Abstract
Background:
A school-based surveillance system entitled the childhood and adolescence surveillance and prevention of Adult Noncommunicable disease (CASPIAN) Study is implemented at national level in Iran. This paper presents the methods and primary findings of the third survey of this surveillance system.
Methods:
This national survey was performed in 2009–2010 in 27 provinces of Iran among 5570 students and one of their parents. In addition to physical examination, fasting serum was obtained. Body mass index was categorized based on the World Health Organization growth charts.
Findings:
Data of 5528 students (2726 girls, 69.37% urban, mean age 14.7 ± 2.4 years) were complete and are reported. Overall, 17.3% (17.3% of girls and 17.5% of boys) were underweight, and 17.7% (15.5% of girls and 19.9% of boys) were overweight or obese. Abdominal obesity was documented in 16.3% of students (17.8% of girls and 15% of boys). 57.6% of families consumed breads, the staple food for Iranians, prepared with white flour. Most families (43.8% in urban areas and 58.6% in rural areas) used solid hydrogenated fats. 22.7% of students did not add salt to the table food. 14.2% of students reported to have a regular daily physical activity for at least 30 min a day. Overall, 10.4% of students (11.7% in urban areas and 7.3% in rural areas) reported that they used tobacco products, often waterpipe. 32.8% of students experienced at least three times of bullying in the previous 3 months. During the year prior to the survey, 14.46% of students had an injury needing the interference by school health providers.
Conclusion:
This survey is confirmatory evidence on the importance of establishing surveillance systems for risk behaviors to implement action-oriented interventions.
Keywords: Chronic diseases, prevention, risk behaviors, risk factors, school health, surveillance
INTRODUCTION
It is generally established that the harmful effects of communicable disease and malnutrition on public health are of the utmost importance notably in the poor countries. Consequently, the priority of the health institutions and care workers has been focusing on control and preventive measures of the infectious diseases.[1–3] However, in many cases, health care promotion and enhancement of medical insurance have tackled these issues.
On the other hand, rapid changes in lifestyle, nutrition, and physical activity, especially among the youngsters, have been accompanied by long-term change in disease patterns which is no longer allocated to industrialized countries.[4,5] As a direct result of this, chronic noncommunicable disease (NCD) is becoming epidemic and global issue as two out of three deaths in the world are related to chronic diseases. These are affecting an abundance of people of all ages, nationalities, and socioeconomic classes[6–8] In addition to developed countries, the prevalence of NCDs is now increasing in developing countries, which would lead to increased morbidity and mortality, as well as to a high financial burden.[9,10]
A growing body of literature documented changes in lifestyle habits and the global increase in childhood overweight.[11,12] Given the long-term consequences of childhood obesity on morbidity and mortality,[13] health care in the pediatrics group deserves further consideration.
Similar to the children and adolescents of other developing countries, Iranian youths are experiencing lifestyle changes, making them prone to risk factors of chronic diseases.[14–19]
Considering the tracking of NCD-related risk behaviors and risk factors from childhood to adult life, surveillance of such factors, e.g., blood pressure, avoidance of smoking, and overweight as well as encouraging regular physical exercise in children and adolescents, can provide useful information for long-term national planning. Some international organizations have implemented surveillance systems for tracking such factors. The global school-based student health survey (GSHS) has developed and supported by the World Health Organization (WHO) in cooperation with United Nations’ UNICEF, UNESCO, UNAIDS, and Centers for Disease Control and Prevention (CDC).[20] The Youth Risk Behavior Surveillance System (YRBSS) aims to monitor those health-risk behaviors contributing to the young and adults’ morbidity and mortality. They include behaviors related to unintentional injuries and violence, tobacco use, alcohol and other drug use, sexual risk behaviors, unhealthy dietary behaviors, and physical inactivity, as well as obesity and asthma.[21] In Iran, a school-based surveillance system entitled the childhood and adolescence surveillance and prevention of Adult Noncommunicable disease (CASPIAN) Study is implemented from 2003–2004.[22] The surveys are repeated every 2 years, with blood sampling for biochemical factors every 4 years. This paper presents the methods and primary findings of the third survey of this school-based surveillance system.
