Abstract
Objective
GPs’ role conflict in connection with sickness certification is widely accepted. The authors explored the relationship between GPs and this difficult task.
Design
Cross-sectional questionnaire study of experiences, attitudes, and management of sickness certification. Data were analysed by hierarchical cluster analysis.
Setting
Norway.
Subjects
Representative sample of 308 general practitioners from a nationwide panel established by the Research Institute of the Norwegian Medical Association.
Main outcome measures
Differentiation of response patterns regarding perceived burden, self-evaluation, doubt, permissiveness, opinions on whether sickness certification is a medical task, and sociopolitical attitude. Associations with hours of patient contact per week, number of sickness certifications per week, job satisfaction, degree of paternalism, and personality characteristics.
Results
Four groups evolved, one (12%) with low burden, high self-esteem, little doubt, and permissiveness, another (12%) with the opposite characteristics. They displayed similar sociopolitical attitudes. The third group (32%) was primarily characterized by a biomedical attitude, while the fourth represented a middle position in all dimensions. The first two groups differed on personality characteristics. There were no differences between groups regarding number of sickness certifications per week, job satisfaction, or degree of paternalism.
Conclusions
Prominent differences in experiences with sickness certification between groups of doctors exist. No evidence was found of associations between group-level GP differences and sickness certification rates.
Keywords: Doctor behaviour, family practice, general practitioner, sickness certification, survey
General practitioners’ relationship to the sickness certification task has not been explored in representative samples.
Two groups with similar sociopolitical attitudes to sickness certification responded oppositely to the task: one was heavily burdened, the other content with high self-esteem.
A third group displayed a more biomedical attitude than the other two.
Sickness certification is part of medical work in European welfare states and is an everyday task of general practitioners (GPs). The task is complex and difficult, and many GPs would like to relinquish this gatekeeper role [1]. They complain that it conflicts with the traditional ethics of patient advocacy [1], [2]. Much pressure has been put on doctors to act restrictively [3]. Doctors feel blamed if they do not, feel that this threatens the doctor–patient relationship, and perceive loss of professional and personal control [1], [4]. GPs often find it difficult to judge patients’ capacity for work [2]. Some doctors admit the exaggeration of severity of patients’ conditions, and admit to having changed diagnoses and reported non-existent signs or symptoms to help their patients [1], [5]. Such strategies are not particular to sickness certifications. US doctors are reported to use deception and manipulation when acting as gatekeepers, in order to help patients manage financially [6], [7].
GPs’ views on sickness certification vary. A UK study concluded that some GPs would prefer to have no role at all in sickness certification; others value the task [2]. This qualitative study could not indicate how widespread such opinions are. We thought that there might be associations between negative experiences, opinions, and certain characteristics of the doctors, but could not find studies that had explored this. One earlier study from Norway found no association between the attitudes of GPs and their actual sickness certification practice [8]. A comprehensive literature study concluded that we do not have valid information about how physician-related factors influence sickness certification [9].
In a nationwide representative sample of doctors, we aimed to identify groups of general practitioners with similar experiences of the gatekeeper role in sickness certification. We sought information on opinions and ways of handling sickness certification and gatekeeping. Finally, we explored associations with job satisfaction, paternalistic style, personality, and frequency of sickness certification of patients.
Material and methods
A representative sample [10] of 1605 Norwegian doctors received a questionnaire in June 2002; non-responders were reminded once. We collected information on job satisfaction, personality, and degree of paternalism using established instruments. The Job Satisfaction Scale (JSS) of Warr et al. consists of 10 items that form a summated score (scale 10–70, with 70 as maximum job satisfaction) [11]. We used a short form of Eysenck's personality inventory [12] consisting of two of the subscales, the extroversion–introversion scale (0–10, with 10 as maximum extroversion) and the neuroticism scale (0–10, with 10 as maximum neuroticism). The short form was developed in an empirical dataset [13] using stepwise linear regression analyses with the original scores as dependent variables. The estimated correlations with the original scores were 0.94 for the extroversion–introversion scale and 0.95 for the neuroticism scale. The measure of paternalistic style originates from a 16-item instrument, of which five items are sufficient to map the degree of paternalism (scale 0–20, with 20 as maximum paternalism) [14]. The doctors’ experiences of gatekeeping in general and sickness certification in particular were mapped by 29 items, which are listed in Table I. Five of the questions were derived from a previous study [8]. We also asked about the average hours of patient contact per week and approximate average of sick leave certifications per week. Doctors reporting to work as GPs with a patient list were included in the analysis.
