Abstract
Background
We have developed an intradiscal pulsed radiofrequency (Disc PRF) technique, using Diskit II® needles (NeuroTherm, Wilmington, MA, USA), as a minimally invasive treatment option for chronic discogenic low back pain (LBP). The purpose of this study was to compare the representative outcomes of Disc PRF and Intradiscal Electrothermal Therapy (IDET) in terms of pain relief and reduction of disability.
Methods
Thirty-one patients with chronic discogenic LBP who underwent either Disc PRF (n = 15) or IDET (n = 16) were enrolled in the study. A Diskit II® needle (15-cm length, 20-gauge needle with a 20-mm active tip) was placed centrally in the disc. PRF was applied for 15 min at a setting of 5 × 50 ms/s and 60 V. The pain intensity score on a 0-10 numeric rating scale (NRS) and the Roland-Morris Disability Questionnaire (RMDQ) were assessed pretreatment and at 1, 3, and 6 months post-treatment.
Results
The mean NRS was significantly improved from 7.2 ± 0.6 pretreatment to 2.5 ± 0.9 in the Disc PRF group, and from 7.5 ± 1.0 to 1.7 ± 1.5 in the IDET group, at the 6-month follow-up. The mean RMDQ also showed significant improvement in both the Disc PRF group and the IDET group at the 6-month follow-up. There were no significant differences in the pretreatment NRS and RMDQ scores between the groups.
Conclusions
Disc PRF appears to be an alternative to IDET as a safe, minimally invasive treatment option for patients with chronic discogenic LBP.
Keywords: intervertebral disc degeneration, Intradiscal Electrothermal Therapy, low back pain, pulsed radiofrequency treatment
INTRODUCTION
Low back pain (LBP) is one of the most common causes of disability [1]. Although there are a variety of etiologies, it has been estimated that discogenic LBP accounts for 28-40% of patients with LBP [2,3]. The pain is often provoked by cumulative loading. In addition, patients experience sitting intolerance. Neurological examination reveals no neurological deficits, and the straight leg raise (SLR) test often gives equivocal results [2,3].
Provocative discography is considered a reference technique for confirming the intervertebral disc as a cause of the LBP [2,3]. Furthermore, achieving pain relief of more than 70% with the injection of a small amount of local anesthetic over three days is also important for the diagnosis of discogenic LBP [4]. Intradiscal Electrothermal Therapy (IDET) has been used as a minimally invasive procedure for managing chronic discogenic LBP in patients failing conservative treatments [5-8]. However, meta-analyses of the available data on the efficacy of IDET generate controversial conclusions [9-11].
In recent years, there has been a general trend in interventional treatment away from radiofrequency thermocoagulation and toward pulsed radiofrequency (PRF), as a less destructive treatment.
Teixeira and Sluijter [12] reported that high-voltage, long-duration intradiscal PRF, achieved by means of an electrode placed in the center of the nucleus pulposus in patients with discogenic LBP, produced excellent to good outcomes in 8 cases. Recently, minimally invasive intradiscal Diskit II® needles, (NeuroTherm, Wilmington, MA, USA) which are able to provide PRF to the disc with the 20-mm active tip, have been developed. However, there have been few investigations of intradiscal PRF treatment with Diskit II® needles for discogenic LBP [12,13].
The purpose of this study was to evaluate the efficacy of the intradiscal PRF (Disc PRF) procedure with Diskit II® needles and to compare the representative outcomes of Disc PRF and IDET [5-8] in terms of pain relief and reduction of disability.
MATERIALS AND METHODS
1. Patients
Thirty-one patients with discogenic LBP who underwent Disc PRF (n = 15) or IDET (n = 16) between April 2003 and March 2011 were enrolled in the study. All patients met the criteria for the Disc PRF procedure and IDET. In these patients, IDET was performed between April 2003 and March 2009, and Disc PRF was performed between April 2009 and March 2011.
