Abstract
Background
Health information technology has been proven to be a successful tool for the management of patients with multiple medical conditions. The purpose of this study was to examine the impact of an enhanced telemedicine system on glucose control and pregnancy outcomes in women with gestational diabetes mellitus (GDM).
Subjects and Methods
We used an Internet-based telemedicine system to also allow interactive voice response phone communication between patients and providers and to provide automated reminders to transmit data. Women with GDM were randomized to either the telemedicine group (n=40) or the control group (n=40) and asked to monitor their blood glucose levels four times a day. Women in the intervention group transmitted those values via the telemedicine system, whereas women in the control group maintained paper logbooks, which were reviewed at prenatal visits. Primary outcomes were infant birth weight and maternal glucose control. Data collection included blood glucose records, transmission rates for the intervention group, and chart review.
Results
There were no significant differences between the two groups (telemedicine vs. controls) in regard to maternal blood glucose values or infant birth weight. However, adding telephone access and reminders increased transmission rates of data in the intervention group compared with the intervention group in our previous study (35.6±32.3 sets of data vs.17.4±16.9 sets of data; P<0.01).
Conclusions
Our enhanced telemedicine monitoring system increased system utilization and contact between women with GDM and their healthcare providers but did not impact upon pregnancy outcomes.
Introduction
Gestational diabetes mellitus (GDM) is a common medical complication of pregnancy affecting more than 200,000 pregnancies1,2 per year in the United States, and epidemiological evidence suggests that its prevalence is increasing.3 The International Association of Diabetes and Pregnancy Study Groups4 recently put forth recommendations that lowered the oral glucose tolerance test thresholds for the diagnosis of GDM. These criteria have been accepted by the American Diabetes Association5 and once implemented would mean that the number of pregnancies complicated by GDM could more than double, resulting in an increased need for prenatal services and potentially challenge available resources. Health information technology might offer a bridge to increase access to care and efficiency in the delivery of health care while maintaining quality for women with pregnancies complicated by GDM.
Studies performed outside of pregnancy have shown that telemedicine monitoring systems can help to improve blood glucose control and lower hemoglobin A1c levels.6–10 Three small telemedicine studies have been performed in pregnant women with type 1 diabetes, and these have also demonstrated improved maternal blood glucose control.11–13 To date there have also been three studies utilizing health information technology in women with GDM. Kruger et al.14 randomized women to either modem transmission or telephone reporting of blood glucose data; although there were no differences in blood glucose control, healthcare providers reported that modem transmission increased clinic workflow efficiency. Investigators in Spain15 utilized a technology system that combined a glucose meter with a mobile phone, allowing transmission to a central database and access to a short message service; they found that unscheduled visits were reduced by 62% while at the same time finding similar neonatal and pregnancy outcomes.
Our group16 has previously reported on the use of an Internet-based telemedicine system to manage women with GDM. The purpose of that study was to determine the feasibility of utilizing this approach to connect poor inner-city women with GDM to their healthcare providers. Women without computer access in that study (approximately half) were provided with computer training, refurbished computers, and free dial-up Internet access. We encountered numerous technical difficulties with hardware installation and maintenance. Twenty-two percent of women never accessed the system, and transmissions by the remaining women were infrequent, which may have masked the potential benefits of the system. Thus in the current study we added an interactive voice response (IVR) telephone system option to reduce these barriers. The IVR system, which is integrated into our Internet-based informatics application, can be accessed from any phone over a dedicated toll-free number and does not require specialized training. In addition, the functionality of the system was upgraded to include asynchronous phone messaging between clinicians and patients as well as automated reminders for patients to transmit data. The purpose of this study was to examine the impact of this enhanced telemedicine system on pregnancy outcomes in women with GDM compared with usual care. We hypothesized that the enhanced telemedicine system with its new functionality, ease of use, and improved access would increase rates of transmissions among women in the intervention group, leading to better maternal glucose control and fewer adverse pregnancy outcomes.
