Abstract
Tyrosine kinase inhibitors (TKIs) that target the epidermal growth factor receptor (EGFR) are effective in most NSCLC patients whose tumors harbor activating EGFR kinase domain mutations. Unfortunately, acquired resistance eventually emerges in these chronically treated cancers. Two of the most common mechanisms of acquired resistance to TKIs seen clinically are the acquisition of a secondary “gatekeeper” T790M EGFR mutation that increases the affinity of mutant EGFR for ATP and activation of MET to offset the loss of EGFR signaling. Although up to one-third of patient tumors resistant to reversible EGFR TKIs harbor concurrent T790M mutation and MET amplification, potential therapies for these tumors have not been modeled in vivo. In this study, we developed a preclinical platform to evaluate potential therapies by generating transgenic mouse lung cancer models expressing EGFR-mutant Del19-T790M or L858R-T790M, each with concurrent MET overexpression. We found that monotherapy targeting EGFR or MET alone did not produce significant tumor regression. In contrast, combination therapies targeting EGFR and MET simultaneously were highly efficacious against EGFR TKI resistant tumors co-driven by Del19-T790M or L858R-T790M and MET. Our findings therefore provide an in vivo model of intrinsic resistance to reversible TKIs and offer preclinical proof of principle that combination targeting of EGFR and MET may benefit patients with NSCLC.
INTRODUCTION
Activating mutations in the kinase domain of epidermal growth factor receptor (EGFR) in non–small cell lung cancers (NSCLC) commonly arise as in-frame deletions in exon 19 and L858R exon 21 substitutions, and confer sensitivity to the reversible tyrosine kinase inhibitors (TKI) gefitinib and erlotinib (1–3). Despite initial responses, NSCLCs driven by EGFR activating mutations inevitably develop resistance to these TKIs. An acquired T790M mutation emerges in ~50% of EGFR-mutated patients with TKI resistance (4–9). The threonine to methionine change at the 790 amino acid “gatekeeper” residue in the EGFR kinase domain has been shown to confer resistance by increasing the affinity for ATP, compromising the potency of reversible TKIs (10). In contrast to the reversible TKIs, irreversible TKIs, including PF00299804 and BIBW2992, are thought to overcome T790M-mediated resistance because they do not compete with ATP, but rather covalently bind to the C797 residue of EGFR to irreversibly inhibit receptor tyrosine kinase activity (7, 11, 12). Irreversible EGFR TKIs, HKI-272 and BIBW2992, are modestly efficacious as single agents in a transgenic mouse model of lung adenocarcinoma driven by EGFR L858R-T790M (13, 14), or in monotherapy clinical trials (15) and they do not fully extinguish downstream signaling, prompting their combination with inhibitors of mTOR preclinically and in clinical trials (16, 17). In contrast, an EGFR mutant-specific irreversible TKI (WZ4002) has been shown to be highly potent and efficacious in both EGFR L858R-T790M and EGFR exon 19 del-T790M-driven lung adenocarcinoma models, and molecules from this class are eagerly anticipated in clinical trials (18).
In addition to the secondary gatekeeper mutation, NSCLC patients whose tumors harbor sensitizing EGFR mutations and who initially respond to reversible EGFR TKIs may also acquire resistance through activation of MET, via HGF ligand and MET gene amplification, which serves to re-activate the PI3K signaling axis (6, 19, 20). The frequency of resistant cases with MET amplification ranges from 5 to 15% depending on the study (6, 9, 21). This mechanism was first demonstrated in HCC827 (EGFR E746_A750del) cells rendered gefitinib-resistant in vitro. In TKI-resistant HCC827 cells, only simultaneous inhibition of both MET and EGFR was able to suppress downstream proliferation and survival pathways, required for antiproliferative effects in vitro and anti-tumor efficacy in vivo (6, 19). In contrast, NCI-H820 cells naturally harbor concurrent EGFR TKI-resistant EGFR mutation (E746_T751del, T790M) and MET amplification. In these cells, small molecule c-Met inhibition or siRNA-mediated MET depletion was sufficient to dephosphorylate ERBB3 and to compromise the cell viability, suggesting that resistant NCI-H820 rely more heavily on MET signaling for survival (16).
Interestingly, several studies have identified primary tumors genotypically similar to NCI-H820 cells, with concurrent T790M mutation and moderate MET amplification in 5 to 33% of NSCLC patients who become refractory to reversible EGFR TKIs (4, 9, 16, 22, 23). The presence of EGFR T790M mutation further enhances the oncogenic potential of EGFRs carrying sensitizing mutations in vitro (24) and in vivo (13). However, the interaction of concomitant T790M mutation with MET amplification has only been studied in NCI-H820 cells to date, and has not been modeled in vivo. In order to clarify whether combined irreversible EGFR and MET inhibition is required for anti-tumor activity when both abnormalities are present, we have generated mouse lung cancer models expressing EGFR-mutant Del19-T790M or L858R-T790M, each with concurrent hMET overexpression. Using these models, we have assessed the efficacy of various monotherapies and combination treatments, providing a platform for development of clinical trials for patients whose tumors harbor multiple mechanisms of EGFR TKI-resistance.
MATERIALS AND MEHTODS
Generation of the CCSP-rtTA/Tet-op-hMET Mouse and the CCSP-rtTA/Tet-op-hMET/EGFR Mouse
A cohort of genetically engineered mice harboring a doxycycline-inducible human MET (hMET) oncogene was generated similar to mouse models we have previously described (13, 21). Briefly, we constructed a 6.5 kb DNA segment consisting of seven direct repeats of the tetracycline (tet)-operator sequence, followed by human MET cDNA and β-globin polyA. The construct was injected into FVB/N blastocysts, and progeny were screened using a PCR strategy (25). Founders were identified and then crossed to Clara cell secretory protein (CCSP)-rtTA mice, harboring an allele that specifically targets the expression of the reverse tetracycline transactivator protein (rtTA) in type II alveolar epithelial cells (26, 27) to generate inducible bitransgenic mouse cohorts harboring both the activator and the responder transgenes. Two tightly regulated hMET founders (#16 and #31) were identified by RT-PCR. CCSP-rtTA/MET mice were then crossed with CCSP-rtTA/EGFR exon 19 deletion/T790M (TD) mice (18) or with CCSP-rtTA/EGFR L858R/T790M (TL) mice (13) to generate animals expressing CCSP-rtTA/EGFR TD/MET (TD/MET) or CCSP-rtTA/EGFR TL/MET (TL/MET), respectively. All mice were housed in a pathogen-free environment at the Harvard School of Public Health and were handled in accordance with Good Animal Practice as defined by the Office of Laboratory Animal Welfare.