The criteria for inclusion in our study of Disc PRF and IDET were the following: (1) Chronic LBP of at least 6 months' continuous duration. (2) Lack of satisfactory improvement with a comprehensively applied non-operative care program including the following: epidural corticosteroid injection, a trial of physical therapy, and oral anti-inflammatory medication. (3) Normal findings on neurologic examination. (4) Negative SLR results. (5) A magnetic resonance scan that showed no evidence of a neural compression lesion. (6) Concordant pain at low pressurization (low volume less than ≤ 1.25 ml of contrast medium) during discography of the concerned disc. (7) A decrease in pain of more than 70% for more than 3 days following intradiscal administration of 1 ml of lidocaine 2% [4].
The exclusion criteria were: (1) Disc extrusion or a sequestered fragment. (2) Severe spinal canal narrowing. (3) Segmental instability, or psychological issues. (4) Systemic infection or localized infection at the anticipated needle entry sites. (5) Chronic lower extremity radiculopathy. (6) History of opioid abuse [14].
In the Disc PRF group, there were 15 patients (10 male, 5 female) and a total of 15 procedures were performed. The mean age of patients was 39.3 ± 9.9 years (range 27-55 years). Of the 15 discs treated, 7 were at L5-S1, 7 were at L4-L5, and 1 was at L2-L3.
In the IDET group, there were 16 patients (11 male, 5 female) and a total of 15 procedures were performed. The mean age of patients was 41.7 ± 10.1 years (range 29-56 years). Of the 16 discs treated, 7 were at L4-L5, 8 were at L5-S1, and 1 was at L2-L3.
The study protocol was approved by the Human Ethics Review Committee of Shiga University of Medical Science. The procedure and its associated potential complications, such as nerve root injuries, epidural space bleeding, and discitis, were explained to the patients, and informed consent was obtained before treatment.
2. Disc PRF procedure
Disc PRF was performed with the patients lying on a fluoroscopy table in the prone position. The discs treated were selected on clinical grounds according to the level of provocative discography.
Under fluoroscopic guidance and via a posterior oblique approach, the Diskit II® needle (20 G, 15-cm length, 20-mm active tip, with radiopaque marker active tip; NeuroTherm) was percutaneously advanced and placed centrally in the disc which was responsible for the symptoms (Fig. 1). Proper placement of the introducer needle was confirmed with anteroposterior, oblique, and lateral fluoroscopic projections. The proximal end of the tip was equipped with a radiopaque marker, and the active tip was advanced to a position where it was completely within the disc.
Fig. 1.
Intradiscal pulsed radiofrequency (Disc PRF) procedures. Lateral view and anteroposterior (AP) view show that the Diskit II® needle is positioned in the L4/5 and the active part of the needle is completely inside the disc.
After performing electro-stimulation at 2 V at 2 and 50 Hz to confirm that the needle position was far enough away from the segmental nerve, we applied higher voltages for longer exposure times. We applied intradiscal PRF at a frequency of 5 Hz, pulse width of 5 ms, amplitude of 60 V, and a maximum temperature of 40℃, for a duration of 15 minutes, with the NT1100 generator (NeuroTherm).
Disc PRF was performed on an outpatient basis. Prophylactic intravenous antibiotics were administered 15-40 minutes prior to beginning the procedure. After an hour of bed rest, patients were allowed to leave the outpatient clinic.
IDET procedures were performed on an outpatient basis under local anesthesia by the same surgeon. Inclusion and exclusion criteria were the same as those for the Disc PRF procedure.
3. Outcome measures
The severity of the pain was assessed using the pain intensity score on a 0-10 numeric rating scale (NRS) preprocedure and at 1, 3, and 6 months after the procedure. In addition, the Roland-Morris Disability Questionnaire (RMDQ) score [8,15] was measured pre-procedure and at 1, 3, and 6 months after the procedure. Patients were examined pre-procedure and at 1, 3, and 6 months after the procedure by blinded staff members.
The Wilcoxon signed-rank test and the Mann-Whitney U test were used to evaluate and compare the differences in NRS and RMDQ scores before and after the procedure. P values < 0.01 were considered statistically significant.
RESULTS
The mean preoperative NRS score was 7.2 ± 0.6 (range 6-8) in the Disc PRF group, and 7.5 ± 1.0 (range 5-9) in the IDET group.
