Abstract
Purpose
To document the neurological outcome, spinal alignment and segmental range of movement after oblique cervical corpectomy (OCC) for cervical compressive myelopathy.
Methods
This retrospective study included 109 patients—93 with cervical spondylotic myelopathy and 16 with ossified posterior longitudinal ligament in whom spinal curvature and range of segmental movements were assessed on neutral and dynamic cervical radiographs. Neurological function was measured by Nurick’s grade and modified Japanese Orthopedic Association (JOA) scores. Eighty-eight patients (81%) underwent either a single- or two-level corpectomy; the remaining (19%) undergoing three- or four-level corpectomies. The average duration of follow-up was 30.52 months.
Results
The Nurick’s grade and the JOA scores showed statistically significant improvements after surgery (p < 0.001). The mean postoperative segmental angle in the neutral position straightened by 4.7 ± 6.5°. The residual segmental range of movement for a single-level corpectomy was 16.7° (59.7% of the preoperative value), for two-level corpectomy it was 20.0° (67.2%) and for three-level corpectomies it was 22.9° (74.3%). 63% of patients with lordotic spines continued to have lordosis postoperatively while only one became kyphotic without clinical worsening. Four patients with preoperative kyphotic spines showed no change in spine curvature. None developed spinal instability.
Conclusions
The OCC preserves segmental motion in the short-term, however, the tendency towards straightening of the spine, albeit without clinical worsening, warrants serial follow-up imaging to determine whether this motion preservation is long lasting.
Keywords: Cervical spondylotic myelopathy, Ossified posterior longitudinal ligament, Oblique corpectomy, Motion preservation
Introduction
Cervical spondylosis and ossified posterior longitudinal ligament (OPLL) are common causes of myelopathy that often require surgical decompression either through multilevel anterior cervical discectomies/corpectomies or laminectomy/laminoplasty when they result in progressive neurological deficits [1–3]. The oblique cervical corpectomy (OCC) has slowly emerged as an established method of decompressing the spine in patients with cervical spondylotic myelopathy (CSM) [4–10]. The reason it is attractive that it allows for a long segment of decompression (up to five levels) without the need for a bone graft or instrumentation as its proponents claim that stability and sagittal alignment are maintained. Central corpectomy, on the other hand, is destabilizing; and grafting with or without instrumentation is mandatory. It offers the best results for one-level corpectomies while the incidence of non-union, instrumentation failure and graft extrusion increases from 6 to 9% in two level corpectomies to more than 50% in three-level corpectomies [11, 12]. Thus, in patients undergoing >3 level central corpectomies, additional posterior instrumentation is recommended for a more stable construct to enhance fusion rates and reduce instrumentation failure [8, 13–15].
There is limited literature available on the results of OCC and although good clinical outcomes have been reported [4, 7–9], there is insufficient data available with regard to the maintenance of sagittal alignment and the degree of preservation of movement on flexion and extension of the neck. The purpose of this retrospective study was to document the neurological outcome, spinal alignment and range of movement after OCC.
Methods
Patients
Between July 2001 and March 2009, we performed 157 oblique corpectomy procedures. All patients underwent a detailed neurological examination, assessment of functional status using the Nurick’s grading system [16] and a modified Japanese Orthopedic Association (JOA) system [17]. Magnetic resonance imaging (MRI) was available in all patients. Patients with CSM and OPLL were selected for an OCC if there was no spinal instability on the dynamic plain radiographs and when the number of levels of cord compression was <4 irrespective of spinal curvature and regardless of whether the discs were collapsed or not. Preoperative clinical and radiological data were entered prospectively into a proforma and subsequently into an access database. For this study, the data on 109 patients with at least 6 months follow-up were retrospectively analyzed. The remaining 48 patients were excluded either because they did not have follow-up imaging or if the imaging was of poor quality.
