Abstract
Purpose
The objectives of this study were to develop consensus on (i) the content of a clinical assessment for adults presenting to primary care with low back and leg pain, and (ii) the most important items for diagnosing spinal nerve root involvement.
Methods
Existing literature and expert knowledge was used to compile a list of items pertaining to clinical history questions and examination tests employed in the assessment of patients with low back pain with suspected spinal nerve involvement. A Delphi consensus method was employed to rate the importance of items for clinical assessment and for diagnosis in two web-based rounds. A multidisciplinary group of 42, including GPs, physiotherapists, osteopaths, rheumatologists, spinal orthopaedic surgeons and chiropractors took part. Items were included in the final assessment when over 70% of participants rated them as important.
Results
Thirty-four items were included in the clinical assessment, and 15 items for diagnosis. History items included pain distribution in the leg, pain quality and behaviour, altered sensation, functional limitations and yellow flags, previous history of similar symptoms and outcome of previous treatment/management. Examination items included typical neurological tests including neural tension and ‘demonstration of movement that produces symptoms’.
Conclusions
We have developed a clinical assessment schedule for patients with low back pain and leg pain presenting in primary care. History and clinical items considered important for their contribution in the diagnosis of nerve root involvement were also established.
Electronic supplementary material
The online version of this article (doi:10.1007/s00586-011-2057-2) contains supplementary material, which is available to authorized users.
Keywords: Sciatica, Delphi, Assessment, Nerve root pain, Consensus, Experts
Introduction
Low back pain (LBP) is defined as pain occurring between the gluteal folds and inferior border of the ribs with or without radiation down the leg [6, 7, 21]. Sciatica, or spinal nerve root pain, represents one distinct presentation of LBP and associated leg pain, and is generally characterised by pain radiating to below the knee and into the foot and toes, with varying neurological findings. Although the prevalence of nerve root pain is less than that of LBP alone [17], the condition is considered by some authors to be responsible for most of the indirect costs and lost workdays associated with LBP [4, 20].
The ability of clinicians however, to distinguish between non-specific LBP that simply spreads to the leg (also called referred pain) and true spinal nerve root involvement (sciatica) is often debated [8] as is the definition of sciatica. This is perhaps reflected in the wide variation of sciatica prevalence estimates reported in the literature [17], which is partly attributed to different definitions of the presentation and different assessment methods.
Compared to non-specific LBP literature investigating prognostic indicators of outcome, there is limited evidence on prognostic factors for LBP-associated leg pain (either referred or due to nerve root involvement). It is unclear whether the prognostic indicators relevant to outcome in patients with nerve root pain (mainly due to disc herniation) are similar to those for LBP alone with published literature providing conflicting views at times as to whether psychosocial or physical factors predominate [3, 12].
Studies investigating the diagnostic value of history and physical examination factors for categorisation of patients with LBP and nerve root symptoms have been conducted within secondary care cohorts and therefore include patients with more severe symptoms [19, 24]. But even with well documented conditions such as nerve root involvement due to disc prolapse or stenosis, there is significant variation in the number and type of eligibility criteria from trials assessing treatment effectiveness [11]. However, current literature suggests that the clinical evaluation remains the most important aspect of diagnosing spinal nerve root involvement in LBP [5, 16, 22, 23].
The development of the clinical assessment for patients with LBP and leg pain by consensus [1, 9, 15] is important to improve management of patients with LBP-associated leg pain. First, such assessment criteria will enable more accurate and appropriate inclusion into research studies, ensuring that a full spectrum of symptoms is captured. Second, this will enable the development of classification criteria for the presence or absence of nerve root involvement in unselected primary care populations with back and leg pain. Ultimately, the goal is to provide a more valid assessment, feasible and appropriate for primary care that distinguishes between non-specific LBP and leg pain and LBP with nerve root pain. This should enable practitioners to offer more appropriate treatment for each group and to test whether management options should differ between the groups.