Subjects and Methods
Telemedicine system
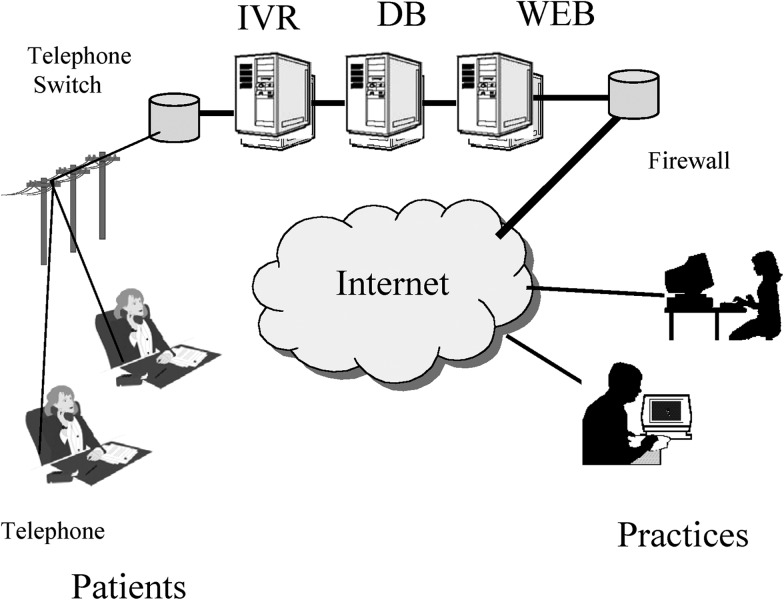
ITSMyHealthrecord® (Insight Telehealth Systems, Valley Forge, PA) is a HIPAA-compliant secure, encrypted, Web-based, nurse-coordinated communication system composed of a secure Internet server, an IVR-enabled phone system, and a database (Fig. 1). The system allows data transfer (messages and/or clinical information) from patient to practice and from practice to the patient in an asynchronous manner. This arrangement allows women to send blood glucose and other health data directly to their care providers and to receive information/advice from their healthcare providers via the Internet or phone.
FIG. 1.
Schematic representation of the integrated Internet-based informatics application and interactive voice response (IVR) system. DB, database.
When a woman is ready to send in her information, she can do so either by dialing a dedicated toll-free number or through the Internet using her unique log-in and password. Both systems allow women to append a message or ask a question (the IVR is set to accept 45 s of speaking, while the Internet-based method allows virtually unlimited text input) after transmitting their health data. The data and messages are then queued for the clinician to respond to when he or she accesses the clinician portal of the system in which the patient data reside.
When reviewing data that have been sent in from a phone, the nurse is able to hear the patient's message, which the IVR system has captured as a wav file, through the clinician portal. The nurse can then respond by typing a response, which is read to the patient via a text-to-voice function the next time she assesses the IVR system. If the patient accesses the system through the Internet, that same message is available to the patient in the form of text that appears as the first thing she sees after logging into her account.
The system is also designed to provide reminders for women to record and transmit their data if information was not received as scheduled. If a woman missed a data transmission either via the Internet or phone, the IVR system was programmed to place up to three phone-call (a day apart) reminders at a time of day chosen as being convenient by the subject. If the three reminder phone calls had been made and there had still not been a response, the nurse could either reset the reminders to send another three calls and/or call the patient directly to follow up.
Research design and methods
Women with GDM were recruited from two sites: the prenatal clinics at Temple University Hospital (Philadelphia, PA) and the Diabetes Education Program at Tallahassee Memorial Hospital (Tallahassee, FL). In order to be eligible for inclusion in the study, women had to be between the ages of 18 and 45 years and have a documented diagnosis of GDM on a 3-h oral glucose tolerance test, using the criteria of Carpenter and Coustan.17 Women were required to be at 33 weeks of gestation or less at study entry. Women with a prior history of glucose intolerance outside of pregnancy or multiple gestations (i.e., twins or triplets) were excluded.
The study was approved by the Temple University and Tallahassee Memorial Hospital Institutional Review Boards and was registered with ClinicalTrials.gov. Women were randomized into one of two groups: telemedicine or control (usual care). Following randomization, patients in the telemedicine group were trained on use of a computer and the Internet, instructed on the details of the Internet program, and introduced to the Web site on a demonstration terminal in the clinic. In addition, we provided an automated telephone communication option and instruction on its use for subjects who did not have Internet access. All subjects in the intervention group were provided with a password and log-in name to gain access to the secure Web site and a personal identification number and toll-free number to gain access to the telephone communication system. When utilizing the IVR system, subjects were prompted to input clinical data (i.e., blood glucose readings, changes in medication, and episodes of hypoglycemia) and identify the day and time using the phone's keypad. For this study women were provided feedback, emotional support, and reinforcement regarding diabetes self-management with each transmission. In addition, women received a brief educational message/tip each time they accessed the system either by phone or Internet.
