Abstract
Background
Anatomical study of the relationship among the cervical nerve roots, intervertebral disc, and lateral mass is important for the neurosurgeon to avoid complications of posterior cervical foraminotomy.
Methods
Six adult cadavers were studied. The muscles of the back of the neck were removed to expose the cervical vertebrae posteriorly from C3 to C7. We measured the length, height, extent, and angulations of the nerve roots from the medial point of the facet (MPF) after a total laminectomy, then after one-half facetectomy. The height, width, anteroposterior diameter of the lateral mass, then the height and anteroposterior diameter of the neural foramen were also measured.
Results
After total laminectomy from C3 to C7, all measures were taken from MPF showed that the mean length of the exposed root was 6.5–8.8 mm while vertical distance was 4–5.4 mm and the horizontal distance was 5.1–7.1 mm. Following a medial one-half facetectomy; the mean length of the exposed root was 8.9–12.3 mm, the vertical distance was 5.5–7.3 mm while the horizontal distance was 7.1–9.8 mm. The mean angulations of the nerve roots were 50.9–53.3º. There was a significant difference after total laminectomy and medial one-half facetectomy.
Conclusion
Anatomic and morphologic study of the cervical nerve roots and their relationships to the lateral mass and the intervertebral disc are useful landmarks to reduce the operative complications of the posterior foraminotomy.
Keywords: Posterior cervical foraminotomy, Cervical laminoforaminotomy, Cervical nerve root anatomy
Introduction
The posterior approach of cervical disc was originally reported by Mixter [19], and the key-hole foraminotomy was subsequently popularized by Scoville, Epstein, and Fager [5, 7, 10, 11, 13, 16, 25, 27]. Many reports noted the term laminoforaminotomy for management of paracentral and foraminal cervical disc. However, despite the lesser intraoperative and postoperative risks, the laminoforaminotomy has lost ground when compared with anterior approaches for the management of lateral and foraminal cervical pathology [9, 22, 27].
The posterior laminoforaminotomy is primarily indicated for foraminal lesions and is highly effective in treating cervical radiculopathy, and improving patient’s quality-of-life outcomes as allows the motion preservation via a minimally invasive approach [2].
Advances have been made with the posterior approach with the development of minimally invasive surgery by microsurgical and endoscopic equipments which gain an excellent outcome results up to 93–96% of patients with motion preservation [7].
The advantages of the posterior approach include, (1) avoid damage to vital structures located in the anterior area of the cervical spine, (2) avoid the structural and biomechanical damage to the remaining vertebral disc (joint morbidity, bone graft complication, as well as the adjacent joint syndrome) [4, 12, 14, 17].
The complications reported with this approach include nerve root injury, dural tear, spinal cord injury with and without K-wire misplacement, same-segment and adjacent-segment syndrome, and spinal instability [2, 18, 26].
When a posterior foraminotomy is performed for the removal of an intervertebral disc, it is essential to understand the anatomical relationships between the nerve roots, its course within the neural foramen, and intervertebral disc and its relation to the nerve root to improve the operative outcome.
The objective of this study was to define the anatomical relationship of the cervical nerve root when crossing over the intervertebral disc through the neural canal, and the lateral mass after a total laminectomy and then after a medial one-half facetectomy to assist neurosurgeons for safely performing posterior foraminotomy.
Materials and methods
Six formalin-fixed adult Egyptian cadavers (four males and two females) with mean age 54 years and age range 42–65 years were used in this work. We dissected all the muscles of the back of the neck to expose the cervical vertebrae from C3 to C7 as it was hard to study the nerve roots and their relationship with the intervertebral discs by minimal cadaveric muscle dissection as in live patients because of the cadaveric muscle stiffness due to Rigor mortis phenomenon.