As part of an ongoing spinal research programme, we plan a clinical epidemiology cohort study investigating prognostic indicators of outcome in adults presenting in primary care with low back and leg pain. In this article, we describe the process of developing a standardised clinical assessment to be used in the cohort study and the derivation of the items of the clinical assessment which contribute most to a diagnosis of nerve root involvement.
The objectives of this study were to develop consensus on the content of the clinical assessment of adults presenting to primary care with low back and leg pain and to identify the items from history and clinical examination that contribute most to the diagnosis of low back and leg pain that is due to spinal nerve root involvement.
Methods
Study design
The study involved three phases; (i) selection of potential items for inclusion in the assessment by a multidisciplinary team, (ii) 2 rounds of web-based Delphi consensus study, and (iii) a final virtual meeting of the multidisciplinary team. Ethical approval was granted by the Staffordshire Research Ethics Committee (09/H1204/96).
Phase 1: Delphi items
In phase 1, a multidisciplinary team of 8 clinicians and researchers with expertise in LBP from the following disciplines; general practice, rheumatology, physiotherapy, orthopaedics, osteopathy, compiled a list of items representing clinical history and examination questions and tests used to assess patients with LBP in whom lumbar spinal nerve involvement is suspected. The items were compiled from textbooks from the clinical specialties and published literature (original research papers) on the topic of the assessment of low back-associated leg pain as well as input from the members of the multidisciplinary team. The items were grouped and presented according to the domain they represented, for example items assessing pain were grouped under ‘pain domain’, items assessing psychosocial issues were grouped under ‘psychosocial factors domain’. These items were to be considered by a panel of experts in the Delphi consensus study first for inclusion in the standardised clinical assessment of patients presenting to primary care with low back and leg pain and second for their contribution in the diagnosis of spinal nerve root involvement. For the purposes of this study and taking into account that in the majority of cases of LBP with nerve root involvement, disc prolapse or spinal stenosis is the underlying cause, the Delphi participants were asked to assume that other possibilities and uncommon diagnoses such as ‘red flags’, vascular conditions and syndromes such as ‘piriformis’ had been excluded.
Phase 2: Delphi study
Participants
The multidisciplinary group who participated in phase 1, identified a second group of GPs, physiotherapists, rheumatologists, osteopaths, chiropractors, orthopaedic surgeons, neurosurgeons, considered to be experts and/or opinion leaders in the assessment and treatment of LBP and leg pain, from primary and secondary care settings. Inclusion criteria for this expert Delphi panel were relevant clinical experience and a declared interest in assessing LBP. All participants were working in clinical practice. Seventy-five experts from the UK were approached and sixty expressed interest in participating. The members of the multidisciplinary team, which compiled the initial list of items, did not participate in the Delphi study.
Delphi procedure
All 60 clinical experts were e-mailed explaining the purpose of the study and inviting their participation. They were also e-mailed an internet link to the online questionnaire. A consent form was electronically completed and submitted with the questionnaire. The Delphi survey ran from March to July 2010. Participants were given 5 weeks to respond to each round. Follow-up reminder e-mails were sent to non-respondents to each round.
Round 1. The items (n = 58) were presented to the Delphi participants by domain and they were asked to rate each item according to its importance on a scale from 1 (extremely unimportant) to 9 (extremely important) and to add any additional comments relating to the question and possible response options. The rating was performed twice: first for the importance of the item for inclusion in the clinical assessment schedule of adults with low back-associated leg pain, and second for the importance of the item in the diagnosis of nerve root involvement. An example is provided below (adapted from Bernstein et al. [2]):
How important to you is item 2 in the assessment of adults with low back-associated leg pain?
![]()
How important to you is item 2 in diagnosing nerve root involvement when assessing adults with low back-associated leg pain?
![]()
The first Delphi round questionnaire offered the opportunity to write general comments as well as specific comments about each item and to suggest additional items for inclusion. The list of all items included in round 1 is presented in Supplementary Appendix 1.
