Abstract
Purpose
Supra-physiological rhBMP loads during spinal fusion may trigger local inflammation and post-operative radiculitis. MRI is an effective tool to detect nerve root compression in severe post-operative leg pain. The aim of this study was to determine if recombinant bone morphogenic protein 2 (rhBMP-2) is associated with immediate post-operative leg pain without evidence of root compression using MRI.
Method
All patients undergoing posterolateral and posterior interbody lumbar spinal fusions with rhBMP-2 between July 2007 and January 2009 at a single surgeon practice were retrospectively reviewed for incidence of severe immediate post-operative leg pain. Patients that presented with immediate post-operative leg pain were interviewed and Oswestry Disability Indices calculated.
Results
Sixty-four rhBMP-2 treated patients and 40 controls were included. Pre-operative demographics and diagnoses were similar and inter-body cages were used equally. Immediate post-operative leg pain incidence was 25 and 12.5% in the rhBMP-2 and non-rhBMP-2 groups, respectively. 17.2% of the patients treated with rhBMP-2 had immediate post-operative leg pain without evidence of nerve root compression on MRI versus 7.5% of the patients treated without rhBMP-2. At follow-up, leg pain incidence was 11.6 and 7.6% in rhBMP-2 and non-rhBMP-2 groups, respectively. There was no difference in Oswestry Disability Indices between groups (36.5 ± 31.2 vs. 23.0 ± 25.5).
Conclusion
RhBMP-2 associated radiculitis presenting as immediate post-operative leg pain without MRI evidence of neuronal compression occurs in 17% of the patients with rhBMP-2 assisted fusion. Patients should be pre-operatively counselled regarding immediate post-operative leg pain with rhBMP-2.
Level of evidence
III.
Keywords: Spinal fusion, rhBMP-2, Leg pain
Introduction
Recombinant bone morphogenic protein 2 (rhBMP-2) is an osteoinductive agent used in posterolateral spinal fusion surgery with superior fusion rates compared to iliac crest autograft [4]. “Off-label” use of rhBMP-2 for posterolateral and posterior interbody fusion is commonplace. Supra-physiological rhBMP loads implanted during spinal fusion may trigger local inflammation and post-operative radiculitis [2]. Severe immediate post-operative leg pain without evidence of nerve root compression on magnetic resonance imaging (MRI) is a clinical dilemma for the spinal surgeon.
In this series, we compare patients treated with and without rhBMP-2-assisted posterolateral lumbar fusion. The aim of this study was to determine if rhBMP-2 is associated with immediate post-operative leg pain without evidence of root compression using MRI.
Methods
This was a single surgeon, retrospective case control study. All patients undergoing posterolateral and posterior interbody lumbar spinal fusions with rhBMP-2 between July 2007 and January 2009 were reviewed. A control group of patients that underwent posterolateral and posterior fusions without rhBMP-2 from September 2005 to June 2007 were included. Patient operative records and clinical notes were examined. Pre-operative demographic data, operative details and post-operative course were recorded.
Magnetic resonance imaging of the lumbar spine was performed pre-operatively in all cases. Patients with significant disc space height loss with or without anterolisthesis secondary to degenerative disc disease underwent inter-vertebral body fusion using cage filled with local bone graft with or without rhBMP-2. Patients with spinal or foraminal stenosis alone did not undergo inter-vertebral body fusion. Operative procedure was performed through a posterior midline incision with patient prone on four-poster table. Surgeon headlight and loupes provided surgical field clarity. The EXPEDIUM™ Spine System (DePuy Spine, Inc., MA, USA) was used in both groups to achieve spinal fusion. The SABER™ LUMBAR I/F CAGE® System (DePuy Spine, Inc., MA, USA) was used when indicated with a posterior lumbar interbody fusion (PLIF) technique. Following dissection to requisite spinous processes, paraspinal muscle was stripped laterally using blunt dissection and careful diathermy to expose facet joint. Strict haemostasis was observed throughout. Laminotomy was performed using Kerrison Rongeurs. Nerve root was protected during laminotomy with Macdonald nerve root retractor. Retraction was avoided except briefly to allow inter-vertebral body cage implantation when indicated. In the rhBMP-2 group, 12 mg reconstituted dibotermin alpha and collagen matrix (InductOs, Wyeth, Dublin, Ireland) was prepared at a concentration of 1.5 mg/ml immediately prior to use. RhBMP-2/collagen matrix enveloped local bone graft was placed posterolaterally in all rhBMP-2 cases. Total rhBMP-2 load was uniform between patients including volume distributed posterolaterally and within cages. Care was taken to maintain rhBMP-2 within confines of cages at implantation. Local bone graft was not used concomitantly with rhBMP-2 within interbody cages. Hydroxyapatite-coated bovine collagen sponge/bone marrow aspirate (Healos®, DePuy Spine) was used on occasion in the non-rhBMP-2 cohort during a short trial period of three cases. Oxiplex®/SP Gel (DePuy Spine) adhesion barrier was used following laminotomy, laminectomy and cage insertion. Skin closure was with sub-cuticular absorbable suture. Deep closed suction drain was used in all cases.