Women in both groups were asked to monitor their blood glucose levels daily (before breakfast and 2 h after each meal), perform fetal movement counting three times a day, and also record insulin doses and episodes of hypoglycemia. Women in the treatment group were asked to transmit this information either via the phone or Internet at least weekly to their healthcare providers. Women in the control group were asked to record this information in a logbook, which was reviewed by the medical team at prenatal visits.
Both groups of women received the present standard of care18,19 in the two programs. All study participants were seen for clinical evaluation every 2 weeks until 36 weeks of gestation, after which they were seen weekly. Clinical care was provided by a team of maternal–fetal medicine subspecialists, residents, certified diabetes educators, and nutritionists as per management protocols at each institution. All subjects received individualized diet counseling and diabetes education. Patients were instructed in glucose self-monitoring and asked to monitor their blood glucose levels four times a day (before breakfast and 2 h after meals). All patients were treated to obtain metabolic goals of a fasting plasma blood glucose level of ≤95 mg/dL and 2-h postprandial blood glucose of ≤120 mg/dL. Women who failed to meet these targets at least 90% of the time were started on either glyburide or insulin therapy.
Outcome variables
The primary end points in this trial were maternal glucose control and infant birth weight. Secondary end points included pregnancy outcomes (mode of delivery, gestational age at delivery, neonatal intensive care unit admission, Apgar scores, and rates of large for gestational age, and other neonatal morbidities) and system use. Infants were considered large for gestational age when the birth weight was greater than the 90th percentile for gestational age. Respiratory outcomes included hyaline membrane disease, transient tachypnea, or need for respiratory support. Hypoglycemia was defined as a blood glucose level of <40 mg/dL. Hyperbilirubinemia was characterized by plasma values >12 mg/dL.
Data analysis
All data were analyzed based on subjects' assigned group regardless of their level of compliance with the testing protocol. Student's t tests were used to compare means of continuous variables. Comparisons between categorical variables were performed by χ2 analysis or by Fisher's exact test when appropriate. Multivariate regression was used to assess the impact of gender, parity, prepregnancy maternal body mass index (BMI), and form of therapy on birth weight. It was also used to evaluate the influence of site, treatment, insurance, prepregnancy BMI, and group on mean maternal glucose levels (SigmaStat statistical software, version 1; Systat, San Jose, CA).
Results
The sample
Eighty women with GDM (30 from Temple University Hospital and 50 from Tallahassee Memorial Hospital) consented to participate in the study protocol and were randomized to either the telemedicine group or the control group. Data collection occurred over a 26-month period from September 2007 through November 2009. Forty women were randomized to the intervention group, and 40 women were randomized to the control group. Two women in the usual care group and three women in the telemedicine group were lost to follow-up. In addition, one woman in the telemedicine group experienced a fetal loss at 19 weeks of gestation. Therefore, outcome data were available for 38 women in the control group and 36 in the intervention group. There were no significant differences at baseline between the two groups (Table 1).
Table 1.
Baseline Maternal Characteristics by Treatment Group
| Characteristic | Controls (n=40) | Telemedicine (n=40) |
|---|---|---|
| Age (years) | 30.3±6.0 | 30.0±7.5 |
| Body mass index (kg/m2) | 34.1±8.5 | 34.1±9.8 |
| Weight gain (pounds) | 21.5±16.1 | 21.7±19.7 |
| Gravidity | 2.9±1.9 | 2.5±1.8 |
| Parity | 1.7±1.8 | 1.1±1.0 |
| GA at entry (weeks) | 28.4±3.4 | 28.5±4.2 |
| Race/ethnicity | ||
| African American | 30% (12) | 37.5% (15) |
| White | 37.5% (15) | 45% (18) |
| Latino/Hispanic | 20% (8) | 15% (6) |
| Asian and other | 12.5% (5) | 2.5% (1) |
| Education | ||
| Less than high school | 10% (4) | 10% (4) |
| High school graduate | 25% (10) | 30% (12) |
| More than high school | 60% (24) | 60% (24) |
| Missing | 5% (2) | 0% (0) |
| Total family income | ||
| <$15,000/year | 20% (8) | 27.5% (11) |
| $15,000–$24,999 | 15% (6) | 22.5% (9) |
| $25,000–$34,999 | 22.5% (9) | 12.5 (5) |
| $35,000–$44,999 | 12.5% (5) | 17.5 (7) |
| $45,000–$54,999 | 0% (0) | 5% (2) |
| >$55,000/year | 12.5% (5) | 12.5% (5) |
| Missing | 17.5% (7) | 2.5% (1) |
| Glucose challenge (mg/dL) | 186.5±29.7 | 173.3±27.2 |
| 3-h OGTT (mg/dL) | ||
| FBS | 95.4±18.6 | 97.7±21.1 |
| 1 h | 195.1±24.5 | 201.5±39.7 |
| 2 h | 180.2±26.7 | 184.0±54.6 |
| 3 h | 128.7±38.4 | 149.0±48.8 |
Data are mean±SD values or percentages (n) as indicated.