Consensus
In consensus research, there are no standardised guidelines about definitive level of agreement required and accepted levels in studies vary considerably [14] with levels set arbitrarily according to the importance of a study’s outcomes [18]. In this study, the level of agreement on the ‘importance’ or ‘unimportance’ of an item was set a priori at >70%. Items rated between ‘7 and 9’ by >70% of the participants were classed as important and items rated between ‘1 and 3’ by >70% and between ‘4 and 6’ by >70% of the participants were classed as unimportant and of uncertain importance, respectively. Disagreement was defined as the outcome in the case of an item being rated as unimportant (1–3) by >30% of the participants and as important (7–9) by >30% [2]. All other combinations in the rating of the items were considered as lack of consensus [2].
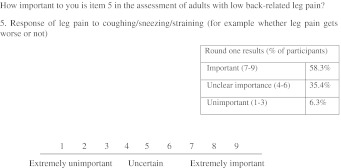
Round 2. The results of Round 1 were presented to the participants in Round 2 using descriptive statistics. A summary of the items for which consensus was reached was e-mailed to all participants and percentage agreement for each remaining item was presented in the Round 2 Delphi questionnaire. An example is presented in Fig. 1.
Fig. 1.
Example of the information on percentage agreement shown to participants in Round 2
All items that reached >70% agreement in Round 1 were excluded from Round 2. The participants were asked to re-rate the remaining items in the light of Round 1 percentage agreement information.
Phase 3
In phase 3, the multidisciplinary group that compiled the initial list of items for consideration in the Delphi survey in phase 1, met again (some face to face meetings and some e-mail and telephone communications) to compiled the final list of items for inclusion in the clinical assessment schedule. This group considered the items that did not reach consensus in the Delphi study for inclusion in the assessment process. An item that did not reach consensus could be included when more than 70% of the multidisciplinary group felt that it should be included in the assessment on the basis of its clinical relevance.
Results
Phase 1
A list of 58 items presented by domain (i.e. pain, function, etc.) was compiled.
Phase 2
The response rates were 80% (n = 48) and 87.5% (n = 42) for Round 1 and 2 of the Delphi process, respectively. The participants’ demographic characteristics are presented in Table 1.
Table 1.
Participant characteristics
| Round 1 (n = 48) | Round 2 (n = 42) | |
|---|---|---|
| Gender | ||
| Male (%) | 35 (73) | 29 (69) |
| Female (%) | 13 (27) | 13 (31) |
| Profession | ||
| GP (%) | 9 (19) | 8 (19) |
| Rheumatologist (%) | 6 (13) | 6 (14) |
| Physiotherapist (%) | 14 (29) | 13 (31) |
| Osteopathy (%) | 6 (13) | 6 (14) |
| Chiropractic (%) | 7 (15) | 5 (12) |
| Spinal surgeon (%) | 6 (13) | 4 (10) |
| Work setting | ||
| Primary care NHS (%) | 16 (33) | 15 (36) |
| Secondary care NHS (%) | 16 (33) | 13 (31) |
| Private (%) | 16 (33) | 14 (33) |
| Clinical experience with LBP patients | Mean = 19.2 years | Mean = 19.4 years |
| (SD 8.1) | (SD 7.9) | |
| Range: 6–43 years | Range: 6–43 years | |
| % of work related to LBP |
Mean = 45.4% (SD 31.2%) Range: 5–100% (n = 47, one missing) |
Mean = 42.8% (SD 29.0%) Range: 5–100% (n = 42) |
In Round 1, there was >70% agreement on 25 items as to their importance in the clinical assessment of adults with low back-associated leg pain and >70% agreement on 13 items as to their importance in diagnosing nerve root involvement. See Tables 2 and 3 for details of the items rated as important in the clinical assessment process and in the diagnosis of nerve root involvement.
Table 2.