Patients that presented with severe immediate post-operative leg pain underwent urgent lumbo-sacral MRI. Subjectively, severe leg pain within 72 h of the index surgery was considered to be “immediate”. Leg pain was considered severe when symptoms were disproportionately high or new. Surgeon discretion was used in such evaluation. Low back pain was not an indication for urgent investigation. Any further therapeutic procedures were conducted on the same admission. Symptom free out-patients were discharged from routine follow-up 3 months post-operatively. Further appointments were made available upon request as standard practice.
Patients that had presented with immediate post-operative leg pain were prospectively selected for interview. The Oswestry Disability Index was used as a measure of leg pain disability at the time of interview in this subset of patients. Back pain was not included as a variable.
Procedures following or pertaining to lumbar trauma were excluded from this study. Data were analysed using Fischer’s exact test and Student’s t test.
Results
Patients
One hundred and four patients that underwent spinal fusion were included for final analysis (Table 1). Sixty-four patients underwent spinal surgery with rhBMP-2 and 40 patients were treated without rhBMP-2. The median age in the rhBMP-2 group was 54.8 (range 19.2–90.1) and the median age in the non-rhBMP-2 group was 56.5 (range 22.7–83.3). There were 31 male patients in the rhBMP-2 group and 12 male patients in the non-rhBMP-2 group. The median follow-up for the rhBMP-2 treated and non-treated groups was 4.1 months (range 1.1–19) and 6.8 months (range 1.6–40), respectively. Five patients lost to follow-up were excluded from follow-up analysis, four in the rhBMP-2 treated group and one in the non-rhBMP-2 treated group.
Table 1.
Patient pre-operative demographics
| Variable | RhBMP-2 cohort (n = 64) | Control group (n = 40) | P value* | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Agea | 54.8 (19.2–90.1) | 56.5 (22.7–83.3) | 0.693 | ||
| Sex | |||||
| Male | 31 | 48.4 | 12 | 30.0 | 0.070 |
| Female | 33 | 51.6 | 28 | 70.0 | |
| Diagnosisb | |||||
| Degenerative spondylolisthesis | 32 | 50.0 | 22 | 55.0 | 0.689 |
| Degenerative disc disease | 32 | 50.0 | 16 | 40.0 | 0.419 |
| Central stenosis | 27 | 42.2 | 14 | 35.0 | 0.539 |
| Degenerative spondylosis | 5 | 7.8 | 2 | 5.0 | 0.704 |
| Isthmic spondylolisthesis | 2 | 3.1 | 3 | 7.5 | 0.370 |
| Other | 5 | 7.8 | 0 | 0.0 | 0.154 |
| Previous lumbar surgery | 29 | 45.3 | 7 | 17.5 | 0.005 |
| Previous fusion surgery | 15 | 23.4 | 0 | 0.0 | <0.005 |
| Previous spinal rhBMP-2 | 1 | 1.6 | 0 | 0.0 | 1.000 |
Pre-operative age, sex and diagnosis were similar in both cohorts. Patients treated with rhBMP-2 tended to have previous spinal fusion
* P values for categorical variables were generated using Fischer’s exact test
aAge: median (range). Variance in age was determined using two-tailed Student’s t test
bPrimary and secondary pre-operative diagnoses: Patients with one or more diagnosis are included
Previous surgery
Twenty-three percent (n = 15) of the patients in the rhBMP-2 group underwent previous fusion surgery (Table 2). None of these patients had previous interbody cages implanted. No patients in the non-rhBMP-2 group had previous fusion surgery. Nerve root decompression without fusion was previously performed in two of the non-rhBMP-2 group and nine of the rhBMP-2 group. Five patients in each group had previous discectomy surgery.