Table I.
List of items: Numbers refer to their sequence in the questionnaire.
| 5-point Likert-scale items (1 = completely disagree to 5 = completely agree) | Dimension | |
| 1.1 | Control tasks have not been a problem for me in practice | Burden (inverted) |
| 1.2 | I have often doubted whether my decisions are consistent with the intent of the relevant regulations | Doubt |
| 1.3 | If I am in doubt, the patient's view most often determines what I write | Permissiveness |
| 1.4 | Having control tasks as a doctor often feels like a personal burden | Burden |
| 1.5 | The times I have been strict, patients have just gone to another doctor | Observed events |
| 1.6 | Having control tasks as a doctor has been meaningful medical work for me | Burden (inverted) |
| 1.7 | I have often experienced that patients withhold information that is important for my decision | (not in dimension) |
| 3.1 | It should be allowed to give patients sick leave based on social indications, for example due to a spouse's illness | Sociopolitical attitude |
| 3.2 | Because of special problems that unemployed patients have, doctors should give them sick leave more easily than others | (not in dimension) |
| 3.3 | The patient should be examined personally by the doctor when sick leave is extended | Medical task |
| 3.4 | Telephone consultations are almost always medically justifiable for filling out a sick leave form | Medical task (inverted) |
| 3.5 | The patient's request for sick leave should be the most important consideration when the doctor fills out a sick leave form | Permissiveness |
| 3.6 | Sick leave is an important treatment alternative | Medical task |
| 3.7 | Decisions about sick leave often give me the feeling of being in conflict with my role as a helper | Burden |
| 3.8 | The simplified functional evaluation is determined entirely on information from the patient | Permissiveness |
| 3.9 | Filling out sick leave forms is a medical task | Medical task |
| 3.10 | Other health personnel besides doctors should not be allowed to make decisions about sick leave | Medical task |
| 3.11 | If a patient with cancer is unable to work because of depression, anxiety or unrest, I prefer to use cancer as the diagnosis on the sick leave form | (not in dimension) |
| 3.12 | If I am in doubt about which diagnosis to write on a sick leave form, I let the patient decide this | Permissiveness |
| 3.13 | I am not knowledgeable enough about examining the musculoskeletal system to be able to make a correct diagnosis | Self-evaluation (inverted) |
| 3.14 | I am not good at handling people with mental or social problems | Self-evaluation (inverted) |
| 3.15 | Filling out sick leave forms is a moral task | Medical task (inverted) |
| 3.16 | Sick leave is a matter for the workplace and it is unnecessary to involve doctors | Medical task (inverted) |
| 3.17 | I am less strict in practice than I think I should be in relationship to sick leave | Self-evaluation (inverted) |
| 2.4 | Do you experience that filling out a sick leave form is a positive or a negative task? (1 = negative −5 = positive) | Burden (inverted) |
| 2.5 | Do you feel that filling out a sick leave form is a meaningful task? (1 = not meaningful −5 = meaningful) | Burden (inverted) |
| Frequencies (never, monthly, weekly, daily) | ||
| 2.1 | How often are you in doubt whether to grant sick leave? | Doubt |
| 2.2 | How often are you in doubt about how long to grant sick leave for? | Doubt |
| 2.3 | How often do you meet patients who do not want be granted sick leave, even if you recommend it? | Observed events |
We used hierarchical cluster analysis [15] to identify relatively homogeneous groups of GPs based on response patterns. A dissimilarity matrix was computed using squared Euclidean distance and clustering done by Ward's method [16]. Comparisons of identified groups were made using a Kruskal–Wallis test, as many of the scale variables did not show normal distributions. Items were amalgamated to express perceived burden, self-evaluation, doubt, permissiveness, opinions on medicine's role, sociopolitical attitude (one single item), and observed events (see Table I). Except for the latter two, Cronbach's alpha and item-to-total correlations were calculated. Differences between the groups were checked using a Kolmogorov–Smirnov test. Forward stepwise logistic regression was used to detect items sufficient to separate doctors into groups.