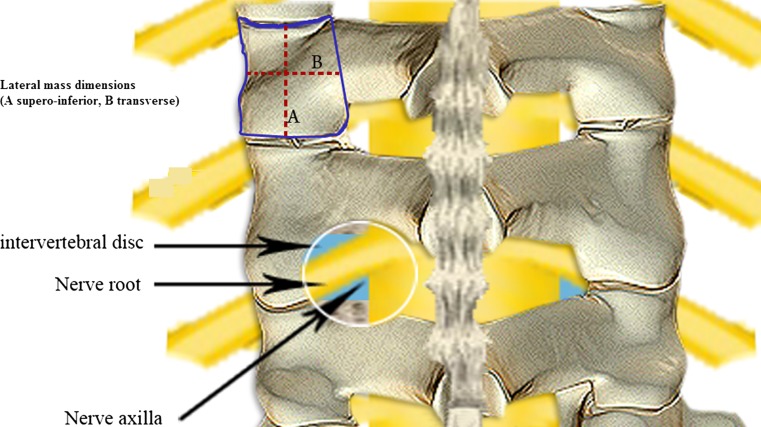
The lateral mass which is the bony part between the superior and inferior facet was exposed and measured in multiple dimensions including (a) the height (superoinferior diameter) posteriorly measured from the edge of the superior facet to the edge of the inferior facet, (b) the width (transverse diameter) of the lateral mass was measured from MPF to the lateral edge of the vertebra, and (c) the anteroposterior diameter of the lateral mass in the sagittal plane.
The supero-inferior as well as the antero-posterior diameter of the neural foramen which located just anterior to the superior articular facet of the inferior vertebra and the inferior articular facet of the superior vertebra were also measured (Fig. 1).
Fig. 1.
Demonstration of lateral mass measures (A superoinferior diameter, B width) and morphological relationship of nerve root after foraminotomy
A meticulous total laminectomy was performed from C3 to C7 vertebrae by excision of the laminae till the medial point of the facet joint (MPF) of the lateral mass. The following measurements were obtained based on MPF: (a) the length of the exposed nerve root, (b) the horizontal distance to the lateral margin of the dura, (c) the vertical distance to the axilla of the nerve root, then after measuring the vertical, horizontal, and oblique distances from the MPF and (d) the angulations of the axilla of nerve roots were measured (Fig. 2).
Fig. 2.
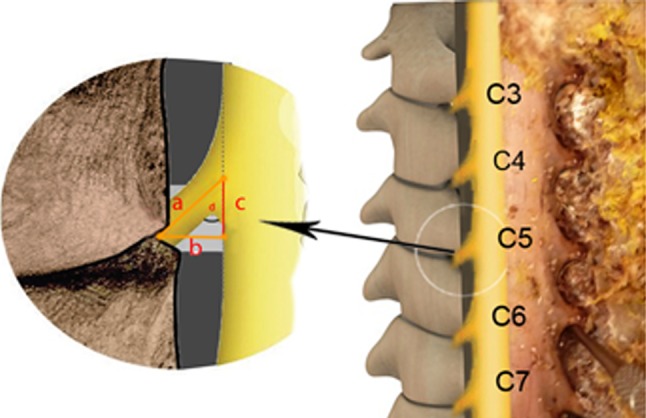
Nerve roots measurements after laminectomy. a The length of the exposed nerve root, b the horizontal distance, c the vertical distance, d the angulations of the nerve roots
Then a medial one-half facetectomy was also done including about 50% of the cervical facet joints. All measurements were done again, based on the MPF of the lateral mass: (a) the length of the exposed nerve root, (b) the horizontal distance to the lateral surface of the dura, (c) the vertical distance to the axilla of the nerve root, (d) the angulations of the axilla of nerve roots (Fig. 3).
Fig. 3.
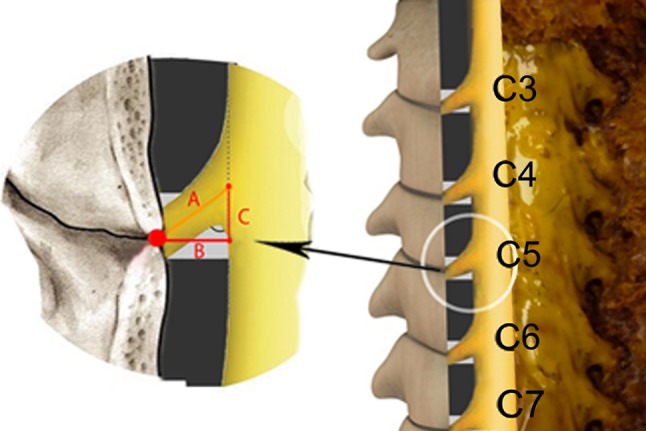
Nerve roots measurements after facetectomy. a The length of the exposed nerve root, b the horizontal distance, c the vertical distance, d the angulations
All measurements were made using (1) a protractor to define the distance between points, (2) a diamond Master Vernier Calliper to measure the distances and (3) an orthopaedic goniometer. All angulations were measured using an internet program rechner for rechtecke (http://www.arndt-bruenner.de/mathe/scripts/rechteckrechner.htm). The SPSS software (version 11.0) was used to perform a t test with the threshold p value set at 0.05.