Table 2.
Surgical procedure
| Variable | RhBMP-2 cohort (n = 64) | Control group (n = 40) | P value* | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Single level surgery | 31 | 48.4 | 23 | 57.5 | 0.423 |
| L2/L3 | 1 | 1.6 | 0 | 0.0 | 1.000 |
| L3/L4 | 1 | 1.6 | 1 | 2.5 | 1.000 |
| L4/L5 | 13 | 20.3 | 9 | 22.5 | 0.809 |
| L5/S1 | 16 | 25.0 | 11 | 27.5 | 0.821 |
| Multi-level surgery | 33 | 51.6 | 18 | 45.0 | 0.550 |
| L2–L5 | 3 | 4.7 | 0 | 0.0 | 0.283 |
| L3–L5 | 3 | 4.7 | 3 | 7.5 | 0.673 |
| L3–S1 | 0 | 0.0 | 1 | 2.5 | 0.394 |
| L3–pelvis | 1 | 1.6 | 0 | 0.0 | 1.000 |
| L4–S1 | 23 | 35.9 | 14 | 35.0 | 1.000 |
| T–L4/5 | 3 | 4.7 | 0 | 0.0 | 0.283 |
| Inter-body cage | 19 | 29.7 | 10 | 25.0 | 0.659 |
| rhBMP-2 | |||||
| Cage rhBMP-2 | 19 | 28.1 | 0 | 0.0 | >1 |
| Posterolateral rhBMP-2 | 64 | 100.0 | 0 | 0.0 | >1 |
| Cage Healos® | 0 | 0.0 | 3 | 7.5 | 0.054 |
The lumbo-sacral operative level was similar in both treatment groups. The majority of surgery was performed at L4/L5 and or L5/S1 in both groups
* P values for categorical variables were generated using Fischer’s exact test
Indications for surgery
Indications for surgery were degenerative disc disease, spondylosis and or spondylolisthesis. Degenerative spondylolisthesis with or without degenerative disc disease was the most common indication for surgery in the rhBMP-2 treated group (n = 32) and in the non-rhBMP-2 treated group (n = 22) (Table 1). There was a prevalence of central canal stenosis in 27 patients in the rhBMP-2 treated group and 14 in the non-rhBMP-2 treated group. All patients had pre-operative leg pain.
Surgical procedure
Single level surgery was performed in forty-eight percent (n = 31) of the patients in the rhBMP-2 treated group and fifty-seven percent (n = 23) of the patients in the non-rhBMP-2 treated group (Table 2). The majority of single or multi-level surgery was performed at vertebral levels L4/L5 and or L5/S1 in both study groups. Inter-body devices were implanted in thirty percent (n = 19) of rhBMP-2 treated patients and twenty-five percent (n = 10) of the non-rhBMP-2 treated patients. All interbody devices were filled with rhBMP-2 in the rhBMP-2 group. RhBMP-2 mixed with local bone graft was implanted posterolaterally in all rhBMP-2 treated patients. Three cages in the non-rhBMP-2 group were filled with hydroxyapatite-coated bovine collagen sponge/bone marrow aspirate (Healos®, DePuy Spine).