METHODS
Study population
This school-based nationwide health survey was conducted in Iran as the national survey of school student high risk behaviors (2009–2010). It was conducted as the third study of the school-based surveillance system entitled CASPIAN-III Study.
It was performed with corporation of the Ministry of Health and Medical Education; Ministry of Education and Training, Child Health Promotion Research Center, Isfahan University of Medical Sciences; and Endocrinology and Metabolism Research Institute of Tehran University of Medical Sciences. The survey was performed among 5570 students aged 10–18 years, who were selected by multistage random cluster sampling from urban and rural areas of 27 provinces of Iran. Eligible schools for our study were stratified according to information bank of Ministry of Education, and then, they were selected randomly. In selected schools, students were also selected randomly.
Ethical concerns
Study protocols were reviewed and approved by ethics committees and other relevant national regulatory organizations was obtained after complete explanation of the study objectives and protocols for students and their parents, written informed consent was obtained from parents and oral assent from students, sampling and examinations and were begun.
Procedure and measurements
We prepared the questionnaires in Farsi based on and the WHO Global School Health Survey, and added some more questions to the questionnaires of parents. Questions were about family dietary habits, students’ past history, and familial history of chronic diseases. The validity of their content was affirmed based on observations of an experts’ panel and item analysis. Reliability measures were assessed based on a pilot study.
Under the supervision of expert health care professionals, the students filled out the self-administered questionnaire at school. A team of trained health care professionals recorded information in a checklist and conducted the examinations under standard protocol by using calibrated instruments. Weight was measured to the nearest 200 g in barefoot and lightly dressed condition. Body mass index (BMI) was calculated as weight (kg) divided by height squared (m2). Waist circumference (WC) was measured by a nonelastic tape to the nearest 0.2 cm at the end of expiration at the midpoint between the top of iliac crest and the lowest rib in standing position.
We used the WHO growth curves to define BMI categories, i.e., underweight as age and sex-specific BMI < -2 z-score, overweight as sex-specific BMI for age of > +1 z-score, and obesity as sex-specific BMI for > +2 z-score. Abdominal obesity was considered as WC to height ratio more than 0.5.
Statistical analysis
We used the SPSS for Windows software (version 16.0, SPSS, Chicago, IL) for statistical analyses, and P < 0.05 was considered as statistically significant.
RESULTS
This national survey was conducted among 5570 school students (2784 girls and 2786 boys) and one of their parents. Data of 5528 students (2726 girls and 2802 boys) were complete and are reported. The mean age of participants was 14.7 ± 2.4 years without significant difference in terms of gender. Overall, 69.37% of participants were from urban areas and 30.63% from rural areas. More than 90% of students were from public schools and the rest from private schools. Most students’ parents were literate; 97.8% of fathers and 98.2% of mothers had at least elementary literacy. The large number of students’ father was worker or employee (45.35%), whereas 90.7% of mothers were housewives. The characteristics of participants are presented in Table 1.
Table 1.
