Abstract
Background
Charcot-Marie-Tooth disease is the most common inherited nerve disorder and typically presents with pes cavus foot deformity and ankle equinus during childhood. Level in the variation of symmetry of musculoskeletal lower limb involvement across the clinical population is unknown, despite early reports describing gross asymmetry.
Methods
We measured foot alignment and ankle flexibility of the left and right limbs using accurate and reliable standardised paediatric outcome measures in 172 patients aged 3–20 years with a variety of disease subtypes recruited from the United States, United Kingdom, Italy and Australia.
Findings
While a large range of differences existed between left and right feet for a small proportion of children, there was no overall significant difference between limbs.
Interpretation
There are two important implications of these findings. Children with Charcot-Marie-Tooth disease generally exhibit symmetrical foot alignment and ankle flexibility between limbs. As such, analysing one limb only for biomechanical-related research is appropriate and satisfies the independence requirements for statistical analysis. However, because there are large differences between feet for a small proportion of children, an individualised limb-focused approach to clinical care is required.
Keywords: Foot, ankle, Charcot-Marie-Tooth disease, Foot Posture Index, children, pes cavus
1. Introduction
Charcot-Marie-Tooth disease (CMT), a group of genetically-based nerve disorders, affects ~1 in 2500 people and is among the most common inherited neurological disorders (Skre, 1974). It is characterised by demyelination and/or axonal loss of the peripheral nerves. As a result there is progressive weakness of the distal, and to a lesser extent proximal, limb musculature, hand, foot and ankle deformities, impairment of motor function, and sensory loss.
During childhood, CMT usually presents with lower limb muscle imbalance and ankle contracture associated with a painful cavus (high-arched) foot deformity which becomes increasingly severe and rigid as the disease progresses (Burns et al., 2005). Foot alignment and ankle flexibility are thought to be generally symmetrical; however cases of asymmetry are reported and are considered more severe. Indeed the original description by Charcot and Marie in 1886 shows gross foot and ankle asymmetry (Figure 1) (Charcot and Marie, 1886). Retrospective chart reviews have previously identified a small proportion of children (4 of 52) with one cavovarus and one planovalgus foot (Wines et al., 2005), and a small proportion of adults (5 of 61) with pes cavus and ankle contracture asymmetry (Bienfait et al., 2006). However, these studies are limited by their retrospective design and unclear methods of foot and ankle assessment.
Figure 1.
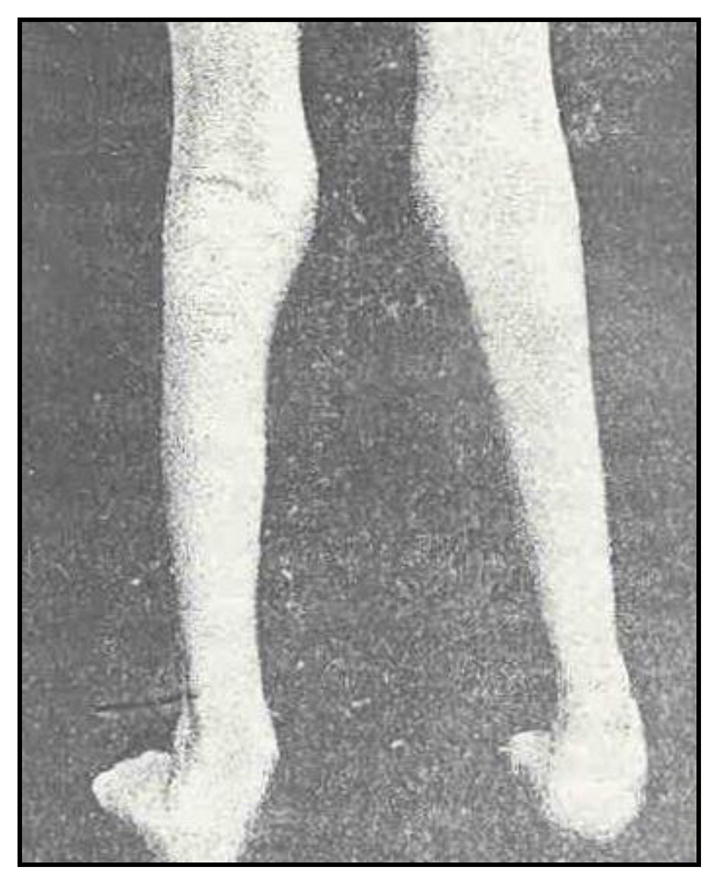
Marked foot and ankle asymmetry as shown in the original description of CMT (Charcot and Marie, 1886).
