Abstract
Recent studies suggest that people living with HIV with lower viral load are at reduced risk for transmitting HIV to their sexual partners. As information about the association between viral load and risk for HIV transmission disseminates throughout high-risk communities, viral load discussions may be used more often as a risk reduction strategy. The overall purpose of this study was to determine the frequency of viral load discussions and unprotected anal intercourse in primary and casual sexual partnerships among men who have sex with men (MSM). An online survey was completed by 326 MSM (82% Caucasian, 62% college educated, 7% HIV-positive or thought they were HIV positive) in January, 2011. Results showed that viral load discussions occurred in 93% of primary partnerships in which at least one partner was HIV-positive; UAI was reported with 46% of all primary partners and 25% of serodiscordant primary partners with whom viral load was discussed. Viral load discussions occurred in 53% of the three most recent sexual episodes with casual sex partners with whom participants had either sex with once or had sex with multiple times in the past 3 months. UAI was more common in sexual encounters with casual sex partners when viral load was not discussed than when viral load was discussed (75% v. 56% of encounters). The finding that casual sexual episodes that did not include viral load discussions had a higher percentage of UAI than those that did include viral load discussions suggests either that men who do not discuss viral load may be higher risk-takers than men who do, or that the former are less adept at negotiating safer sex with casual sex partners than men who do discuss viral load. More research is needed to understand the role of viral load discussions in negotiating sexual activities among MSM.
Introduction
Studies suggest that people living with HIV (PLWH) with lower viral load are at reduced risk for transmitting HIV to their sexual partners (Cohen, et al., 2011; Montaner, et al., 2011). As information about the association between viral load and risk for HIV transmission disseminates throughout high-risk communities, viral load discussions may be used more often as a risk reduction strategy.
Beliefs about viral load have been shown across a number of studies to be associated with sexual risk behavior among groups at risk for HIV acquisition or transmission. In a study of 57 HIV-positive men who have sex with men (MSM), perceived viral load was associated with higher risk behaviors with steady partners, although actual viral load was not (Stolte, de Wit, van Eeden, Coutinho, & Dukers, 2004). A second study showed that belief among HIV-positive (n=536) and HIV-negative (n=102) MSM that they or their sex partner, respectively, had an undetectable viral load was associated with higher rates of unprotected anal intercourse (UAI; (Prestage, et al., 2009). Finally, a recent study of 212 HIV-positive Dutch MSM found that 57% considered their viral load into in their decision to have UAI with a casual partner, and 64% used such information in their decisions to have UAI with a steady partner (van den Boom, Davidovich, Witlox & Stolte, 2011).
Although these studies provide evidence that viral load beliefs may be associated with sexual risk practices, few (if any) studies have examined whether viral load discussions are occurring among sexual episodes among MSM in which at least one partner is HIV-positive. Therefore, we conducted this exploratory study to answer the following questions: How common are viral load discussions with primary and casual sexual partners among a US sample of MSM? How common is unprotected anal intercourse (UAI) with primary and casual partners in the context of viral load discussions?
Method
An online survey was completed by 326 MSM in January, 2011. The primary purpose of the survey was to investigate the association between men’s attitudes and practices about pornography and their sexual risk behavior. Inclusion criteria were: 18 years of age or older, self-reported male identity, having had sex with another man in the past 5 years, and residing in the United States or one of its territories. Participants entered the study by clicking on banner advertisements placed on 148 websites that target gay and bisexual men. Once men completed the eligibility screening questions, those who were eligible for the study viewed a series of consent webpages, and were allowed to begin the survey immediately.
Sexual behavior in the past 3 months was assessed for three partner types: a) frequency of UAI with a primary partner (defined as “…a regular sex partner such as a boyfriend, husband, domestic partner that you have been in a relationship with for at least three months”); b) UAI with the three most recent episodes with casual partners they had sex with only once (described as “1-time casual partner” below); and c) UAI with the three most recent episodes with casual partners they had sex with more than once (described as “repeat casual partner” below). In sexual partnerships in which at least one partner reported being HIV-positive, men were asked whether viral load discussions took place (e.g., “Has [sexual partner name] ever told you about the results of any viral load test (that is, a test that measures how much HIV is present in his body) he has had?”). For HIV-positive participants, viral load discussion questions were only asked if they reported that they had discussed ART with their sexual partner. All procedures and materials were approved by the University of Minnesota Institutional Review Board.
Results
Demographic Characteristics
The mean age of participants was 32 years, and most identified as Caucasian (82%), single (65%), and college educated (62%). For the purpose of analysis, men who reported being HIV-negative (n=270), thought they were HIV-negative (n=32), or unsure of their HIV status (n=2) were collapsed into one category (“HIV-negative); men who self-reported as HIV-positive (n=20) or thought they were HIV-positive (n=2) were collapsed into a second category.
