Abstract
Background
The aim of the study was to investigate the feasibility of fluoroscopy-guided anterior approach for suprascapular nerve block (SSNB).
Methods
Twenty patients with chronic shoulder pain were included in the study. All of the nerve blocks were performed with patients in a supine position. Fluoroscopy was tilted medially to obtain the best view of the scapular notch (medial angle) and caudally to put the base of coracoid process and scapular spine on same line (caudal angle). SSNB was performed by introducing a 100-mm, 21-gauge needle to the scapular notch with tunnel view technique. Following negative aspiration, 1.0 ml of contrast was injected to confirm the scapular notch, and 1 % mepivacaine 2 ml was slowly injected. The success of SSNB was assessed by numerical rating scale (NRS) before and after the block.
Results
The average NRS was decreased from 4.8 ± 0.6 to 0.6 ± 0.5 after the procedure (P < 0.05). The best view of the scapular notch was obtained in a medial angle of 15.1 ± 2.2 (11-19°) and a caudal angle of 15.4 ± 1.7° (12-18°). The average distance from the skin to the scapular notch was 5.8 ± 0.6 cm. None of the complications such as pneumothorax, intravascular injection, and hematoma formation was found except one case of partial brachial plexus block.
Conclusions
SSNB by fluoroscopy-guided anterior approach is a feasible technique. The advantage of using a fluoroscopy resulted in an effective block with a small dose of local anesthetics by an accurate placement of a tip of needle in the scapular notch while avoiding pneumothorax.
Keywords: contrast media, fluoroscopy, nerve block, shoulder pain
INTRODUCTION
A shoulder joint is vulnerable to a various disease due to a large range of motion and a complex structure. A suprascapular nerve block (SSNB) has been used as an effective method to relieve pain of a shoulder joint and surrounding structures [1-3]. Traditionally SSNB has been performed by a landmark-guided or a fluoroscopy-guided posterior approach [4-8]. Although it is reported that the incidence of pneumothorax in SSNB is less than 1% [5], the risk still remains.
The study investigated the feasibility of fluoroscopy-guided anterior approach for SSNB. The authors measured the optimal angle of fluoroscopy for anterior approach in SSNB and changes of numerical rating scale (NRS). The incidence of other complications such as pneumothorax, intravascular injection, and hematoma formation were observed.
MATERIALS AND METHODS
The Research Ethics Committee of our hospital approved this pilot study. After discussing about the new approach of SSNB with each individual patient, written informed consents were obtained. Twenty patients complaining of chronic shoulder pain despite of analgesics, nonsteroidal anti-inflammatory drugs, physiotherapy were included. Enrolled patients were fifteen with impingement syndrome, three with adhesive capsulitis, and two with calcific supraspinatus tendonitis. Patients who had any pre-existing neurologic deficit, coagulopathy, a body mass index greater than 30 kg/m2, or pre-existing psychological disease were excluded from the study.
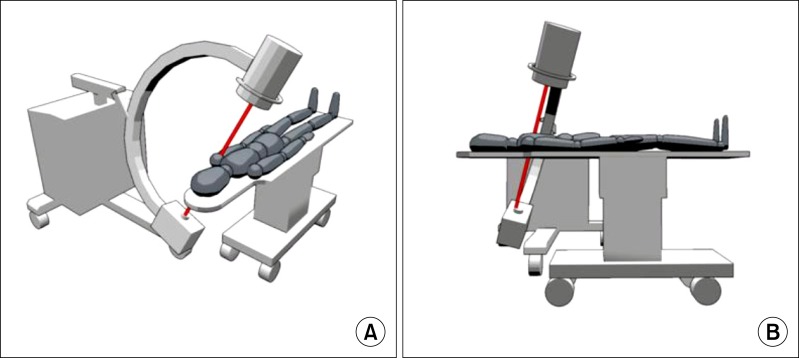
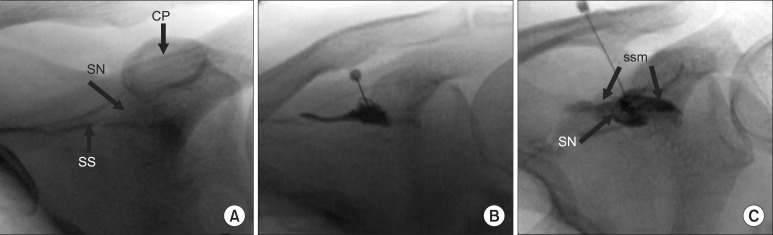