Results
A total of 1168 (73%) of 1605 doctors responded to the questionnaire. They did not differ significantly from non-responders as regards age and sex. Among doctors who answered the questionnaire, 308 were general practitioners. Missing values, comprising 0.8% of all item values, were substituted using bootstrap [17]. For age, hours of patient contact per week, and number of sickness certifications per week, the distribution was approximately normal; for the other scale variables it was not.
We identified four groups with 38 (12% – group A), 37 (12% – B), 98 (32% – C), and 135 (44% – D) GPs. Group A differed most from the rest, followed by group B. Group D did not present outlier positions on any item and is not presented further (data not shown). The groups were not significantly different as regards percentage of female doctors, age, paternalistic style, job satisfaction, hours of patient contact per week, or reported number of sick leave certifications per week (Table II). Group B scored significantly lower on the extroversion–-introversion scale and significantly higher on the neuroticism scale.
Table II.
Characteristics of groups A, B, C, and D
| Groups |
All |
|||||
| A (n = 38) | B (n = 37) | C (n = 98) | D (n = 135) | n = 308 | ||
| Mean (SD) Mean rank | Mean (SD) Mean rank | Mean (SD) Mean rank | Mean (SD) Mean rank | Kruskal–Wallis H (p-value) | Mean (SD) | |
| Females (%) | 1.851 | |||||
| 27.4 | 24.3 | 36.8 | 26.5 | (0.67) | 27.9 | |
| Age | 50.21 (8.23) | 45.08 (8.54) | 46.72 (8.30) | 47.67 (8.31) | 7.02 | |
| 181.53 | 131.78 | 146.58 | 158.87 | (0.07) | 47.4 (8.4) | |
| Hours of patient contact per week | 30.61 (8.53) | 31.48 (6.68) | 30.86 (6.99) | 29.88 (7.51) | 1.54 | |
| 158.14 | 162.37 | 157.99 | 146.63 | (0.67) | 30.4 (7.4) | |
| Number of sick leaves granted per week | 18.71 (10.70) | 22.84 (11.77) | 18.38 (9.22) | 19.88 (13.90) | 4.78 | |
| 148.08 | 183.48 | 147.54 | 149.77 | (0.19) | 19.7 (12.1) | |
| Job satisfaction | 54.66 (7.56) | 51.24 (8.30) | 52.45 (9.62) | 52.52 (8.69) | 2.80 | |
| 172.32 | 138.05 | 153.43 | 154.77 | (0.42) | 52.6 (8.8) | |
| Degree of paternalism | 8.74 (4.01) | 7.78 (3.35) | 7.80 (3.87) | 8.50 (3.60) | 3.26 | 8.2 |
| 167.34 | 147.15 | 143.48 | 160.90 | (0.35) | (3.7) | |
| Extroversion–introversion | 7.34 (2.45) | 5.68 (2.72) | 7.09 (2.71) | 6.78 (2.79) | 8.44 | 6.8 |
| 169.45 | 118.18 | 163.84 | 153.47 | (0.04) | (2.8) | |
| Neuroticism | 2.29 (2.05) | 4.00 (2.60) | 3.03 (2.30) | 2.91 (2.33) | 9.45 | 3.0 |
| 127.55 | 189.04 | 156.35 | 151.27 | (0.02) | (2.4) | |
1Chi-squared.