Characteristics of study participants: CASPIAN-III Study
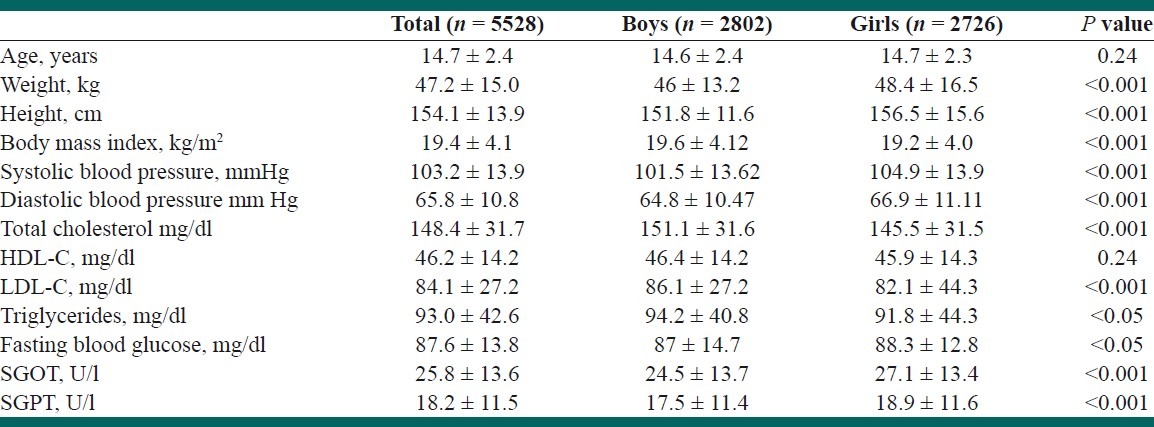
Overall, 17.3% (17.3% of girls and 17.5% of boys) were underweight, and 17.7% (15.5% of girls and 19.9% of boys) were overweight or obese. Abdominal obesity was documented in 16.3% of students (17.8% of girls and 15% of boys; 18.6% in urban and 11.2% in rural areas).
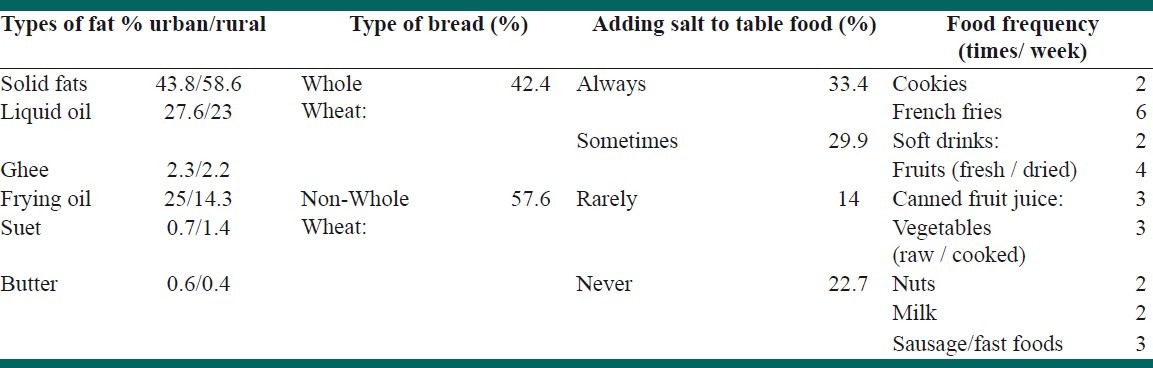
Table 2 shows some dietary habits of study participants. Bread is the staple food for Iranians, 42.4% of families consumed whole wheat bread, and the rest used breads prepared with white flour. Most families, i.e., 43.8% in urban areas and 58.6% in rural areas used solid fats for food preparation at home. 22.7% of students stated that they did not add salt to the table food.
Table 2.