RT-PCR and Quantitative PCR
Total RNA samples were prepared as previously described (25) and then retro-transcribed into first-strand cDNA using the Superscript First Strand Synthesis System following the manufacturer’s protocol (Life Technologies, Carlsbad, CA). Quantitative real-time PCR was performed by monitoring the increase in fluorescence of SYBR green, FAM or VIC dyes in real-time (Qiagen, Valencia, CA) with the ABI 7700/StepOne Plus sequence detection system (Life Technologies, Carlsbad CA). Primers used for RT-PCR and real-time PCR are as follows. Real-time PCR primers: Forward TTACGGACCCAATCATGAGC; Reverse ACTTCGCTGAATTGACCCAT; genotyping PCR primers: Forward CTGGCACCCTAAAGCCGAAA; Reverse TGCTTTATTTGTGAAATTTGTGATGC. Real-time Primers and probes for human MET and EGFR were purchased from Life Technologies (Assay IDs: Hs01565584_m1 and Hs01076078_m1, respectively). Each sample was amplified in duplicate or triplicate for quantification of both transgenes and β-actin transcripts. Data were analyzed by relative quantitation using the ΔΔCt method and normalization to β-actin.
Mouse drug treatment studies
All animal treatment studies were reviewed and approved by the IACUC at the Dana-Farber Cancer Institute. As previously described (12, 13, 25, 28–31), transgenic mice were exposed to a doxycycline-containing diet for 8 to 12 weeks, and subjected to magnetic resonance imaging (MRI) to document tumor burden. After initial imaging, animals were subjected to treatment with WZ4002 formulated in 10% 1-methyl-2-pyrrolidinone/90% PEG-300 by gavage at 50mg/kg daily; crizotinib (PF-02341066) formulated in saline by gavage at 20mg/kg daily or 50mg/kg daily; or 17-DMAG (LC laboratories) formulated in saline by i.p. injection at 20mg/kg daily. Cetuximab was used at 50mg/kg (Q3D). Drugs were administered as single agents or in combination.
MRI imaging and tumor volume measurement
Mice were imaged by MRI to determine the reduction in tumor volume after two-weeks of treatment, and then sacrificed for further histological and biochemical studies. For pharmacodynamic studies, 2 doses of drugs were administrated within 24 hours, with the first dose on day 1 and the second dose on day 2, two hours prior to sacrifice and the harvesting of tumor nodules. MRI measurements were performed as previously described (13, 25). Using the RARE sequence scans, tumor volume measurements were generated using in-house custom software. The MRI images were optimized for the mediastinal window setting and were saved on a computer as 8-bit grayscale JPEG files. Analysis was performed using ImageJ software (NIH). Consecutive 10 to 16 images (slice thickness, 1mm; interslice gap, 1mm) containing lung tumor were used for each mouse to measure tumor areas. Normal structures of the body, including chest wall, heart, liver, and normal mediastinal structures, were omitted manually from the images, so that lung fields were selected for further examination. High intensity areas above the automatic threshold of the software were selected and measured to calculate total tumor areas.
Histology and immunohistochemistry
Mice were sacrificed and the left lung was dissected and snap-frozen for biochemical analysis. The right lung was inflated with buffered 10% formalin for 10 min and fixed in 10% formalin overnight at room temperature. The specimen was washed once in PBS, placed in 70% ethanol, and embedded in paraffin, from which 5μm sections were generated. Immunohistochemistry (IHC), and Hematoxylin and eosin (H&E) stains were performed in the Department of Pathology at Brigham and Women’s Hospital; all antibodies were from Cell Signaling Technologies (CST, Danvers MA).
Western blot analysis
Snap-frozen tumor nodules were homogenized in RIPA buffer supplemented with protease and phosphatase inhibitor cocktails (EMD Biosciences, San Diego, CA) and subjected to Western blotting using the antibodies indicated in the figures. A list of antibodies used is available in the Supplementary Methods.
Statistical analysis
Statistical analyses were performed using Student’s t-test (32). A p-value < 0.05 was considered statistically significant.
RESULTS
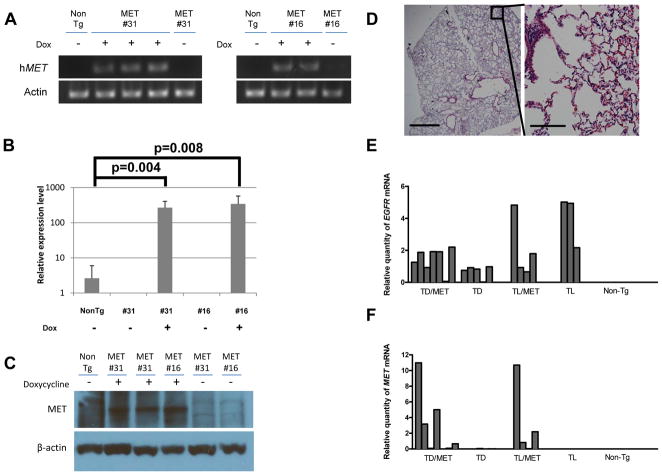
Tightly regulated expression of hMET mRNA and protein in lung tissue
We generated a cohort of genetically engineered mice, Tet-op-hMET/CCSP-rtTA, harboring a doxycycline-inducible human MET (hMET) oncogene, similar to mouse models we have previously described (13, 25). RT-PCR with transgene-specific primers was performed to determine the inducibility of hMET RNA expression in the lungs of each potential founder before and after 12 weeks of doxycycline administration. The hMET transcripts were undetectable from both non-transgenic and the bitransgenic mice without doxycycline administration, but 12 weeks of doxycycline administration robustly induced transgene expression (Fig. 1A and 1B). The induction of hMET was verified at the protein level by Western blotting of lung lysates from the non-transgenic and the bitransgenic mice before and after doxycycline administration (Fig. 1C). Induction of hMET protein was shown in samples from bitransgenic mice after doxycycline administration, but not in samples from bitransgenic mice before doxycycline administration or non-transgenic mice (Fig. 1C). The expression of hMET alone was not sufficient to form tumors in the bitransgenic models (Fig. 1D).
Figure 1. Induction of hMET tyrosine kinase at both RNA and protein levels in bitransgenic mice from different founders.
(A) Bitransgenic mice were fed a diet without (−) or with (+) doxycycline. After 12 weeks of doxycycline treatment, mRNA from the lungs from two founders (#31 and #16) was subjected to RT-PCR analysis to determine the transcriptional level of hMET.
(B) Quantitative RT-PCR analysis of total MET transcript induction in bitransgenic mice fed a diet without (−) or with (+) doxycycline for 12 weeks. Each sample was amplified in triplicate for quantification of both total MET and β-actin transcripts. The endogenous mouse met level from normal mice was arbitrarily designated as 1. Data were analyzed by relative quantitation using the ΔΔCt method with normalization to β-actin. Error bars, S.D.
(C) Bitransgenic mouse founders were treated without (-) or with (+) doxycycline for 12 weeks, and lung lysates were subjected to Western blotting for total MET and β-actin.