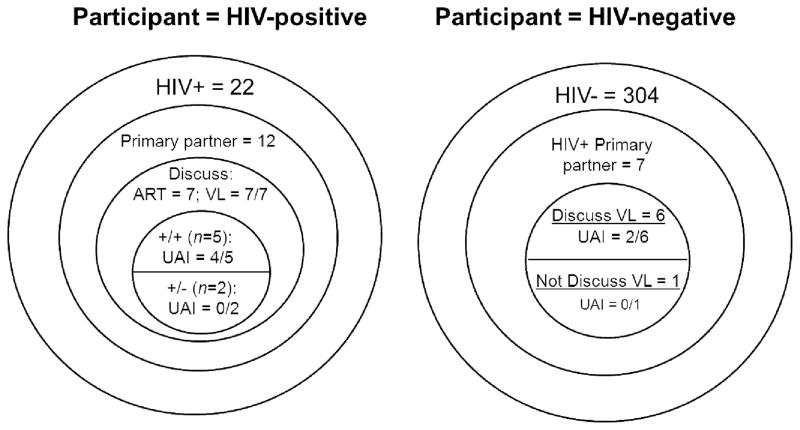
Viral load discussions with primary partners (see Figure 1)
Figure 1.
Viral load discussions and UAI with primary partner by HIV status of participant
Of the 12 HIV-positive men who reported a primary partner, seven reported discussing being on ART and their viral load with their partner. Five of the seven men who discussed their viral load were in seroconcordant primary relationships, and four of those men reported UAI. Neither of the two HIV-positive men in serodiscordant primary relationships who had discussed viral load with their partner reported UAI.
Seven HIV-negative men reported being in a serodiscordant primary relationship. Among those seven men, six reported having viral load discussions with their partner and, of those, two reported UAI. The one HIV-negative participant who was in a serodiscordant primary partnership who did not discuss viral load reported no UAI.
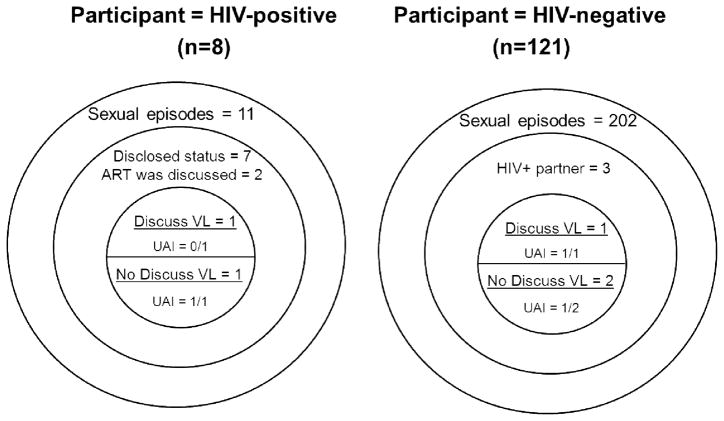
Viral load discussions with 1-time casual partners (see Figure 2)
Figure 2.
Viral load discussions and UAI in sexual episodes with casual partner with whom participants had sex with only once in the past 3 months by HIV status of participant
Eight HIV-positive participants reported on 11 sexual episodes with casual partners they had sex with only once. Although men reported disclosing their HIV status in seven of those sexual episodes, ART was discussed in only two episodes. The one sexual episode in which ART and viral load was discussed did not include UAI. In comparison, UAI was reported in the one sexual episode in which ART was discussed, but viral load was not.
One hundred twenty-one HIV-negative MSM reported 202 sexual episodes with causal partners they had sex with only once. Of those, only three episodes were reported to have occurred with HIV-positive partners. No UAI was reported in the one sexual episode in which viral load was discussed. In comparison, UAI was reported in one of the two episodes in which viral load was not discussed.
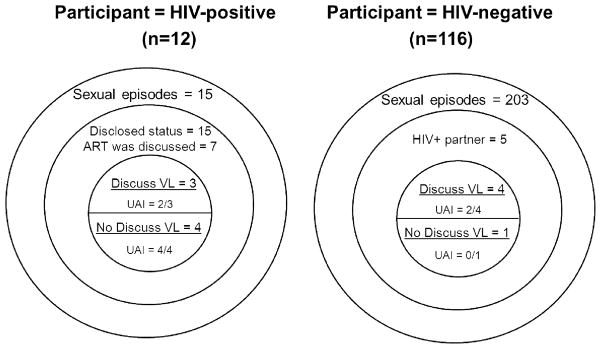
Viral load discussions with repeat casual partners (see Figure 3)
Figure 3.