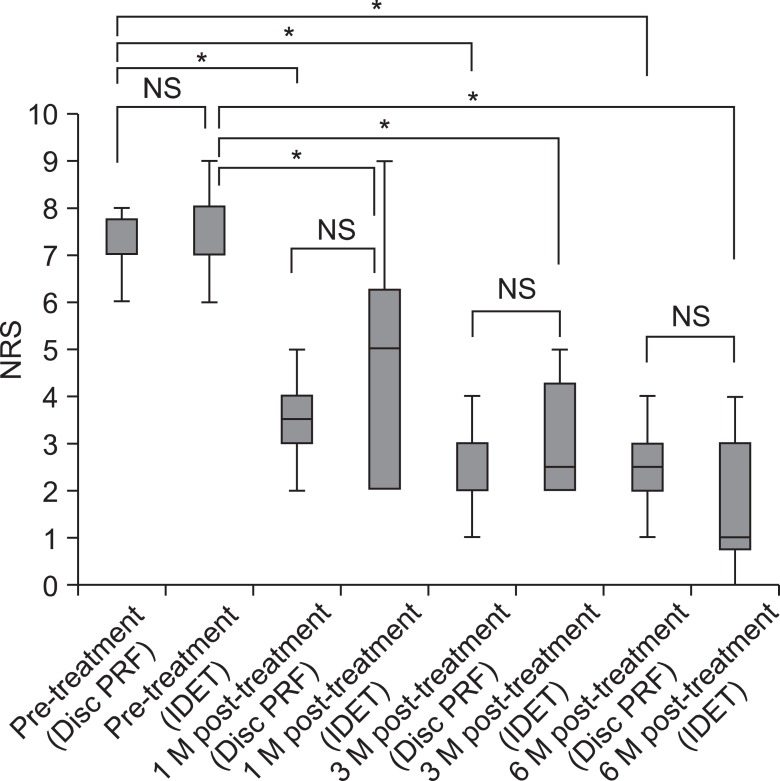
Mean NRS scores decreased from 7.2 and 7.5 at pretreatment to 3.4 ± 0.9 (range 2-5) and 4.6 ± 2.4 (range 2-9) at 1 month post-treatment, 2.6 ± 0.9 (range 1-4) and 3.1 ± 1.3 (range 2-5) at 3 months post-treatment, and 2.5 ± 0.9 (range 1-4) and 1.7 ± 1.5 (range 0-4) at 6 months post-treatment in the Disc PRF group and the IDET group, respectively (Fig. 2). In both groups, these decreases were statistically significant (P < 0.01, Wilcoxon signed-rank test) (Fig. 2).
Fig. 2.
Numeric Rating Scale (NRS) scores pre-procedure and at 1, 3, and 6 months post-treatment in the Disc PRF and IDET groups. Data are presented as median and lower limit, 25th, 75th, and upper limit percentiles. Wilcoxon signed-rank test and Mann-Whitney U test. *P < 0.01. NS: not significant.
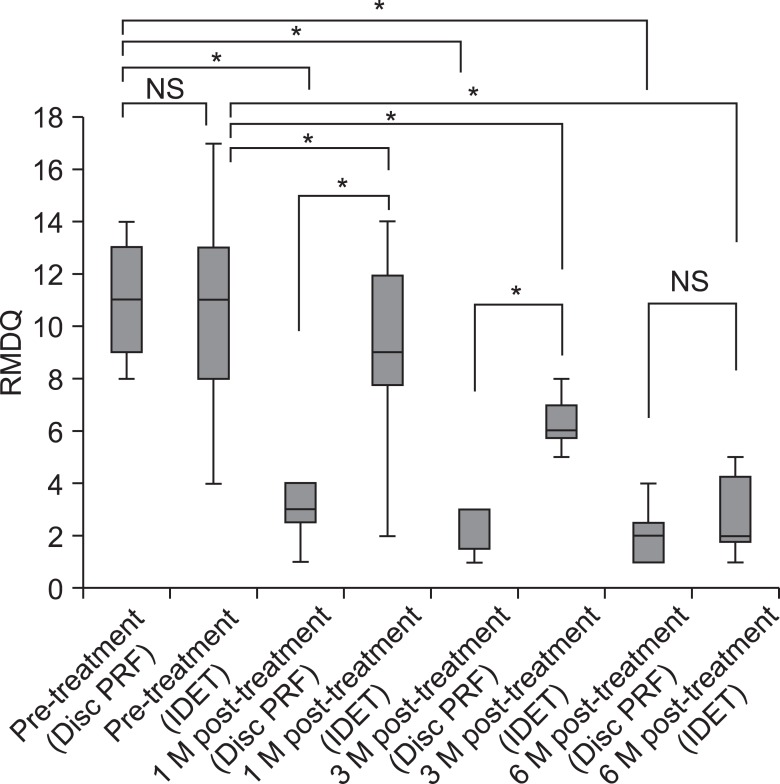
Mean RMDQ scores improved from 10.8 ± 2.3 (range 8-14) and 10.4 ± 4.0 (range 4-17) pretreatment to 3.5 ± 2.0 (range 1-7) and 8.9 ± 3.6 (range 2-14) at 1 month post-treatment, 2.9 ± 2.0 (range 1-7) and 5.8 ± 2.0 (range 2-9) at 3 months post-treatment, and 2.3 ± 1.8 (range 1-7) and 2.8 ± 1.6 (range 1-5) at 6 months post-treatment in the Disc PRF group and the IDET group, respectively (Fig. 3). These decreases were also statistically significant (P < 0.01, Wilcoxon signed-rank test) in both groups (Fig. 3).
Fig. 3.
Roland-Morris Disability Questionnaire (RMDQ) scores pre-procedure and at 1, 3, and 6 months post-treatment in the Disc PRF and IDET groups. Data are presented as median and lower limit, 25th, 75th, and upper limit percentiles. Wilcoxon signed-rank test and Mann-Whitney U test. *P < 0.01. NS: not significant.
The baseline NRS and RMDQ scores did not show statistically significant differences between the two groups. There were also no significant differences in the NRS scores between the two groups at 1, 3, and 6 months post-treatment (Fig. 2, 3).
The mean RMDQ scores in the Disc PRF group at 1 month post-treatment and at 3 months post-treatment were significantly (P < 0.01, Mann-Whitney U test) lower than the scores in the IDET group (Fig. 2, 3). There were no significant (P < 0.01, Mann-Whitney U test) differences between the groups in the RMDQ scores at 6 months post-treatment (Fig. 2, 3).