(D) H&E images of normal lung from a CCSP-rtTA/MET bitransgenic mouse fed with a doxycycline-containing diet for 52 weeks. The right micrograph is a magnified view of the area indicated in the low magnification micrograph shown on the left. Scale bars indicate 1000 μm (left) or 100 μm (right), respectively. There was no evidence of malignant tumor observed in six CCSP-rtTA/MET bitransgenic mice that were maintained on a doxycycline-containing diet for more than 40 weeks.
(E,F) Quantitative RT-PCR analysis of total hEGFR (E) and hMET (F) transcript in bi- or tri-transgenic mice on a doxycycline-containing diet. Each sample was amplified in duplicate for quantification of EGFR, MET and β-actin transcripts. Mean expression level of human MET or human EGFR from TD/MET mouse was arbitrarily designated as 1. Data were analyzed by relative quantitation using the ΔΔCt method and normalization to β-actin. Each bar represents the relative quantity of mRNA in one mouse.
Previously, we reported that the irreversible EGFR TKIs BIBW2992 and the EGFR mutant-specific irreversible EGFR TKI WZ4002 promote tumor regression in murine lung cancers driven by human EGFR L858R/T790M (TL) (12) or human EGFR exon19 deletion/T790M (TD) (18). To investigate if the overexpression of the hMET oncogene confers intrinsic resistance to irreversible EGFR TKI treatment in murine lung cancer expressing TD or TL, we crossed Tet-op-hMET/CCSP-rtTA expressing animals with those expressing Tet-op-EGFR TD/CCSP-rtTA (18) or Tet-op-EGFR TL/CCSP-rtTA (13) to generate Tet-op-hMET/EGFR TD/CCSP-rtTA (TD/MET) or Tet-op-hMET/EGFR TL/CCSP-rtTA (TL/MET) cohorts. hEGFR transcripts were undetectable from non-transgenic mice but 12 weeks of doxycycline administration robustly induced transgene expression in all mouse models used in this study (Fig. 1E). The hMET transcripts were abundantly expressed in tumors from TD/MET and TL/MET mice but virtually undetectable in tumors from non-transgenic mice, as well as in tumors from TD and TL mice (Fig. 1F). Expression of hMET protein and its phosphorylated form in the TD/MET and TL/MET models was also verified by Western blot (Supplementary Fig. 1A and B). In both the TD/MET and TL/MET models, there were no significant differences in expression of the hMET transgene between total lung and tumor nodules (Supplementary Fig. 2).
Overexpression of the hMET oncogene confers intrinsic resistance to irreversible EGFR TKI treatment in murine lung cancer models with mutant EGFR
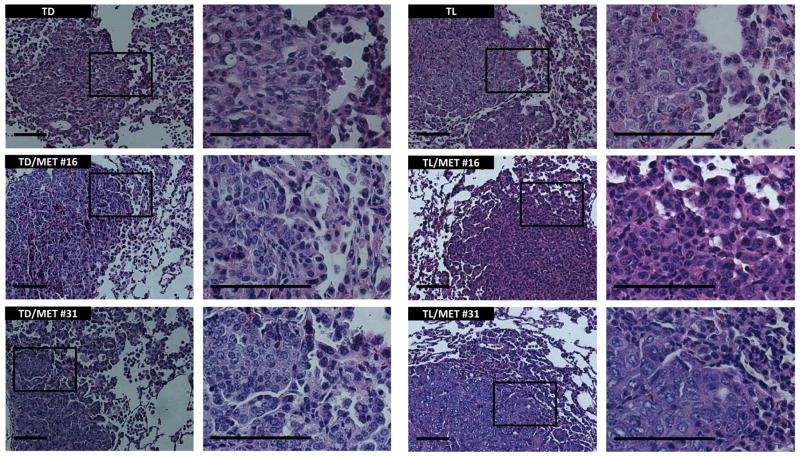
After 8–12 weeks of doxycycline administration, mice were sacrificed and lung sections were stained with H&E (Fig. 2). TD and TL mice developed both parenchymal and bronchial adenocarcinomas as previously reported (13) and co-expression of hMET and TD or TL did not significantly change the histopathologic features of these lung tumors. Similarly, there was no significant increase in tumor burden in TL/MET mice due to the expression of hMET (Supplementary Fig. 3).
Figure 2. Histological comparison of the murine mutant EGFR lung tumors with or without co-expression of hMET.
Representative hematoxylin and eosin (H&E) staining of cross-sectional views of different transgenic mouse lungs showing no significant difference in histopathologic assessments of lung carcinoma. Picture on the right for each genotype is a magnified view of the area indicated in the picture with low magnification on the left. Scale bars 100μm.
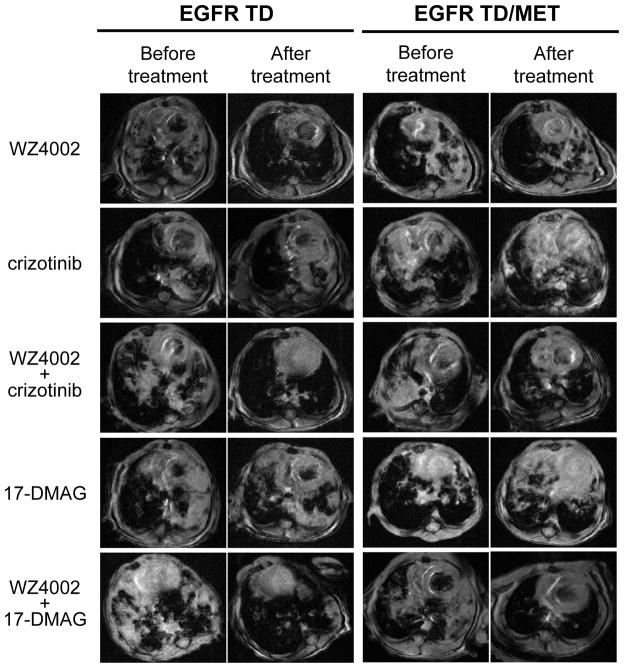
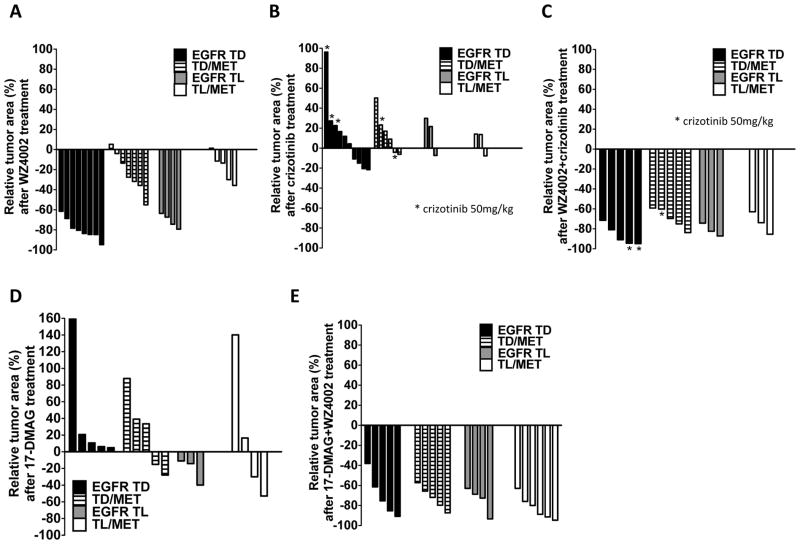
Before treatment, TD, TL, TD/MET and TL/MET mice were imaged with MRI to document the baseline tumor burden (Fig. 3 and Supplementary Fig. 4). Tumor-bearing mice were then treated with 50mg/kg WZ4002 daily for 2 weeks, a previously established effective regimen in the TD and TL models (25). Quantification of MRI images revealed that all of the TD or TL mice showed significant tumor reduction by MRI (−79.6% and −71.2%, respectively, Fig. 4A). In contrast, the introduction of the MET oncogene confers intrinsic resistance to WZ4002 in TD/MET or TL/MET transgenic mouse models (Fig. 3 right, Fig. 4A). TD/MET and TL/MET mice showed significantly less tumor reduction compared to TD and TL mice (−23.2% vs −79.6%; p<0.001, and −17.9% vs −71.2%; p<0.001, respectively, Fig. 4A). To ensure the complete inhibition of EGFR activity, we also treated TD/MET mice with WZ4002 (50mg/kg, daily) along with the anti-EGFR antibody cetuximab (50mg/kg, Q3D) for two weeks. The combination of WZ4002 and cetuximab did not improve the radiographic responses in TD/MET mice (data not shown).