Operative procedure
Only a brief description of the technique of the OCC will be made here since it has been described in detail before [6]. Through a longitudinal skin incision along the anterior border of the right sternocleidomastoid muscle, the carotid sheath is retracted medially to expose the transverse processes of the cervical vertebrae. The sympathetic chain lying on the longus colli is generally retracted medially but on occasion when it is situated far laterally it is retracted laterally. The vertebral artery (VA) lies unprotected between two consecutive vertebrae but is protected above C6 in the foramen transversarium by the costotransverse bar of the transverse process. The microscope is brought in and the diamond drill is used to thin down the costotransverse bar to the periosteum over the VA. An 8 mm cutting burr is then used to make a vertical trough down to the OPLL on the lateral part of the vertebral body leaving about 3 mm of cortical bone to protect the VA laterally. Drilling then continues obliquely across to the contralateral side of the canal along the posterior cortical margin minimizing vertebral body removal. Patients are mobilized on the first day and were initially advised to wear a cervical collar for 3 months, but we discontinued advising a collar after 2005.
Outcome assessment
Patients were advised to send us lateral cervical spine radiographs in neutral, flexion and extension views in the standing position. The patient was asked to flex and extend his neck to the maximum extent possible without experiencing discomfort. He was also asked to send at least one MRI scan postoperatively by post along with a questionnaire for the Nurick’s grade and JOA scores. Images done elsewhere were scanned into and stored on a General Electric (GE) Centricity 1.0 Picture Archival and Retrieval Computer System (PACS) server and measurements performed on GE Centricity 1.0 PACS workstations. Whole spine curvature was defined in relation to a line joining the postero-inferior edge of C2 to the postero-inferior edge of C7. When the inferior edge of C7 was not visible, we used the upper edge of C7 in eight patients. The spine was called lordotic when the posterior surfaces of the C3–C6 bodies were anterior to the line, straight when at least one vertebral body touched the line and kyphotic when even one body lay behind the line. The segmental angle was assessed using the Cobb’s method on the neutral lateral view at the level operated, that is, the angle between a line on the superior end plate of the vertebral body above and a line on the inferior border of the body below the levels operated. Thus for C5 corpectomies, the first line was on the superior end plate of C4 and the 2nd line was on the inferior end plate of C6. However, for C6 corpectomies the superior end plate of C7 was used in the measurements as the shoulders on the plain radiographs, particularly on flexion, often obscured the inferior end plate of C7. The Cobb’s angle over the segments operated was also measured in flexion and extension to give a range of movement. Two observers (AGC and MJ) independently assessed the angles and spine curvatures on their computer consoles after doing a few trial measurements together to arrive at a protocol.
Statistical analysis
Paired t test and McNemar’s test were employed to assess the significance of change before and after surgery for continuous and nominal data, respectively. Student t test was used to compare the statistical significant of the association for continuous data. Multiple linear regression was used to adjust for the effects of age, gender and number of levels operated.
Results
The majority of the 109 patients were male (n = 97; 89%) with a mean age ±SD of 50.39 ± 9.86 years and an average duration of myelopathic symptoms and problems with gait 17.21 ± 22.06 and 13.44 ± 18.33 months, respectively. The clinical and pre-operative radiological findings are depicted in Tables 1 and 2. An intraoperative dural tear with a CSF leak occurred in 4 patients (3.7%) that was successfully managed with a lumbar subarachnoid catheter and bed rest. Temporary Horner’s syndrome was seen in 35 (32.1%) that persisted in 9 (8.2%). Four (3.7%) patients required narcotic analgesia and 10 (9.2%) were catheterized, postoperatively. The average duration of follow-up was 30.52 ± 19.71 months.
Table 1.
Clinical and radiological findings (n = 109)
| Clinical feature | Number (%) |
|---|---|
| Radicular pain | 15 (14) |
| Paresthesiae | 94 (86) |
| Bladder dysfunction | 36 (33) |
| Romberg’s sign positive | 40 (37) |
| Radiology | |
| T2 hyperintensity | 79 (73) |
| Ossified anterior longitudinal ligament | 13 (12) |
| Ossified posterior longitudinal ligament | 16 (15) |
Table 2.
