LDH, more frequent B symptoms, and higher involvement of the skin or lung than EBV-negative DLBCL. The polymorphic type presents difficulty in differential diagnosis from classical Hodgkin lymphoma. EBV exhibits a type 3 latency pattern, which demonstrates the relative immunodeficiency of these patients. Naturally, questions arise as to whether the diagnosis can be used in EBV-associated DLBCL in patients younger than 50 years without immunodeficiency. A study from Korea reported aggressive behavior of EBV+ DLBCL for the non-germinal center subtype irrespective of age [39].
Extranodal NK/T cell lymphoma, nasal type, is more common in East Asia and Central and South America, accounting for 7-10% of NHLs compared to Western countries, where it comprises less than 1% of all NHL [7, 40]. It presents primarily in the nose and upper aerodigestive tract, but shows distant metastasis in 20%. Up to 25% of cases present as extranasal diseases, and reveal markedly poorer outcomes than their nasal counterparts [40-42]. Recently, a decreasing tendency in extranodal NK/T-cell lymphoma incidence was suggested, but confirmation from population-based analysis awaits [43]. Asian cases are uniformly EBV type A, whereas cases reported in Europe are frequently type B, which suggests a geographic difference. A familial case was reported in which frequent high-volume use of pesticide was noted [44]. An increased OR for nasal NK/T cell lymphoma was reported in farmers, crop producers, and pesticide users [45]. The tumor cells exhibit the type 2 latency pattern of EBV.
T cell LPD after chronic EBV infection has been renamed as systemic EBV-positive LPD, and is characterized by fever, lymphadenopathy, and splenomegaly after primary infection in non-immunocompromised individuals [46-51]. It is most commonly reported in, but not limited to, East Asia. Patients have high levels of EBV viremia, and the viral genome is detected in the affected organs. Affected cell lineages are usually T or NK cell, but may also involve B cells. Patients frequently have hemophagocytic syndrome (HPS). Systemic EBV+ LPD includes overt lymphoma, hydroa vacciniformis, and severe mosquito bite allergy [3, 46-51]. Clinically overt systemic EBV-positive T-LPD may or may not reveal rearranged T cell receptor genes. Some cases may be accompanied with or followed by aggressive NK cell leukemia. Even among East Asians, this is an extremely rare condition. While most reported cases involved children and young adults, similar cases have been observed in middle-aged or older adults in Korea, with an extremely aggressive clinical course (personal observation). Many adult patients initially present with smoldering gastrointestinal manifestation, often mimicking inflammatory bowel disease or enteric tuberculosis, only to progress to fulminant HPS-associated disseminated intravascular coagulation or sepsis in a matter of a few weeks to months. Biopsy of the affected tissue is often misdiagnosed because EBV+ cells are bland-looking and variable in number. As the disease progresses, the infiltrate tends to become heavy, and becomes noticeable to the unsuspecting eye (personal observation).
Other T cell LPDs may be associated with EBV, including peripheral T-cell lymphomas not otherwise specified, enteropathy-type T-cell lymphomas, γδ T-cell lymphomas, angioimmunoblastic T-cell lymphoma, and aggressive NK cell leukemias/lymphomas [31].
HUMAN HERPESVIRUS 8
The seroprevalence of HHV8 is generally below 10% in USA, northern Europe, and Asia, including Korea (5%), but is much higher in the Mediterranean region (10-30%) and sub-Saharan Africa (>50%) [31]. HHV8 is detected in all cases of primary effusion lymphoma (PEL), and in a high proportion of multicentric Castleman disease (MCD) and MCD-derived DLBCL. HIV is a strong cofactor in both PEL and MCD [31]. Treatment of MCD with ganciclovir (an inhibitor of KSHV lytic replication) may ameliorate MCD, while treatment with cidofovir (an inhibitor of KSHV DNA polymerase) is not effective [31]. Some studies have reported the association of HHV8 with multiple myeloma, but this was not substantiated in recent reports [52].
HUMAN T CELL LEUKEMIA VIRUS TYPE 1
HTLV-1 is the causative agent of adult T-cell leukemia (ATL). HTLV-1 is endemic in the southwestern regions of Japan, the Caribbean islands, Papua New Guinea, and areas of Central and South America [31]. In non-endemic areas, it is seen in intravenous drug users and immigrants from endemic areas. For HTLV-1 carriers, the lifetime risk of developing ATL is 6.6% for men and 2.1% for women [53]. The distribution of ATL is similar to HTLV-1. In Korea, HTLV-1 seroprevalence is low, with a positivity of 0.007% among healthy blood donors [54], although higher positivity was observed in Cheju island, which is geographically close to the southwestern regions of Japan [55]. Reported cases of ATL are distinctly rare in Korea.