Figure 3. Combination therapy of WZ4002/crizotinib or WZ4002/17-DMAG shows tumor regression in the mice with concurrent hEGFR del19/T790M mutation and MET overexpression.
Tumor-bearing mice were subjected to MRI imaging prior to and after two weeks of treatment with the indicated drugs. Representative MRI images show tumor regression in TD mice but not in TD/MET mice after 2 weeks of WZ4002 treatment. Tumors from either TD or TD/MET mice also do not respond to treatment with single agent crizotinib or 17-DMAG. However, the WZ4002/crizotinib or WZ4002/17-DMAG combinations lead to tumor regression.
Figure 4. Waterfall plots of percentage change in tumor area for individual mice.
Tumor-bearing mice were treated daily with WZ4002 (50mg/kg) (A), crizotinib (20mg/kg or 50mg/kg, as indicated) (B), WZ4002 (50mg/kg) plus crizotinib (20mg/kg or 50mg/kg, as indicated) (C), 17-DMAG (20mg/kg) (D), or WZ4002 (50mg/kg) plus 17-DMAG (20mg/kg) (E). Tumor area was documented by MRI imaging prior to and after two weeks of treatment. Each color represents a different mouse colony; each bar represents the % tumor area change in one mouse.
Inhibition of MET alone does not result in tumor regression in murine lung cancer models with concurrent EGFR mutation and MET overexpression
While lung cancer driven by EGFR TD or TL demonstrated a significant tumor regression upon WZ4002 treatment, hMET overexpression rendered these cancers resistant to the same treatment. In NCI-H820 cells, which express mutant EGFR (E746_T751del, T790M) with the presence of MET amplification, MET inhibition alone was shown to be sufficient to compromise cell growth (16). Based on this finding, we evaluated whether TD/MET and TL/MET mice could respond to therapy with the ATP-competitive small-molecule MET inhibitor crizotinib (PF-02341066), which also inhibits ALK. Tumor-bearing TD/MET or TL/MET mice were treated orally with crizotinib (20mg/kg) daily for 2 weeks. Crizotinib treatment failed to induce radiographic responses, not only in TD and TL mice but also in TD/MET or TL/MET mice (Fig. 3, Supplementary Fig. 4), confirmed by tumor volumetric analyses (Fig. 4B). TD and TD/MET mice were also challenged with the higher dose of 50mg/kg daily for 2 weeks with no improvement in tumor reduction (Fig. 4B) despite the significant dephosphorylation of MET (Supplementary Fig. 1B).
Combined inhibition of EGFR and MET results in significant tumor regression in murine lung cancer models with concurrent EGFR mutation and MET overexpression
Since neither TD/MET nor TL/MET mice responded to single agent EGFR or MET inhibition, we hypothesized that either receptor alone is insufficient to promote TD/MET and TL/MET tumor growth and survival. To test this hypothesis, tumor-bearing TD/MET or TL/MET mice were treated orally with concomitant WZ4002 (50mg/kg) and crizotinib (20mg/kg) daily for 2 weeks. For controls, we treated tumor-bearing TD or TL mice with the same combination therapy schedule. All four mouse models treated with this combination showed significant radiographic responses (Fig. 3, Supplementary Fig. 4) and quantification of tumor burden pre- and post-treatment confirmed the response in TD/MET mice (−69.5%) and TL/MET mice (−74.0%) (Fig. 4C). Taken together with our previous experiments, these results indicate that concomitant treatment with EGFR and MET inhibitors produces greater shrinkage than treatment with either alone in tumors harboring compound EGFR mutations (TD or TL) along with MET overexpression.
HSP90 inhibition potentiates WZ4002 to inhibit tumor growth co-driven by mutant EGFR and MET
Our results show that TD/MET and TL/MET are highly sensitive to combined EGFR and MET inhibition, suggesting co-dependence of these tumors on these receptors. To assess another strategy of depleting cancer cells of EGFR and MET activities, we treated mice with the HSP90 inhibitor 17-DMAG (20mg/kg) daily. We and others have shown that mutant EGFR and MET are clients of HSP90 and are subject to degradation upon HSP90 inhibition (33, 34). We previously demonstrated that TL mice respond to 17-DMAG, but only transiently; tumor regression was observed after 1 week, but substantial tumor regrowth was documented by three weeks (35). Consistent with these results, in the current experiments, we treated TD and TL mice with 17-DMAG for two weeks and did not observe significant radiographic response (Fig. 3 and Supplementary Fig. 4). Similarly, two weeks of 17-DMAG did not produce response in TD/MET and TL/MET mice (Fig. 4D).
Recently, utilizing NCI-H1975 EGFR L858R/T790M xenografts, we have shown that depletion of mutant EGFR upon HSP90 inhibition is brief, lasting only 48 hours before expression is restored, despite persistent intratumoral drug levels (36). We therefore hypothesized that the addition of WZ4002 to 17-DMAG would serve to inhibit re-expressed EGFR, and that the two compounds together may be synergistic. We treated TD, TL, TD/MET, and TL/MET mice with the combination of WZ4002 (50mg/kg, daily) and 17-DMAG (20mg/kg, daily) for two weeks. For TD or TL mice, combination therapy did not afford advantage over treatment with WZ4002 alone by MRI analyses (Fig. 3 and Supplementary Fig. 4), presumably because of the substantial single-agent activity of WZ4002 in these models. However, significant reductions in tumor volume were observed in TD/MET and TL/MET mice with the combination regimen (Fig. 4E) and the reductions in tumor size post-treatment were comparable to those observed with combined WZ4002 and crizotinib therapy (Fig. 4C).