Corpectomy levels (n = 109)
| Cervical level | Number (%) |
|---|---|
| C3 | 3 (2.8) |
| C4 | 52 (48) |
| C5 | 78 (72) |
| C6 | 63 (58) |
| C7 | 2 (1.8) |
| Number of segments | |
| One | 41 (38) |
| Two | 47 (43) |
| Three | 20 (18) |
| Four | 1 (0.9) |
Clinical outcome and range of cervical motion
Table 3 documents the Nurick’s grades, JOA scores and radiological measurements in neutral, flexion and extension positions. All postoperative clinical scores showed statistically significant changes after surgery with improvement in the Nurick’s grade and the JOA score. At follow-up 45 patients improved by 1 Nurick grade, 22 by 2 grades, 12 by 3 grades and 1 patient improved by 4 grades. This corresponded to an overall improvement of 72.5% on the Nurick’s grade. The amount of flexion decreased by a mean of 2.5° (SD 6.4) and extension by 7.1° (SD 7.5). The residual range of movement across the operated segments for a single-level corpectomy was 16.7° (59.7% of the preoperative value), for two-level corpectomies it was 20.0° (67.2%) and for three-level corpectomies it was 22.9° (74.3%).
Table 3.
Statistical significance of differences between preoperative and postoperative clinical scores and radiological angles
| Assessment | Preoperative mean (SD) | Last follow-up mean (SD) | No. of patients | Mean difference (SD) | Statistics using paired t test | ||
|---|---|---|---|---|---|---|---|
| t value | df | p value | |||||
| Nurick’s grade | 3.55 (0.73) | 2.46 (0.73) | 101 | −1.10 (0.90) | 12.27 | 100 | <0.001 |
| JOA Score | 11.43 (2.10) | 14.15 (1.74) | 95 | 2.72 (2.20) | −12.05 | 94 | <0.001 |
| Segmental angle in neutral position | 10.76 (9.28) | 6.02 (8.32) | 92 | −4.74 (6.51) | 6.99 | 91 | <0.001 |
| Segmental angle in flexion | −12.69 (7.94) | −10.20 (8.03) | 52 | −2.49 (6.42) | −2.80 | 51 | 0.007 |
| Segmental angle in extension | 16.27 (8.26) | 9.18 (7.69) | 39 | −7.09 (7.45) | 5.95 | 38 | 0.007 |
| Range of neck movement | 29.52 (11.11) | 19.75 (9.51) | 38 | −9.77 (8.68) | 6.94 | 37 | <0.001 |
Segmental angle and whole spine curvature
The mean postoperative segmental angle in the neutral position of the entire group of patients showed a straightening of 4.7° (SD 6.5). The change in segmental angle after surgery was not significantly greater in the three- and four-level corpectomies when compared with the one- and two-level corpectomies (Table 4). In the assessment of whole spine curvature, 67 (71.3%) patients had lordotic spines, 23 (24.5%) were straight while 4 (4.3%) were kyphotic. A substantial majority of patients with lordotic spines continued to have lordosis post-operatively (63%) or developed a straight spine (35.8%) and only one became kyphotic with no worsening of clinical symptoms (Fig. 1; Table 5). The majority of patients (78%) with preoperative straight spines continued to have straight spines with 2 becoming kyphotic. The four patients with preoperative kyphotic spines showed no change in whole spine curvature, their mean segmental neutral angles changing by only 1° from −8.2° to −9.1° at follow-up (Fig. 2). The incidence of loss of lordosis did not correlate with the number of levels operated (Table 6) (p = 0.72); nor was there a correlation with age, gender, disease process (CSM/OPLL) or preoperative range of movement.
Table 4.