Some dietary habits of study participants: CASPIAN-III Study
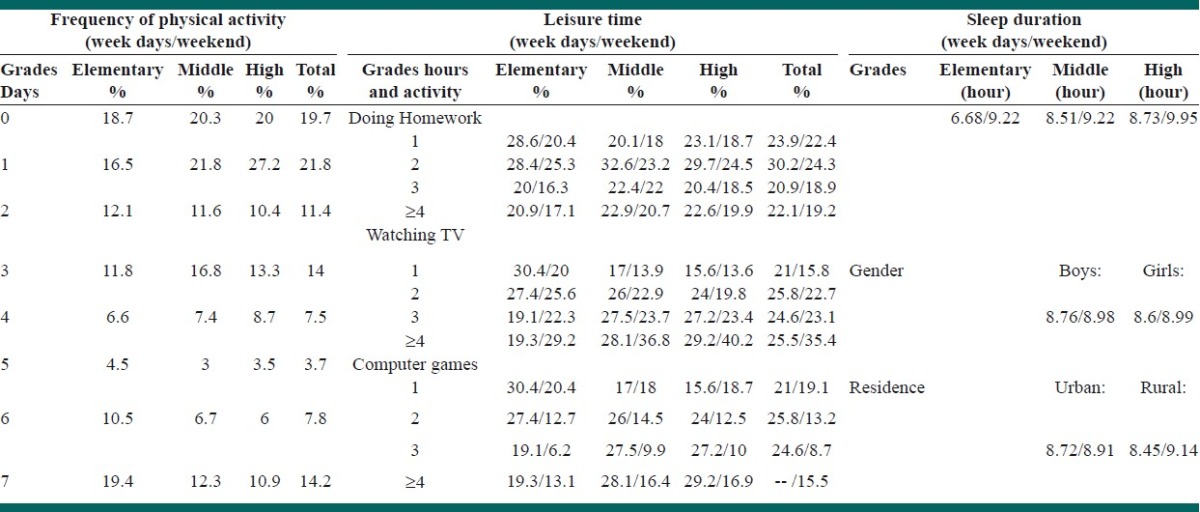
According to the students’ report, 14.2% of them had a regular daily physical activity for at least 30-min a day; 19.7% reported not to have any physical activity. Of students studied, 45% used computer in week days and 56.5% in weekends; these frequencies were higher in urban areas and among girls [Table 3].
Table 3.
Physical activity pattern of study participants: CASPIAN-III Study
Regarding passive smoking, 48.5% of students reported to have at least one cigarette smoker in their relatives, the corresponding figure was 33.9% for waterpipe. Overall, 10.4% of students (11.7% in urban areas and 7.3% in rural areas) reported that they used tobacco products, often waterpipe. 31% of participants mentioned that had at least an attempt of tobacco use. The mean age of the first attempt to smoke was 11.88 years.
Overall, 32.8% of students asserted that in the 3 months before the study, they experienced at least three times of bullying at school. Bullying was more frequent among girls than boys and decreased from elementary to high-school levels.
Regarding injuries, 14.46% of students (14.8% elementary, 15.2% middle, and 14% in high school) reported that during the year prior to the survey, they had suffered an injury needing the interference by school health providers. The prevalence of these injuries was higher in girls than in boys, and in rural than in urban areas. In the most cases, the injury type has been cuts and scratching, and 42.4% of injuries occurred when students were exercising, running, and/or jogging.
DISCUSSION
The findings of this national survey can serve for action-oriented policy making for health promotion of children and adolescents, as well as for primordial/primary prevention of chronic diseases.
Most students were in a good health condition; however, in most of the time, the lifestyle habits of families exposed them to chronic diseases in their future adulthood. Most families consumed hydrogenated solid fat and white-flour bread. Moreover, 80% of children and adolescents mentioned that they often add salt to their table food. Despite that youths’ taste have changed recently, and the preference for salty food has been escalated,[23,24] our findings were about double in comparison with Australian (10%–39%)[25] or Greek children (39%).[26]
Unhealthy eating habits among children and their families are considered as a problem for both developed and developing countries, which necessitate taking heed of needs for improvements in family and school food environments.[27–29]
In addition to some unhealthy dietary habits, the frequency and intensity of physical activity were low among children and adolescents. Girls’ activity was significantly lower than their boy peers. Furthermore, physical activity level was lesser in students of higher grades than in lower grades. Overall, the screen time, watching TV or computer games, was about 4 h a day, i.e., twice than the recommended time. Our findings are consistent with some other studies in showing low time allocated to physical activity among children and adolescents.[30,31]
Similar to the populations of most developing countries, in the current survey, we documented a dual burden of nutritional disorders in terms of underweight and overweight among Iranian children and adolescents. The epidemiologic transition with rapid changes in the habitual diet along with physical inactivity makes young individuals more susceptible to weight disorders.[32–34] Our findings also demonstrated a considerable prevalence of abdominal obesity, which even needs more attention for future chronic diseases.[35,36]
High blood pressure is another inevitable consequence of youths’ harmful lifestyles.[37,38] Principally, one of the leading causes of hypertension in this age group is the frequency of consuming fast food and solid hydrogenated fat.[39]
Many developing countries have encountered with dyslipidemia among children and adolescences, which can be justified by their sedentary lifestyle and high consumption of hydrogenated fat.[40–42] Thus, according to the association of dyslipidemia in childhood and its relation to the future cardiovascular morbidity and mortality,[43,44] encouraging healthy lifestyle from childhood is of crucial importance.
