To the Editor,
It was with great interest that we read the article by N. Rahamimov et al., “Percutaneous augmented instrumentation of unstable thoracolumbar burst fractures,” published in the 2011 December issue of European Spine Journal [1].
This is a well-prepared article, which introduces a novel approach, combining percutaneous posterior short-segment pedicle screw augmentation with polymethylmethacrylate (PMMA) and fractured vertebra kyphoplasty to treat unstable thoracolumbar burst fractures. The kyphoplasty mentioned in the article yielded a high ratio of cement leakage (52/52) mainly through fracture line or segmental veins and caused three cases of PMMA pulmonary emboli.
In our experience, the risk of cement leakage can be avoided with some good manners [2–4]. The higher viscosity PMMA injected is the key factor to prevent cement leakage. In the procedure, we control ideal level of viscosity when the cement is not runny any more, becomes doughy, does not stick to the fingers and can stand erect at the tip of the bone cement inserter when pushed out, it is considered to be able to block mostly segmental veins. For the fracture line in the anterior wall, small amounts of middle- or late-stage bone cement in the dough phase are used to block the defect to protect against anterior leakage firstly. After the cement has solidified, late-stage bone cement in the paste phase or early stage bone cement in the dough phase is applied to allow the filling to diffuse evenly. For patients with damaged posterior wall, the filling process is stopped as soon as the bone cement reaches the lateral margin or when one-fourth of the distance to the posterior wall of vertebra left under continuous fluoroscopic monitoring (Figs. 1, 2). When the lateral wall is damaged, we fill 1 mL of viscous cement after expanding the intravertebral space and removing the balloon. Then we reinsert the balloon into the cement and reinflating it, in order to expand the surrounding cement until it abuts the compromised lateral wall. Finally, conventional cement filling is performed.
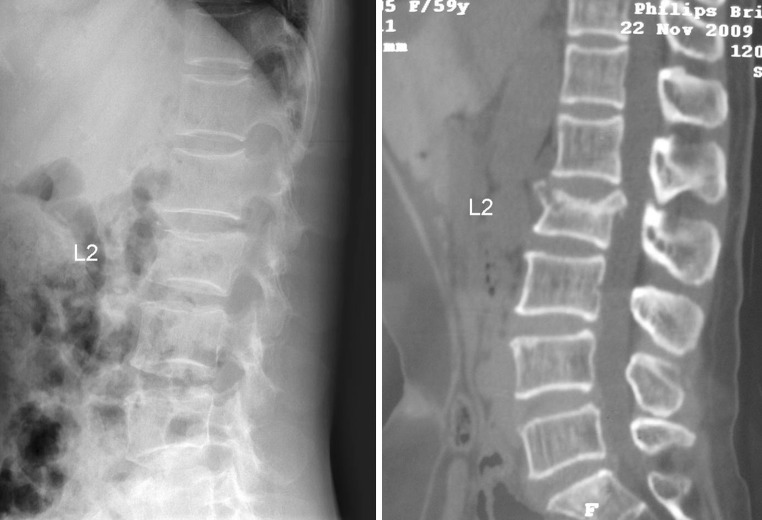
Fig. 1.
Radiographs from a 60-year-old woman with fractures of L2 with anterior and posterior vertebral wall deficiency preoperatively
Fig. 2.
Postoperative radiographs showed a cement barrier in the anterior wall (white arrows) and a safe distance to posterior wall, no cement leakage was found. A small amount of bone cement was used to prevent anterior leakage, just after the first filling had solidified, late-stage bone cement in the paste phase was injected and stopped as soon as one-fourth of the distance to the posterior wall of vertebra left
In summary, to patients with unstable thoracolumbar burst fractures, regardless of whether the fracture line is located at the anterior, posterior or lateral wall of the vertebral body, bone cement leakage can be prevented by some tips introduced above.
Conflict of interest
There is no actual or potential conflict of interest.
References
- 1.Rahamimov N, Mulla H, Shani A, Freiman S (2011) Percutaneous augmented instrumentation of unstable thoracolumbar burst fractures. Eur Spine J. doi:10.1007/s00586-011-2106-x [DOI] [PMC free article] [PubMed]
- 2.Zou J, Mei X, Gan M, Yang H. Is kyphoplasty reliable for osteoporotic vertebral compression fracture with vertebral wall deficiency? Injury. 2010;41:360–364. doi: 10.1016/j.injury.2009.09.033. [DOI] [PubMed] [Google Scholar]
- 3.Qian Z, Sun Z, Yang H, Yong G, Chen K, Guizhong W. Kyphoplasty for the treatment of malignant vertebral compression fractures caused by metastases. J Clin Neurosci. 2011;18:763–767. doi: 10.1016/j.jocn.2010.09.021. [DOI] [PubMed] [Google Scholar]
- 4.Zou J, Mei X, Gan M, Yang H. Kyphoplasty for spinal fractures from multiple myeloma. J Surg Oncol. 2010;102(1):43–47. doi: 10.1002/jso.21574. [DOI] [PubMed] [Google Scholar]