Correlation of postoperative change in segmental angle (n = 90) with the number of levels operated
| Number of levels operated | No. of patients | Mean segmental angle in neutral position | Difference per operated segment | ||
|---|---|---|---|---|---|
| Preoperative (SD) | Postoperative (SD) | Difference | |||
| 1 | 31 | 8.9 (7.3) | 4.2 (7.9) | 4.7 | 4.7 |
| 2 | 41 | 11.0 (8.5) | 6.8 (7.7) | 4.2 | 2.1 |
| 3 | 17 | 15.7 (10.8) | 9.2 (9.0) | 6.5 | 2.2 |
| 4 | 1 | 18.5 | 7.2 | 11.3 | 3.8 |
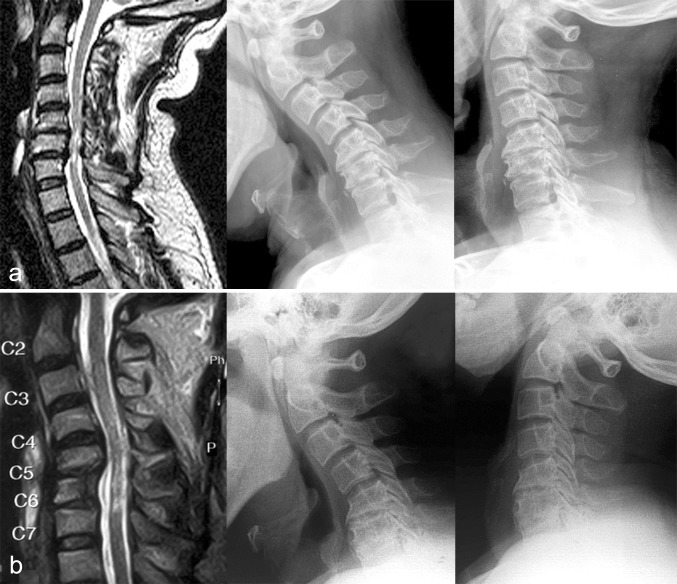
Fig. 1.
Preoperative (a) and postoperative (b) MR sagittal images with plain lateral radiographs in neutral, flexion and extension showing good decompression of the cord after a C5/C6 oblique corpectomy, preservation of lordosis and cervical movement on dynamic views
Table 5.
Pre and postoperative whole spine curvature (n = 94)
| Post operative lordosis (n = 45) | Post operative straight spines (n = 42) | Postoperative kyphosis (n = 7) | |
|---|---|---|---|
| Preoperative lordosis (n = 67; 71.3%) | 42 | 24 | 1 |
| Preoperative straight spine (n = 23; 24.5%) | 3 | 18 | 2 |
| Preoperative kyphosis | 0 | 0 | 4 |
Fig. 2.
Preoperative (a) and postoperative (b) MR sagittal images in a patient with preoperative kyphosis showing similar spine alignment on the plain radiographs after a C6 oblique corpectomy
Table 6.
Correlation of change in postoperative spine curvature with the number of levels operated in patients with preoperative lordotic spines (n = 67)
| Number of levels operated | Postoperative spine curvature | ||
|---|---|---|---|
| Lordotic | Straight | Kyphotic | |
| 1 | 18 (67%) | 8 (30%) | 1 (3%) |
| 2 | 16 (57%) | 12 (43% | 0 |
| 3 or 4 | 8 (67%) | 4 (33%) | 0 |
Table 7 documents the univariate and multivariate statistics for the functional outcomes recorded. The univariate analysis was performed using the Students t test and Pearson’s correlation. The Nurick’s grade at last follow-up was tested against the presence of OPLL, preoperative Nurick’s score, one or two level versus longer corpectomies, JOA score and patient’s assessment of improvement at last follow up. Similarly, the JOA score at last follow up was tested against the presence of OPLL, preoperative JOA score, one or two level versus longer corpectomies and to the Nurick’s grade and patients assessment of improvement at last follow-up. The Nurick’s grade at last follow-up correlated significantly with the preoperative Nurick’s grade, postoperative JOA at last follow-up and the patients’ assessment of improvement. Likewise, the JOA score at last followup was significantly correlated with the preoperative JOA score, the Nurick’s grade at last follow-up and the patients’ assessment of improvement. These associations remained statistically significant even after adjustment for age, gender and respective preoperative clinical score. The relationship between the presence of an OPLL and length of corpectomy was not significant on the multivariate statistical procedure. The following variables were not significantly associated with outcomes: the presence of radicular pain, paresthesiae, bladder symptoms, posterior column involvement, preoperative spine curvature, T1 hypointensity and T2 hyperintensity on MRI scan.
Table 7.