All of the nerve blocks were performed with patients in a supine position on a radiolucent table and the affected shoulder in a neutral position. Fluoroscopy was tilted medially to obtain the best view of the scapular notch (medial angle) and caudally to put the base of coracoid process and scapular spine on same line (caudal angle) (Fig. 1). Antiseptic preparation was done around the deltopectoral groove and skin infiltration was done with 1 ml of mepivacaine 2%. The needle entry point on the skin was about 2-3 cm inferior to the junction of medial 2/3rd and lateral 1/3rd of shaft of the clavicle. SSNB was performed by introducing a 100-mm, 21-gauge needle to the scapular notch by using a fluoroscopy-guided tunnel view technique. In tunnel view, the needle was advanced to scapular notch with 1 cm incrementally. During the procedure, when paresthesia was elicited, 1.0 ml of contrast was injected to confirm the scapular notch (Fig. 2A, B). In case, paresthesia was not elicited with radioopacification of supraspinatus muscle, the needle was withdrawn with 0.5 cm incrementally and 0.5 ml of contrast was injected until the scapular notch was radioopacified (Fig. 2C). After confirming the scapular notch, 1% mepivacaine 2 ml was slowly injected.
Fig. 1.
This figure shows fluoroscopic angulation for the anterior approach for suprascapular nerve. (A) Fluoroscopy was tilted medially (medial angle). (B) Fluoroscopy was tilted caudally (caudal angle).
Fig. 2.
This figure shows fluoroscopic images of the anterior approach for suprascapular nerve block. (A) Optimal fluoroscopic image for SSNB. (B) Contrast material suffusing through the suprascapular notch. (C) In case of radioopacification of supraspinatus muscle, the needle was withdrawn with 0.5 cm incrementally and 0.5 ml of contrast was injected until the scapular notch was radioopacified. CP: coracoids process, SN: suprascapular notch, SS: scapular spine, ssm: supraspinatus muscle.
A distance from the skin to the scapular notch was measured. The success of SSNB was assessed by numerical rating scale (NRS: 0, no pain and 10, unbearable pain) before and after the block. The time point of the NRS assessment was five minutes after the block. The patients were closely followed up in the outpatient department and advised to immediately visit hospital in the occurrence of symptoms of pneumothorax such as chest pain, dyspnea, or tachypnea. Data was analyzed by paired t-test using SPSS (version 12.0, SPSS Inc., Chicago, IL, USA), and all values were expressed in mean ± SD and defined as statistically valuable when P < 0.05.
RESULTS
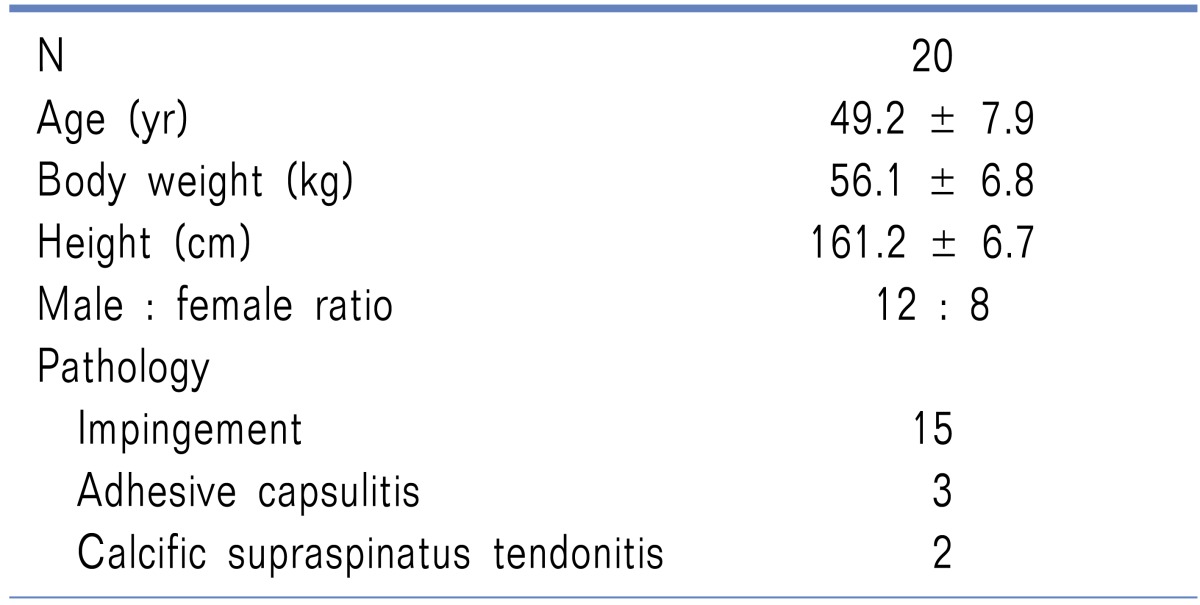
Demographic characteristics of the patients are summarized in Table 1. The average NRS was changed from 4.8 ± 0.6 to 0.6 ± 0.5 after the procedure which was statistically valuable (P < 0.05). Under fluoroscopy, the best view of the scapular notch was obtained in a medial angle of 15.1 ± 2.2° (11-19°) and a caudal angle of 15.4 ± 1.7° (12-18°). The average distance between the skin and the scapular notch was 5.8 ± 0.6 cm. None of the complications such as pneumothorax, intravascular injection, and hematoma formation was found except one case of partial brachial plexus block.