Items contributing to the assessment process in general, rated as important by >70% of the participants
| Clinical assessment of low back-related leg pain in primary care | |
|---|---|
| Importance of each item rated according to its contribution to any of the following decisions: | |
| Establishing severity of symptoms | |
| Establishing need for investigations | |
| Establishing need for treatment/onwards referral | |
| Establishing the likely diagnosis | |
| Informing treatment | |
| Predicting prognosis | |
| History items | |
| Items/questions | Important (7–9 on scale) |
| Domain: pain | |
| Area or distribution of pain in the leg | 93.8% (n = 45) |
| Progression of pain in the leg since onset of current episode (e.g. better/worse/same) | 87.5% (n = 42) |
| Severity of pain in the leg compared with severity of pain in the low back | 85.4% (n = 41) |
| Progression of LBP (e.g. better/worse/same) | 83.3% (n = 35) |
| Pain intensity in the leg | 79.2% (n = 38) |
| Aggravating and easing factors for the leg pain | 77.1% (n = 37) |
| Duration of symptoms in the leg | 75% (n = 36) |
| Response of leg pain to cough/sneeze/strain | 73.8% (n = 31) |
| Quality of pain in leg (e.g. burning, sharp, tingling, etc.) | 73.8% (n = 31) |
| Domain: symptoms other than pain | |
| Altered sensation in the leg (e.g. reporting of numbness and/or pins and needles, etc.) | 83.3% (n = 40) |
| Feeling of weakness in the leg | 83.3% (n = 40) |
| Domain: previous history | |
| Effect of previous self-management | 81.0% (n = 34) |
| Effect of previous treatment for similar symptoms | 78.6% (n = 33) |
| Previous history of similar leg pain | 76.2% (n = 32) |
| Domain: function | |
| Effect of leg pain on ability to work | 83.3% (n = 40) |
| Effect of leg pain on activities of daily living | 83.3% (n = 40) |
| Effect of back pain on activities of daily living | 79.2% (n = 38) |
| Effect of back pain on ability to work | 79.2% (n = 38) |
| Effect of leg pain on ability to do leisure activities/sports | 71.4% (n = 30) |
| Domain: psychosocial factors | |
| Assessment of patient’s perceptions and beliefs pertaining to their condition | 91.7% (n = 44) |
| Assessment of patient’s coping strategies | 89.6% (n = 43) |
| Assessment of patient’s distress | 87.5% (n = 42) |
| Assessment of patient’s fear and apprehension of movement | 85.4% (n = 41) |
| Assessment of patient’s future outlook | 85.4% (n = 41) |
| Assessment of patient’s mood | 83.3% (n = 40) |
| Assessment of effect of symptoms on family situation | 79.2% (n = 38) |
| Assessment of work issues | 77.1% (n = 37) |
| Examination items | |
| Observation | |
| Muscle wasting | 85.4% (n = 41) |
| Spinal movements | |
| Demonstration of movement that produces symptoms | 71.4% (n = 30) |
| Neurological examination | |
| Assessment of muscle strength related to specific myotomes | 89.6% (n = 43) |
| Assessment of reflexes | 83.3% (n = 40) |
| SLR response on ‘well’ leg (cross-over pain) | 83.3% (n = 35) |
| Assessment of neural tension tests (SLR, femoral, slump) | 77.1% (n = 37) |
| Assessment of sensory appreciation | 72.9% (n = 35) |
Table 3.
Items contributing only to the diagnosis of nerve root involvement rated as important by >70% of the participants
| Clinical assessment of low back-related leg pain in primary care | |
|---|---|
| Importance of each item rated according to its contribution to the diagnosis of nerve root involvement only | |
| History items | |
| Domain: pain | Important (7–9 on scale) |
| Area or distribution of pain in the leg | 97.9% (n = 47) |
| Severity of pain in the leg compared with severity of pain in the low back | 83.3% (n = 40) |
| Pain intensity in the leg | 72.9% (n = 35) |
| Quality of pain in the leg (e.g. pain descriptors such as burning, tingling, etc.) | 72.9% (n = 35) |
| Response of leg pain to coughing/sneezing/straining (e.g. whether leg pain gets worse or not) | 72.9% (n = 35) |
| Aggravating and easing factors for the leg pain | 72.9% (n = 35) |
| Progression of leg pain (e.g. better/worse/same) | 71.4% (n = 30) |
| Domain: symptoms other than pain | |
| Altered sensation in the leg (e.g. reporting of numbness and/or pins and needles, etc.) | 91.7% (n = 44) |
| Feeling of weakness in the leg | 77.1% (n = 37) |
| Examination items | |
| Observation | |
| Muscle wasting | 91.7% (n = 44) |
| Neurological examination | |
| Assessment of muscle strength related to specific myotomes | 95.8% (n = 46) |
| Assessment of neural tension tests (SLR, femoral, slump) | 89.6% (n = 43) |
| Assessment of reflexes | 87.5% (n = 42) |
| Assessment of sensory appreciation | 83.3% (n = 40) |
| SLR response on ‘well’ leg (cross-over pain) | 81.0% (n = 34) |
The ‘agreed upon’ items were removed from Round 2. One new item was suggested by two participants and was added in the Round 2 Delphi questionnaire. In Round 2, there was >70% agreement on a further nine items, as to their importance for inclusion in the clinical assessment. Over 70% agreement was also reached for 2 items, including the one added from Round 1, regarding the importance of their contribution to diagnosing nerve root involvement. See Tables 2 and 3 for details.