The aim of this study was to prospectively evaluate the frequency and extent of symmetrical foot and ankle involvement between limbs of children with CMT using reliable and validated outcome measures.
2. Methods
This study was conducted as part of the Inherited Neuropathies Consortium and included leading paediatric tertiary healthcare institutions of Detroit, London, Milan, Philadelphia, Rochester and Sydney. Ethics approval from all institutions for all studies, and written informed assent/consent from all children and their families was obtained.
Objective measurements of left and right foot alignment and ankle flexibility were obtained from all children using highly reliable and validated age-appropriate items from the Charcot-Marie-Tooth disease Pediatric Scale (CMTPedS) (Burns et al., 2012). Specifically, foot alignment was measured using the Foot Posture Index (FPI) (Cain et al., 2007, Menz and Munteanu, 2005, Redmond et al., 2006), and ankle dorsiflexion range of motion assessed with the lunge test (Burns and Crosbie, 2005, Khan et al., 1997).
Data were analysed in SPSS version 18.0 (Chicago, IL, USA). Normality of data distribution was assessed using the Kolmogorov-Smirnov test, and the appropriate parametric or non-parametric tests subsequently employed. To account for the ordinal nature of FPI data, left and right total FPI scores were transformed to their equivalent logit values as per the Rasch model for parametric statistical analysis (Keenan et al., 2007) and back transformed to raw FPI values for descriptive purposes. Cross-checking for external validation using baseline data from the Australian Ascorbic Acid Trial of 81 children with the most common type of CMT, Type 1A, was also conducted (Burns et al., 2009).
3. Results
During a 14-month prospective period, 172 patients aged 3–20 years were recruited. Patient profile was: 90 female (52%); mean age 10.8yrs (SD 4.2); mean height 1.44m (SD 0.22); mean weight 42.5kg (SD 18.9). The sample comprised a broad range of CMT subtypes. Lower limb symptoms reported by the children included: foot pain in 66 (38%); leg cramps in 68 (40%); ankle instability during walking in 84 (49%); daily trips/falls in 82 (48%); sensory symptoms in 54 (31%). Foot drop was evident in 104 (60%) cases, difficulty heel walking in 146 (85%) and difficulty toe-walking was evident in 65 (38%) children. Sixteen (9%) children required Ankle-Foot-Orthoses to walk.
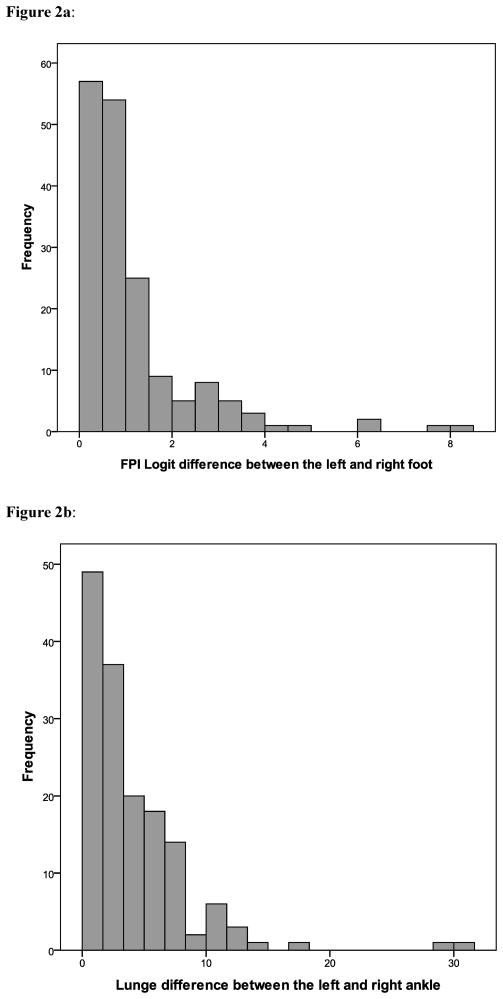
The raw mean FPI of the left foot was 1.2 (SD 4.6, range −12 to 12) and raw mean FPI of the right foot was 1.2 (SD 4.4, range −11 to 11). The mean FPI logit of the left foot was 0.7 (SD 3.1, range −10.5 to 8.7) and mean FPI logit of the right foot was 0.6 (SD 2.9, range −8.0 to 7.8). According to FPI criteria (Redmond et al., 2008), 55 (32%) children had pes cavus (FPI logit < −0.21) which became more prevalent with advancing age (r=0.317, p<0.0001, point-biserial correlation coefficient). Based on absolute values of left-right differences there was a large range between individual left and right FPI logit scores (0 to 8) (Figure 2a), but there were no significant group differences between limbs (mean difference 0.02, SD 1.7, t=1.44, p=0.89). Correlation between feet was very high (r=0.84, p<0.001). Nine (5%) children had a large clinically significant difference (>2SD) between limbs (FPI logit >3.4) and 138 (80%) children had a negligible difference (<1SD) between limbs (FPI logit <1.7). Asymmetrical cases were generally more disabled according to the CMTPedS (24 vs 20 points on the 0–44 point scale) (Burns et al., 2012).