Results
Lateral mass
The mean superoinferior diameters of the lateral mass from C3 to C7 ranged from 11.2 ± 1.4 to 2.3 ± 1.6 mm, and the mean transverse diameters ranged from 10.3 ± 1.7 to 12.8 ± 1.5 mm while the mean anteroposterior diameter ranged from 10.4 ± 1.3 to 11.9 ± 1.7 mm.
The mean height of the neural foramen was insignificantly different from C3 to C7 which was 7.8 ± 1–8.8 ± 1.1 mm while the anteroposterior diameter was found 4.4 ± 0.9–6.2 + 1.1 mm at C3 through C7 (Table 1).
Table 1.
Measurements of the lateral mass and the neural foramen
| Distance in mm (mean + SD) mm | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lateral mass | Foramen | ||||||||||||||
| Superoinferior | Anteroposterior | Mediolateral | Height | Anteroposterior | |||||||||||
| Mean | Min | Max | Mean | Min | Max | Mean | Min | Max | Mean | Min | Max | Mean | Min | Max | |
| C3 | 11.2 ± 1.4 | 9 | 14 | 10.4 ± 1.3 | 8 | 12 | 10.3 ± 1.7 | 8 | 14 | 8.4 ± 0.9 | 7 | 10 | 4.4 ± 0.9 | 3 | 6 |
| C4 | 11.3 ± 2 | 9 | 15 | 11.3 ± 1.7 | 8 | 13 | 11.3 ± 2.1 | 8 | 16 | 7.8 ± 1 | 6 | 9 | 4.1 ± 0.7 | 3 | 5.5 |
| C5 | 11.2 ± 1.6 | 8 | 14 | 11.3 ± 0.9 | 10 | 13 | 11.3 ± 1.1 | 10 | 13 | 8.1 ± 1.3 | 6 | 10 | 4.7 ± 0.8 | 4 | 6 |
| C6 | 11.3 ± 1.4 | 9 | 14 | 11 ± 1.8 | 8 | 14 | 12.1 ± 2.1 | 9 | 17 | 8.6 ± 1.2 | 7 | 11 | 5 ± 0.7 | 4 | 6 |
| C7 | 12.3 ± 1.6 | 9 | 13 | 11.9 ± 1.7 | 10 | 15 | 12.8 ± 1.5 | 8 | 13 | 8.8 ± 1.1 | 7 | 11 | 6.2 ± 1.1 | 5 | 9 |
Measurements of the nerve roots after laminectomy
After total laminectomy, the length of the exposed nerve roots to the medial point of facet (MPF) at all levels from C3 to C7 was found 6.5 ± 0.8–8.8 ± 0.8 mm with insignificant difference. The horizontal distance from the MPF to the lateral surface of the dura was found 5.1 ± 0.9–7.1 ± 0.9 mm with gradual elongation downward. The vertical distance to the axilla of the nerve root was 4 ± 0.6–5.4 ± 0.5 mm without significant difference Table 2.
Table 2.