All other remaining items did not reach the >70% agreement threshold for being either unimportant or of uncertain importance indicating lack of consensus. There was no disagreement on any item in the sense that no item was simultaneously rated by >30% of the respondents as important and by >30% of the respondents as unimportant.
Phase 3
The multidisciplinary group that compiled the initial list of items discussed and made a final decision on the items that did not reach consensus in the Delphi study, and compiled the final list of items for inclusion in the clinical assessment schedule to be used in the planned cohort study. The agreed clinical assessment schedule is presented in Supplementary Appendix 2 (‘red flags’ items are also part of the assessment as is standard practice but that was outside the remit of the Delphi consensus study).
All the items reaching consensus from the Delphi procedure were included. From the 24 history items that did not reach consensus for inclusion in the clinical assessment, the team agreed to include four items. The first was about medication intake and its effect on symptoms (‘important’ 64.3%), the second about sleep disturbances (‘important’ 57.1%), the third was combining the questions about similar previous history of back/leg pain (the question about similar previous history of back pain not reaching consensus) and the forth enquiring about compensation issues if relevant (‘important’ 57.1%). Although these items did not reach the consensus threshold of 70%, the multidisciplinary group considered the question about medication and its effect on symptoms as important in deciding further management, the question about sleep disturbances was deemed important in assessing the possibility of red flags and also deciding management (i.e. medication). The question about compensation issues was retained as it may influence prognosis.
From the 11 examination items that did not reach consensus for inclusion in the clinical assessment, the team agreed to include four items. The first was postural assessment (i.e. antalgic shift, scoliosis) (‘important’ 54.8%), the second was palpation of the lumbar spine (‘important’ 42.9%), the third was range of movement in relation to pain reproduction (see assessment schedule in Supplementary Appendix 2 for detail). Brief assessment of the hip joint as an exclusion test was also included in the assessment (‘important’ 61.9%). Again, the multidisciplinary group considered that simple observation findings such as antalgic shift, scoliosis should be recorded as an indication of severity and rarely as an indication of serious underlying pathology. Palpation was included for assessing severe bony tenderness. Pain response to movements was included as an extension to the item; ‘demonstration of movement that produces symptoms’, as it was thought to provide clues as to the mechanical nature of LBP. Finally, brief assessment of the hip joint for the purpose of excluding it as the source of symptoms was included as most participants commented in free text that they would assess the hip for that reason.
Discussion
This study used a Delphi approach to first identify and agree on the items that were important in the clinical assessment of patients consulting with low back-associated leg pain, for use in primary care, and second to identify and agree on the items that were most likely to contribute to the diagnosis of nerve root involvement. The assessment schedule thus formed will be used in a future cohort study investigating prognostic indicators of outcome in patients presenting in primary care with back and leg pain. The validity of the diagnostic items will also be investigated in future studies involving primary care populations and agreed reference standards.