To extend our findings to human lung cancer cells, we assessed the efficacy of similar treatments in mice bearing xenografts of gefitinib-resistant MET amplified HCC827 cells (HCC827GR6) (19) engineered to ectopically express EGFR E746_A750del/T790M (Supplementary Fig. 5). Here, partial tumor response was observed after monotherapy with 17-DMAG or WZ4002; however, the combination was more efficacious than either agent alone in suppressing tumor growth (Supplementary Fig. 5).
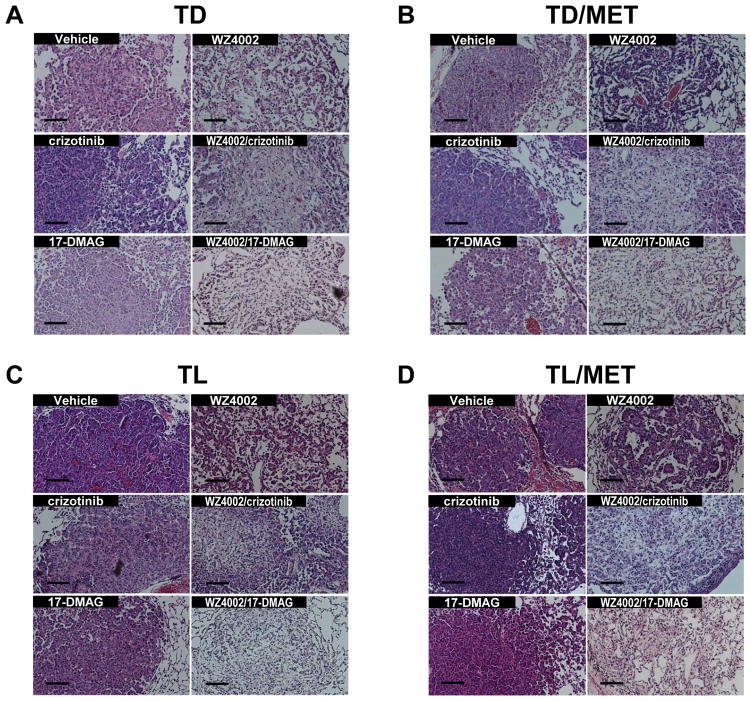
Histological confirmation of radiographic responses to combination treatments
TD/MET and TL/MET tumors responded to combinations of WZ4002 and crizotinib or WZ4002 and 17-DMAG within two weeks. In order to confirm radiographic responses, we examined H&E stains from treated tumor. In TD mice, single agent crizotinib or 17-DMAG failed to show reduction in tumor cell content, while there was noticeable response to WZ4002 (Fig. 5A), consistent with our previous data (18). In contrast, single agent WZ4002 (as well as crizotinib or 17-DMAG) failed to show a significant decrease in tumor cell content in the TD/MET model (Fig. 5B); however, in this model, tumor cell content was markedly decreased after combination therapy with WZ4002 and crizotinib or WZ4002 and 17-DMAG, with fibrosis evident in the tumor nests (Fig. 5B). Identical results were obtained in TL/MET mice, where the superiority of combination treatment was also evident (Fig. 5C and 5D).
Figure 5. H&E staining of lung tumors demonstrates that combination treatments are more efficacious that individual treatments against tumors harboring compound EGFR mutations and MET overexpression.
Representative images of H&E staining of lung tumors from TD mice (A), TD/MET mice (B), TL mice (C), and TL/MET mice (D). All mice were sacrificed for pathological analysis after 2 weeks of treatment with vehicle, WZ4002, crizotinib, 17-DMAG, WZ4002/crizotinib, or WZ4002/17-DMAG. Scale bars, 100μm.
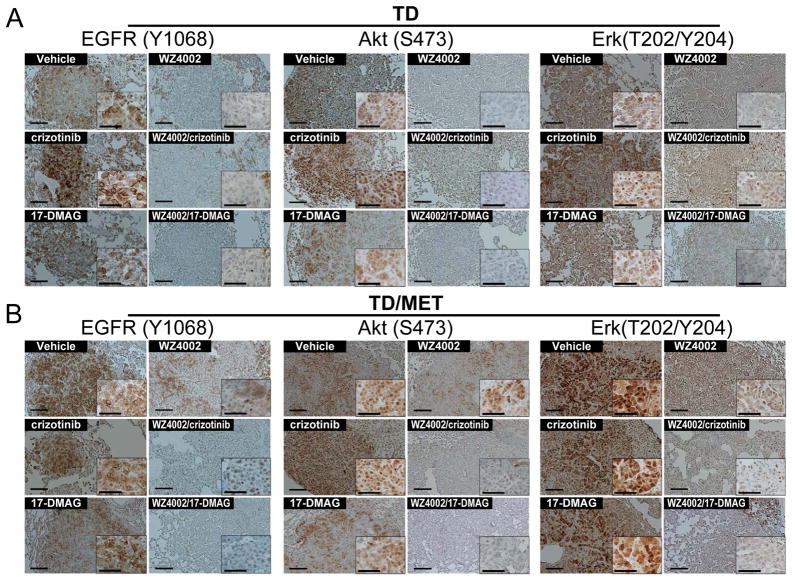
Combination therapies promote efficient growth inhibition of tumors with concurrent expression of mutant EGFR and MET by suppressing both PI3-K and MAPK pathways
Since PI3-K and MAPK pathways are downstream of mutant EGFR and MET (2, 3, 6, 13, 25), we used phospho-Akt and phospho-Erk as pharmacodynamic markers to evaluate the efficacies of targeted therapies in the mouse models. Mice were treated over 24 hours with 2 doses of vehicle, WZ4002 alone, crizotinib alone, crizotinib/WZ4002, or WZ4002/17-DMAG prior to sacrifice and harvesting of tumors for immunohistochemical analysis. In TD mice, WZ4002 alone resulted in EGFR dephosphorylation (Fig. 6A, left) and suppressed both Akt and Erk phosphorylation, while crizotinib treatment alone failed to suppress Akt and Erk phosphorylation (Figure 6A middle and right panels). In contrast, WZ4002 alone failed to suppress phospho-Akt and phospho-Erk signals in TD/MET mice (Fig. 6B, middle and right panels) even though considerable suppression of EGFR phosphorylation was achieved (Fig. 6B, left).
Figure 6. IHC staining of lung tumors shows combination treatments are more efficacious than individual agents for suppression of critical signaling pathways in mice with lung cancers harboring EGFR T790M mutation and MET overexpression.
IHC for phospho-EGFR (left), phospho-Akt (S473, middle), and phospho-Erk (T202/Y204, right) of lung tumors from (A) TD or (B) TD/MET mice. Mice were treated with the indicated drugs (single agent or combination) for 2 doses over 24 hours and sacrificed 2 hours following the second dose, and lung sections were stained with indicated antibodies. Photos shown are representative fields in each group in low and high magnification. Scale bars in the main images and in the insets indicate 100μm and 50μm, respectively.
