Abstract
Liver inflammatory pseudotumor (IPT) is considered a benign inflammatory lesion mostly presented as a solitary solid mass in the right hepatic lobe. It may clinically and radiologically mimic a malignant liver tumor or an abscess. Accordingly, diagnoses of most of the reported cases have been established after surgical resection. In this report, we describe a 52-year-old woman with a 1-year history of fever of unknown origin. In the following investigation, abdominal computed tomography (CT) scan showed infiltrative lesion in the right hepatic lobe. The patient underwent a CT-guided needle biopsy of the hepatic lesion. Histopathologic study of biopsy specimen revealed the features of IPT. The patient was discharged and followedup for 6 months. After 6 months she had no complaint of fever and control liver ultrasonography disclosed no lesion. As liver IPT has favorable response to conservative therapy and may also resolve spontaneously, precise recognition of this condition with the help of fine-needle biopsy may help to avoid unnecessary surgery.
Keywords: Fever of unknown origin, fine needle biopsy, inflammatory pseudotumor, radiology
INTRODUCTION
Inflammatory pseudotumor (IPT) is an uncommon benign lesion histologically defined as a localized mass consisting of dense fibrous tissue infiltrated by inflammatory cells.[1] Liver IPT may clinically and radiologically mimic malignant liver tumors.[2] Therefore, surgical resection and histopathologic study are often unavoidable for establishing the diagnosis. However, very few reported cases have been diagnosed by fine-needle biopsy.[2] The authors present a case of infiltrating liver IPT, which was diagnosed by fine-needle sampling and histopathologic examination.
CASE REPORT
A 52-year-old woman presented at our hospital (Alzahra Hospital, Isfahan University of Medical Sciences) for evaluation of fever of unknown origin. She had a 1-year history of intermittent fever, night sweating, and myalgia. Physical examination was normal. Following laboratory study showed leukocytes 16,000/μl (neutrophils 80%, lymphocytes 18%). The blood culture, urine culture, and stool culture were negative. Abdominal ultrasonography revealed diffuse hypodense lesions (7–15 mm) in the liver. Following abdominal computed tomography (CT) scan showed infiltrative lesion in the right hepatic lobe [Figure 1]. In the subsequent step, the patient underwent a CT-guided needle biopsy of hepatic lesions.
Figure 1.
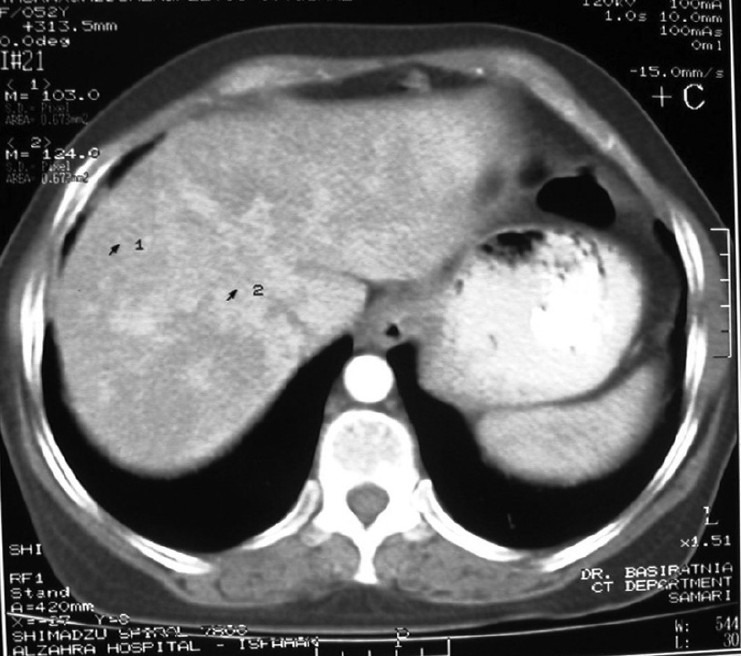
Abdominal computed tomography scan with contrast showing diffuse infiltrating lesion in right hepatic lobe
On microscopic evaluation of the biopsy specimen infiltration of chronic inflammatory cells and lymphoplasma cells in portal spaces with mild penetration to hepatocytes were seen. There was also lytic necrosis and confluent necrosis and dilatation of some portal spaces due to fibrosis. Tumor markers were all within normal range except for serum cancer antigen 19-9 (CA 19-9), which was slightly increased. HBs Ag, HBC IgM, HCV Ab, and HIV Ab were negative. She underwent an upper and lower gastrointestinal endoscopy to rule out the related malignancies. These findings were compatible with the diagnosis of liver IPT. The patient was discharged and an outpatient followup was arranged. After 6 months she had no complaint of fever or malaise and control liver ultrasonography disclosed no lesion.