A large number of students were exposed to secondhand smoking; families should be aware of the hazards of their smoking habits on the health and the tendency of their children to begin smoking in the near future. Although the prevalence of self-reported smoking was lower than some other countries,[45–47] but these statistics deserve more consideration for preventive measures in this vulnerable age group, particularly because of the young age of begging to smoke at about 11 years.
Needless to say that exposure to violence and bullying is extremely likely to impose detrimental effects to the overall well-being and development of all youths. Moreover, to establish successful socioeconomic life and subsequently prosperous society, having a healthy educational system is essential. Our findings were consistent with studies conducted in some other countries.[48–50] Barriers to healthy lifestyles, e.g., physical activity, should be recognized in each community,[51] and facilities should be provided accordingly.
CONCLUSION
The current study documented important and preventable unhealthy lifestyle behaviors, which need proper attention both within the family and at school. Living a healthier life is every society's right, but it will not become true without amending the young's lifestyle and behavior. This survey is confirmatory evidence on the importance of establishing surveillance systems for risk behaviors to implement action-oriented interventions for primordial and primary prevention of chronic diseases.
ACKNOWLEDGEMENTS
The authors are thankful of the large team working on this study and all participants in different provinces.
Footnotes
Source of Support: This nationwide survey was funded by the Bureau of Population, Family, and School Health, Ministry of Health and Medical education in Iran.
Conflict of Interest: None declared.
REFERENCES
- 1.Brouqui P. Facing highly infectious diseases: New trends and current concepts. Clin Microbiol Infect. 2009;15:700–5. doi: 10.1111/j.1469-0691.2009.02873.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bannister B, Prygodzicz A, Ippolito G. Training health care workers to face highly infectious diseases. Clin Microbiol Infect. 2009;15:740–2. doi: 10.1111/j.1469-0691.2009.02872.x. [DOI] [PubMed] [Google Scholar]
- 3.de Haen H, Thompson B. Food security in a world without borders. Forum Nutr. 2003;56:375–9. [PubMed] [Google Scholar]
- 4.Fulton JE, Dai S, Steffen LM, Grunbaum JA, Shah SM, Labarthe DR. Physical activity, energy intake, sedentary behavior, and adiposity in youth. Am J Prev Med. 2009;37(1 Suppl):S40–9. doi: 10.1016/j.amepre.2009.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DiPietro L. Physical activity, body weight, and adiposity: An epidemiologic perspective. Exerc Sport Sci Rev. 1995;23:275–303. [PubMed] [Google Scholar]
- 6.Morabia A, Abel T. The WHO report “Preventing chronic diseases: A vital investment” and us. Soz Praventivmed. 2006;51:74. doi: 10.1007/s00038-005-0015-7. [DOI] [PubMed] [Google Scholar]
- 7.Lohse N, Ersboll C, Kingo L. Taking on the challenge of noncommunicable diseases: We all hold a piece of the puzzle. Int J Gynaecol Obstet. 2011;115(Suppl 1):S52–4. doi: 10.1016/S0020-7292(11)60016-7. [DOI] [PubMed] [Google Scholar]
- 8.Daar AS, Singer PA, Persad DL, Pramming SK, Matthews DR, Beaglehole R, et al. Grand challenges in chronic non-communicable diseases. Nature. 2007;450:494–6. doi: 10.1038/450494a. [DOI] [PubMed] [Google Scholar]