Crizotinib alone did not completely suppress phosphorylation of EGFR, Akt or Erk in either the TD or the TD/MET models (Fig. 6A and 6B). In contrast, combination treatment with WZ4002 and crizotinib robustly suppressed expression of phospho-EGFR, phospho-Akt and phospho-Erk in both of these mouse models (Fig. 6A and 6B). Similarly, the WZ4002/17-DMAG combination was also efficacious and substantially reduced phosphorylation of components of the signaling cascades dramatically in both TD and TD/MET mice (Fig. 6A and 6B).
To confirm the results from IHC, tumor lysates from TD and TD/MET mice similarly treated with vehicle, WZ4002 alone, crizotinib alone, crizotinib/WZ4002 or WZ4002/17-DMAG were subjected to Western blot (Supplementary Fig. 6). In tumors from TD mice, WZ4002 treatment alone was sufficient to downregulate phospho-EGFR, phospho-Akt, and phospho-Erk while single-agent WZ4002 or crizotinib alone was not sufficient to inhibit the same phosphorylation events in TD/MET mice. In agreement with the immunohistochemical results, (Fig. 6), Western blotting confirms that only the WZ4002/crizotinib and WZ4002/17-DMAG combinations can suppress the phosphorylation of EGFR, Akt, and Erk in tumors from TD/MET mice.
DISCUSSION
To date, the two most common mechanisms of acquired resistance to gefitinib and erlotinib therapies are development of a secondary gatekeeper mutation T790M (~50%) and a focal amplification of MET (~5–20%, (6, 19, 21)). According to several studies, anywhere from 5–30% of instances of MET amplification occur concurrently with T790M in patients (4, 6, 16, 19, 22, 23, 37). It remains unclear if EGFR T790M and amplified-MET coexist in a single tumor cell or whether these somatic genetic changes exist in distinct cells within the same tumor mass. However, in vivo models suggest that they can coexist in a single cell, since they are found naturally occurring together in the NCI-H820 cell line (16, 35).
Previous in vitro studies suggested that MET inhibition or MET depletion alone could suppress the growth and compromise the viability of the NCI-H820 cell line, suggesting that the presence of MET amplification is dominant and supersedes any dependence on EGFR carrying compound mutation with T790M. To test this further, we modeled similar genetic changes in vivo. Here, we have demonstrated that mouse lung adenocarcinomas with concurrent TD or TL along with MET amplification clearly depend on both receptors, and that treatment with individual EGFR or MET inhibitors (i.e. WZ4002 or crizotinib) is ineffective.
These results are different from those observed in the NCI-H820 model (16). However our experimental results in vivo are in line with the original report describing MET-amplified EGFR TKI-resistant cells as sensitive to concomitant suppression of EGFR and MET (6). The discrepancy may be explained by differences in how these models were derived or other differences in their underlying genetic composition that are yet to be defined.
Although our mouse model facilitated the evaluation of drugs designed for human kinases in the presence of human transgenes, these models carry some limitations since they do not completely simulate the human disease. First, these models might not express MET at the level observed in human EGFR TKI-resistant tumors with MET amplification. However, since most EGFR TKI-resistant tumors are analyzed for MET amplification but not for MET overexpression, the exact level of MET expression required in these models is unclear. Second, our mouse model does not account for the impact of HGF on overexpressed MET. However, it has been demonstrated that overexpression of HGF is able to confer resistance in vivo that is also overcome with simultaneous inhibition of both EGFR and MET (6).
Despite these caveats, we propose that simultaneous inhibition of mutant EGFR carrying T790M and MET is likely necessary in tumors in which both genetic abnormalities are observed. Our EGFR/MET mutant mouse models provide novel platforms to preclinically evaluate compounds in vivo to suppress EGFR and MET signaling simultaneously. Our data suggest that the combination of an EGFR T790M mutant-selective kinase inhibitor such as WZ4002, combined with a MET inhibitor such as crizotinib, should be a high priority once T790M mutant-selective compounds are evaluated on their own.
EGFR and MET are both client proteins of HSP90 (33–35, 38). To date, however, HSP90 inhibitors have had limited efficacy in our preclinical TD and TL models, where regressions are short-lived, as well as in clinical trials in the EGFR mutant population (39, 40). This may be in part because of very transient suppression of the EGFR mutant client protein upon HSP90 inhibition (36). It was therefore not a surprise that 17-DMAG alone performed poorly in the TD/MET and TL/MET models. Of note, it is possible that regression occurred over the first week of treatment that we did not capture with an assessment only at the 2-week mark. However, the combination of 17-DMAG and WZ4002 did cause substantial regression in these models, presumably because WZ4002 was capable of inhibiting the activity of EGFR TD and TL after expression re-emerges. Of note, these results also suggest that HSP90 inhibition is capable of prolonged suppression of MET expression, so that co-depletion of both activities is accomplished by the combination. Further studies will be required to assess the relative sensitivities of MET and mutant EGFR to degradation in response HSP90 inhibition. Of note, the combination of WZ4002 and 17-DMAG was similar to that of WZ4002 and crizotinib in the clearance of TD/MET and TL/MET tumor cells, as assessed by H&E staining (Fig. 6 and Supplementary Fig. 6).
Previous studies suggested that MET can couple with ERBB3 to activate downstream signals mediated by Akt that bypass the inhibited EGFR (6). Additionally, MET could activate PI3K pathway through Gab1 (19, 41). Correspondingly, single agent WZ4002 didn’t significantly diminish phospho-Akt in the TD/MET mouse model (Fig. 6B and Supplementary Fig.6), suggesting MET maintains Akt activity in our in vivo model when EGFR signaling is inhibited. Therefore, combination therapies (WZ4002 and crizotinib or WZ4002 and 17-DMAG) most efficiently suppressed PI3-K and MAPK signaling in all the models tested (Fig. 6B and Supplementary Fig.6). The suppression of critical downstream signaling resulted in radiographic and histological responses overcoming resistance to EGFR inhibition conferred by MET overexpression.
In conclusion, we have developed in vivo models of intrinsic resistance to reversible EGFR TKIs conferred by both EGFR mutants containing T790M and MET overexpression in order to identify efficacious combination therapies against these genetically defined lung cancers. Our data support the design of appropriate combination clinical trials for patients with EGFR mutant NSCLCs carrying compound TKI-resistance mechanisms.
Supplementary Material
Acknowledgments
This work is supported by NIH grants CA122794, CA140594, CA163896 and CA141576, as well as grants from United Against Lung Cancer, American Lung Association, and the Susan Spooner Research Fund, all to K.K.W. K.K.W. and G.I.S. were supported by NIH grant P50 CA090578 [Dana-Farber/Harvard Cancer Center Specialized Program of Research Excellence (SPORE) in Lung Cancer]. T.S. was supported by a DF/HCC Lung SPORE Career Development Award.