There are a number of published papers related to the assessment and treatment of lumbar spinal nerve root involvement or sciatica [10, 11, 22, 23]. Although many studies in the field of LBP with spinal nerve root involvement describe their inclusion criteria based on history and physical examination findings and diagnostic tests, these vary considerably between studies and often there is very little information provided on the actual assessment employed. Hence, the characteristics of each study’s cohort are particular to each study and comparisons between cohorts is difficult. In this study, we endeavoured to produce a generalisable assessment schedule by consensus, by involving all relevant disciplines that assess patients with LBP and leg pain in the UK, from all relevant settings.
An initial multidisciplinary group produced a list of items, which was presented to the Delphi panel of expert clinicians for scoring. The Delphi participants were asked to score each item first considering its importance to the clinical assessment and second considering its contribution to the diagnosis of nerve root involvement only. The term ‘nerve root involvement’ rather than specific pathology, such as disc prolapse for example, which may be the reason for nerve root involvement, was considered more appropriate diagnostic heading for use in a primary care population, who would not usually have access to imaging required to confirmed specific diagnoses, at least in the initial stages.
Assessment items
The clinical items and physical examination tests that were considered by the Delphi participants as important for their contribution to the clinical assessment process were typical of those described in guidelines and specialty textbooks and relate to leg symptoms, such as pain distribution, pain quality and behaviour as well as altered sensations, with pain distribution given higher levels of importance as compared to quality descriptors of pain and altered sensations such as pins and needles or numbness. Assessment of function and psychological status (yellow flags) as well as previous history of similar symptoms and the outcome of previous treatment/management were considered important aspects of the assessment. There was high consensus on the importance of psychosocial factors in the assessment which is indicative of the integration of the biopsychosocial model’s principles in the assessment of back pain problems. Examination tests considered important included typical neurological tests including neural tension tests (e.g. Straight Leg Raise). In terms of spinal movement examination only ‘demonstration of movement that produces symptoms’ was considered important. Delphi participants were uncertain about the usefulness of tests such as active lumbar range of movement and effect of repeated movements on pain. The assessment of ‘repeated movements’ and the value of this item to prognosis for example, is more often encountered in the physiotherapy literature and other disciplines may not use it as much, hence the low rating in this multidisciplinary Delphi study. There was no consensus on palpation and observation items despite textbooks generally recommending observations of spinal posture, curvature and palpation and clinicians typically making such observations. Perhaps these observations are made for other reasons and not because of their direct contribution to informing diagnosis or management in the absence of any indication of serious pathology.
Diagnostic items
When considered the set of items from the history that contribute to diagnosis of nerve root involvement alone, only items relating to pain and its behaviour and feeling of altered sensations or weakness, together with aggravating and easing factors, were considered important in diagnosis. Although specific aggravating/easing factors and their effect on pain were not always defined in detail, a number of participants quoted examples such as walking and sitting for spinal stenosis. All of the nine history items considered important by the Delphi participants in this study and their diagnostic accuracy have been reported in the literature [24], although these were derived from a highly selected population at the severe end of the spectrum of suspected lumbosacral nerve root compression.
In terms of examination items, only neurological examination tests, including neural tension and observational findings relating to potential nerve root compromise (such as muscle wasting) were considered important. Evidence of muscle wasting or weakness was the most important (95.8% consensus) and it is reported in the literature as the most diagnostic sign (Odds ratio; 5.2) [24]. Overall, six items from examination were considered important (>70% agreement) in contributing to the diagnosis of nerve root involvement.
In agreement with the literature on associations of various clinical findings and lumbosacral nerve root compression due to suspected disc herniations, there are more history items than examination items that are considered helpful in diagnosis although their relative contributing strength (as indicated by the odds ratios) varies considerably [24].
Limitations
Although the Delphi method involving experts for reaching consensus agreement is used widely in issues of LBP such as definitions [25] or for minimal necessary documentation of treatments [26], there are potentially a number of limitations inherent to consensus studies that must be considered when interpreting the results of this study. The choice of the expert Delphi participants in the absence of standardised guidelines for defining and selecting experts, may be open to challenge. We selected participants based on assumptions about skills, clinical role and participants’ expressed interest in the area. From the characteristics, we inferred expertise. It is possible that using different selection criteria or selecting an alternative group of experts may have produced different results. Nevertheless, a strength of this study is that participants came from several disciplines (including general practice, physiotherapy and rheumatology) increasing the likelihood that our results will be generalisable, or strongly suggesting that these results are key factors in the assessment and diagnosis across a wide range of professions.