Measurements after laminectomy
| Distance in mm (mean + SD) mm | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N root length | Horizontal distance | Height | Angulation | |||||||||
| Mean | Min | Max | Mean | Min | Max | Mean | Min | Max | Mean | Min | Max | |
| C3 | 6.5 ± 0.8 | 5.5 | 8 | 5.1 ± 0.9 | 3.9 | 6.5 | 4 ± 0.6 | 2.7 | 5.0 | 51.3 ± 6.4 | 43.9 | 61.0 |
| C4 | 7.1 ± 0.6 | 6.1 | 8 | 5.6 ± 0.7 | 4.5 | 6.5 | 4.4 ± 0.6 | 3.3 | 5.7 | 50.9 ± 5.4 | 44.4 | 62.7 |
| C5 | 7.5 ± 0.5 | 6.5 | 8 | 5.8 ± 0.6 | 5 | 6.9 | 4.7 ± 0.6 | 3.6 | 5.3 | 51.3 ± 4.9 | 46.4 | 62.2 |
| C6 | 8.6 ± 0.8 | 7.6 | 10 | 6.6 ± 0.5 | 5.2 | 7.9 | 5.4 ± 0.5 | 4.4 | 6.1 | 50.9 ± 3.9 | 43.2 | 59.3 |
| C7 | 8.8 ± 0.8 | 7.4 | 10 | 7.1 ± 0.9 | 5.1 | 8.3 | 5.2 ± 0.4 | 4.4 | 5.8 | 53.3 ± 4.2 | 43.6 | 61.7 |
Measurements following medial one-half facetectomy
After one-half facetectomy; the length of the exposed nerve roots from C3 to C7, was found 8.9 ± 0.8–12.3 ± 0.8 mm. There was a significant difference compared with the total laminectomy (P 0.002–0.004).
The horizontal distance to the lateral surface of the dura was 7.1 ± 1–9.8 ± 0.7 mm. This was significant compared with the total laminectomy (P 0.001–0.004); the horizontal distance to the dura was longer by about 3–4 mm on average.
The vertical distance to the axilla of nerve roots from C3 to C7 was 5.5 ± 0.6–7.3 ± 1. There was a significant difference at C3–C5 (P 0.001–0.004) Table 3.
Table 3.
Measurements following medial one-half facetectomy
| Distance in mm (mean + SD) mm | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N root length | Horizontal | Height | Angulation | ||||||||||||
| Mean | Min | Max | P | Mean | Min | Max | P | Mean | Min | Max | P | Mean | Min | Max | |
| C3 | 8.9 ± 0.8 | 7.7 | 10 | 0.002 | 7.1 ± 1 | 5.5 | 8.2 | 0.001 | 5.5 ± 0.6 | 4.6 | 6.6 | 0.001 | 51.3 ± 6.4 | 43.9 | 61 |
| C4 | 9.5 ± 0.9 | 8.2 | 11 | 0.002 | 7.3 ± 0.9 | 6 | 8.9 | 0.001 | 6 ± 0.9 | 4.2 | 7.9 | 0.001 | 50.9 ± 5.4 | 44.4 | 62.7 |
| C5 | 9.8 ± 0.7 | 9 | 12 | 0.002 | 7.6 ± 0.8 | 6.5 | 9.7 | 0.01 | 6.1 ± 0.7 | 4.4 | 7 | 0.001 | 51.3 ± 5 | 46.4 | 62.2 |
| C6 | 11.3 ± 1 | 9.6 | 13 | 0.004 | 8.8 ± 1 | 7.3 | 10.1 | 0.004 | 7.1 ± 0.9 | 5.6 | 8.7 | 0.001 | 50.9 ± 3.9 | 43.2 | 59.3 |
| C7 | 12.3 ± 0.8 | 11 | 14 | 0.002 | 9.8 ± 0.7 | 8.7 | 11 | 0.003 | 7.3 ± 1 | 5.7 | 9.4 | 0.004 | 53.3 ± 4.2 | 43.6 | 61.7 |
The angle between the nerve root and the lateral margin of the dura was measured. The smallest angle was 50.9 ± 6.4°, corresponding to the C6 nerve root while the angle of the C7 nerve root was 53.3 ± 4.2° without any significant difference (P 0.7).
Discussion
Various anterior and posterior operative approaches for the treatment of cervical radiculopathy have been reported [5, 7, 8, 11, 13, 16, 25, 27]. Scoville [23] firstly described posterior foraminotomy through a partial resection of the medial part of facet joint to relieve the compression of the cervical nerve root.
Although the posterior approach has a great outcome results, the anterior approach has been more commonly used by neurosurgeons to treat cervical disc. There is a renewed interest by many surgeons with regard to the posterior approach to treat the paracentral and foraminal cervical disc due to the advancements of minimally invasive surgery and endoscopy with a series of reports detailing excellent treatment outcomes as the anterior approach need a more depth in dissection of structures to reach the cervical disc [2, 4, 12, 14, 15, 22]. Tumialan et al. [24] reported that posterior cervical foraminotomy offers a benefit relative to anterior cervical foraminotomy in immediate short-term direct costs and long-term indirect costs, early mobilization and outcome.