FBS, fasting blood sugar; GA, gestational age; OGTT, oral glucose tolerance test.
Maternal outcomes
Both groups of women achieved similar levels of glycemic control (Table 2) as assessed by self-reported blood glucose records recorded in logbook format (control group) or by telemedicine transmissions (intervention group). Mean blood glucose levels did vary by site, with women from Tallahassee achieving lower mean glucose levels than the women in the Philadelphia cohort (104.7±9.3 mg/dL vs. 114.4±19.7 mg/dL; P=0.005). Women treated by medical nutrition therapy only also achieved lower mean blood glucose levels than women requiring pharmacotherapy (104.1±13.2 mg/dL vs. 114.6±15.1 mg/dL; P=0.002), either glyburide or insulin. After controlling for site, therapy, insurance, prepregnancy BMI, and group assignment, the effects of site differences were attenuated, and only mode of therapy remained significant (P<0.05). Approximately 40% of women in each group required pharmacological therapy (Table 3). Seven percent of women in the study developed pre-eclampsia or gestational hypertension, including two women from the control group and three from the telemedicine group (Table 4). Two women experienced premature rupture of membranes, and there were two cases of chorioamnionitis. Rates of cesarean delivery were increased among both groups but highest among women in the control group, although this difference did not reach statistical significance (P=0.53).
Table 2.
Maternal Glucose Control by Treatment Group
| Controls | Telemedicine | P | |
|---|---|---|---|
| FBS (mg/dL) | 94.3±10.5 | 91.5±10.5 | 0.26 |
| Blood glucose (mg/dL) | |||
| Breakfast | 110.9±18.5 | 108.1±17.0 | 0.50 |
| Lunch | 111.1±18.5 | 110.6±17.2 | 0.90 |
| Dinner | 117.6±22.0 | 119.8±17.3 | 0.64 |
| Mean | 109.7±16.5 | 107.4±12.9 | 0.44 |
Data are mean±SD values.
FBS, fasting blood sugar.
Table 3.
Diabetes Therapy by Treatment Group
| Diabetes therapy | Controls | Telemedicine |
|---|---|---|
| Diet | 60% (24) | 57.5% (23) |
| Oral agents | 20% (8) | 15% (6) |
| Insulin | 20% (8) | 27.5% (11) |
Data are percentages (n).
Table 4.
Maternal Outcomes by Treatment Group
| Controls | Telemedicine | P | |
|---|---|---|---|
| Cesarean delivery | 50% (19) | 36% (13) | 0.3 |
| Pre-eclampsia/gestational hypertension | 5% (2) | 8% (3) | 0.7 |
| Premature rupture of membranes | 0% (0) | 5.5% (2) | 0.2 |
| Chorioamnionitis | 2.6% (1) | 2.8% (1) | 1.0 |
Data are percentages (n).
Neonatal outcomes
Neonatal outcomes are summarized in Table 5. No significant differences were found between the two groups with regard to birth weight on univariate or multivariate analysis (after controlling for gender, parity, prepregnancy BMI, and treatment), gestational age at delivery, 1- and 5-min Apgar scores, and rates of large for gestational age. Eleven infants required admission to the neonatal intensive care unit, but there were no perinatal/neonatal deaths. One infant was born with chromosomal abnormalities and multiple congenital anomalies to a mother in the control group. Neonates born to mothers in the intervention group were less likely to be preterm, had lower rates of respiratory disorders, and were less likely to be admitted to the intensive care unit (11% vs. 18.4%), and if admitted, their length of stay was shorter (5.5 days vs. 9.7 days), but none of these differences was statistically significant.