Figure 2.
Figure 2a: Symmetry of foot alignment in children with CMT.
Figure 2b: Symmetry of ankle flexibility in childhood CMT.
The mean lunge angle of the left ankle was 22.10 (SD 8.9, range −12 to 380). Mean lunge angle of the right ankle was 22.60 (SD 8.6, range 0 to 390). Again based on absolute values of left-right differences there was a large range between individual left and right ankles for the lunge test (0 to 310) (Figure 2b), but there were no significant group differences between limbs (mean difference 0.70, SD 6.1, t=1.34, p=0.18). Correlation between ankles was high (r=0.76, p<0.001). Five (3%) children had a large clinically significant difference (>2SD) between limbs (Lunge >12.20) and 123 (72%) children had a negligible difference (<1SD) between limbs (Lunge <6.10). Asymmetrical cases were generally more disabled according to the CMTPedS (26 vs 19 points on the 0–44 point scale) (Burns et al., 2012).
Cross-checking with the Australian Ascorbic Acid Trial of 81 children (47 boys, 34 girls) aged 2–16 years, showed that the mean FPI logit of the left foot was 1.3 (SD 3.6, range -10.5 to 7.8) and the mean FPI logit of the right foot was 1.0 (SD 3.4, range −10.5 to 7.8). Again, there was no significant FPI difference between limbs (mean difference 0.3, SD 1.9, t=0.1.38, p=0.17).
4. Discussion
There are two important implications of these findings. Children with CMT generally exhibit symmetrical foot alignment and ankle flexibility between limbs. As such, analysing one limb only for biomechanical-related research (e.g. dominant foot, worst foot, or randomly selected foot) is appropriate and satisfies the independence requirements for statistical analysis (Menz, 2005). However, because there are large differences between feet for a small proportion of children, an individualised limb-focused approach to clinical care is required.
While asymmetry in this large cohort was rare, it was related to overall disability of the disease, as measured by the CMTPedS. The CMTPedS score has been shown to be highly sensitive to CMT type, worsens with age, and clearly reflects the severity of the disease (Burns et al., 2012). As such asymmetry of foot alignment and ankle flexibility is more likely to be observed in children more affected by the disease.
Interestingly, it has been reported that in pairs of male homozygotic twins with CMT1A the symmetry of neurophysiologic deficit contrasted markedly with the variable and asymmetric clinical presentations, including unilateral foot drop (Garcia et al., 1995). Variability of clinical expression in these patients with identical mutations, and in our sample, suggests the action of endogenous factors, environmental modulation or gene modifiers of disease asymmetry.
5. Conclusion
Despite early classical reports showing gross foot and ankle asymmetry (Figure 1), most children with CMT typically have symmetrical foot alignment and ankle flexibility, as shown in Figure 3.
Figure 3.

Foot and ankle pes cavus foot deformity shown in a typical symmetrical case of CMT.
Acknowledgments
We are grateful for the assistance of site co-investigators: Allan Glanzman, PT (Children's Hospital of Philadelphia, PA, USA), Polly Swingle, PT; Agnes Patzko, MD; Sindhu Ramchandren, MD (Wayne State University Detroit, MI, USA), Isabella Moroni, MD; Emanuela Pagliano, MD (IRCCS Foundation Carlo Besta Neurological Institute, Milan, Italy); Andy Hiscock, PT (UCL Institute of Child Health & Great Ormond Street Hospital, London, UK), Monique Ryan, MD; Eppie Yiu, MD (Royal Children's Hospital, Melbourne, Australia), Manoj Menezes, MD (Children's Hospital at Westmead, University of Sydney, Australia). Part of this work was undertaken at University College London Hospitals/University College London, which received a proportion of funding from the Department of Health's National Institute for Health Research Biomedical Research Centres funding scheme. We also wish to thank the patients and their families for their participation in the study.