In order to simplify this approach we studied the anatomical landmarks and measurements of the lateral mass, nerve root (length, height, angulation), and disc “triad” to give an idea for the neurosurgeons to facilitate the approach, minimize the risk of complication, and to improve the outcome.
In order to do posterior key hole foraminotomy; it is necessary to remove 4–5 mm from the superior and inferior lamina using a high-speed drill to allow visibility of the dura till the lateral mass then about 4–5 mm from the lateral mass to provide a significantly greater exposure of the exiting nerve root for decompression and removal of laterally herniated disc [22].
In cases where posterior cervical foraminotomy and discectomy is performed via the posterior approach, the muscles should dissected to a minimal extent, using a narrow retractor and the lateral mass at the site of the lesion is secured after initial resection of the lateral part of the lamina to the point where it meets the lateral mass. This allows for visibility of the dura and the nerve root (6.5–8.8 mm) and the horizontal distance (5.1–7.1 mm) from MPF of the lateral mass at C3–C7. Based on our results, this short distance of nerve root clinically allows minimal mobilization of the nerve root to do discectomy and nerve root decompression. This agrees with Hwang et al. [15] who reported that after total laminectomy; the nerve root is still short to do easy mobilization and discectomy.
The extent of facet resection is based on the extent of foraminal pathology. Zdeblick et al. [26] performed successive 25, 50, 75, and 100% facetectomy in in vitro model to evaluate the impact of progressive facet resection on instability. They found significant segmental hypermobility occurred with greater than 50% facet resection and noted that resection of the facet should be limited to less than 50% to preserve the biomechanical function of the cervical vertebrae and to avoid the risk of cervical instability. This was confirmed by many authors [3, 6, 20, 21].
In our measurements of the lateral mass from C3 through C7, we found similar to the work of Abdullah et al. [1] that the mean range of superoinferior diameters was 11.2 + 1.4–12.3 + 1.6 mm, transverse diameters was 10.3 + 1.7–12.8 + 1.5 mm while the anteroposterior diameters was 10.4 + 1.3–11.9 + 1.7 mm. The mean height of the neural foramen was insignificantly different from C3 through C7 (7.8 + 1–8.8 + 1.1 mm) while the anteroposterior diameter was 4.4 + 0.9–6.2 + 1.1 mm. So, according to the previous reports [3, 6, 20, 21] and our results; it is safe to remove up to 5 mm of the lateral mass to allow easy mobilization of the nerve roots for discectomy without instability.
Our findings showed that the vertical distance to the axilla of the nerve root from C3 to C7 was 4–5.2 mm after laminectomy and 5.5–7.3 mm after facetectomy. So, it is important to put in mind that vertical distance to the axilla of the nerve root is 4–5 mm superior from the location of MPF after laminectomy and 5–7 mm after facetectomy. This mean that when the decompressive laminectomy of each segment is performed primarily for the superior rather than the inferior lamina, it should facilitates the disc removal from the axilla of nerve root, allows easy mobilization to attack it also from the shoulder, and prevent unnecessary damage to normal tissue. Hwang et al. [15] found other results varying from 1 to 3 mm without any significant difference.
In the present study; after total laminectomy from C3 through C7, we found the mean nerve root length was 6.5–8.8 mm while it was 8.9–12.3 mm after facetectomy with significant difference. The horizontal distance from MPF to the lateral surface of the dura was 5.1–7.1 mm after total laminectomy while it was 7.1–9.8 mm after facetectomy with significant difference. The vertical distance to the axilla of the nerve root was 4–5.4 mm after total laminectomy while it was 5.5–7.3 mm after facetectomy with significant difference (P 0.001). This indicates that length, height, and horizontal distance of the nerve roots changed significantly after facetectomy as reported by Hwang et al. [15].