HUMAN IMMUNODEFICIENCY VIRUS
AIDS increases the risks of central nervous system NHL (CNS NHL, almost universally EBV-positive) by 5,000 times, DLBCL (50% EBV-positive) by 100-140 times, and BL (30% EBV-positive) by 100 times that of the general population [31]. The risk for CNS NHL and DLBCL increases linearly as the CD4 lymphocyte count declines [30, 31]. AIDS also increases the risk of HHV8-associated lymphomas and LPD, including PEL (HHV8- and EBV-positive), MCD, plasmablastic lymphoma of the oral cavity, and Hodgkin lymphoma (×10 increase) [31]. With the widespread use of highly active anti-retroviral therapy (HAART), AIDS-associated lymphomas, especially brain NHL, have declined markedly in recent years. Interestingly, the incidence of Hodgkin lymphoma increased after widespread use of HAART in HIV+ populations, which suggests that the development of Hodgkin lymphoma requires a relatively intact immune status [30, 31].
HEPATITIS C VIRUS
The hepatitis C virus (HCV) causes NHL through chronic immune stimulation [30, 31]. The virus increases the risk of essential mixed cryoglobulinemia, DLBCL, follicular lymphoma, lymphoplasmacytic lymphoma, marginal zone lymphoma, CLL/SLL, multiple myeloma, and T-cell NHL. HCV may induce LPD by binding to the CD81 receptor on B cells, which lowers the threshold for antigen response or induces DNA mutations [56]. Furthermore, HCV carriers have an elevated prevalence of circulating lymphocytes with abnormal chromosomal translocations such as t(14;18). An HCV infection precedes the development of NHL by at least 7 years [31]. In HCV+ splenic marginal zone lymphoma, interferon with or without ribavirin treatment for HCV was shown to regress the lymphoma [57], which suggests that HCV directly contributes to lymphoproliferation in at least a subset of NHL. In a large-scale case-control study from Korea, association of HCV infection was seen not only with B- and T-NHL, but also with B-cell acute lymphoid leukemia [58]. HCV-positive DLBCL cases in Korean patients were associated with older age, nodal disease, and superior outcome compared with HCV-negative DLBCL in another study [59].
HEPATITIS B VIRUS
A large body of literature demonstrates the association of the hepatitis B virus (HBV) with malignant lymphoma [31, 58, 60, 61]. A recent large-cohort study of the Korean population revealed a significant association of HBV with malignant lymphoma with a hazard ratio (HR) of 1.74, and a HR of 2.01 for DLBCL [60]. In the largest case-control study carried out in Korea, HBV was associated with increased risks for most subtypes of B- and T/NK-cell lymphomas, Hodgkin lymphoma, and acute myeloid leukemia [58] in Korea HBV is responsible for a much higher number of malignant lymphoma cases than HCV. Compared with HBsAg-negative patients, a report from China found that HBsAg-positive DLBCL patients were associated with earlier onset and more advanced stage [62]. Hepatic dysfunction during chemotherapy and withdrawal hepatitis in the-post-chemotherapy period remain a challenge, and warrant judicious use of anti-viral treatment and careful monitoring during and after chemotherapy [63].
HELICOBACTER PYLORI
Helicobacter pylori infection causes gastric MALT-type extranodal marginal zone lymphoma. MALT lymphoma has been demonstrated in mouse models infected with H. pylori and H. felis [31]. Infection by H. pylori or H. heilmannii induces MALT in the gastric mucosa, from which MALT lymphoma originates [31]. In the early stages of MALT lymphoma, B cell proliferation depends on both H. pylori antigens and tumor-infiltrating T cells, and responds to H. pylori eradication [64]. However, 20% of MALT lymphoma acquires additional mutations, in particular, the API2-MALT1 fusion gene that results from a [t(11;18)(q21;q21)] translocation, which leads to NF-κB activation, thereby inhibiting the apoptosis of these cells. Other mutations include P53, c-MYC, and gene promoter hypermethylation of p16 [64, 65].
The prevalence rates of H. pylori differ by age, race/ethnicity, and socioeconomic conditions, usually being higher in developing countries than in developed ones. In Korea, H. pylori prevalence exceeds 80% in individuals over 7 years of age [66], much higher than the global prevalence of around 50%. MALT lymphoma is the second most common subtype among the mature B-cell lymphomas in Korea [7, 24, 26]. Studies of the trend of lymphoma subtypes over time have shown that MALT lymphoma has increased in Korea over the last few decades [7, 26]. This increasing trend stands in sharp contrast to a study from Italy, which reported a marked decrease after the widespread practice of H. pylori eradication for gastritis [67].
Other MALT-type lymphomas with bacterial etiology include small intestinal MALT lymphoma with Campylobacter jejuni, ocular adnexa MALT lymphoma with Chlamydophila psittaci, and cutaneous MALT lymphoma with Borrelia burgdorferi [31]. Unlike the remarkable success of H. pylori eradication in gastric MALT lymphoma, MALT lymphomas in other sites exhibit inconsistent association with the purported pathogens and variable response to antibiotic treatment [68]. One unique feature of these chronic infection-related lymphomas is that they are not increased in immunosuppressed states [30]. Therefore, the current WHO classification explicitly excludes MALT lymphoma from the category of PTLD [3]. These findings suggest that a certain level of host immunocompetence is a prerequisite for these neoplasms [30].