All patients had been taking a variety of medications, including various nonsteroidal anti-inflammatory drugs (NSAIDs) and cyclooxygenase (COX) inhibitors. No patients complained of flare-up pain after the Disc PRF procedure. In addition, none of the patients increased either the amount or types of medication taken following the Disc PRF procedure. In contrast, 14 patients (87.5%) complained of flare-up pain after the IDET procedure. Fourteen patients also increased the amount of medication or increased the types of medication taken transiently, for 1-8 weeks after the IDET procedure.
All procedures were considered technically successful. There were no complications of nerve root injuries, epidural space bleeding, discitis, or infection related to the procedures. There were also no cases of worsening motor or sensory status.
DISCUSSION
Chronic discogenic LBP may result from mechanical stimulation of annulus fissures, or from delamination, in which the annular lamellae repeatedly stimulate nociceptors that may have been presensitized [16]. IDET has been used to manage chronic discogenic LBP in patients for whom conservative treatments fail [5-8]. However, meta-analyses and systematic reviews of the data on IDET produce contradictory results [9]. Furthermore, most patients who undergo IDET experience long-lasting (up to 2 months) post-procedure flare-up pain [17].
Teixeira and Sluijter [12] first reported on PRF treatment for discogenic pain. However, there have been no investigations of Disc PRF with Diskit II® needles in patients with discogenic LBP.
In the present study, Disc PRF produced significant effects in patients with discogenic LBP, leading to the improvement of RMDQ scores. Patients who underwent Disc PRF for discogenic LBP showed significant improvements in terms of pain relief and reduction of disability. Based on our results, Disc PRF appears to be an effective and promising non-operative treatment for chronic discogenic LBP.
Furthermore, no patients in the Disc PRF group complained of flare-up pain after the Disc PRF procedure. Disc PRF could eliminate the long-lasting flare-up pain linked to other techniques using radiofrequency thermocoagulation, such as IDET [17]. Disc PRF do not apply heat over 42℃ to the intervertebral disc, leading to no flare-up pains following the procedure.