Footnotes
On behalf of all authors on this manuscript, following conflicts of interest that need to be disclosed. All authors have completed separate conflict of interest forms and we have no other conflicts of interest to report.
Kwok-Kin Wong
Conflict of interest disclosure statement:
Drs. Jänne and Engelman have following ownership and consulting relationship.
Dr. Jänne:
Consultant/Advisory Board
(Minor $10,000 or less)
Astra Zeneca, Boehringher Ingelheim, Pfizer, Roche, Genentech.
(Major $10,000 or more)
Lab Corp
Dr. Engelman:
Ownership
(Minor $10,000 or less)
Ventanan/Roche
Consultant/Advisory Board
(Minor $10,000 or less)
Amgen, Astra Zeneca, Bristol Myers Squibb, Genentech, Glaxo Smith Kline, Roche, Sanofi Aventis
References
- 1.Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350:2129–39. doi: 10.1056/NEJMoa040938. [DOI] [PubMed] [Google Scholar]
- 2.Paez JG, Janne PA, Lee JC, Tracy S, Greulich H, Gabriel S, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–500. doi: 10.1126/science.1099314. [DOI] [PubMed] [Google Scholar]
- 3.Sordella R, Bell DW, Haber DA, Settleman J. Gefitinib-sensitizing EGFR mutations in lung cancer activate anti-apoptotic pathways. Science. 2004;305:1163–7. doi: 10.1126/science.1101637. [DOI] [PubMed] [Google Scholar]
- 4.Chen HJ, Mok TS, Chen ZH, Guo AL, Zhang XC, Su J, et al. Clinicopathologic and molecular features of epidermal growth factor receptor T790M mutation and c-MET amplification in tyrosine kinase inhibitor-resistant Chinese non-small cell lung cancer. Pathol Oncol Res. 2009;15:651–8. doi: 10.1007/s12253-009-9167-8. [DOI] [PubMed] [Google Scholar]
- 5.Engelman JA, Mukohara T, Zejnullahu K, Lifshits E, Borras AM, Gale CM, et al. Allelic dilution obscures detection of a biologically significant resistance mutation in EGFR-amplified lung cancer. J Clin Invest. 2006;116:2695–706. doi: 10.1172/JCI28656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Engelman JA, Zejnullahu K, Mitsudomi T, Song Y, Hyland C, Park JO, et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science. 2007;316:1039–43. doi: 10.1126/science.1141478. [DOI] [PubMed] [Google Scholar]
- 7.Kobayashi S, Ji H, Yuza Y, Meyerson M, Wong KK, Tenen DG, et al. An alternative inhibitor overcomes resistance caused by a mutation of the epidermal growth factor receptor. Cancer Res. 2005;65:7096–101. doi: 10.1158/0008-5472.CAN-05-1346. [DOI] [PubMed] [Google Scholar]
- 8.Kobayashi S, Shimamura T, Monti S, Steidl U, Hetherington CJ, Lowell AM, et al. Transcriptional profiling identifies cyclin D1 as a critical downstream effector of mutant epidermal growth factor receptor signaling. Cancer Res. 2006;66:11389–98. doi: 10.1158/0008-5472.CAN-06-2318. [DOI] [PubMed] [Google Scholar]
- 9.Sequist LV, Waltman BA, Dias-Santagata D, Digumarthy S, Turke AB, Fidias P, et al. Genotypic and Histological Evolution of Lung Cancers Acquiring Resistance to EGFR Inhibitors. Sci Transl Med. 2011;3:75ra26. doi: 10.1126/scitranslmed.3002003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yun CH, Mengwasser KE, Toms AV, Woo MS, Greulich H, Wong KK, et al. The T790M mutation in EGFR kinase causes drug resistance by increasing the affinity for ATP. Proc Natl Acad Sci U S A. 2008;105:2070–5. doi: 10.1073/pnas.0709662105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Engelman JA, Zejnullahu K, Gale CM, Lifshits E, Gonzales AJ, Shimamura T, et al. PF00299804, an irreversible pan-ERBB inhibitor, is effective in lung cancer models with EGFR and ERBB2 mutations that are resistant to gefitinib. Cancer Res. 2007;67:11924–32. doi: 10.1158/0008-5472.CAN-07-1885. [DOI] [PubMed] [Google Scholar]
- 12.Li D, Ambrogio L, Shimamura T, Kubo S, Takahashi M, Chirieac LR, et al. BIBW2992, an irreversible EGFR/HER2 inhibitor highly effective in preclinical lung cancer models. Oncogene. 2008;27:4702–11. doi: 10.1038/onc.2008.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li D, Shimamura T, Ji H, Chen L, Haringsma HJ, McNamara K, et al. Bronchial and peripheral murine lung carcinomas induced by T790M-L858R mutant EGFR respond to HKI-272 and rapamycin combination therapy. Cancer Cell. 2007;12:81–93. doi: 10.1016/j.ccr.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 14.Regales L, Gong Y, Shen R, de Stanchina E, Vivanco I, Goel A, et al. Dual targeting of EGFR can overcome a major drug resistance mutation in mouse models of EGFR mutant lung cancer. J Clin Invest. 2009;119:3000–10. doi: 10.1172/JCI38746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sequist LV, Besse B, Lynch TJ, Miller VA, Wong KK, Gitlitz B, et al. Neratinib, an irreversible pan-ErbB receptor tyrosine kinase inhibitor: results of a phase II trial in patients with advanced non-small-cell lung cancer. J Clin Oncol. 2010;28:3076–83. doi: 10.1200/JCO.2009.27.9414. [DOI] [PubMed] [Google Scholar]
- 16.Bean J, Brennan C, Shih JY, Riely G, Viale A, Wang L, et al. MET amplification occurs with or without T790M mutations in EGFR mutant lung tumors with acquired resistance to gefitinib or erlotinib. Proc Natl Acad Sci U S A. 2007;104:20932–7. doi: 10.1073/pnas.0710370104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong KK. HKI-272 in non small cell lung cancer. Clin Cancer Res. 2007;13:s4593–6. doi: 10.1158/1078-0432.CCR-07-0369. [DOI] [PubMed] [Google Scholar]
- 18.Zhou W, Ercan D, Chen L, Yun CH, Li D, Capelletti M, et al. Novel mutant-selective EGFR kinase inhibitors against EGFR T790M. Nature. 2009;462:1070–4. doi: 10.1038/nature08622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Turke AB, Zejnullahu K, Wu YL, Song Y, Dias-Santagata D, Lifshits E, et al. Preexistence and clonal selection of MET amplification in EGFR mutant NSCLC. Cancer Cell. 2010;17:77–88. doi: 10.1016/j.ccr.2009.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yano S, Wang W, Li Q, Matsumoto K, Sakurama H, Nakamura T, et al. Hepatocyte growth factor induces gefitinib resistance of lung adenocarcinoma with epidermal growth factor receptor-activating mutations. Cancer Res. 2008;68:9479–87. doi: 10.1158/0008-5472.CAN-08-1643. [DOI] [PubMed] [Google Scholar]