Table 5.
Neonatal Outcomes by Treatment Group
| Controls | Telemedicine | P | |
|---|---|---|---|
| Birth weight (g) | 3,249±611 | 3,372±469 | 0.3 |
| GA at delivery (weeks) | 37.9±2.0 | 38.6±1.3 | 0.08 |
| Apgar score | |||
| 1 min | 8.1±1.0 | 7.6±2.0 | 0.2 |
| 5 min | 8.9±0.3 | 8.9±0.5 | 0.8 |
| LGA | 18.4% (7) | 25% (9) | 0.7 |
| Neonatal hypoglycemia | 10.5% (4) | 11% (4) | 1.0 |
| ICU admissions | 18.4% (7) | 11% (4) | 0.6 |
| Preterm delivery | 13.2% (5) | 5.6% (2) | 0.4 |
| Jaundice/hyperbilirubinemia | 5% (2) | 2.8% (1) | 1.0 |
| RDS/respiratory | 13.2% (5) | 5.6% (2) | 0.4 |
Data are mean±SD values or percentages (n) as indicated.
GA, gestational age; ICU, intensive care unit; LGA, large for gestational age; RDS, respiratory distress syndrome.
Use of the system
Seven women (18%) in the intervention group did not have access to the Internet at home. These seven women and an additional two women with Internet access used the IVR system to transmit their data. Of the 36 women in the intervention group available for follow-up until delivery, two women (6%) never used the system, and an additional five women (14%) used the system infrequently (<10 transmissions). On average, women sent 35.6 (±32.3) sets of data, which included fasting and postprandial blood glucose levels, fetal movement counts, and insulin doses when appropriate. However, women using the Internet sent in significantly more transmissions than did women using the phone/IVR system (42.8±32.4 vs. 10.9±16.3 data sets; P=0.007). As in our previous study, system use did not correlate with age, number of children, education, computer ownership, or treatment (diet vs. medication). However, in the current study there was a significant correlation between total family income and number of transmissions, with women with higher incomes transmitting more frequently (r=0.50, P<0.01). Sets of self-reported glucose data, either transmitted via the telemedicine system or provided in written form (logbooks) to providers, did not differ between the two groups (34.4±26.6 vs. 35.6±32.3 data sets for the control and intervention groups, respectively; P=0.75).
Discussion
This research sought to examine the impact of an enhanced telemedicine system, with IVR capabilities, on pregnancy outcomes in women with GDM. The system provided the women with feedback and reinforcement regarding diabetes self-management and facilitated communication between the women and their healthcare team. The system could be accessed either through the Internet or by phone, increasing its reach and utilization. In addition, the enhanced functionality provided automated reminders (phone calls generated by the IVR system) if women failed to transmit their data as scheduled. We postulated that the increased contact and feedback would enhance adherence to the diabetes self-management regimen, ultimately leading to improved glucose control and improved pregnancy outcomes.
It is disappointing that the system did not improve maternal glucose control, although more than two-thirds of women did achieve a mean glucose level of <110 mg/dL. The study was powered to detect a 10 mg/dL difference between the two groups. The lack of effect of the system on diabetes control could be related to the short period of the intervention (typically the period from diagnosis to delivery is only about 2 months) as well as the relatively small sample size, a limitation of this study. Similarly, pregnancy and neonatal outcomes did not differ significantly between the two groups. However, infants from the telemedicine group were less likely to be admitted to the intensive care unit and if admitted had shorter stays. In addition, the neonates in the intervention group had lower rates of preterm delivery, and the rate of respiratory distress syndrome was reduced by more than half. Although gestational age at delivery was also not statistically significant, the fact that the neonates from the intervention group were born 0.7 week later than controls may at least partially explain the lower rates of prematurity and respiratory distress syndrome/respiratory complications. One could postulate that these differences in neonatal outcomes may have reached statistical significance with a larger sample size.
Our findings are consistent with previous studies that also found little to no impact of technology on pregnancy outcomes in women with GDM. Kruger et al.14 reported increased clinic workflow efficiency with modem transmission but no effect on glucose control and pregnancy outcomes in their sample of women with GDM. Perez-Ferre et al.15 were able to reduce the number of unscheduled visits with their telemedicine system among women with GDM. They also reported high patient satisfaction with the system but no differences again in maternal glucose control or outcomes. Unfortunately, in the current study we did not examine the impact of our system on patient satisfaction or workflow efficiency. However, it would appear from the above-mentioned studies that the strength of these systems may be in their ability to increase efficiency while maintaining high-quality care and not in their ability to provide superior care. With the prevalence of GDM on the increase, the true benefit of this technology may be their capacity to streamline care.