The mean RMDQ scores at 1 and 3 months post-treatment were significantly (P < 0.01) lower in the Disc PRF group compared to the IDET group (Fig. 2, 3). Disc PRF resulted in significantly more rapid improvement after treatment compared to IDET.
The findings of our study suggest that Disc PRF may be a safe and effective alternative to IDET as a minimally invasive treatment for chronic discogenic LBP.
A major advantage of Disc PRF with Diskit II® needles is that, when performing procedures in discectomized discs, it is relatively easy to place the Diskit II® needle, eliminating the need to thread a long heating portion of an IDET catheter.
The Diskit II® needles are thin (20 G), allowing treatment of discs with a residual height as low as 10-25% of the original height, while IDET electrodes are up to 17 G and treatment can only be performed in discs that still have at least 50% of the original height. Other advantages of Disc PRF include that it is an outpatient procedure, only local anesthesia is needed, and the procedure takes a very short time.
The exact mechanism by which Disc PRF reduces discogenic pain is uncertain. It is thought, however, that the procedure decreases discogenic pain by two different mechanisms. First, the high-voltage PRF current applied intradiscally by means of Diskit II® needles may cause very strong electric fields, and these fields could potentially have a biological effect on the nerve endings in the disc [18,19]. The electric field generated is assumed to induce changes in the tissue that may explain changes in pain conduction [18,19]. The second effect could possibly reflect an action of the electric field on immune cells, thus influencing the production of anti-inflammatory cytokines, resulting in increased levels of pro-inflammatory cytokines such as interleukin (IL)-1b, tumor necrosis factor-α, and IL-6 [20].
Carefully selected patients with discogenic LBP, nonresponsive to conservative care and provocative discography and disc block [4], seem to benefit clinically from Disc PRF in terms of pain reduction and also in terms of functional and quality-of-life improvement. With the latest equipment such as the NT1100 generator (NeuroTherm), pulse width, pulse frequency, voltage, force, and time can be changed freely, allowing providers to propose more options for treatment parameters. Further research is needed to define the optimal time and the proper setting conditions for applying PRF current.
In conclusion, Disc PRF appears to be a safe, minimally invasive treatment option and alternative to IDET for carefully selected patients with chronic lumbar discogenic LBP who have not responded to aggressive non-operative care. F urther randomized placebo-controlled studies with longer follow-up periods are needed to elucidate the effects of Disc PRF and confirm its safety and efficacy.
References
- 1.Andersson GB. Epidemiology of low back pain. Acta Orthop Scand Suppl. 1998;281:28–31. doi: 10.1080/17453674.1998.11744790. [DOI] [PubMed] [Google Scholar]
- 2.Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. The prevalence and clinical features of internal disc disruption in patients with chronic low back pain. Spine (Phila Pa 1976) 1995;20:1878–1883. doi: 10.1097/00007632-199509000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Zhou Y, Abdi S. Diagnosis and minimally invasive treatment of lumbar discogenic pain--a review of the literature. Clin J Pain. 2006;22:468–481. doi: 10.1097/01.ajp.0000208244.33498.05. [DOI] [PubMed] [Google Scholar]
- 4.Ohtori S, Kinoshita T, Yamashita M, Inoue G, Yamauchi K, Koshi T, et al. Results of surgery for discogenic low back pain: a randomized study using discography versus discoblock for diagnosis. Spine (Phila Pa 1976) 2009;34:1345–1348. doi: 10.1097/BRS.0b013e3181a401bf. [DOI] [PubMed] [Google Scholar]