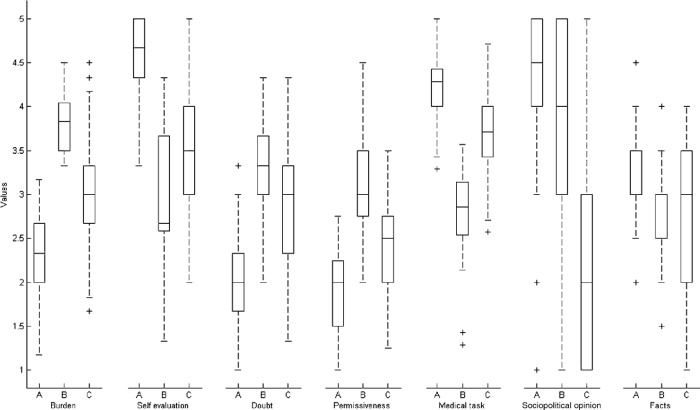
The groups were, with the exception of observed events and sociopolitical attitude, significantly different on all dimensions (Table III, Figure 1). Group C was clearly against sickness certification on social grounds, while groups A and B favoured this. On all other dimensions groups A and B differed the most. Group A displayed low perceived burden, very high self-evaluation, little doubt and low permissiveness. They stated clearly that sickness certification is a medical task. Group B were burdened, had comparatively low self-evaluation, much doubt, were quite permissive and very uncertain whether sickness certification is a medical task. Group C (and of course, group D) responded somewhere in between. Items that described concrete patient behaviour did not differ between the groups. The Cronbach's alpha of the dimensions ranged from 0.48 to 0.64. The item-to-total correlations were higher than 0.50 for all but three items.
Table III.
Responses in groups A, B, and C. Higher scores mean more perceived burden, better self-evaluation, more doubt, more permissive management, more clear that sickness certification is a medical task, more liberal sociopolitical attitude, and higher frequency of observed events.
| Groups |
Discriminating ability (rank) |
|||||
| A (n = 38) | B (n = 37) | C (n = 98) | A–B | A–C | B–C | |
| Dimension | Median (25th;75th) Mean rank | Median (25th;75th) Mean rank | Median (25th;75th) Mean rank | (p-value1) rank | (p-value1) rank | (p-value1) rank |
| Burden | 2.33 | 3.83 | 3.00 | 4.33 | 2.44 | 3.76 |
| (2.00; 2.67) | (3.50; 4.08) | (2.63; 3.33) | (< 0.001) | (< 0.001) | (< 0.001) | |
| 58.59 | 266.91 | 143.75 | 1 | 4 | 1 | |
| Self-evaluation | 4.67 | 2.67 | 3.50 | 3.42 | 3.15 | 1.55 |
| (4.33;5.00) | (2.50; 3.67) | (3.00; 4.00) | (< 0.001) | (< 0.001) | (0.016) | |
| 262.72 | 88.14 | 143.55 | 3 | 2 | 6 | |
| Doubt | 2.00 | 3.33 | 3.00 | 3.28 | 2.70 | 1.83 |
| (1.67; 2.33) | (3.00; 3.67) | (2.33; 3.33) | (< 0.001) | (< 0.001) | (0.002) | |
| 61.45 | 228.86 | 164.95 | 4 | 5 | 5 | |
| Permissiveness | 2.00 | 3.00 | 2.50 | 3.18 | 1.90 | 2.01 |
| (1.50; 2.25) | (2.75; 3.50) | (2.00; 2.75) | (< 0.001) | (0.001) | (0.001) | |
| 74.05 | 233.61 | 142.17 | 5 | 6 | 4 | |
| Medical task | 4.29 | 2.86 | 3.71 | 3.87 | 2.25 | 3.16 |
| (3.96; 4.46) | (2.50; 3.14) | (3.43; 4.04) | (< 0.001) | (< 0.001) | (< 0.001) | |
| 243.92 | 51.59 | 171.93 | 2 | 3 | 2 | |
| Sociopolitical attitude | 4.50 | 4.00 | 2.00 | 0.41 | ||
| (4.00; 5.00) | (3.00; 5.00) | (1.00; 3.00) | (0.996) | 3.27 (< 0.001) | 2.95 (< 0.001) | |
| 195.03 | 175.96 | 78.13 | 7 | 1 | 3 | |
| Observed events | 3.00 | 3.00 | 3.00 | 1.17 | 0.71 | |
| (2.88; 3.50) | (2.50; 3.00) | (2.00; 3.50) | 0.85 (0.470) | (0.132) | (0.692) | |
| 184.08 | 151.36 | 158.62 | 6 | 7 | 7 | |
1Kolmogorov–Smirnov test.