Part of the challenge with any health information technology is to overcome the digital divide. Although clearly computers and access are more commonplace, gaps still exist, particularly among disadvantaged populations. In our first study16 published 4 years ago, only half of the women had Internet access in the home compared with more than 80% of women in the current study. In our previous studies both during and outside of pregnancy ownership of a computer as well as low socioeconomic status has not been found to be an impediment to successful participation. However, in this study we did find a significant correlation between total family income and number of transmissions, with women with higher incomes transmitting more frequently. In actuality, women at the lower end of the economic spectrum may have less access to support and resources, making it difficult to prioritize their own healthcare needs and implement self-care regimens.
In our original study, the system was totally Internet based. Women in that study who did not have a computer/Internet access at home were provided with computers. However, the computers were refurbished and used dial-up Internet access. The computers were delivered to the participant's home, and women received training from college and graduate students following installation. This approach was found to be very labor intensive and time consuming. Frequent technical difficulties required return visits to the home. Additional barriers to system use included the slowness of the refurbished computer with dial-up Internet access. As a result of these difficulties we redesigned the system to include IVR access. Women could access the system using either a landline or cell phone. We postulated that this option coupled with the capacity for automated reminders would increase system use, and in fact that did occur. In comparing the two studies, the number of data sets transmitted increased from 17.4±16.9 in the first study to 35.6±32.3 in the current study (P<0.01). This finding is consistent with the large literature suggesting that reminders can improve compliance with preventive services and increase positive health behaviors such as self-monitoring.20,21
In summary, our enhanced telemedicine monitoring system increased contact between women with GDM and their healthcare providers but did not impact upon pregnancy outcomes. The expectation that such systems may lead to improved control and outcomes among pregnant women with GDM may be unrealistic. However, the real potential of these emerging healthcare technologies may be their ability to increase efficiency while maintaining the quality of care. Future studies should focus on these issues as well as the impact of health technology on patient satisfaction with treatment.
Acknowledgments
This study was supported by grant R21-DK-071694 from the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health.
Author Disclosure Statement
C.J.H., L.D., K.R., W.M., D.M., and J.G. have nothing to disclose. W.P.S. has stock ownership in Insight Telehealth Systems. A.A.B. is a consultant for Insight Telehealth Systems.
References
- 1.Engelgau MM. Herman WH. Smith PJ. German RR. Aubert RE. The epidemiology of diabetes and pregnancy in the U.S., 1988. Diabetes Care. 1995;18:1029–1033. doi: 10.2337/diacare.18.7.1029. [DOI] [PubMed] [Google Scholar]
- 2.Coustan DR. Diabetes in America. 2nd. Bethesda, MD: National Institute of Diabetes and Digestive and Kidney Diseases; 1995. Gestational diabetes. [Google Scholar]
- 3.Ferrara A. Increasing prevalence of gestational diabetes mellitus: a public health perspective. Diabetes Care. 2007;30(Suppl 2):S141–S146. doi: 10.2337/dc07-s206. [DOI] [PubMed] [Google Scholar]
- 4.International Association of Diabetes and Pregnancy Study Groups Consensus Panel. International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33:676–682. doi: 10.2337/dc09-1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Diabetes Association: Standards of medical care in diabetes—2011. Diabetes Care. 2011;34(Suppl 1):S11–S61. doi: 10.2337/dc11-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bellazzi R. Larizza C. Montani S. Riva A. Stefanelli M. d'Annunzio G. Lorini R. Gomez EJ. Hernando E. Burgues E. Cermeno J. Corcoy R. de Leiva A. Cobelli C. Nucci G. Del Prato S. Maran A. Kilkki E. Tuominen J. A telemedicine support for diabetes management: the T-IDDM project. Comput Methods Programs Biomed. 2002;69:147–161. doi: 10.1016/s0169-2607(02)00038-x. [DOI] [PubMed] [Google Scholar]