Outcome score and their relationship other variables
| Outcome variable | Independent variable | Univariate statistics | Multivariate statistics using multiple linear regressiona | |||
|---|---|---|---|---|---|---|
| Student’s t test/Pearson’s correlation | p value | β | t | p value | ||
| Nurick’s score at last follow-up | OPLL | t = −2.17; df = 22.08 | 0.037 | −0.160 | −1.632 | 0.106 |
| Nurick’s score preoperative | 0.236 | 0.018 | 0.242 | 2.438 | 0.017 | |
| Corpectomy involving only one or two levels | t = 2.218; df = 41.31 | 0.033 | 0.159 | 1.624 | 0.108 | |
| JOA score at last follow-up | −0.697 | <0.001 | −0.703 | −9.698 | <0.001 | |
| Improvement reported by patientb | −0.546 | <0.001 | −0.533 | −5.901 | <0.001 | |
| Duration of symptoms >12 months | 0.125 | 0.214 | 0.185 | 1.783 | 0.08 | |
| JOA score at last follow-up | OPLL | t = 1.096; df = 98 | 0.276 | 0.162 | 1.672 | 0.098 |
| JOA preoperative score | 0.358 | <0.001 | 0.344 | 3.480 | 0.001 | |
| Corpectomy involving only one or two levels | t = −1.91; df = 98 | 0.059 | −0.179 | −1.857 | 0.067 | |
| Nurick’s score at last follow up | −0.697 | <0.001 | −0.667 | −9.714 | <0.001 | |
| Improvement reported by patientb | 0.484 | <0.001 | 0.457 | 4.757 | <0.001 | |
| Duration of symptoms | −0.077 | 0.451 | −0.084 | −0.816 | 0.417 | |
aJOA; adjusted for age, gender and respective preoperative score
bImprovement reported by patient
The patients with OPLL were compared to those with CSM. Those with OPLL had significantly more postoperative problems in the form of CSF leak (p = 0.04), radicular deficit (p = 0.003), and lower range of movement (p = 0.006 and lower Nurick’s grade at last follow-up (0.04). The other variables did not differ significantly between the two groups.
Interobserver variability
There was substantial agreement (Interclass correlation coefficient = 0.86) in the measurement of segmental angles by the two observers.
Discussion
Although the OCC was described more than a decade ago, [6] it has not gained popularity probably due to the demanding technique related to mobilization of the sympathetic chain and concomitant Horner’s syndrome as well as the risk of vertebral artery injury. We found that in most cases the Horner’s syndrome is temporary and our incidence of permanent Horner’s syndrome was 8.2%, although patients were asymptomatic. Koc et al. [7] excise the longus colli muscle medial to the sympathetic chain thus avoiding mobilization of the latter structure and report a lower incidence of Horner’s syndrome. George et al. [6] reiterated that only those patients with CSM in whom imaging showed hard, collapsed discs and probably fused spines were offered the OCC. Other reports of the OCC do not mention whether they excluded patients with soft discs and non-fused spines [8, 9]. Our series included all patients with CSM regardless of spinal alignment or status of the discs whether hard or soft. Reports on the OCC have established that the technique yields excellent results determined by clinical outcome measures for myelopathy and radiological assessment of spinal alignment [4, 7–9]. However, data pertaining to the preservation of segmental motion is limited [4] and no detailed studies are available.
Clinical and radiological predictive factors
Men constituted the vast majority of our patients with only 3% being women. Apart from studies recruiting patients from Veterans Affairs clinics [18, 19] most reports from western literature indicates an equal gender distribution or a slight male preponderance [4, 13]. The mean age of 50 years in our cohort of patients is significantly lower than that seen in other series [4, 6, 20] and may have a bearing on the spondylotic changes in the discs—hard, collapsed discs in CSM, as described by George et al. [6] tend to occur in the older age group. Age did not correlate with outcome in our series, a finding that is supported by most studies [9, 20] except for a few suggesting that older patients have a worse outcome [21, 22] and one that suggests a better outcome in elderly patients [23]. In addition, number of levels operated on, duration of symptoms and MR intramedullary changes did not predict outcome. Duration of preoperative symptoms greater than 12 months has been associated with poorer outcomes [24, 25]. Although many authors are not impressed with intramedullary MR changes as a predictor of outcome, some data exists to suggest that T1 hypointensity along with T2 hyperintensity within the cord, particularly if multisegmental, are associated with poor outcomes and probably an irreversible pathology [26, 27]. Our findings indicate that patients with OPLL did not do as well as those with CSM with higher complication rates and lower range of movement after surgery. Anterior surgery for OPLL has been reported by others to provide better clinical outcomes as compared with posterior decompression particularly in those patients with preoperative kyphosis albeit with higher complication rates [28, 29].