AUTOIMMUNE DISEASE
Autoimmune rheumatic diseases such as systemic lupus erythematosus, rheumatoid arthritis, Sjögren's syndrome, psoriasis, and celiac disease are associated with moderately increased risk of NHL [69]. On the other hand, allergic and atopic conditions and their correlates such as early birth order are associated with a decreased risk of NHL. Patients with autoantibody-positive autoimmune diseases with systemic involvement face the highest risk of developing DLBCL and marginal zone lymphoma, especially in Sjögren's syndrome (×6.5 for NHL, ×1,000 for parotid gland MALT lymphoma, DLBCL, follicular lymphoma) [69]. The male gender, old age, prolonged disease course, and severe disease activity increase the risk of NHL. The mode of action includes chronic immune stimulation with increase in the B-cell compartment and the use of immunosuppressive drugs. In Korea, a study of primary thyroid MALT lymphoma reported a history of Hashimoto's thyroiditis in 72% of the cases [70].
EXPOSURE TO ENVIRONMENTAL CARCINOGENS
A variety of chemical and pharmaceutical agents is implicated in lymphomagenesis, and is summarized in Table 3. Among pharmaceutical carcinogens, azathioprine and cyclosporine are classified as group 1 agents for NHL [31]. Among the chemical carcinogens, benzene, 1,3-butadienes, ethylene oxide, and poorly defined chemicals in the rubber manufacturing industry can cause leukemia or NHL. Butadiene is used primarily in the production of synthetic rubbers and polymers. Exposure usually involves an occupational setting. However, butadiene has been widely detected in ambient air. Butadiene exposure is associated with all types of leukemia [30]. Benzene is used in the manufacture of organic chemicals. The International Agency for Research on Cancer (IARC) lists benzene as a group 2 agent for lymphoid tumors, including NHL, multiple myeloma, and CLL.
Table 3.
Environmental carcinogens implicated in malignant lymphoma.
Abbreviations: ANLL, acute non-lymphocytic leukemia; ALL, acute lymphoblastic leukemia; CLL, chronic lymphocytic leukemia; MM, multiple myeloma; NHL, non-Hodgkin lymphoma.
BODY MASS INDEX, OBESITY, AND NON-INSULIN DEPENDENT DIABETES
A body mass index (BMI, weight in kilograms/squared height in meters, kg/m2) of 25-29.9 is considered overweight, and a BMI of 30 or higher is considered obese. A high BMI is associated with risk of DLBCL and Hodgkin lymphoma [71-74]. Height is also associated with NHL risk [73, 75]. Other studies showed that weight and BMI in early adulthood had a higher association with NHL risk than recent weight or BMI, particularly for DLBCL [74-76]. It is believed that the white adipose tissue that accumulates in obesity secretes an excessive amount of adipokines, which leads to disordered secretion of insulin, insulin-like growth factor 1, and inflammatory cytokines, which promote cancer growth [77]. A meta-analysis showed that type 2 diabetes mellitus increased the risk of NHL, especially T-cell NHL, leukemia, and myeloma, but not of Hodgkin lymphoma [78]. In the European Prospective Investigation into Cancer and Nutrition (EPIC), Khan et al. however, did not find any association between diabetes with NHL, except for CLL in men [79].
SMOKING, ALCOHOL, SUN EXPOSURE
A meta-analysis revealed an association between smoking with a higher OR for follicular lymphoma [80]. Another meta-analysis showed that smoking increased the risk of developing Hodgkin lymphoma in current smokers; the risk of Hodgkin lymphoma was higher in men and older individuals, and increased with a higher intensity and longer duration of smoking [81]. In other studies, compared with never smokers, current smokers and recent quitters (≤4 years ago) had a higher risk of developing Hodgkin lymphoma, whereas current or former smokers had a lower risk of follicular lymphoma [75, 82]. In contrast with smoking, alcohol use was shown to lower the risk of NHL [75, 82, 83]. Similarities in the epidemiology of melanoma, other types of skin cancers, and NHL have led to the hypothesis that UV exposure could play a role in NHL risk; studies suggest a protective effect of sun exposure against NHL, whereas the effect of vitamin D is unclear [84, 85].