Figure 1.
Boxplots of scores for groups A, B, and C. Median, interquartile range, outliers, and range after excluding outliers. Higher scores mean more burden, better self-evaluation, more doubt, more permissive management, more clear that sickness certification is a medical task, more liberal sociopolitical attitude, and higher frequency of observed events.
Item 3.16 (see Table I) was sufficient to separate 97% of group A and B doctors; adding item 3.17 separated these groups completely (see Table III). Items 1.3, 3.1, 3.9, and 3.16 separated 94% of group B and C doctors; three more items were necessary to separate theses groups completely (1.1, 3.3, 3.17). Groups A and C needed seven items to discriminate 94% of them (1.2, 2.4, 3.1, 3.8, 3.15, 3.16, 3.17), and another two (1.7, 3.13) to do so completely.
Discussion
We have identified three groups with distinct response patterns differing from the majority of GPs. These patterns describe how substantial groups of GPs relate to sickness certification and gatekeeping in general. The most distinct group is characterized by professional self-confidence, firm ways of handling sickness certification, and by being in favour of allowing sickness certification on purely social grounds. An equally large group – with the same sociopolitical attitude – consists of less confident, more permissive doctors who feel more burdened by these tasks. A third larger group is primarily distinguished by being clearly against allowing sickness certification on social grounds. Hiscock & Ritchie describe a group of GPs that value their role in sickness certification and want to retain it as part of holistic thinking [10]. This group resembles our group A. In this British study, another group of doctors that would prefer to have no role in sickness certification argued that it created dilemmas for the patient–doctor relationship, and that it was not a core part of what they wanted and were trained to do (medicine). These are points of view that fit with our groups B and C, respectively. The opinions of group C doctors fit their biomedical position; the role of the GP is obvious, if sickness certifications were applicable only to well-defined diseases only. Their experiences of sickness certification are mixed, but their firm biomedical anchoring seems to protect them from doubt, feeling burdened or being tempted to use deceptions. Group B doctors seem to be striving. Their wish to liberalize allowable reasons for sickness certification might derive from this frustration, but it could also be that their sociopolitical attitude does not go well with certain personalities and leads to more distress when meeting dilemmas.
Despite their differences, we find that the three groups of GPs report similar practices, having on average the same amount of patient contact and number of sickness certifications per week. Their responses on observed events are also similar. This is in line with the findings in a study by Tellnes et al. from 1985, in which associations between attitudes of GPs and their actual sickness certification practice were not found [8]. This could imply that quite different personal experiences of the dilemmas of sickness certification do not lead to substantial differences in practice. One must, however, bear in mind that we could not study the actual sickness certification practices of these doctors (as the panel under study had not given consent to being identified by the researchers). But our study and Tellnes's study point in the same direction. We suggest that the most likely reason is that it is the individual patient's situation (and possibly the nature of the doctor–patient relationship) that decides what the GP does, more than his attitude, opinion, or experiences. The literature gives weak support for the effect of patient factors [9]. A recent Swedish study suggests that correlation between the GP's length of experience (and the strongly correlated variable GP age) and the proportion of patients certified sick [18]. We could not reproduce this finding in our dataset (data not shown). Their study was based on practice registration. The contrast reminds us that indirect measures should be interpreted with caution.