Table 1.
Demographic Data
Values are expressed as mean ± SD. N: number of the patients.
DISCUSSION
Shoulder pain is a common musculoskeletal complaint that may be due either to intrinsic disorders of the shoulder or a referred pain. The former include injuries and an acute or chronic inflammation of the shoulder joint, tendons, surrounding ligaments, or periarticular structures [9,10]. There are many conservative treatments available for managing shoulder pain, which include physiotherapy, nonsteroidal anti-inflammatory drugs and intra-articular corticosteroid injections. And SSNB has also been widely and effectively used in managing shoulder pain.
Anatomically, suprascapular nerve (SSN) supplies 70% of the sensory nerve innervating the shoulder joint, including the superior and posterosuperior regions of the shoulder joint, capsule, and the overlying skin [3]. SSN originates from the C5 and C6 nerve roots of the superior trunk of the brachial plexus; contribution from the C4 is usually present as well. It descends posteriorly, passing through the scapular notch, innervating the supraspinatus and the infraspinatus muscle.
Traditionally, SSNB technique has been performed by a posterior approach, originally described by Granirer [4]. The most commonly used posterior technique involves introducing a needle perpendicular to all planes approximately 2.5 cm superior and lateral to the midpoint of the scapular spine [5]. The notch is then located by seeking a loss of bony resistance. Another modified techniques using computed tomography were reported to increase the accuracy rates of needle placement, and to decrease possible complications in SSNB technique [11,12]. Moore [5] reported that the incidence of pneumothorax in SSNB is less than 1% in their study, although a risk of pneumothorax still remains. As shown in this study, keeping an enough distance between a tip of a needle and the thoracic wall is expected to lower the risk of a pneumothorax.
Under C-arm fluoroscopy, the best view of the scapular notch was obtained in a medial angle of 15.1 ± 2.2° (11-19°) and a caudal angle of 15.4 ± 1.7° (12-18°). Considering an exposure to a radiation, initiating with lateral angle of 15° and caudal angle of 15° of fluoroscopy may be helpful in minimizing the radiation exposure to both patients and clinicians. Also the advantage of using a fluoroscopy resulted in an effective block with a small dose of local anesthetics by a more accurate placement of a tip of needle in the scapular notch.
The average distance between from the skin to the scapular notch was 5.8 ± 0.6 cm in this study. In case of a radioopacification of the supraspinatus muscle by a contrast media during fluoroscopy-guided anterior approach, the depth of a needle should be withdrawn until the scapular notch is radioopacified.
A paresthesia in the arm had occurred in one case, we observed that the tip of needle was slightly inferior to the base of coracoid process. We withdrew the needle and redirected it in more cranial and medial direction. A brachial plexus passes between clavicle and 1st rib and reaches a humerus through an axilla 2 cm inferior to a coracoid process [13,14]. Therefore in a tunnel view technique, the direction of a needle must be kept away from the base of coracoid process and redirected in an occurrence of paresthesia of an arm.