CONCLUSION
The epidemiology of malignant lymphoma is complicated due to the great number of subtypes and their unique biology, and their complex relationship with infection, immunological abnormality, and genetic predisposition. Much of the infection-related lymphoma burden is expected to decrease with the advances in preventive and therapeutic measures. On the other hand, an aging population and the widespread use of immunosuppressive measures for autoimmune and other diseases may open the gates for an increase in opportunistic-type lymphomas. While many subtypes of malignant lymphoma in Korea display ethnic idiosyncrasy, it is becoming clear that they have begun to resemble those of Western countries. In contrast to the Western countries, where the increasing incidence of malignant lymphoma has recently slowed down, other parts of the world have maintained an upward trend. In view of the ongoing economic development and increasing adoption of the Western lifestyle, we may see new epidemics of old diseases such as follicular lymphoma and CLL in Asia in the near future.
References
- 1.Jaffe ES, Harris NL, Stein H, et al., editors. Pathology and genetics of tumours of haematopoietic and lymphoid tissues. Lyon, France: IARC Press; 2001. [Google Scholar]
- 2.Harris NL, Jaffe ES, Diebold J, Flandrin G, Muller-Hermelink HK, Vardiman J. Lymphoma classification-From controversy to consensus: the R.E.A.L. and WHO classification of lymphoid neoplasms. Ann Oncol. 2000;11(Suppl 1):3–10. [PubMed] [Google Scholar]
- 3.Swerdlow SH. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon, France: IARC Press; 2007. [Google Scholar]
- 4.Roman E, Smith AG. Epidemiology of lymphomas. Histopathology. 2011;58:4–14. doi: 10.1111/j.1365-2559.2010.03696.x. [DOI] [PubMed] [Google Scholar]
- 5.Morton LM, Turner JJ, Cerhan JR, et al. Proposed classification of lymphoid neoplasms for epidemiologic research from the Pathology Working Group of the International Lymphoma Epidemiology Consortium (InterLymph) Blood. 2007;110:695–708. doi: 10.1182/blood-2006-11-051672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turner JJ, Morton LM, Linet MS, et al. InterLymph hierarchical classification of lymphoid neoplasms for epidemiologic research based on the WHO classification (2008): update and future directions. Blood. 2010;116:e90–e98. doi: 10.1182/blood-2010-06-289561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yoon SO, Suh C, Lee DH, et al. Distribution of lymphoid neoplasms in the Republic of Korea: analysis of 5318 cases according to the World Health Organization classification. Am J Hematol. 2010;85:760–764. doi: 10.1002/ajh.21824. [DOI] [PubMed] [Google Scholar]
- 8.Park HJ, Park EH, Jung KW, et al. Statistics of hematologic malignancies in Korea: incidence, prevalence and survival rates from 1999 to 2008. Korean J Hematol. 2012;47:28–38. doi: 10.5045/kjh.2012.47.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CANCERmondial. Lyon, France: International Agency for Research on Cancer; 2008. [Accessed April 5, 2012]. http://www.dep.iarc.fr/ [Google Scholar]
- 10.Parkin DM International Association of Cancer Registries. Cancer incidence in five continents. Vols. I-VIII. Lyon, France: IARC Press; 2005. [Google Scholar]
- 11.Curado MP International Association of Cancer Registries. Cancer incidence in five continents. Vol. IX. Lyon, France: IARC Press; 2007. [Google Scholar]
- 12.Clarke CA, Glaser SL. Changing incidence of non-Hodgkin lymphomas in the United States. Cancer. 2002;94:2015–2023. doi: 10.1002/cncr.10403. [DOI] [PubMed] [Google Scholar]
- 13.Hartge P, Devesa SS, Fraumeni JF., Jr Hodgkin's and non-Hodgkin's lymphomas. Cancer Surv. 1994;19-20:423–453. [PubMed] [Google Scholar]
- 14.Blinder V, Fisher SG. The role of environmental factors in the etiology of lymphoma. Cancer Invest. 2008;26:306–316. doi: 10.1080/07357900701805686. [DOI] [PubMed] [Google Scholar]
- 15.Müller AM, Ihorst G, Mertelsmann R, Engelhardt M. Epidemiology of non-Hodgkin's lymphoma (NHL): trends, geographic distribution, and etiology. Ann Hematol. 2005;84:1–12. doi: 10.1007/s00277-004-0939-7. [DOI] [PubMed] [Google Scholar]