Footnotes
Conflict of Interest Statement and Funding
The authors have no conflicts of interest to declare related to this study. This research was supported by grants from the NHMRC (National Health and Medical Research Council of Australia, #1007569), NIH (National Institutes of Neurological Disorders and Stroke and Office of Rare Diseases, #U54NS065712), Charcot Marie Tooth Association (CMTA), Muscular Dystrophy Association (MDA) and CMT Association of Australia (CMTAA).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bienfait HM, Verhamme C, Van Schaik IN, Koelman JH, De Visser BW, De Haan RJ, et al. Comparison of CMT1A and CMT2: similarities and differences. Journal of Neurology. 2006;253:1572–80. doi: 10.1007/s00415-006-0260-6. [DOI] [PubMed] [Google Scholar]
- Burns J, Crosbie J. Weight bearing ankle dorsiflexion range of motion in idiopathic pes cavus compared to normal and pes planus feet. The Foot. 2005;15:91–94. [Google Scholar]
- Burns J, Crosbie J, Hunt A, Ouvrier R. The effect of pes cavus on foot pain and plantar pressure. Clinical Biomechanics. 2005;20:877–82. doi: 10.1016/j.clinbiomech.2005.03.006. [DOI] [PubMed] [Google Scholar]
- Burns J, Ouvrier R, Estilow T, Shy R, Laurá M, Pallant J, et al. Validation of the CMT Pediatric Scale as an outcome measure of disability. Annals of Neurology. doi: 10.1002/ana.23572. Epub ahead of print, DOI: 10.1002/ana.23572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns J, Ouvrier RA, Yiu EM, Joseph PD, Kornberg AJ, Fahey MC, et al. Ascorbic acid for Charcot-Marie-Tooth disease type 1A in children: a randomised, double-blind, placebo-controlled, safety and efficacy trial. Lancet Neurology. 2009;8:537–44. doi: 10.1016/S1474-4422(09)70108-5. [DOI] [PubMed] [Google Scholar]
- Cain LE, Nicholson LL, Adams RD, Burns J. Foot morphology and foot/ankle injury in indoor football. Journal of Science & Medicine in Sport. 2007;10:311–9. doi: 10.1016/j.jsams.2006.07.012. [DOI] [PubMed] [Google Scholar]
- Charcot JM, Marie P. Sur une forme particulière d'atrophie musculaire progressive, souvent familiale débutant par les pieds et les jambes et atteignant plus tard les mains. Rev Med (Paris) 1886;6:97–138. [Google Scholar]
- Garcia CA, Malamut RE, England JD, Parry GS, Liu P, Lupski JR. Clinical variability in two pairs of identical twins with the Charcot-Marie-Tooth disease type 1A duplication. Neurology. 1995;45:2090–3. doi: 10.1212/wnl.45.11.2090. [DOI] [PubMed] [Google Scholar]
- Keenan AM, Redmond AC, Horton M, Conaghan PG, Tennant A. The Foot Posture Index: Rasch analysis of a novel, foot-specific outcome measure. Archives of Physical Medicine & Rehabilitation. 2007;88:88–93. doi: 10.1016/j.apmr.2006.10.005. [DOI] [PubMed] [Google Scholar]
- Khan K, Roberts P, Nattrass C, Bennell K, Mayes S, Way S, et al. Hip and ankle range of motion in elite classical ballet dancers and controls. Clinical Journal of Sport Medicine. 1997;7:174–9. doi: 10.1097/00042752-199707000-00004. [DOI] [PubMed] [Google Scholar]
- Menz HB. Analysis of paired data in physical therapy research: Time to stop double dipping? Journal of Orthopaedic & Sports Physical Therapy. 2005;35:477–78. doi: 10.2519/jospt.2005.0108. [DOI] [PubMed] [Google Scholar]
- Menz HB, Munteanu SE. Validity of 3 clinical techniques for the measurement of static foot posture in older people. J Orthop Sports Phys Ther. 2005;35:479–86. doi: 10.2519/jospt.2005.35.8.479. [DOI] [PubMed] [Google Scholar]
- Redmond A, Crane Y, Menz H. Normative values for the Foot Posture Index. Journal of Foot and Ankle Research. 2008;1:6. doi: 10.1186/1757-1146-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redmond A, Crosbie J, Ouvrier R. Development and validation of a novel rating system for scoring standing foot posture: The Foot Posture Index. Clinical Biomechanics. 2006;21:89–98. doi: 10.1016/j.clinbiomech.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Skre H. Genetic and clinical aspects of Charcot-Marie-Tooth disease. Clinical Genetics. 1974;6:98–118. doi: 10.1111/j.1399-0004.1974.tb00638.x. [DOI] [PubMed] [Google Scholar]
- Wines AP, Chen D, Lynch B, Stephens MM. Foot deformities in children with hereditary motor and sensory neuropathy. Journal of Pediatric Orthopedics. 2005;25:241–44. doi: 10.1097/01.bpo.0000151057.39485.4b. [DOI] [PubMed] [Google Scholar]