The anatomical relationship of the intervertebral disc to the overlaying obliquely situated nerve root when looking from the narrow interlaminar fenester is too important to understand. To remove the herniated intervertebral disc and hypertrophied osteophyte, a nerve hook is placed in the axillary region. This is retracted superiorly, exposing the intervertebral disc after facetectomy and a sufficient degree of decompression can be confirmed based on findings that the nerve root is released freely when using a probe to manipulate an intervertebral foramen.
Conclusion
Anatomic and morphologic study of the cervical nerve roots and their relationships to the lateral mass and the intervertabral disc are useful landmarks to reduce the operative complications of the posterior foraminotomy.
Conflict of interest
I certify that there is no actual or potential conflict of interest in relation to this article. No previous presentation in any conference or journal.
Glossary
- MPF
Medial point of the facet
References
- 1.Abdullah K, Steinmetz M, Mroz T (2009) Morphometric and volumetric analysis of the lateral masses of the lower cervical spine. Spine (Phila Pa 1976) 34(14):1476–1479 [DOI] [PubMed]
- 2.Adamson T. Microendoscopic posterior cervical laminoforaminotomy for unilateral radiculopathy: results of a new technique in 100 cases. J Neurosurg. 2001;95(1):51–57. doi: 10.3171/jns.2001.95.1.0051. [DOI] [PubMed] [Google Scholar]
- 3.Baba H, Chen Q, Uchida K, Imura S, Morikawa S, Tomita K (1996) Laminoplasty with foraminotomy for coexisting cervical myelopathy and unilateral radiculopathy: a preliminary report. Spine (Phila Pa 1976) 21(2):196–202 [DOI] [PubMed]
- 4.Burke T, Caputy A. Microendoscopic posterior cervical foraminotomy: a cadaveric model and clinical application for cervical radiculopathy. J Neurosurg. 2000;93(1 Suppl):126–129. doi: 10.3171/spi.2000.93.1.0126. [DOI] [PubMed] [Google Scholar]
- 5.Cağlar YS, Bozkurt M, Kahilogullari G, Tuna H, Bakir A, Torun F, Ugur H. Keyhole approach for posterior cervical discectomy: experience on 84 patients. Minim Invasive Neurosurg. 2007;50(1):7–11. doi: 10.1055/s-2007-970138. [DOI] [PubMed] [Google Scholar]
- 6.Chen B, Natarajan R, An H, Andersson G. Comparison of biomechanical response to surgical procedures used for cervical radiculopathy: posterior keyhole foraminotomy versus anterior foraminotomy and discectomy versus anterior discectomy with fusion. J Spinal Disord. 2001;14(1):17–20. doi: 10.1097/00002517-200102000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Coric D, Adamson T. Minimally invasive cervical microendoscopic laminoforaminotomy. Neurosurg Focus. 2008;25(2):E2. doi: 10.3171/FOC/2008/25/8/E2. [DOI] [PubMed] [Google Scholar]
- 8.Epstein J, Lavine L, Aronson H, Epstein B. Cervical spondylotic radiculopathy. The syndrome of foraminal constriction treated by foraminotoy and the removal of osteophytes. Clin Orthop Relat Res. 1965;40:113–122. doi: 10.1097/00003086-196500400-00012. [DOI] [PubMed] [Google Scholar]
- 9.Epstein N. Minimally invasive/endoscopic vs. “open” posterior cervical laminoforaminotomy: do the risks outweigh the benefits? Surg Neurol. 2009;71(3):330–331. doi: 10.1016/j.surneu.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 10.Epstein N. A review of laminoforaminotomy for the management of lateral and foraminal cervical disc herniations or spurs. Surg Neurol. 2002;57(4):226–234. doi: 10.1016/S0090-3019(02)00644-4. [DOI] [PubMed] [Google Scholar]
- 11.Fager C. Posterolateral approach to ruptured median and paramedian cervical disk. Surg Neurol. 1983;20(6):443–452. doi: 10.1016/0090-3019(83)90025-3. [DOI] [PubMed] [Google Scholar]