- 16.Baris D, Zahm SH. Epidemiology of lymphomas. Curr Opin Oncol. 2000;12:383–394. doi: 10.1097/00001622-200009000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Glaser SL, Swartz WG. Time trends in Hodgkin's disease incidence. The role of diagnostic accuracy. Cancer. 1990;66:2196–2204. doi: 10.1002/1097-0142(19901115)66:10<2196::aid-cncr2820661026>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 18.Glaser SL. Reproductive factors in Hodgkin's disease in women: a review. Am J Epidemiol. 1994;139:237–246. doi: 10.1093/oxfordjournals.aje.a116990. [DOI] [PubMed] [Google Scholar]
- 19.Correa P, O'Conor GT. Epidemiologic patterns of Hodgkin's disease. Int J Cancer. 1971;8:192–201. doi: 10.1002/ijc.2910080203. [DOI] [PubMed] [Google Scholar]
- 20.MacMahon B. Epidemiology of Hodgkin's disease. Cancer Res. 1966;26:1189–1201. [PubMed] [Google Scholar]
- 21.Glaser SL, Jarrett RF. The epidemiology of Hodgkin's disease. Baillieres Clin Haematol. 1996;9:401–416. doi: 10.1016/s0950-3536(96)80018-7. [DOI] [PubMed] [Google Scholar]
- 22.Mani H, Jaffe ES. Hodgkin lymphoma: an update on its biology with new insights into classification. Clin Lymphoma Myeloma. 2009;9:206–216. doi: 10.3816/CLM.2009.n.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jarrett RF. Viruses and Hodgkin's lymphoma. Ann Oncol. 2002;13(Suppl 1):23–29. doi: 10.1093/annonc/13.s1.23. [DOI] [PubMed] [Google Scholar]
- 24.Ko YH, Kim CW, Park CS, et al. REAL classification of malignant lymphomas in the Republic of Korea: incidence of recently recognized entities and changes in clinicopathologic features. Hematolymphoreticular Study Group of the Korean Society of Pathologists. Revised European-American lymphoma. Cancer. 1998;83:806–812. [PubMed] [Google Scholar]
- 25.Vose J, Armitage J, Weisenburger D. International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J Clin Oncol. 2008;26:4124–4130. doi: 10.1200/JCO.2008.16.4558. [DOI] [PubMed] [Google Scholar]
- 26.Kim JM, Ko YH, Lee SS, et al. WHO Classification of malignant lymphomas in Korea: Report of the Third Nationwide Study. Korean J Pathol. 2011;45:254–260. [Google Scholar]
- 27.Parkin DM. International variation. Oncogene. 2004;23:6329–6340. doi: 10.1038/sj.onc.1207726. [DOI] [PubMed] [Google Scholar]
- 28.Clarke CA, Glaser SL, Gomez SL, et al. Lymphoid malignancies in U.S. Asians: incidence rate differences by birthplace and acculturation. Cancer Epidemiol Biomarkers Prev. 2011;20:1064–1077. doi: 10.1158/1055-9965.EPI-11-0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carreon JD, Morton LM, Devesa SS, et al. Incidence of lymphoid neoplasms by subtype among six Asian ethnic groups in the United States, 1996-2004. Cancer Causes Control. 2008;19:1171–1181. doi: 10.1007/s10552-008-9184-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hjalgrim H, Engels EA. Infectious aetiology of Hodgkin and non-Hodgkin lymphomas: a review of the epidemiological evidence. J Intern Med. 2008;264:537–548. doi: 10.1111/j.1365-2796.2008.02031.x. [DOI] [PubMed] [Google Scholar]
- 31.WHO International Agency for Research on Cancer. IARC Monographs on the evaluation of carcinogenic risks to humans. Vol. 100. Lyon, France: IARC Press; 2012. [Google Scholar]
- 32.Magrath I. Epidemiology: clues to the pathogenesis of Burkitt lymphoma. Br J Haematol. 2012;156:744–756. doi: 10.1111/j.1365-2141.2011.09013.x. [DOI] [PubMed] [Google Scholar]
- 33.Alexander FE, Lawrence DJ, Freeland J, et al. An epidemiologic study of index and family infectious mononucleosis and adult Hodgkin's disease (HD): evidence for a specific association with EBV+ve HD in young adults. Int J Cancer. 2003;107:298–302. doi: 10.1002/ijc.11156. [DOI] [PubMed] [Google Scholar]
- 34.Huh J, Park C, Juhng S, Kim CE, Poppema S, Kim C. A pathologic study of Hodgkin's disease in Korea and its association with Epstein-Barr virus infection. Cancer. 1996;77:949–955. doi: 10.1002/(sici)1097-0142(19960301)77:5<949::aid-cncr22>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 35.Koh YW, Yoon DH, Suh C, Huh J. Impact of the Epstein-Barr virus positivity on Hodgkin's lymphoma in a large cohort from a single institute in Korea. Ann Hematol. 2012 doi: 10.1007/s00277-012-1464-8. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 36.Yoon SO, Yu E, Cho YM, et al. Post-transplant lymphoproliferative disorders: clinicopathological analysis of 43 cases in a single center, 1990-2009. Clin Transplant. 2012;26:67–73. doi: 10.1111/j.1399-0012.2010.01392.x. [DOI] [PubMed] [Google Scholar]