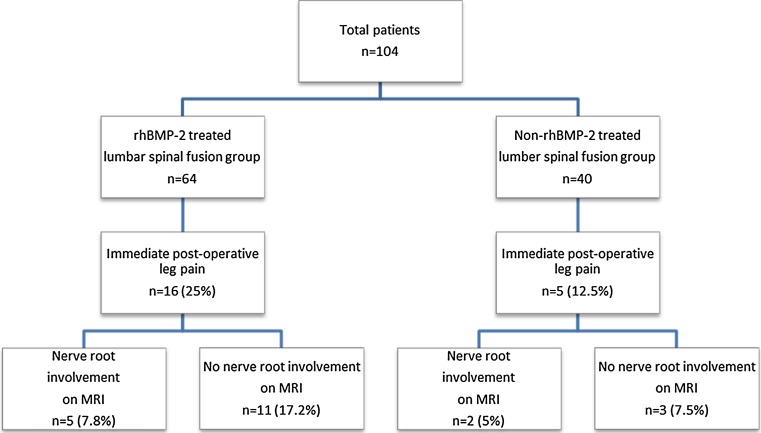
Immediate post-operative leg pain
Twenty-five percent (n = 16) of the patients treated with rhBMP-2 and twelve percent (n = 5) of the patients treated without rhBMP-2 complained of severe leg pain within 72 h of index surgery (p = 0.140) (Fig. 1; Table 3). The relative risk and odds ratio for developing severe immediate leg pain following rhBMP-2 assisted fusion were 2 and 2.33, respectively. No mechanical cause was identified on MRI in sixty-nine percent (n = 11/16) of the patients with leg pain in the rhBMP-2 treated group and sixty percent (n = 3/5) of the non-rhBMP-2 treated group (p = 1.00). Overall, 17.2% (n = 11/64) of the patients treated with rhBMP-2 had immediate post-operative leg pain without evidence of nerve root compression on MRI. This compares with 7.5% (n = 3/40) of the patients treated without rhBMP-2 that had immediate post-operative leg pain without MRI evidence of nerve root compression (p = 0.238). Twenty-one percent of the patients (n = 4/19) with inter-vertebral body cage rhBMP-2 had immediate post-operative leg pain. Ten percent of the patients (n = 1/10) fused with inter-vertebral body cage in the non-rhBMP-2 group had immediate post-operative leg pain (p = 0.632).
Fig. 1.
Immediate post-operative leg pain
Table 3.
Subsequent intervention in patients with post-operative leg pain
| Variable | rhBMP-2 cohort (n = 64) | Control group (n = 40) | P value* | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Post-op leg pain | 16 | 25.0 | 5 | 12.5 | 0.140 |
| Cause for leg pain on MRI | 5 | 7.8 | 2 | 5.0 | 0.704 |
| No cause for leg pain on MRI | 11 | 17.1 | 3 | 7.5 | 0.238 |
| Retreatment | |||||
| Overall | 5 | 7.8 | 4 | 10 | 0.730 |
| Revision surgery | 1 | 6.3 | 0 | 0 | 1.000 |
| Nerve root block | 3 | 18.8 | 2 | 40.0 | 1.000 |
| Facet/SI joint anaesthesia | 1 | 6.3 | 3 | 60.0 | 0.028 |
Twenty-five percent (n = 16) of the patients treated with rhBMP-2 and twelve percent (n = 5) of the patients treated without rhBMP-2 complained of severe post-operative leg pain. Overall, 17.2% (n = 11/64) of the patients treated with rhBMP-2 had immediate post-operative leg pain without evidence of nerve root compression on MRI. This compares with 7.5% (n = 3/40) of the patients treated without rhBMP-2 that had immediate post-operative leg pain without MRI evidence of nerve root compression
* P values for categorical variables were generated using Fischer’s exact test
Immediate post-operative leg pain in patients treated with rhBMP-2 (n = 16) and without rhBMP-2 (n = 5) was investigated with MRI to exclude nerve root compression. Patients treated with and without rhBMP-2 had no nerve root involvement in sixty-nine percent and sixty percent of the cases, respectively. Overall, 17.2% (n = 11/64) of the patients treated with rhBMP-2 had immediate post-operative leg pain without evidence of nerve root compression on MRI. This compares with 7.5% (n = 3/40) of the patients treated without rhBMP-2 that had immediate post-operative leg pain without MRI evidence of nerve root compression.