DISCUSSION
Liver IPT is considered a benign inflammatory lesion,[3] mostly presented as a solitary solid mass in the right hepatic lobe.[4] Multifocal liver IPTs were also reported,[5,6] but infiltrating IPT, which was seen in the present case, is very rare.
Despite several theories suggesting the possible etiology of liver IPT, the exact etiology remains unknown.[7] Infectious agents, autoimmune factors, and inflammatory effect of the biliary steroid lithocholic acid are some of the suggested etiologies.[8,9] Patients may present with fever, upper abdominal pain, weight loss, and jaundice.[8,10] Liver IPT is an uncommon differential diagnosis of fever of unknown origin (FUO). However, as most of the cases of liver IPT, such as the present case, have been described with prolonged fever, this condition should be considered in differential diagnosis of all patients with FUO.[10]
Histopathologic features of IPTs include the presence of myofibroblastic spindle cells infiltrated by plasma cells and chronic inflammatory cells without cellular anaplasias or atypical mitoses.[4,7]
In our patient, the serum level of CA19-9 was raised. Interestingly, there are some evidences suggested that liver IPT itself may increase serum CA19-9.[2,3,11]
Ultrasound, CT scan, and magnetic resonance imaging of liver IPT have revealed various patterns, probably due to various proportions or the distribution of histologic components in different cases.[3,12] Liver IPT may also both clinically and radiologically mimic a hepatocellular carcinoma, cholangiocarcinoma, hepatic metastasis, or a liver abscess.[1,5,7] Accordingly, diagnoses of most of the reported cases were established after surgical resection.[2]
Diagnosis of liver IPT by fine-needle biopsy, which was carried out in the present case is very beneficial.[2,3,8] Indeed, with the help of clinical manifestations, imaging findings, level of serum tumor markers, and results of histopathologic examination of specimens obtained from fine-needle biopsy, we may reach to the diagnosis of liver IPT.
Following the diagnosis, as the liver IPT has a favorable response to conservative therapy and may also resolve spontaneously, followup or conservative therapy should be the first line of management.[2] Antibiotics, nonsteroidal anti-inflammatory drugs, steroids, and biliary drainage are the options of conservative therapy.[3] This strategy may help to avoid unnecessary surgery. Surgical resection should be reserved for cases where the diagnosis is uncertain, the patient does not respond to conservative therapy, or in the presence of severe complications.[2,3,13]
In conclusion, liver IPT should be considered in the differential diagnosis of both FUO and mass lesions of the liver. After proper evaluation for exclusion of malignancy, followup or conservative therapy should be the first line of management, and surgical resection should be reserved for uncertain diagnosis or failure of conservative therapy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Deng FT, Li YX, Ye L, Tong L, Yang XP, Chai XQ. Hilar inflammatory pseudotumor mimicking hilar cholangiocarcinoma. Hepatobiliary Pancreat Dis Int. 2010;9:219–21. [PubMed] [Google Scholar]