- 37.Asano N, Yamamoto K, Tamaru J, et al. Age-related Epstein-Barr virus (EBV)-associated B-cell lymphoproliferative disorders: comparison with EBV-positive classic Hodgkin lymphoma in elderly patients. Blood. 2009;113:2629–2636. doi: 10.1182/blood-2008-06-164806. [DOI] [PubMed] [Google Scholar]
- 38.Hofscheier A, Ponciano A, Bonzheim I, et al. Geographic variation in the prevalence of Epstein-Barr virus-positive diffuse large B-cell lymphoma of the elderly: a comparative analysis of a Mexican and a German population. Mod Pathol. 2011;24:1046–1054. doi: 10.1038/modpathol.2011.62. [DOI] [PubMed] [Google Scholar]
- 39.Park S, Lee J, Ko YH, et al. The impact of Epstein-Barr virus status on clinical outcome in diffuse large B-cell lymphoma. Blood. 2007;110:972–978. doi: 10.1182/blood-2007-01-067769. [DOI] [PubMed] [Google Scholar]
- 40.Au WY, Weisenburger DD, Intragumtornchai T, et al. Clinical differences between nasal and extranasal natural killer/T-cell lymphoma: a study of 136 cases from the International Peripheral T-Cell Lymphoma Project. Blood. 2009;113:3931–3937. doi: 10.1182/blood-2008-10-185256. [DOI] [PubMed] [Google Scholar]
- 41.Ko YH, Cho EY, Kim JE, et al. NK and NK-like T-cell lymphoma in extranasal sites: a comparative clinicopathological study according to site and EBV status. Histopathology. 2004;44:480–489. doi: 10.1111/j.1365-2559.2004.01867.x. [DOI] [PubMed] [Google Scholar]
- 42.Jo JC, Yoon DH, Kim S, et al. Clinical features and prognostic model for extranasal NK/T-cell lymphoma. Eur J Haematol. 2012 doi: 10.1111/j.1600-0609.2012.01796.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 43.Aozasa K, Takakuwa T, Hongyo T, Yang WI. Nasal NK/T-cell lymphoma: epidemiology and pathogenesis. Int J Hematol. 2008;87:110–117. doi: 10.1007/s12185-008-0021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kojya S, Matsumura J, Ting L, et al. Familial nasal NK/T-cell lymphoma and pesticide use. Am J Hematol. 2001;66:145–147. doi: 10.1002/1096-8652(200102)66:2<145::AID-AJH1033>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 45.Xu JX, Hoshida Y, Yang WI, et al. Life-style and environmental factors in the development of nasal NK/T-cell lymphoma: a case-control study in East Asia. Int J Cancer. 2007;120:406–410. doi: 10.1002/ijc.22313. [DOI] [PubMed] [Google Scholar]
- 46.Kimura H, Ito Y, Kawabe S, et al. EBV-associated T/NK-cell lymphoproliferative diseases in nonimmunocompromised hosts: prospective analysis of 108 cases. Blood. 2012;119:673–686. doi: 10.1182/blood-2011-10-381921. [DOI] [PubMed] [Google Scholar]
- 47.Cohen JI, Kimura H, Nakamura S, Ko YH, Jaffe ES. Epstein-Barr virus-associated lymphoproliferative disease in non-immuno-compromised hosts: a status report and summary of an international meeting, 8-9 September 2008. Ann Oncol. 2009;20:1472–1482. doi: 10.1093/annonc/mdp064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Suzuki K, Ohshima K, Karube K, et al. Clinicopathological states of Epstein-Barr virus-associated T/NK-cell lymphoproliferative disorders (severe chronic active EBV infection) of children and young adults. Int J Oncol. 2004;24:1165–1174. [PubMed] [Google Scholar]
- 49.Cho KH, Kim CW, Heo DS, et al. Epstein-Barr virus-associated peripheral T-cell lymphoma in adults with hydroa vacciniforme-like lesions. Clin Exp Dermatol. 2001;26:242–247. doi: 10.1046/j.1365-2230.2001.00805.x. [DOI] [PubMed] [Google Scholar]
- 50.Ishihara S, Yabuta R, Tokura Y, Ohshima K, Tagawa S. Hypersensitivity to mosquito bites is not an allergic disease, but an Epstein-Barr virus-associated lymphoproliferative disease. Int J Hematol. 2000;72:223–228. [PubMed] [Google Scholar]
- 51.Kimura H, Hoshino Y, Kanegane H, et al. Clinical and virologic characteristics of chronic active Epstein-Barr virus infection. Blood. 2001;98:280–286. doi: 10.1182/blood.v98.2.280. [DOI] [PubMed] [Google Scholar]