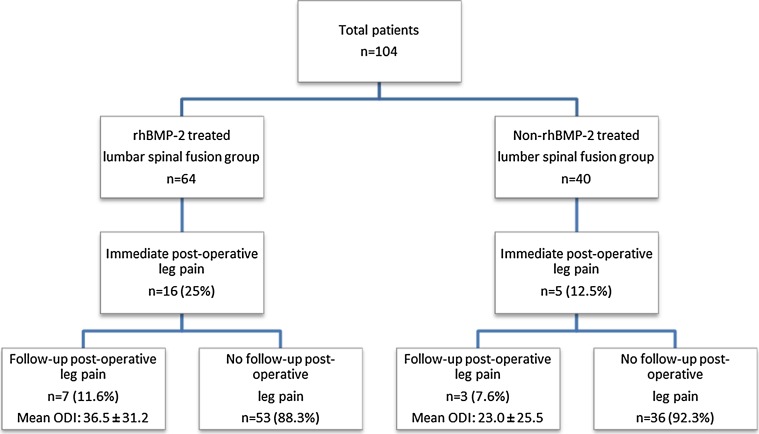
Follow-up post-operative leg pain
The overall incidence of leg pain at follow-up was 11.6% (n = 7/60) in the rhBMP-2 treated group and 7.6% (n = 3/39) in the non-rhBMP-2 treated group (p = 0.735) (Fig. 2). The incidence of follow-up leg pain in patients that had immediate post-operative leg pain was 43.7% (n = 7/16) and 75% (n = 3/4) in the rhBMP-2 and non-rhBMP-2 treated groups, respectively (p = 0.58). The mean follow-up Oswestry Disability Indices in patients with severe immediate post-operative leg pain was 36.5 ± 31.2 and 23.0 ± 25.5 for the rhBMP-2 and non-rhBMP-2 treated groups, respectively (p = 0.47).
Fig. 2.
Early follow-up post-operative leg pain and Oswestry Disability Index scores in patients treated with or without rhBMP-2
Median follow-up in patients treated with rhBMP-2 was 4.1 months (1.1–19). Median follow-up in the control group was 6.8 (1.6–40).
Subsequent intervention
Five patients (7.8%) in the rhBMP-2 treated group required intervention following fusion surgery. Four patients not treated with rhBMP-2 required intervention following surgery (10%) (p = 0.730) (Table 3). Selective nerve root block during operative admission was required in three patients in the rhBMP-2 treated group and two patients in the non-rhBMP-2 treated group. One patient in the rhBMP-2 treated group and three patients in the non-rhBMP-2 treated group required either facet or sacro-iliac joint injection as an out-patient. One patient in the non-rhBMP-2 group underwent both nerve root block and sacro-iliac joint injection. One patient in the rhBMP-2 treated group required later admission and revision surgery for pseudoarthrosis.
Complications
There were no intra-operative dural tears with subsequent cerebrospinal fluid leak. None of the patients required immediate inpatient operative intervention during operative admission. There were no post-operative haematomas or wound infections. One patient sustained a myocardial infarction during operative admission. There were no mortalities during operative admission.
Discussion
Recombinant BMPs are commonly used in spinal fusion [1, 5]. Concern has arisen regarding unpredictable post-operative peri-BMP inflammation presenting as radiculopathy [2]. BMPs are members of the transforming growth factor-beta (TGF-β) superfamily of cytokines. BMP-2 is pro-inflammatory and has been implicated in pathological processes such as atherosclerosis [6, 7]. Many clinical reports exist associating BMP use with inappropriate inflammation or ossification [8–12]. This study presents sufficient circumstantial evidence to implicate rhBMP-2 in post-operative radiculopathy. Overall, the relative risk of patients fused with rhBMP-2 to present with severe immediate post-operative leg pain in this series was double compared to patients treated without rhBMP-2. The odds ratio was 2.33 thus severe immediate post-operative leg pain was strongly associated with rhBMP-2 use.