- 12.Fessler R, Khoo L. Minimally invasive cervical microendoscopic foraminotomy: an initial clinical experience. Neurosurgery. 2002;51(5):S37–S45. [PubMed] [Google Scholar]
- 13.Heary R, Ryken T, Matz P, Anderson P, Groff M, Holly L, Kaiser M, Mummaneni P, Choudhri T, Vresilovic E, Resnick D (2009) Joint section on disorders of the spine and peripheral nerves of the american association of neurological surgeons and congress of neurological surgeons cervical laminoforaminotomy for the treatment of cervical degenerative radiculopathy. J Neurosurg Spine 11(2):198–202 [DOI] [PubMed]
- 14.Hilton D. Minimally invasive tubular access for posterior cervical foraminotomy with three-dimensional microscopic visualization and localization with anterior/posterior imaging. Spine J. 2007;7(2):154–158. doi: 10.1016/j.spinee.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 15.Hwang J, Bae H, Cho S, Cho S, Park H, Chang J. Morphometric study of the nerve roots around the lateral mass for posterior foraminotomy. J Korean Neurosurg Soc. 2010;47(5):358–364. doi: 10.3340/jkns.2010.47.5.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jagannathan J, Sherman J, Szabo T, Shaffrey C, Jane J. The posterior cervical foraminotomy in the treatment of cervical disc/osteophyte disease: a single-surgeon experience with a minimum of 5 years’ clinical and radiographic follow-up. J Neurosurg Spine. 2009;10(4):347–356. doi: 10.3171/2008.12.SPINE08576. [DOI] [PubMed] [Google Scholar]
- 17.Krupp W, Schattke H, Müke R. Clinical results of the foraminotomy as described by Frykholm for the treatment of lateral cervical disc herniation. Acta Neurochir (Wien) 1990;107(1–2):22–29. doi: 10.1007/BF01402608. [DOI] [PubMed] [Google Scholar]
- 18.Kumar G, Maurice-Williams R, Bradford R. Cervical foraminotomy: an effective treatment for cervical spondylotic radiculopathy. Br J Neurosurg. 1998;12(6):563–568. doi: 10.1080/02688699844448. [DOI] [PubMed] [Google Scholar]
- 19.Mixter W (1949) Rupture of the intervertebral disk; a short history of this evolution as a syndrome of importance to the surgeon. J Am Med Assoc 140(3):278–82 [DOI] [PubMed]
- 20.Raynor R, Pugh J, Shapiro I. Cervical facetectomy and its effect on spine strength. J Neurosurg. 1985;63(2):278–282. doi: 10.3171/jns.1985.63.2.0278. [DOI] [PubMed] [Google Scholar]
- 21.Rodrigues M, Hanel R, Prevedello D, Antoniuk A, Araújo J. Posterior approach for soft cervical disc herniation: a neglected technique? Surg Neurol. 2001;55(1):17–22. doi: 10.1016/S0090-3019(00)00349-9. [DOI] [PubMed] [Google Scholar]
- 22.Roh S, Kim D, Cardoso A, Fessler R (2000) Endoscopic foraminotomy using MED system in cadaveric specimens.Spine (Phila Pa 1976) 25(2):260–4 [DOI] [PubMed]
- 23.Scoville W. Cervical spondylosis treated by bilateral facetectomy and laminectomy. J Neurosurg. 1961;18:423–428. doi: 10.3171/jns.1961.18.4.0423. [DOI] [PubMed] [Google Scholar]
- 24.Tumialán L, Ponton R, Gluf W. Management of unilateral cervical radiculopathy in the military: the cost effectiveness of posterior cervical foraminotomy compared with anterior cervical discectomy and fusion. Neurosurg Focus. 2010;28(5):E17. doi: 10.3171/2010.1.FOCUS09305. [DOI] [PubMed] [Google Scholar]
- 25.Winder M, Thomas K. Minimally invasive versus open approach for cervical laminoforaminotomy. Can J Neurol Sci. 2011;38(2):262–267. doi: 10.1017/s0317167100011446. [DOI] [PubMed] [Google Scholar]
- 26.Zdeblick T, Zou D, Warden K, McCabe R, Kunz D, Vanderby R. Cervical stability after foraminotomy. A biomechanical in vitro analysis. J Bone Joint Surg Am. 1992;74(1):22–27. [PubMed] [Google Scholar]
- 27.Zeidman S, Ducker T. Posterior cervical laminoforaminotomy for radiculopathy: review of 172 cases. Neurosurgery. 1993;33(3):356–362. doi: 10.1227/00006123-199309000-00002. [DOI] [PubMed] [Google Scholar]