- 2.Sari A, Tunakan M, Unsal B, Ekinci N, Rezanko T, Elcin F, et al. Inflammatory pseudotumor of the liver diagnosed by needle biopsy: Report of three cases (one with neuroendocrine tumor of the rectum and lung) Turk J Gastroenterol. 2010;21:308–12. doi: 10.4318/tjg.2010.0107. [DOI] [PubMed] [Google Scholar]
- 3.Tsou YK, Lin CJ, Liu NJ, Lin CC, Lin CH, Lin SM. Inflammatory pseudotumor of the liver: Report of eight cases, including three unusual cases, and a literature review. J Gastroenterol Hepatol. 2007;22:2143–7. doi: 10.1111/j.1440-1746.2006.04514.x. [DOI] [PubMed] [Google Scholar]
- 4.Ueda J, Yoshida H, Taniai N, Onda M, Hayashi H, Tajiri T. Inflammatory pseudotumor in the liver associated with intrahepatic bile duct stones mimicking malignancy. J Nihon Med Sch. 2009;76:154–9. doi: 10.1272/jnms.76.154. [DOI] [PubMed] [Google Scholar]
- 5.Chong A, Jeong SY, Min JJ. Inflammatory pseudotumours resembling multiple hepatic metastases and their complete regression, as revealed by 18F-FDG PET/CT. Eur J Nucl Med Mol Imaging. 2009;36:1199–200. doi: 10.1007/s00259-009-1132-y. [DOI] [PubMed] [Google Scholar]
- 6.Brage-Varela A, Estevez-Boullosa P, Pombo-Otero J, Blanco-Rodriguez M, Lago-Novoa M, Arnal-Monreal F. Multifocal hepatic inflammatory pseudotumor: Spontaneous regression in a diabetic patient. Rev Esp Enferm Dig. 2010;102:507–9. doi: 10.4321/s1130-01082010000800012. [DOI] [PubMed] [Google Scholar]
- 7.Milias K, Madhavan KK, Bellamy C, Garden OJ, Parks RW. Inflammatory pseudotumors of the liver: Experience of a specialist surgical unit. J Gastroenterol Hepatol. 2009;24:1562–6. doi: 10.1111/j.1440-1746.2009.05951.x. [DOI] [PubMed] [Google Scholar]
- 8.Faraj W, Ajouz H, Mukherji D, Kealy G, Shamseddine A, Khalife M. Inflammatory pseudo-tumor of the liver: A rare pathological entity. World J Surg Oncol. 2011;9:5. doi: 10.1186/1477-7819-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geramizadeh B, Tahamtan MR, Bahador A, Sefidbakht S, Modjalal M, Nabai S, et al. Inflammatory pseudotumor of the liver: Two case reports and a review of the literature. Indian J Pathol Microbiol. 2009;52:210–2. doi: 10.4103/0377-4929.48920. [DOI] [PubMed] [Google Scholar]
- 10.Fisher RG, Wright PF, Johnson JE. Inflammatory pseudotumor presenting as fever of unknown origin. Clin Infect Dis. 1995;21:1492–4. doi: 10.1093/clinids/21.6.1492. [DOI] [PubMed] [Google Scholar]
- 11.Ogawa T, Yokoi H, Kawarada Y. A case of inflammatory pseudotumor of the liver causing elevated serum CA19-9 levels. Am J Gastroenterol. 1998;93:2551–5. doi: 10.1111/j.1572-0241.1998.00717.x. [DOI] [PubMed] [Google Scholar]
- 12.Kawaguchi T, Mochizuki K, Kizu T, Miyazaki M, Yakushijin T, Tsutsui S, et al. Inflammatory pseudotumor of the liver and spleen diagnosed by percutaneous needle biopsy. World J Gastroenterol. 2012;18:90–5. doi: 10.3748/wjg.v18.i1.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goldsmith PJ, Loganathan A, Jacob M, Ahmad N, Toogood GJ, Lodge JP, et al. Inflammatory pseudotumours of the liver: A spectrum of presentation and management options. Eur J Surg Oncol. 2009;35:1295–8. doi: 10.1016/j.ejso.2009.04.003. [DOI] [PubMed] [Google Scholar]