Magnetic resonance imaging is an effective tool to detect nerve root compression in severe post-operative leg pain [3]. Appropriately, all patients that presented with severe leg pain underwent MRI. In the series, 17.2% of the patients treated with rhBMP-2 had immediate post-operative leg pain without evidence of root compression on MRI. This compared with 7.5% of the patients fused without rhBMP-2. Importantly, at follow-up the incidence of leg pain had reduced in both groups, most noticeably in the rhBMP-2 treated group. There was 14% relative reduction in leg pain in the rhBMP-2 treated group versus 5% reduction in the control group at follow-up. The median follow-up in the rhBMP-2 group was 4.1 months. Severe leg pain to recover in such a short period without evidence of neuronal compression supports the hypothesis of transient radiculitis with rhBMP-2 use. It has been shown that leg pain improvement occurs in the first 2 months post-operatively, but remains static thereafter [13]. Leg pain at 4-month follow-up in this report is appropriate.
RhBMP-2 was implanted posterolaterally in the majority of the patients in the treatment group, perhaps protecting nerve root from direct rhBMP-2 contact. Nerve root involvement should therefore be lower in those patients treated without inter-body cage devices. The evidence did not support this. Similar to overall results, patients treated with rhBMP-2 filled inter-body cages were twice as likely to develop severe post-operative leg pain as patients treated without rhBMP-2 filled inter-body cages (21 vs. 10%).
Higher incidence of severe immediate post-operative leg pain in the rhBMP-2 treated group was not associated with worse outcome. Leg pain at final follow-up was not statistically significant between both groups. Similarly, the mean Oswestry disability indices for leg pain were not statistically significant between groups. This further supports the theory of a transient rhBMP-2 induced radiculitis.
Posterior lumbar interbody fusion technique was used when indicated. Nerve root was only retracted to facilitate inter-vertebral body cage placement. The incidence of immediate leg pain was 21, 26 and 25% with inter-vertebral body cage, without inter-vertebral body cage and overall in the rhBMP-2 treated group, respectively. Similarly, the incidence of immediate leg pain was 10, 13 and 12% with inter-vertebral body cage, without inter-vertebral body cage and overall in the non-treatment group, respectively. Thus, rate of severe leg pain is not attributable to use of inter-vertebral body cages and procedure required for implantation.
As a retrospective analysis, this study is inherently weak yet strengths also exist; primarily, as a single surgeon series. Furthermore, the study cohorts are comparatively similar with no differences in demographic, indication for surgery or surgical procedure. Incidence of previous lumbar fusion was significantly higher in the rhBMP-2 group. In these cases, failed fusion was augmented using an osteoinductive agent, rhBMP-2. This may more readily reflect current off-label use where surgeons seek improved union following failure. Careful surgical technique is clearly demonstrated with an absence of dural tears in 104 decompressions, 51 of which were multi-level. Careful technique excludes excessive root retraction intra-operatively as a cause of severe post-operative leg pain. Patients that presented with severe post-operative leg pain were prospectively appraised using a validated scoring system. Such patient scores are not routinely documented pre-operatively and surgeon discretion is required when determining suitability for surgery or evaluating disproportionate post-operative leg pain at our institutions. Succinct patient interview differentiated between back pain and leg pain both pre- and post-operatively.
In conclusion, the results of this series suggest that rhBMP-2 induced radiculitis presenting as immediate post-operative leg pain occurs in a quarter of the patients. It is a transient phenomenon and in this series was not associated with adverse outcome. MRI remains an expensive outlay to exclude root compression. Patients should be pre-operatively counselled regarding immediate post-operative leg pain when “off label” use of rhBMP-2 is proposed.
Acknowledgments
Conflict of interest
The authors report no conflict of interest in the production or publication of this manuscript.