- 7.Biermann E. Dietrich W. Standl E. Telecare of diabetic patients with intensified insulin therapy. A randomized clinical trial. Stud Health Technol Inform. 2000;77:327–332. [PubMed] [Google Scholar]
- 8.Shultz EK. Bauman A. Hayward M. Holzman R. Improved care of patients with diabetes through telecommunications. Ann N Y Acad Sci. 1992;670:141–145. doi: 10.1111/j.1749-6632.1992.tb26084.x. [DOI] [PubMed] [Google Scholar]
- 9.McMahon GT. Gomes HE. Hohne SH. Hu TM-J. Levine BA. Conlin PR. Web-based care management in patients with poorly controlled diabetes. Diabetes Care. 2005;28:1624–1629. doi: 10.2337/diacare.28.7.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weinstock RS. Teresi JA. Goland R. Izquierdo R. Palmas W. Eimicke JP. Ebner S. Shea S IDEATel Consortium. Glycemic control and health disparities in older ethnically diverse underserved adults with diabetes: five-year results from the Informatics for Diabetes Eduation and Telemedicine (IDEATel) study. Diabetes Care. 2011;34:274–279. doi: 10.2337/dc10-1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Frost D. Beischer W. Telemedicine in the management of pregnancy in type 1 diabetic women. Diabetes Care. 2000;23:863–864. doi: 10.2337/diacare.23.6.863. [DOI] [PubMed] [Google Scholar]
- 12.di Biase N. Napoli A. Sabbatini A. Borrello E. Buongiorno AM. Fallucca F. Telemedicine in the treatment of diabetic pregnancy. Ann 1st Super Sanita. 1997;33:347–351. [PubMed] [Google Scholar]
- 13.Wojcicki JM. Ladyzynski P. Krzymien J. Jozwicka E. Blachowicz J. Jamczewska E. Czajkowski K. Karnafel W. What we can really expect from telemedicine in intensive diabetes treatment: results from 3-year study on type 1 diabetic women. Diabetes Technol Ther. 2001;3:581–589. doi: 10.1089/15209150152811207. [DOI] [PubMed] [Google Scholar]
- 14.Kruger DF. White K. Galpern A. Mann K. Massirio A. McLellan M. Stevenson J. Effect of modem transmission of blood glucose data on telephone consultation time, clinic work flow, and patient satisfaction for patients with gestational diabetes mellitus. J Am Acad Nurse Pract. 2003;15:371–375. doi: 10.1111/j.1745-7599.2003.tb00410.x. [DOI] [PubMed] [Google Scholar]
- 15.Perez-Ferre N. Galindo M. Fernandez MD. Velasco V. de la Cruz MJ. Martin P. del Valle L. Calle-Pascual AL. A telemedicine system based on Internet and short message service as a new approach in the follow-up of patients with gestational diabetes. Diabetes Res Clin Pract. 2010;87:e15–e17. doi: 10.1016/j.diabres.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 16.Homko CJ. Santamore WP. Whiteman V. Bower M. Berger P. Geifman-Holtzman O. Bove AA. Use of an Internet-based telemedicine system to manage underserved women with gestational diabetes. Diabetes Technol Ther. 2007;9:277–286. doi: 10.1089/dia.2006.0034. [DOI] [PubMed] [Google Scholar]
- 17.Carpenter MW. Coustan DR. Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol. 1982;144:768–773. doi: 10.1016/0002-9378(82)90349-0. [DOI] [PubMed] [Google Scholar]
- 18.American College of Obstetricians and Gynecologists Committee on Practice Bulletins—Obstetrics: ACOG Practice Bulletin. Clinical management guidelines for obstetrician-gynecologists. Number 30, September 2001 (replaces Technical Bulletin Number 200, December 1994). Gestational diabetes. Obstet Gynecol. 2001;98:525–538. [PubMed] [Google Scholar]
- 19.American Diabetes Association: Clinical practice recommendations: gestational diabetes mellitus. Diabetes Care. 2003;26(Suppl 1):S103–S105. [Google Scholar]
- 20.Macharia WM. Leon G. Rowe BH. Stephenson BJ. Haynes RB. An overview of interventions to improve compliance with appointment keeping for medical services. JAMA. 1992;267:1813–1817. [PubMed] [Google Scholar]
- 21.van Dulmen S. Sluijs E. van Dijk L. de Ridder D. Heerdink R. Bensing J. Patient adherence to medical treatment: a review of reviews. BMC Health Serv Res. 2007;7:55–68. doi: 10.1186/1472-6963-7-55. [DOI] [PMC free article] [PubMed] [Google Scholar]