Spinal alignment and straightening of cervical spine
We found that there is a mean loss of lordosis of 4.7° at the operated segments that probably contributes to the straightening of the whole spine in a third of our patients. However, there was no correlation between kyphotic change and age, number of levels operated, OPLL/CSM or the amount of spine motion present preoperatively. This loss of lordosis was not associated with any clinical deterioration. Of note is that fact that patients with kyphotic spines did not have a worsening of the kyphosis postoperatively. None of the studies on OCC measure segmental angles at the operated levels. Instead they measure whole spine curvature as the Cobb’s angle between C2 and C7 and define lordotic spines as angles >5º; straight as +5° to −5° and kyphotic as <−5° [6–8]. Koc et al. [7] in their series of 26 patients documented a reduction of 1° in the whole spine curvature from 13° preoperatively to 12° postoperatively but make no mention of the segmental angles. One of their patients (4%) developed a kyphosis from a straight spine. George et al. [6] in their first publication of 101 cases report three patients who developed instability after the OCC one of whom had a soft disc preoperatively. In all other patients, including 16 with preoperative kyphosis, the change in the whole spine curvature was less than 5°. Kiris et al. [8] report similar findings in 40 patients undergoing OCC for CSM, 23 with preoperative straight or kyphotic spines. No patient had more than a 5° change in whole spine curvature.
Segmental motion
Cagli et al. [10] studied the biomechanical effects of a two-level oblique corpectomy (C5 and C6) on cadaveric specimens. They compared OCC with the normal cervical spine and then with standard median corpectomy with a fibular graft alone and with a graft and plating. The range of motion after OCC increased uniformly in all directions by a mean of approximately 15% greater than normal. These in vitro studies cannot be simply transposed to in vivo practice as a result of limitations induced by the lack of muscle, healing, and adaptation. We lacked immediate postoperative radiographs to comment on whether our patients had increased spine mobility immediately after surgery, however our follow-up radiological findings clearly show that more than 50% of segmental motion is preserved. Thus, the residual range of movement across the operated segments for a single-level corpectomy was 16.7° (59.7% of the preoperative value), for two-level corpectomies it was 20.0° (67.2%) and for three-level corpectomies it was 22.9° (74.3%). Interestingly, the relative segmental motion preservation is more for longer segments of decompression that may be a result of the extensive removal of the PLL and the ipsilateral uncovertebral joints. Chibbaro et al. [4] mention that the mean angular motion in their series of OCC was 7.25° preoperatively, and 7.42 and 7.50° at 12 and 24 months, however, it is not clear how these angles were measured. No other studies have addressed segmental motion preservation after the OCC.
Conclusions
We found that OCC results in significant clinical improvement in patients with CSM and OPLL. Although there is a tendency for a kyphotic change in the whole spine curvature at follow-up there is no concomitant clinical worsening. In addition, we have shown that following an OCC there is preservation of motion at the operated segment at short term follow-up that is greater for longer segments of decompression. Whether this motion preservation persists in the long-term or whether progressive spinal fusion occurs to limit motion remains to be determined.
Conflict of interest
There are no sources of financial support or conflict of interest.