- 21.Arcila ME, Oxnard GR, Nafa K, Riely GJ, Solomon SB, Zakowski MF, et al. Rebiopsy of lung cancer patients with acquired resistance to EGFR inhibitors and enhanced detection of the T790M mutation using a locked nucleic acid-based assay. Clin Cancer Res. 2011;17:1169–80. doi: 10.1158/1078-0432.CCR-10-2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jiang SX, Yamashita K, Yamamoto M, Piao CJ, Umezawa A, Saegusa M, et al. EGFR genetic heterogeneity of nonsmall cell lung cancers contributing to acquired gefitinib resistance. Int J Cancer. 2008;123:2480–6. doi: 10.1002/ijc.23868. [DOI] [PubMed] [Google Scholar]
- 23.Onitsuka T, Uramoto H, Nose N, Takenoyama M, Hanagiri T, Sugio K, et al. Acquired resistance to gefitinib: the contribution of mechanisms other than the T790M, MET, and HGF status. Lung Cancer. 2010;68:198–203. doi: 10.1016/j.lungcan.2009.05.022. [DOI] [PubMed] [Google Scholar]
- 24.Godin-Heymann N, Bryant I, Rivera MN, Ulkus L, Bell DW, Riese DJ, 2nd, et al. Oncogenic activity of epidermal growth factor receptor kinase mutant alleles is enhanced by the T790M drug resistance mutation. Cancer Res. 2007;67:7319–26. doi: 10.1158/0008-5472.CAN-06-4625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ji H, Li D, Chen L, Shimamura T, Kobayashi S, McNamara K, et al. The impact of human EGFR kinase domain mutations on lung tumorigenesis and in vivo sensitivity to EGFR-targeted therapies. Cancer Cell. 2006;9:485–95. doi: 10.1016/j.ccr.2006.04.022. [DOI] [PubMed] [Google Scholar]
- 26.Fisher GH, Wellen SL, Klimstra D, Lenczowski JM, Tichelaar JW, Lizak MJ, et al. Induction and apoptotic regression of lung adenocarcinomas by regulation of a K-Ras transgene in the presence and absence of tumor suppressor genes. Genes Dev. 2001;15:3249–62. doi: 10.1101/gad.947701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perl AK, Zhang L, Whitsett JA. Conditional expression of genes in the respiratory epithelium in transgenic mice: cautionary notes and toward building a better mouse trap. Am J Respir Cell Mol Biol. 2009;40:1–3. doi: 10.1165/rcmb.2008-0011ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Engelman JA, Chen L, Tan X, Crosby K, Guimaraes AR, Upadhyay R, et al. Effective use of PI3K and MEK inhibitors to treat mutant Kras G12D and PIK3CA H1047R murine lung cancers. Nat Med. 2008;14:1351–6. doi: 10.1038/nm.1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ji H, Ramsey MR, Hayes DN, Fan C, McNamara K, Kozlowski P, et al. LKB1 modulates lung cancer differentiation and metastasis. Nature. 2007;448:807–10. doi: 10.1038/nature06030. [DOI] [PubMed] [Google Scholar]
- 30.Ji H, Zhao X, Yuza Y, Shimamura T, Li D, Protopopov A, et al. Epidermal growth factor receptor variant III mutations in lung tumorigenesis and sensitivity to tyrosine kinase inhibitors. Proc Natl Acad Sci U S A. 2006;103:7817–22. doi: 10.1073/pnas.0510284103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li D, Ji H, Zaghlul S, McNamara K, Liang MC, Shimamura T, et al. Therapeutic anti-EGFR antibody 806 generates responses in murine de novo EGFR mutant-dependent lung carcinomas. J Clin Invest. 2007;117:346–52. doi: 10.1172/JCI30446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sun Y, Schmidt NO, Schmidt K, Doshi S, Rubin JB, Mulkern RV, et al. Perfusion MRI of U87 brain tumors in a mouse model. Magn Reson Med. 2004;51:893–9. doi: 10.1002/mrm.20029. [DOI] [PubMed] [Google Scholar]
- 33.Shimamura T, Lowell AM, Engelman JA, Shapiro GI. Epidermal growth factor receptors harboring kinase domain mutations associate with the heat shock protein 90 chaperone and are destabilized following exposure to geldanamycins. Cancer Res. 2005;65:6401–8. doi: 10.1158/0008-5472.CAN-05-0933. [DOI] [PubMed] [Google Scholar]
- 34.Shimamura T, Shapiro GI. Heat shock protein 90 inhibition in lung cancer. J Thorac Oncol. 2008;3:S152–9. doi: 10.1097/JTO.0b013e318174ea3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shimamura T, Li D, Ji H, Haringsma HJ, Liniker E, Borgman CL, et al. Hsp90 inhibition suppresses mutant EGFR-T790M signaling and overcomes kinase inhibitor resistance. Cancer Res. 2008;68:5827–38. doi: 10.1158/0008-5472.CAN-07-5428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shimamura T, Borgman C, Chen L, Li D, Foley K, Sang J, et al. A4679: The novel Hsp90 inhibitor STA-9090 has potent anticancer activity in in vitro and in vivo models of lung cancer. Proc Am Asssoc Cancer Res. 2009:A4679. [abstr] [Google Scholar]
- 37.Costa DB, Nguyen KS, Cho BC, Sequist LV, Jackman DM, Riely GJ, et al. Effects of erlotinib in EGFR mutated non-small cell lung cancers with resistance to gefitinib. Clin Cancer Res. 2008;14:7060–7. doi: 10.1158/1078-0432.CCR-08-1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang S, Pashtan I, Tsutsumi S, Xu W, Neckers L. Cancer cells harboring MET gene amplification activate alternative signaling pathways to escape MET inhibition but remain sensitive to Hsp90 inhibitors. Cell Cycle. 2009;8:2050–6. doi: 10.4161/cc.8.13.8861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sequist LV, Gettinger S, Senzer NN, Martins RG, Janne PA, Lilenbaum R, et al. Activity of IPI-504, a novel heat-shock protein 90 inhibitor, in patients with molecularly defined non-small-cell lung cancer. J Clin Oncol. 2010;28:4953–60. doi: 10.1200/JCO.2010.30.8338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wong KK, Koczywas J, Goldman JW, Paschold EH, Horn L, Lufkin JM, et al. An open-label phase II study of the Hsp90 inhibitor ganetespib (STA-9090) as monotherapy in patients with advanced non-small cell lung cancer. J Clin Oncol. 2011;29(15S):A7500. [abstr] [Google Scholar]
- 41.Fan S, Ma YX, Gao M, Yuan RQ, Meng Q, Goldberg ID, et al. The multisubstrate adapter Gab1 regulates hepatocyte growth factor (scatter factor)-c-Met signaling for cell survival and DNA repair. Mol Cell Biol. 2001;21:4968–84. doi: 10.1128/MCB.21.15.4968-4984.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.