However, the assessment schedule compiled based on the Delphi results and the list of diagnostic criteria for nerve root involvement produced, are quite similar to those proposed in the literature. This suggests that the assessment schedule derived from our results would be in accord to that used by other clinicians in the field of LBP. In addition, the diagnostic criteria for nerve root involvement appear to have face and content validity being quite similar to those proposed in the literature [13, 24].
Conclusion
This study has generated an expert consensus derived assessment schedule for use in a primary care unselected cohort of patients with low back and leg pain which is designed to investigate prognostic indicators in this patient group. It has also produced a list of items from the history and clinical examination that are considered to contribute to the diagnosis of nerve root involvement. The validity of these items in diagnosing nerve root involvement in an unselected primary care population will also be investigated in further studies.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
We thank Carol Doyle, Nasri Ahmed, Elaine Hay and Paula Salmon, members of the multidisciplinary Delphi team that compiled the initial list of items. This study is funded through a National Institute for Health Research (NIHR) Programme Grant. Dr Konstantinou is supported by an NIHR Clinical Lectureship Grant. We are grateful to all 42 experts that participated in the Delphi consensus study and completed Round 2. Peter Millner, Chris Gerber, Philip Sell, John O’Dowd, Alan Breen, Haymo Thiel, Paul Bruno, Aaron Coode, Neil Osborne, Ruth Sephton, Susan Greenhalgh, Janet Suckley, Carl Hancock, Anna White, Frances Arnall, Jo Jarvis, Verna Cuthbert, Catherine Cliffe, Narender Nalajala, Elaine Whiltshire, Michael Reddington, Claire Small, Julie Dawson, David Walsh, Jon Packham, Marwan Bukhari, Jeremy Jones, Adrian Jones, Ian Bernstein, Simon P Petrides, Louise Thwaites, Louise Warburton, Bruce Thompson, Mark Devlin, Mark Couldrick, Adrian Dunbar, Jorge Esteves, David Evans, Paddy Searle-Barnes, Greg Sharp, Tim McClune and Charles Peers.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Beech B. The Delphi approach: recent applications in health care. Nurse Res. 2001;8:38–47. [Google Scholar]
- 2.Bernstein SJ et al (1992) Coronary angiography: a literature review and ratings of appropriateness and necessity. Santa Monica (CM). Report JRA-03
- 3.Carragee EJ. Psychological screening in the surgical treatment of lumbar disc herniation. Clin J Pain. 2001;17:215–219. doi: 10.1097/00002508-200109000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Chiodo A, Haig AJ. Lumbosacral radiculopathies: conservative approaches to management. Phys Med Rehabil Clin N Am. 2002;13:609–621. doi: 10.1016/S1047-9651(02)00021-9. [DOI] [PubMed] [Google Scholar]
- 5.Dagenais S, Tricco AC, Haldeman S. Synthesis of recommendations for the assessment and management of low back pain from recent clinical practice guidelines. Spine J. 2010;10:514–529. doi: 10.1016/j.spinee.2010.03.032. [DOI] [PubMed] [Google Scholar]
- 6.European Commission (EC), Cost Action B13 Management Committee (2004) European Guidelines for the management of acute low back pain. Available from: http://www.backpaineurope.org [Accessed January 2009]
- 7.European Commission (EC), Cost Action B13 Management Committee (2004) European Guidelines for the management of chronic low back pain. Available from: http://www.backpaineurope.org [Accessed January 2009]
- 8.Fairbank JCT. An archaic term. BMJ. 2007;335:112. doi: 10.1136/bmj.39275.951343.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Felson DT, Anderson JJ. Methodological and statistical approaches to criteria development in rheumatic diseases. Baillieres Clin Rheumatol. 1995;9(2):253–266. doi: 10.1016/S0950-3579(05)80189-X. [DOI] [PubMed] [Google Scholar]