References
- 1.Lu J, Wu X, Li Y, Kong X. Surgical results of anterior corpectomy in the aged patients with cervical myelopathy. Eur Spine J. 2008;17(1):129–135. doi: 10.1007/s00586-007-0518-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kristof RA, Kiefer T, Thudium M, Ringel F, Stoffel M, Kovacs A, Mueller CA. Comparison of ventral corpectomy and plate-screw-instrumented fusion with dorsal laminectomy and rod-screw-instrumented fusion for treatment of at least two vertebral-level spondylotic cervical myelopathy. Eur Spine J. 2009;18(12):1951–1956. doi: 10.1007/s00586-009-1110-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lin Q, Zhou X, Wang X, Cao P, Tsai N, Yuan W (2011) A comparison of anterior cervical discectomy and corpectomy in patients with multilevel cervical spondylotic myelopathy. Eur Spine J (2011) [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 4.Chibbaro S, Mirone G, Makiese O, George B. Multilevel oblique corpectomy without fusion in managing cervical myelopathy: long-term outcome and stability evaluation in 268 patients. J Neurosurg Spine. 2009;10(5):458–465. doi: 10.3171/2009.1.SPINE08186. [DOI] [PubMed] [Google Scholar]
- 5.Chacko AG, Daniel RT. Multilevel cervical oblique corpectomy in the treatment of ossified posterior longitudinal ligament in the presence of ossified anterior longitudinal ligament. Spine. 2007;32(20):E575–E580. doi: 10.1097/BRS.0b013e31814b84fe. [DOI] [PubMed] [Google Scholar]
- 6.George B, Gauthier N, Lot G. Multisegmental cervical spondylotic myelopathy and radiculopathy treated by multilevel oblique corpectomies without fusion. Neurosurgery. 1999;44(1):81–90. doi: 10.1097/00006123-199901000-00046. [DOI] [PubMed] [Google Scholar]
- 7.Koc RK, Menku A, Akdemir H, Tucer B, Kurtsoy A, Oktem IS. Cervical spondylotic myelopathy and radiculopathy treated by oblique corpectomies without fusion. Neurosurg Rev. 2004;27(4):252–258. doi: 10.1007/s10143-004-0342-9. [DOI] [PubMed] [Google Scholar]
- 8.Kiris T, Kilincer C (2008) Cervical spondylotic myelopathy treated by oblique corpectomy: a prospective study. Neurosurgery 62(3):674–682. doi:10.1227/01.neu.0000317316.56235.a7 (discussion 674–682) [DOI] [PubMed]
- 9.Rocchi G, Caroli E, Salvati M, Delfini R. Multilevel oblique corpectomy without fusion: our experience in 48 patients. Spine. 2005;30(17):1963–1969. doi: 10.1097/01.brs.0000176327.04725.1b. [DOI] [PubMed] [Google Scholar]
- 10.Cagli S, Chamberlain RH, Sonntag VK, Crawford NR. The biomechanical effects of cervical multilevel oblique corpectomy. Spine. 2004;29(13):1420–1427. doi: 10.1097/01.BRS.0000129896.80044.B6. [DOI] [PubMed] [Google Scholar]
- 11.Vaccaro AR, Falatyn SP, Scuderi GJ, Eismont FJ, McGuire RA, Singh K, Garfin SR. Early failure of long segment anterior cervical plate fixation. J Spinal Disord. 1998;11(5):410–415. doi: 10.1097/00002517-199810000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Sasso RC, Ruggiero RA, Jr., Reilly TM, Hall PV (2003) Early reconstruction failures after multilevel cervical corpectomy. Spine (Phila Pa 1976) 28(2):140–142. doi:10.1097/00007632-200301150-00009 [DOI] [PubMed]
- 13.Gok B, Sciubba DM, McLoughlin GS, McGirt M, Ayhan S, Wolinsky JP, Bydon A, Gokaslan ZL, Witham TF. Surgical treatment of cervical spondylotic myelopathy with anterior compression: a review of 67 cases. J Neurosurg Spine. 2008;9(2):152–157. doi: 10.3171/SPI/2008/9/8/152. [DOI] [PubMed] [Google Scholar]
- 14.Mummaneni PV, Haid RW, Rodts GE Jr (2007) Combined ventral and dorsal surgery for myelopathy and myeloradiculopathy. Neurosurgery 60(1 Supp1 1):S82–S89. doi:10.1227/01.NEU.0000215355.64127.76 [DOI] [PubMed]
- 15.Konya D, Ozgen S, Gercek A, Pamir MN. Outcomes for combined anterior and posterior surgical approaches for patients with multisegmental cervical spondylotic myelopathy. J Clin Neurosci. 2009;16(3):404–409. doi: 10.1016/j.jocn.2008.07.070. [DOI] [PubMed] [Google Scholar]