- 9.Nugent R. Chronic diseases in developing countries: Health and economic burdens. Ann N Y Acad Sci. 2008;1136:70–9. doi: 10.1196/annals.1425.027. [DOI] [PubMed] [Google Scholar]
- 10.Preventing chronic diseases: A vital investment. WHO. 2005. [Last accessed on April 2012]. [cited 2012]; Available from: http://www.who.int/chp/chronic_disease_report/en/
- 11.Freedman DS, Ogden CL, Berenson GS, Horlick M. Body mass index and body fatness in childhood. Curr Opin Clin Nutr Metab Care. 2005;8:618–23. doi: 10.1097/01.mco.0000171128.21655.93. [DOI] [PubMed] [Google Scholar]
- 12.Whitlock EP, Williams SB, Gold R, Smith PR, Shipman SA. Screening and interventions for childhood overweight: A summary of evidence for the US Preventive Services Task Force. Pediatrics. 2005;116:e125–44. doi: 10.1542/peds.2005-0242. [DOI] [PubMed] [Google Scholar]
- 13.Whitlock EA, O’Connor EP, Williams SB, Beil TL, Lutz KW. Effectiveness of weight management programs in children and adolescents. Evid Rep Technol Assess (Full Rep) 2008;(170):1–308. [PMC free article] [PubMed] [Google Scholar]
- 14.Kelishadi R, Pour MH, Zadegan NS, Kahbazi M, Sadry G, Amani A, et al. Dietary fat intake and lipid profiles of Iranian adolescents: Isfahan Healthy Heart Program-Heart Health Promotion from Childhood. Prev Med. 2004;39:760–6. doi: 10.1016/j.ypmed.2004.02.047. [DOI] [PubMed] [Google Scholar]
- 15.Ziaoddini H, Kelishadi R, Kamsari F, Mirmoghtadaee P, Poursafa P. First nationwide survey of prevalence of weight disorders in Iranian children at school entry. World J Pediatr. 2010;6:223–7. doi: 10.1007/s12519-010-0206-z. [DOI] [PubMed] [Google Scholar]
- 16.Kelishadi R, Ardalan G, Gheiratmand R, Majdzadeh R, Hosseini M, Gouya MM, et al. Caspian Study Group. Thinness, overweight and obesity in a national sample of Iranian children and adolescents: CASPIAN Study. Child Care Health Dev. 2008;34:44–54. doi: 10.1111/j.1365-2214.2007.00744.x. [DOI] [PubMed] [Google Scholar]
- 17.Kelishadi R, Pour MH, Sarraf-Zadegan N, Sadry GH, Ansari R, Alikhassy H, et al. Obesity and associated modifiable environmental factors in Iranian adolescents: Isfahan Healthy Heart Program - Heart Health Promotion from Childhood. Pediatr Int. 2003;45:435–42. doi: 10.1046/j.1442-200x.2003.01738.x. [DOI] [PubMed] [Google Scholar]
- 18.Hosseini-Esfahani F, Mousavi Nasl Khameneh A, Mirmiran P, Ghanbarian A, Azizi F. Trends in risk factors for cardiovascular disease among Iranian adolescents: The Tehran Lipid and Glucose Study, 1999-2008. J Epidemiol. 2011;21:319–28. doi: 10.2188/jea.JE20100162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rafraf M, Gargari BP, Safaiyan A. Prevalence of prehypertension and hypertension among adolescent high school girls in Tabriz, Iran. Food Nutr Bull. 2010;31:461–5. doi: 10.1177/156482651003100308. [DOI] [PubMed] [Google Scholar]
- 20.Global School-based Student Health Survey. Centers for Disease Control and Prevention (CDC) 2009. [Last accessed 2012 Feb 21]. [cited 2012]; Available from: http://www.cdc.gov/GSHS/
- 21.Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, et al. Youth risk behavior surveillance - United States, 2009. MMWR Surveill Summ. 2010;59:1–142. [PubMed] [Google Scholar]