- 10.Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Prac Res Clin Rheumatol. 2010;24:253–265. doi: 10.1016/j.berh.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Genevay S, Atlas SJ, Katz JN. Variation in eligibility criteria from studies of radiculopathy due to a herniated disc and of neurogenic claudication due to lumbar spinal stenosis. A structured literature review. Spine. 2010;35:803–811. doi: 10.1097/BRS.0b013e3181bc9454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hasenbring M, Marienfeld G, Kuhlendahl D, et al. Risk factors of chronicity in lumbar discpatients. A prospective investigation of biologic, psychologic, and social predictors oftherapy outcome. Spine. 1994;19:2759–2765. doi: 10.1097/00007632-199412150-00004. [DOI] [PubMed] [Google Scholar]
- 13.Haswell K, Gilmour J, Moore B. Clinical decision rules for identification of low back pain patients with neurologic involvement in primary care. Spine. 2008;33:68–73. doi: 10.1097/BRS.0b013e31815e3949. [DOI] [PubMed] [Google Scholar]
- 14.Hicks CM. The Delphi technique. Research methods for clinical therapists: applied project design and analysis. Edinburgh: Churchill Livingstone; 1999. pp. 243–249. [Google Scholar]
- 15.Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311:376–380. doi: 10.1136/bmj.311.7001.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koes BW, van Tulder MW, Peul WC. Diagnosis and treatment of sciatica. BMJ. 2007;334:1313–1317. doi: 10.1136/bmj.39223.428495.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Konstantinou K, Dunn KM. Sciatica: review of epidemiological studies and prevalence estimates. Spine. 2008;33(22):2464–2467. doi: 10.1097/BRS.0b013e318183a4a2. [DOI] [PubMed] [Google Scholar]
- 18.Powell C. The Delphi technique: myths and realities. J Adv Nurs. 2003;41:376–382. doi: 10.1046/j.1365-2648.2003.02537.x. [DOI] [PubMed] [Google Scholar]
- 19.van der Windt DA, Simons E, Riphagen II et al. (2010) Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain. Cochrane Database Syst Rev. Feb 17;(2):CD007431 [DOI] [PubMed]
- 20.van Tulder MW, Koes BW, Bouter LM. A cost-of-illness study of back pain in The Netherlands. Pain. 1995;62:233–240. doi: 10.1016/0304-3959(94)00272-G. [DOI] [PubMed] [Google Scholar]
- 21.van Tulder M, Koes B, Bombardier C. Low back pain. Best Prac Res Clin Rheumatol. 2002;16:761–775. doi: 10.1053/berh.2002.0267. [DOI] [PubMed] [Google Scholar]
- 22.van Tulder M, Peul W, Koes B. Sciatica: what the rheumatologists needs to know. Nat Rev Rheumatol. 2010;6:139–145. doi: 10.1038/nrrheum.2010.3. [DOI] [PubMed] [Google Scholar]
- 23.Valat JP, Genevay S, Marty M, Rozenberg S, Koes B. Sciatica. Best Prac Res Clin Rheumatol. 2010;24:241–252. doi: 10.1016/j.berh.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 24.Vroomen PCAJ, de Krom MCTFM, Wilmink JT, et al. Diagnostic value of history and physical examination in patients suspected of lumbosacral nerve root compression. J Neurol Neurosurg Psychiatr. 2002;72:630–634. doi: 10.1136/jnnp.72.5.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stanton TR, Latimer J, Maher CG, Hancock M. A modified Delphi approach to standardise low back pain recurrence terminology. Eur Spine J. 2011;20:744–752. doi: 10.1007/s00586-010-1671-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kessler JT, Melloh M, Zweig T, et al. Development of a documentation instrument for the conservative treatment of spinal disorders in the International Spine Registry, Spine Tango. Eur Spine J. 2011;20:369–379. doi: 10.1007/s00586-010-1474-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.