Viral load discussions and UAI in sexual episodes with casual partner with whom participants had sex with more than once in the past 3 months by HIV status of participant
Twelve HIV-positive participants reported on 15 sexual episodes with casual partners they had sex with more than once on the past three months. Although men reported disclosing their HIV status in all 15 of those episodes, ART was discussed in only seven of those episodes. Two of the three sexual episodes in which viral load was discussed included UAI. In comparison, all four episodes in which viral load was not discussed included UAI.
One hundred sixteen HIV-negative MSM reported 203 sexual episodes with causal partners they had sex with more than once. Of those, only five episodes were reported to have occurred with HIV-positive partners. UAI was reported in two of the four sexual episodes in which viral load discussed. In comparison, no UAI was reported to have taken place in the one episode in which viral load was not discussed.
Discussion
Viral load discussions nearly always (with 93% of partners) occurred in primary partnerships in which at least one partner was HIV-positive. When viral load discussions took place with primary partners, UAI occurred with 46% of all primary partners and 25% of serodiscordant primary partners in the past three months. In comparison, viral load discussions were less common in sexual encounters with casual sex partners. Viral load discussions took place in 53% of the three most recent sexual episodes with casual sex partners with whom participants either had sex with once or had sex with multiple times in the past three months. UAI was more common in sexual encounters with casual sex partners when viral load was not discussed than when viral load was discussed (75% v. 56% of encounters).
There are a number of limitations to this study. First, all data are self-reported, and subject to recall and social desirability biases. Second, HIV-positive participants were only asked viral load discussion questions if they reported having discussions about ART with their partners. It is possible that viral load discussions took place in the absence of ART discussions. Third, we did not collect information on whether the HIV-positive partner’s viral load was undetectable or detectable, which may play an important role in men’s decisions about condom use. Finally, few men reported serodiscordant primary partners or sexual encounters with serodiscordant casual partners, and therefore the results are based on a relatively small number of cases. Future studies may benefit from a larger sample of MSM or enrolling more HIV-positive MSM.
In sum, viral load discussions were not common in this sample of MSM, although that may be due to the low number of participants reporting serodiscordant primary and casual partners. The finding that casual sexual episodes that did not include viral load discussions had a higher percentage of UAI than those that did include viral load discussions suggests either that men who do not discuss viral load may be higher risk-takers than men who do, or that the former are less adept at negotiating safer sex with casual sex partners than men who do discuss viral load. Greater understanding of the effects of serostatus disclosure, beliefs about viral load, and viral load discussions between MSM at risk for acquiring or transmitting HIV is needed to inform intervention targeting high risk MSM.
Acknowledgments
This grant was funded by the National Institute of Mental Health (#1R01MH087231-01). Portions of this research were presented at the 10th Annual AIDS Impact conference, Santa Fe, NM. We wish to thank the participants for their time.
References
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, Hakim J, Kumwenda J, Grinsztejn B, Pilotto JH, Godbole SV, Mehendale S, Chariyalertsak S, Santos BR, Mayer KH, Hoffman IF, Eshleman SH, Piwowar-Manning E, Wang L, Makhema J, et al. Prevention of HIV-1 infection with early antiretroviral therapy. NEJM. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montaner JSG, Lima VD, Barrios R, Yip B, Wood E, Kerr T, et al. Association of highly active antiretroviral therapy coverage, population viral load, and yearly new HIV diagnoses in British Columbia, Canada: a population-based study. The Lancet. 2011;376:532–539. doi: 10.1016/S0140-6736(10)60936-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prestage G, Mao L, Kippax S, Jin F, Hurley M, Grulich A, et al. Use of Viral Load to Negotiate Condom Use Among Gay Men in Sydney, Australia. AIDS and Behavior. 2009;13(4):645–651. doi: 10.1007/s10461-009-9527-0. [DOI] [PubMed] [Google Scholar]
- Stolte IG, de Wit JB, van Eeden A, Coutinho RA, Dukers NH. Perceived viral load, but not actual HIV-1-RNA load, is associated with sexual risk behaviour among HIV-infected homosexual men. AIDS. 2004;18(14):1943–1949. doi: 10.1097/00002030-200409240-00010. [DOI] [PubMed] [Google Scholar]
- van den Boom W, Davidovich U, Witlox R, Stolte I. Frequent use of viral sorting by HIV-positive MSM: the consideration of viral load when deciding to engage in unprotected anal intercourse with HIV-positive and HIV-negative partners. Presented at 10th Annual Aids Impact conference; Santa Fe, New Mexico. September 14, 2011.2011. [Google Scholar]