- 5.Saal JA, Saal JS. Intradiscal electrothermal treatment for chronic discogenic low back pain: Prospective outcome study with a minimum 2-year follow-up. Spine (Phila Pa 1976) 2002;27:966–973. doi: 10.1097/00007632-200205010-00017. [DOI] [PubMed] [Google Scholar]
- 6.Saal JA, Saal JS. Intradiscal electrothermal treatment for chronic discogenic low back pain: a prospective outcome study with minimum 1-year follow-up. Spine (Phila Pa 1976) 2000;25:2622–2627. doi: 10.1097/00007632-200010150-00013. [DOI] [PubMed] [Google Scholar]
- 7.Pauza KJ, Howell S, Dreyfuss P, Peloza JH, Dawson K, Bogduk N. A randomized, placebo-controlled trial of intradiscal electrothermal therapy for the treatment of discogenic low back pain. Spine J. 2004;4:27–35. doi: 10.1016/j.spinee.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 8.Lutz C, Lutz GE, Cooke PM. Treatment of chronic lumbar diskogenic pain with intradiskal electrothermal therapy: a prospective outcome study. Arch Phys Med Rehabil. 2003;84:23–28. doi: 10.1053/apmr.2003.50059. [DOI] [PubMed] [Google Scholar]
- 9.Appleby D, Andersson G, Totta M. Meta-analysis of the efficacy and safety of intradiscal electrothermal therapy (IDET) Pain Med. 2006;7:308–316. doi: 10.1111/j.1526-4637.2006.00172.x. [DOI] [PubMed] [Google Scholar]
- 10.Freeman BJ. IDET: a critical appraisal of the evidence. Eur Spine J. 2006;15(Suppl 3):S448–S457. doi: 10.1007/s00586-006-0156-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Urrútia G, Kovacs F, Nishishinya MB, Olabe J. Percutaneous thermocoagulation intradiscal techniques for discogenic low back pain. Spine (Phila Pa 1976) 2007;32:1146–1154. doi: 10.1097/01.brs.0000261492.55121.93. [DOI] [PubMed] [Google Scholar]
- 12.Teixeira A, Sluijter ME. Intradiscal high-voltage, long-duration pulsed radiofrequency for discogenic pain: a preliminary report. Pain Med. 2006;7:424–428. doi: 10.1111/j.1526-4637.2006.00138.x. [DOI] [PubMed] [Google Scholar]
- 13.Rohof O. Intradiscal pulsed radiofrequency application following provocative discography for the management of degenerative disc disease and concordant pain: a pilot study. Pain Pract. 2012;12:342–349. doi: 10.1111/j.1533-2500.2011.00512.x. [DOI] [PubMed] [Google Scholar]
- 14.Webster BS, Verma S, Pransky GS. Outcomes of workers' compensation claimants with low back pain undergoing intradiscal electrothermal therapy. Spine (Phila Pa 1976) 2004;29:435–441. doi: 10.1097/01.brs.0000092376.41688.1a. [DOI] [PubMed] [Google Scholar]
- 15.Fujiwara A, Kobayashi N, Saiki K, Kitagawa T, Tamai K, Saotome K. Association of the Japanese Orthopaedic Association score with the Oswestry Disability Index, Roland-Morris Disability Questionnaire, and short-form 36. Spine (Phila Pa 1976) 2003;28:1601–1607. [PubMed] [Google Scholar]
- 16.Freemont AJ, Peacock TE, Goupille P, Hoyland JA, O'Brien J, Jayson MI. Nerve ingrowth into diseased intervertebral disc in chronic back pain. Lancet. 1997;350:178–181. doi: 10.1016/s0140-6736(97)02135-1. [DOI] [PubMed] [Google Scholar]
- 17.Derby R, Seo KS, Kazala K, Chen YC, Lee SH, Kim BJ. A factor analysis of lumbar intradiscal electrothermal annuloplasty outcomes. Spine J. 2005;5:256–261. doi: 10.1016/j.spinee.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 18.Bogduk N. Pulsed radiofrequency. Pain Med. 2006;7:396–407. doi: 10.1111/j.1526-4637.2006.00210.x. [DOI] [PubMed] [Google Scholar]
- 19.Cosman ER, Jr, Cosman ER., Sr Electric and thermal field effects in tissue around radiofrequency electrodes. Pain Med. 2005;6:405–424. doi: 10.1111/j.1526-4637.2005.00076.x. [DOI] [PubMed] [Google Scholar]
- 20.Chua NH, Vissers KC, Sluijter ME. Pulsed radiofrequency treatment in interventional pain management: mechanisms and potential indications-a review. Acta Neurochir (Wien) 2011;153:763–771. doi: 10.1007/s00701-010-0881-5. [DOI] [PMC free article] [PubMed] [Google Scholar]