- 16.Nurjck S. The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Brain. 1972;95(1):87. doi: 10.1093/brain/95.1.87. [DOI] [PubMed] [Google Scholar]
- 17.Benzel EC, Lancon J, Kesterson L, Hadden T. Cervical laminectomy and dentate ligament section for cervical spondylotic myelopathy. J Spinal Disord Tech. 1991;4(3):286. doi: 10.1097/00002517-199109000-00005. [DOI] [PubMed] [Google Scholar]
- 18.King JT, Jr, Moossy JJ, Tsevat J, Roberts MS. Multimodal assessment after surgery for cervical spondylotic myelopathy. J Neurosurg Spine. 2005;2(5):526–534. doi: 10.3171/spi.2005.2.5.0526. [DOI] [PubMed] [Google Scholar]
- 19.Boakye M, Patil CG, Santarelli J, Ho C, Tian W, Lad SP (2008) Cervical spondylotic myelopathy: complications and outcomes after spinal fusion. Neurosurgery 62(2):455–461. doi:10.1227/01.neu.0000316013.97926.4c (discussion 461–462) [DOI] [PubMed]
- 20.Yamazaki T, Yanaka K, Sato H, Uemura K, Tsukada A, Nose T. Cervical spondylotic myelopathy: surgical results and factors affecting outcome with special reference to age differences. Neurosurgery. 2003;52(1):122–126. doi: 10.1097/00006123-200301000-00015. [DOI] [PubMed] [Google Scholar]
- 21.Hukuda S, Mochizuki T, Ogata M, Shichikawa K, Shimomura Y. Operations for cervical spondylotic myelopathy. A comparison of the results of anterior and posterior procedures. J Bone Joint Surg Br. 1985;67(4):609–615. doi: 10.1302/0301-620X.67B4.4030860. [DOI] [PubMed] [Google Scholar]
- 22.Emery SE, Bohlman HH, Bolesta MJ, Jones PK. Anterior cervical decompression and arthrodesis for the treatment of cervical spondylotic myelopathy. Two to seventeen-year follow-up. J Bone Joint Surg Am. 1998;80(7):941–951. doi: 10.2106/00004623-199807000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Singh A, Crockard HA, Platts A, Stevens J. Clinical and radiological correlates of severity and surgery-related outcome in cervical spondylosis. J Neurosurg. 2001;94(2 Suppl):189–198. doi: 10.3171/spi.2001.94.2.0189. [DOI] [PubMed] [Google Scholar]
- 24.Fessler RG, Steck JC, Giovanini MA (1998) Anterior cervical corpectomy for cervical spondylotic myelopathy. Neurosurgery 43(2):257–265. doi:10.1097/00006123-199808000-00044 (discussion 265–257) [DOI] [PubMed]
- 25.Ebersold MJ, Pare MC, Quast LM. Surgical treatment for cervical spondylitic myelopathy. J Neurosurg. 1995;82(5):745–751. doi: 10.3171/jns.1995.82.5.0745. [DOI] [PubMed] [Google Scholar]
- 26.Alafifi T, Kern R, Fehlings M. Clinical and MRI predictors of outcome after surgical intervention for cervical spondylotic myelopathy. J Neuroimaging. 2007;17(4):315–322. doi: 10.1111/j.1552-6569.2007.00119.x. [DOI] [PubMed] [Google Scholar]
- 27.Mastronardi L, Elsawaf A, Roperto R, Bozzao A, Caroli M, Ferrante M, Ferrante L. Prognostic relevance of the postoperative evolution of intramedullary spinal cord changes in signal intensity on magnetic resonance imaging after anterior decompression for cervical spondylotic myelopathy. J Neurosurg Spine. 2007;7(6):615–622. doi: 10.3171/SPI-07/12/615. [DOI] [PubMed] [Google Scholar]
- 28.Liu T, Xu W, Cheng T, Yang HL (2011) Anterior versus posterior surgery for multilevel cervical myelopathy, which one is better? A systematic review. Eur Spine J 20(2):224–235 [DOI] [PMC free article] [PubMed]
- 29.Sakai K, Okawa A, Takahashi M, Arai Y, Kawabata S, Enomoto M, Kato T, Hirai T, Shinomiya K (2011) 5-year Follow-up evaluation of surgical treatment for cervical myelopathy caused by ossification of the posterior longitudinal ligament: a prospective comparative study of anterior decompression and fusion with floating method versus laminoplasty. Spine (Phila Pa 1976) [Epub ahead of print] [DOI] [PubMed]