- 52.Tedeschi R, Luostarinen T, De Paoli P, et al. Joint Nordic prospective study on human herpesvirus 8 and multiple myeloma risk. Br J Cancer. 2005;93:834–837. doi: 10.1038/sj.bjc.6602751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Arisawa K, Soda M, Endo S, et al. Evaluation of adult T-cell leukemia/lymphoma incidence and its impact on non-Hodgkin lymphoma incidence in southwestern Japan. Int J Cancer. 2000;85:319–324. doi: 10.1002/(sici)1097-0215(20000201)85:3<319::aid-ijc4>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 54.Kwon SY, Lim AH, Park JY, Han SH, Cho NS. Seroprevalence of human T-lymphotropic virus type 1 and 2 in Korean blood donors. J Med Virol. 2008;80:1864–1867. doi: 10.1002/jmv.21260. [DOI] [PubMed] [Google Scholar]
- 55.Kim JM, Chang KH, Choi YH, et al. Seroprevalence of HTLV-I in Cheju Island, a Korean island adjacent to the endemic area of Japan. J Acquir Immune Defic Syndr. 1999;22:409–412. doi: 10.1097/00126334-199912010-00016. [DOI] [PubMed] [Google Scholar]
- 56.Weng WK, Levy S. Hepatitis C virus (HCV) and lymphomagenesis. Leuk Lymphoma. 2003;44:1113–1120. doi: 10.1080/1042819031000076972. [DOI] [PubMed] [Google Scholar]
- 57.Hermine O, Lefrère F, Bronowicki JP, et al. Regression of splenic lymphoma with villous lymphocytes after treatment of hepatitis C virus infection. N Engl J Med. 2002;347:89–94. doi: 10.1056/NEJMoa013376. [DOI] [PubMed] [Google Scholar]
- 58.Kang J, Cho JH, Suh CW, et al. High prevalence of hepatitis B and hepatitis C virus infections in Korean patients with hematopoietic malignancies. Ann Hematol. 2011;90:159–164. doi: 10.1007/s00277-010-1055-5. [DOI] [PubMed] [Google Scholar]
- 59.Park BB, Kim JS, Lee YY, et al. Clinical characteristics and outcome for hepatitis C virus-positive diffuse large B-cell lymphoma. Leuk Lymphoma. 2008;49:88–94. doi: 10.1080/10428190701732861. [DOI] [PubMed] [Google Scholar]
- 60.Marcucci F, Spada E, Mele A, Caserta CA, Pulsoni A. The association of hepatitis B virus infection with B-cell non-Hodgkin lymphoma - a review. Am J Blood Res. 2012;2:18–28. [PMC free article] [PubMed] [Google Scholar]
- 61.Engels EA, Cho ER, Jee SH. Hepatitis B virus infection and risk of non-Hodgkin lymphoma in South Korea: a cohort study. Lancet Oncol. 2010;11:827–834. doi: 10.1016/S1470-2045(10)70167-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang F, Xu RH, Luo HY, et al. Clinical and prognostic analysis of hepatitis B virus infection in diffuse large B-cell lymphoma. BMC Cancer. 2008;8:115. doi: 10.1186/1471-2407-8-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kim YM, Jeong SH, Kim JW, et al. Chronic hepatitis B, non-Hodgkin's lymphoma, and effect of prophylactic antiviral therapy. J Clin Virol. 2011;51:241–245. doi: 10.1016/j.jcv.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 64.Isaacson PG. Update on MALT lymphomas. Best Pract Res Clin Haematol. 2005;18:57–68. doi: 10.1016/j.beha.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 65.Sagaert X, Van Cutsem E, De Hertogh G, Geboes K, Tousseyn T. Gastric MALT lymphoma: a model of chronic inflammation-induced tumor development. Nat Rev Gastroenterol Hepatol. 2010;7:336–346. doi: 10.1038/nrgastro.2010.58. [DOI] [PubMed] [Google Scholar]
- 66.Youn HS, Baik SC, Cho YK, et al. Comparison of Helicobacter pylori infection between Fukuoka, Japan and Chinju, Korea. Helicobacter. 1998;3:9–14. doi: 10.1046/j.1523-5378.1998.08011.x. [DOI] [PubMed] [Google Scholar]
- 67.Luminari S, Cesaretti M, Marcheselli L, et al. Decreasing incidence of gastric MALT lymphomas in the era of anti-Helicobacter pylori interventions: results from a population-based study on extranodal marginal zone lymphomas. Ann Oncol. 2010;21:855–859. doi: 10.1093/annonc/mdp402. [DOI] [PubMed] [Google Scholar]
- 68.Bertoni F, Coiffier B, Salles G, et al. MALT lymphomas: pathogenesis can drive treatment. Oncology (Williston Park) 2011;25:1134–1142. 1147. [PubMed] [Google Scholar]
- 69.Dias C, Isenberg DA. Susceptibility of patients with rheumatic diseases to B-cell non-Hodgkin lymphoma. Nat Rev Rheumatol. 2011;7:360–368. doi: 10.1038/nrrheum.2011.62. [DOI] [PubMed] [Google Scholar]