References
- 1.Burkus JK, Gornet MF, Schuler TC, Kleeman TJ, Zdeblick TA. Six-year outcomes of anterior lumbar interbody arthrodesis with use of interbody fusion cages and recombinant human bone morphogenetic protein-2. J Bone Jt Surg Am. 2009;91(5):1181–1189. doi: 10.2106/JBJS.G.01485. [DOI] [PubMed] [Google Scholar]
- 2.Shimer AL, Oner FC, Vaccaro AR. Spinal reconstruction and bone morphogenetic proteins: open questions. Injury. 2009;40(Suppl 3):S32–S38. doi: 10.1016/S0020-1383(09)70009-9. [DOI] [PubMed] [Google Scholar]
- 3.Crocker M, Jones TL, Rich P, Bell BA, Papadopoulos MC. The clinical value of early postoperative MRI after lumbar spine surgery. Br J Neurosurg. 2010;24(1):46–50. doi: 10.3109/02688690903374067. [DOI] [PubMed] [Google Scholar]
- 4.Papakostidis C, Kontakis G, Bhandari M, Giannoudis PV. Efficacy of autologous iliac crest bone graft and bone morphogenetic proteins for posterolateral fusion of lumbar spine: a meta-analysis of the results. Spine (Phila Pa 1976) 2008;33(19):E680–E692. doi: 10.1097/BRS.0b013e3181844eca. [DOI] [PubMed] [Google Scholar]
- 5.Haid RW, Jr, Branch CL, Jr, Alexander JT, Burkus JK. Posterior lumbar interbody fusion using recombinant human bone morphogenetic protein type 2 with cylindrical interbody cages. Spine J. 2004;4(5):527–538. doi: 10.1016/j.spinee.2004.03.025. [DOI] [PubMed] [Google Scholar]
- 6.Csiszar A, Smith KE, Koller A, Kaley G, Edwards JG, Ungvari Z. Regulation of bone morphogenetic protein-2 expression in endothelial cells: role of nuclear factor-kappa B activation by tumor necrosis factor-alpha, H2O2, and high intravascular pressure. Circulation. 2005;111(18):2364–2372. doi: 10.1161/01.CIR.0000164201.40634.1D. [DOI] [PubMed] [Google Scholar]
- 7.Csiszar A, Ahmad M, Smith KE, Labinskyy N, Gao Q, Kaley G, et al. Bone morphogenetic protein-2 induces proinflammatory endothelial phenotype. Am J Pathol. 2006;168(2):629–638. doi: 10.2353/ajpath.2006.050284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MacDonald KM, Swanstrom MM, McCarthy JJ, Nemeth BA, Guliani TA, Noonan KJ. Exaggerated inflammatory response after use of recombinant bone morphogenetic protein in recurrent unicameral bone cysts. J Pediatr Orthop. 2010;30(2):199–205. doi: 10.1097/BPO.0b013e3181cec35b. [DOI] [PubMed] [Google Scholar]
- 9.Shahlaie K, Kim KD. Occipitocervical fusion using recombinant human bone morphogenetic protein-2: adverse effects due to tissue swelling and seroma. Spine (Phila Pa 1976) 2008;33(21):2361–2366. doi: 10.1097/BRS.0b013e318183971d. [DOI] [PubMed] [Google Scholar]
- 10.Smucker JD, Rhee JM, Singh K, Yoon ST, Heller JG. Increased swelling complications associated with off-label usage of rhBMP-2 in the anterior cervical spine. Spine. 2006;31(24):2813–2819. doi: 10.1097/01.brs.0000245863.52371.c2. [DOI] [PubMed] [Google Scholar]
- 11.Vaidya R, Carp J, Sethi A, Bartol S, Craig J, Les CM. Complications of anterior cervical discectomy and fusion using recombinant human bone morphogenetic protein-2. Eur Spine J. 2007;16(8):1257–1265. doi: 10.1007/s00586-007-0351-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wong DA, Kumar A, Jatana S, Ghiselli G, Wong K. Neurologic impairment from ectopic bone in the lumbar canal: a potential complication of off-label PLIF/TLIF use of bone morphogenetic protein-2 (BMP-2) Spine J. 2008;8(6):1011–1018. doi: 10.1016/j.spinee.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 13.Mannion AF, Denzler R, Dvorak J, Grob D. Five year outcome of surgical decompression of the lumbar spine without fusion. Eur Spine J. 2010;19(11):1883–1891. doi: 10.1007/s00586-010-1535-2. [DOI] [PMC free article] [PubMed] [Google Scholar]