Considering a nerve stimulator is a more accurate assessment tool for a nerve block, using a change of NRS as a tool for assessing a nerve block may be limitation of this study. Possibility of an inadvertent puncture of subclavian vessels exists in the absence of a hematoma or woozing. Therefore patients with an anatomical distortion around a deltopectoral groove and arteriovenous fistula in affected arm should be avoided.
In conclusion, SSNB by fluoroscopy-guided anterior approach is feasible and an effective technique. This fluoroscopy-guided anterior approach for SSNB provides a comfortable condition for both clinicians and patients in supine position, so the authors think that accurate and fast nerve block could be performed. The advantage of using a fluoroscopy resulted in an effective block with a small dose of local anesthetics by an accurate placement of a tip of needle in the scapular notch.
References
- 1.Shanahan EM, Ahern M, Smith M, Wetherall M, Bresnihan B, FitzGerald O. Suprascapular nerve block (using bupivacaine and methylprednisolone acetate) in chronic shoulder pain. Ann Rheum Dis. 2003;62:400–406. doi: 10.1136/ard.62.5.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Emery P, Bowman S, Wedderburn L, Grahame R. Suprascapular nerve block for chronic shoulder pain in rheumatoid arthritis. BMJ. 1989;299:1079–1080. doi: 10.1136/bmj.299.6707.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dahan TH, Fortin L, Pelletier M, Petit M, Vadeboncoeur R, Suissa S. Double blind randomized clinical trial examining the efficacy of bupivacaine suprascapular nerve blocks in frozen shoulder. J Rheumatol. 2000;27:1464–1469. [PubMed] [Google Scholar]
- 4.Granirer LW. A simple technic for suprascapular nerve block. N Y State J Med. 1951;51:1048. [PubMed] [Google Scholar]
- 5.Moore DC. Regional block. 4th ed. Springfield, Ill.: Thomas; 1965. pp. 300–303. [Google Scholar]
- 6.Waldman SD. Suprascapular nerve block. In: Waldman SD, editor. Atlas of interventional pain management. 2nd ed. Philadelphia: Saunders; 2004. pp. 163–165. [Google Scholar]
- 7.Gado K, Emery P. Modified suprascapular nerve block with bupivacaine alone effectively controls chronic shoulder pain in patients with rheumatoid arthritis. Ann Rheum Dis. 1993;52:215–218. doi: 10.1136/ard.52.3.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim CS, Lim KJ, Chung CD, Lee EY. The analgesic effect of continuous suprascapular nerve block after arthroscopic shoulder surgery. Korean J Anesthesiol. 2004;47:92–95. [Google Scholar]
- 9.Hawkins RJ, Bokor DJ. Clinical evaluation of shoulder problems. In: Rockwood CA Jr, Matsen FA III, editors. The shoulder. 2nd ed. Philadelphia: Saunders; 1998. pp. 164–197. [Google Scholar]
- 10.Aszmann OC, Dellon AL, Birely BT, McFarland EG. Innervation of the human shoulder joint and its implications for surgery. Clin Orthop Relat Res. 1996;(330):202–207. doi: 10.1097/00003086-199609000-00027. [DOI] [PubMed] [Google Scholar]
- 11.Feigl GC, Anderhuber F, Dorn C, Pipam W, Rosmarin W, Likar R. Modified lateral block of the suprascapular nerve: a safe approach and how much to inject? A morphological study. Reg Anesth Pain Med. 2007;32:488–494. doi: 10.1016/j.rapm.2007.06.394. [DOI] [PubMed] [Google Scholar]
- 12.Schneider-Kolsky ME, Pike J, Connell DA. CT-guided suprascapular nerve blocks: a pilot study. Skeletal Radiol. 2004;33:277–282. doi: 10.1007/s00256-003-0733-y. [DOI] [PubMed] [Google Scholar]
- 13.Brown DL, Bridenbaugh LD. The upper extremity somatic block. In: Cousins MJ, Bridenbaugh PO, editors. Neural blockade in clinical anesthesia and management of pain. 3rd ed. Philadelphia: Lippincott-Raven; 1998. pp. 345–371. [Google Scholar]
- 14.Moorthy SS, Schmidt SI, Dierdorf SF, Rosenfeld SH, Anagnostou JM. A supraclavicular lateral paravascular approach for brachial plexus regional anesthesia. Anesth Analg. 1991;72:241–244. doi: 10.1213/00000539-199102000-00018. [DOI] [PubMed] [Google Scholar]