- 70.Oh SY, Kim WS, Kim JS, et al. Primary thyroid marginal zone B-cell lymphoma of the mucosa-associated lymphoid tissue type: clinical manifestation and outcome of a rare disease - consortium for improving survival of lymphoma study. Acta Haematol. 2012;127:100–104. doi: 10.1159/000333113. [DOI] [PubMed] [Google Scholar]
- 71.Willett EV, Morton LM, Hartge P, et al. Non-Hodgkin lymphoma and obesity: a pooled analysis from the InterLymph Consortium. Int J Cancer. 2008;122:2062–2070. doi: 10.1002/ijc.23344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Larsson SC, Wolk A. Body mass index and risk of non-Hodgkin's and Hodgkin's lymphoma: a meta-analysis of prospective studies. Eur J Cancer. 2011;47:2422–2430. doi: 10.1016/j.ejca.2011.06.029. [DOI] [PubMed] [Google Scholar]
- 73.Keegan TH, Glaser SL, Clarke CA, et al. Body size, physical activity, and risk of Hodgkin's lymphoma in women. Cancer Epidemiol Biomarkers Prev. 2006;15:1095–1101. doi: 10.1158/1055-9965.EPI-06-0020. [DOI] [PubMed] [Google Scholar]
- 74.Maskarinec G, Erber E, Gill J, Cozen W, Kolonel LN. Overweight and obesity at different times in life as risk factors for non-Hodgkin's lymphoma: the multiethnic cohort. Cancer Epidemiol Biomarkers Prev. 2008;17:196–203. doi: 10.1158/1055-9965.EPI-07-0716. [DOI] [PubMed] [Google Scholar]
- 75.Lim U, Morton LM, Subar AF, et al. Alcohol, smoking, and body size in relation to incident Hodgkin's and non-Hodgkin's lymphoma risk. Am J Epidemiol. 2007;166:697–708. doi: 10.1093/aje/kwm122. [DOI] [PubMed] [Google Scholar]
- 76.Pylypchuk RD, Schouten LJ, Goldbohm RA, Schouten HC, van den Brandt PA. Body mass index, height, and risk of lymphatic malignancies: a prospective cohort study. Am J Epidemiol. 2009;170:297–307. doi: 10.1093/aje/kwp123. [DOI] [PubMed] [Google Scholar]
- 77.Hursting SD, Nunez NP, Varticovski L, Vinson C. The obesity-cancer link: lessons learned from a fatless mouse. Cancer Res. 2007;67:2391–2393. doi: 10.1158/0008-5472.CAN-06-4237. [DOI] [PubMed] [Google Scholar]
- 78.Castillo JJ, Mull N, Reagan JL, Nemr S, Mitri J. Increased incidence of non-Hodgkin lymphoma, leukemia, and myeloma in patients with diabetes mellitus type 2: a meta-analysis of observational studies. Blood. 2012;119:4845–4850. doi: 10.1182/blood-2011-06-362830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Khan AE, Gallo V, Linseisen J, et al. Diabetes and the risk of non-Hodgkin's lymphoma and multiple myeloma in the European Prospective Investigation into Cancer and Nutrition. Haematologica. 2008;93:842–850. doi: 10.3324/haematol.12297. [DOI] [PubMed] [Google Scholar]
- 80.Morton LM, Hartge P, Holford TR, et al. Cigarette smoking and risk of non-Hodgkin lymphoma: a pooled analysis from the International Lymphoma Epidemiology Consortium (interlymph) Cancer Epidemiol Biomarkers Prev. 2005;14:925–933. doi: 10.1158/1055-9965.EPI-04-0693. [DOI] [PubMed] [Google Scholar]
- 81.Castillo JJ, Dalia S, Shum H. Meta-analysis of the association between cigarette smoking and incidence of Hodgkin's Lymphoma. J Clin Oncol. 2011;29:3900–3906. doi: 10.1200/JCO.2011.35.4449. [DOI] [PubMed] [Google Scholar]
- 82.Troy JD, Hartge P, Weissfeld JL, et al. Associations between anthropometry, cigarette smoking, alcohol consumption, and non-Hodgkin lymphoma in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial. Am J Epidemiol. 2010;171:1270–1281. doi: 10.1093/aje/kwq085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kanda J, Matsuo K, Kawase T, et al. Association of alcohol intake and smoking with malignant lymphoma risk in Japanese: a hospital-based case-control study at Aichi Cancer Center. Cancer Epidemiol Biomarkers Prev. 2009;18:2436–2441. doi: 10.1158/1055-9965.EPI-09-0050. [DOI] [PubMed] [Google Scholar]
- 84.Negri E. Sun exposure, vitamin D, and risk of Hodgkin and non-Hodgkin lymphoma. Nutr Cancer. 2010;62:878–882. doi: 10.1080/01635581.2010.509535. [DOI] [PubMed] [Google Scholar]
- 85.Kricker A, Armstrong BK, Hughes AM, et al. Personal sun exposure and risk of non Hodgkin lymphoma: a pooled analysis from the Interlymph Consortium. Int J Cancer. 2008;122:144–154. doi: 10.1002/ijc.23003. [DOI] [PubMed] [Google Scholar]