- 22.Kelishadi R, Ardalan G, Gheiratmand R, Gouya MM, Razaghi EM, Delavari A, et al. Association of physical activity and dietary behaviours in relation to the body mass index in a national sample of Iranian children and adolescents: CASPIAN Study. Bull World Health Organ. 2007;85:19–26. doi: 10.2471/BLT.06.030783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim GH, Lee HM. Frequent consumption of certain fast foods may be associated with an enhanced preference for salt taste. J Hum Nutr Diet. 2009;22:475–80. doi: 10.1111/j.1365-277X.2009.00984.x. [DOI] [PubMed] [Google Scholar]
- 24.Drake SL, Lopetcharat K, Drake MA. Salty taste in dairy foods: Can we reduce the salt? J Dairy Sci. 2011;94:636–45. doi: 10.3168/jds.2010-3509. [DOI] [PubMed] [Google Scholar]
- 25.Grimes CA, Campbell KJ, Riddell LJ, Nowson CA. Sources of sodium in Australian children's diets and the effect of the application of sodium targets to food products to reduce sodium intake. Br J Nutr. 2011;105:468–77. doi: 10.1017/S0007114510003673. [DOI] [PubMed] [Google Scholar]
- 26.Adamopoulos PN, Chaniotis F, Kodoyianis S, Boutsicakis J, Madalos P, Kassos D, et al. Table salt and blood pressure in Greek children. J Hum Hypertens. 1987;1:209–13. [PubMed] [Google Scholar]
- 27.Fox MK, Gordon A, Nogales R, Wilson A. Availability and consumption of competitive foods in US public schools. J Am Diet Assoc. 2009;109(2 Suppl):S57–66. doi: 10.1016/j.jada.2008.10.063. [DOI] [PubMed] [Google Scholar]
- 28.Weker H. Simple obesity in children. A study on the role of nutritional factors. Med Wieku Rozwoj. 2006;10:3–191. [PubMed] [Google Scholar]
- 29.Langevin DD, Kwiatkowski C, McKay MG, Maillet JO, Touger-Decker R, Smith JK, et al. Evaluation of diet quality and weight status of children from a low socioeconomic urban environment supports “at risk” classification. J Am Diet Assoc. 2007;107:1973–7. doi: 10.1016/j.jada.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 30.Ridgers ND, Stratton G, Fairclough SJ. Physical activity levels of children during school playtime. Sports Med. 2006;36:359–71. doi: 10.2165/00007256-200636040-00005. [DOI] [PubMed] [Google Scholar]
- 31.Nader PR. Frequency and intensity of activity of third-grade children in physical education. Arch Pediatr Adolesc Med. 2003;157:185–90. doi: 10.1001/archpedi.157.2.185. [DOI] [PubMed] [Google Scholar]
- 32.Hodges EA. A primer on early childhood obesity and parental influence. Pediatr Nurs. 2003;29:13–6. [PubMed] [Google Scholar]
- 33.Schwartz MB, Puhl R. Childhood obesity: A societal problem to solve. Obes Rev. 2003;4:57–71. doi: 10.1046/j.1467-789x.2003.00093.x. [DOI] [PubMed] [Google Scholar]
- 34.Al-Hazzaa HM, Abahussain NA, Al-Sobayel HI, Qahwaji DM, Musaiger AO. Physical activity, sedentary behaviors and dietary habits among Saudi adolescents relative to age, gender and region. Int J Behav Nutr Phys Act. 2011;8:140. doi: 10.1186/1479-5868-8-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Korsic M, Fister K, Ivankovic D, Jelcic J. Visceral obesity. Lijec Vjesn. 2011;133:284–7. [PubMed] [Google Scholar]
- 36.Despres JP, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, et al. Abdominal obesity and the metabolic syndrome: Contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol. 2008;28:1039–49. doi: 10.1161/ATVBAHA.107.159228. [DOI] [PubMed] [Google Scholar]
- 37.Schutte AE, van Rooyen JM, Huisman HW, Kruger HS, Malan NT, De Ridder JH. Dietary risk markers that contribute to the aetiology of hypertension in black South African children: The THUSA BANA study. J Hum Hypertens. 2003;17:29–35. doi: 10.1038/sj.jhh.1001508. [DOI] [PubMed] [Google Scholar]
- 38.The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 Suppl):555–76. 4th Report. [PubMed] [Google Scholar]
- 39.Kelishadi R, Ardalan G, Gheiratmand R, Majdzadeh R, Delavari A, Heshmat R, et al. Blood pressure and its influencing factors in a national representative sample of Iranian children and adolescents: The CASPIAN Study. Eur J Cardiovasc Prev Rehabil. 2006;13:956–63. doi: 10.1097/01.hjr.0000219109.17791.b6. [DOI] [PubMed] [Google Scholar]
- 40.Yamada M, Wong FL, Kodama K, Sasaki H, Shimaoka K, Yamakido M. Longitudinal trends in total serum cholesterol levels in a Japanese cohort, 1958-1986. J Clin Epidemiol. 1997;50:425–34. doi: 10.1016/s0895-4356(96)00423-4. [DOI] [PubMed] [Google Scholar]
- 41.Li YH, Li Y, Davis CE, Chen Z, Tao S, Folsom AR, et al. Serum cholesterol changes from 1983-1984 to 1993-1994 in the People's Republic of China. Nutr Metab Cardiovasc Dis. 2002;12:118–26. [PubMed] [Google Scholar]
- 42.Esmaillzadeh A, Mirmiran P, Azadbakht L, Etemadi A, Azizi F. High prevalence of the metabolic syndrome in Iranian adolescents. Obesity (Silver Spring) 2006;14:377–82. doi: 10.1038/oby.2006.50. [DOI] [PubMed] [Google Scholar]
- 43.Haney EM, Huffman LH, Bougatsos C, Freeman M, Steiner RD, Nelson HD. Screening and treatment for lipid disorders in children and adolescents: Systematic evidence review for the US Preventive Services Task Force. Pediatrics. 2007;120:e189–214. doi: 10.1542/peds.2006-1801. [DOI] [PubMed] [Google Scholar]
- 44.Kavey RE, Daniels SR, Lauer RM, Atkins DL, Hayman LL, Taubert K. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. J Pediatr. 2003;142:368–72. doi: 10.1067/mpd.2003.205. [DOI] [PubMed] [Google Scholar]
- 45.Slama K, David-Tchouda S, Plassart JM. Tobacco consumption among young adults in the two French departments of Savoie in 2008. Rev Epidemiol Sante Publique. 2009;57:299–304. doi: 10.1016/j.respe.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 46.Befinoana M, Razanamihaja N. Prevalence of tobacco use and associated factors among teenage students in Madagascar. Sante Publique. 2011;23:465–74. [PubMed] [Google Scholar]
- 47.Qing Y, Termsirikulchai L, Vatanasomboon P, Sujirarat D, Tanasugarn C, Kengganpanich M. Factors related to tobacco use among middle school students in China. Southeast Asian J Trop Med Public Health. 2011;42:1249–61. [PubMed] [Google Scholar]
- 48.Lemstra M, Rogers M, Redgate L, Garner M, Moraros J. Prevalence, risk indicators and outcomes of bullying among on-reserve First Nations youth. Can J Public Health. 2011;102:462–6. doi: 10.1007/BF03404201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lemstra ME, Nielsen G, Rogers MR, Thompson AT, Moraros JS. Risk indicators and outcomes associated with bullying in youth aged 9-15 years. Can J Public Health. 2012;103:9–13. doi: 10.1007/BF03404061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dake JA, Price JH, Telljohann SK. The nature and extent of bullying at school. J Sch Health. 2003;73:173–80. doi: 10.1111/j.1746-1561.2003.tb03599.x. [DOI] [PubMed] [Google Scholar]
- 51.Kelishadi R, Ghatrehsamani S, Hosseini M, Mirmoghtadaee P, Mansouri S, Poursafa P. Barriers to Physical Activity in a Population-based Sample of Children and Adolescents in Isfahan, Iran. Int J Prev Med. 2010;1:131–7. [PMC free article] [PubMed] [Google Scholar]