One main limit of the study is that it is cross-sectional and cannot address questions of causality. Our sample is representative of Norwegian general practitioners [10]. Patients in general practice in Norway are similar to those in other European countries regarding age and sex, and GPs are not very different from those in other Northern European countries regarding years in practice or hours of work per week [19]. A list system similar to the system in the UK and Denmark was introduced in Norway in 2001 [20]. The maximum of 2500 patients allowed on one GP's list is below the UK average, but the challenges of gatekeeping are nevertheless similar [1–3], [20–22]. Since the regulation of short- and long-term sickness certification tasks tends to differ between countries, and we do not have data on this, we would be reluctant to claim validity outside Norway. Nevertheless, the scales we have used for the characterization of the GPs are widely used and it would be interesting to see if the results could be replicated elsewhere.
We chose hierarchical cluster analysis because we did not have any a priori expectations concerning the data structure. The pitfall of this method is that one draws borders between not predefined numbers of sets of individuals that overlap to some extent. Small adjustments could lead to some individuals being moved from one group to another. We judged the validity of the analysis mainly in two ways: that the identified groups made sense (e.g. it was possible to place them in a reasonable way in light of the literature), and that the subsequent regression analysis worked. In this case, not many variables were needed to separate the groups, which supports the conclusions we have made.
Our questionnaire clearly identifies a small group of GPs that might profit from external support, as suggested by some doctors in the study by Hiscock & Ritchie [10]. In fact, a shortened version with 13 items would discriminate sufficiently from the rest the three groups described. One possible intervention could be to let more contented doctors function as mentors for their frustrated colleagues. Such an intervention could be led by national medical associations in order to support striving colleagues. But the purpose of this should not be to reduce sickness certification rates, only to alleviate the sickness certification burden felt by some GPs. With this in mind, there is reason to debate whether sickness certification is a reasonable task for doctors at all.
References
- 1.Hussey S, Hoddinott P, Wilson P, Dowell J, Barbour R. Sickness certification system in the United Kingdom: Qualitative study of views of general practitioners in Scotland. BMJ. 2004;328:88. doi: 10.1136/bmj.37949.656389.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hiscock J. Ritchie J. London: Department of Work and Pensions; 2001. The role of GPs in sickness certification. Research report No 148. [Google Scholar]
- 3.Nilsson B, Heath I. Patients, doctors, and sickness benefit. BMJ. 2003;327:1057. [Google Scholar]
- 4.Gulbrandsen P. Førde R. Aasland OG. Hvordan har legen det som portvakt? [What does it feel like to be a gatekeeper?] Tidsskr Nor Laegeforen. 2002;122:1874–9. (in Norwegian, summary in English) [PubMed] [Google Scholar]
- 5.Gulbrandsen P. Førde R. Aasland OG. Legeattester for å hjelpe pasienten. [Medical certificates issued to help the patient.] Tidsskr Nor Lægeforen. 2004;124:192–4. (in Norwegian, summary in English) [PubMed] [Google Scholar]
- 6.Freeman VG, Rathore SS, Weinfurt KP, Schulman KA, Sulmasy DP. Lying for patients: Physician deception of third-party payers. Arch Intern Med. 1999;159:2263–70. doi: 10.1001/archinte.159.19.2263. [DOI] [PubMed] [Google Scholar]
- 7.Wynia MK, Cummins DS, VanGeest JB, Wilson IB. Physician manipulation of reimbursement rules for patients: Between a rock and a hard place. JAMA. 2000;283:1858–65. doi: 10.1001/jama.283.14.1858. [DOI] [PubMed] [Google Scholar]
- 8.Tellnes G, Sandvik L, Moum T. Inter-doctor variation in sickness certification. Scand J Prim Health Care. 1990;8:45–52. doi: 10.3109/02813439008994928. [DOI] [PubMed] [Google Scholar]
- 9.Wahlström R, Alexanderson K. Physicians’ sick-listing practices. Scand J Public Health. 2004;32:222–55. doi: 10.1080/14034950410021916. [DOI] [PubMed] [Google Scholar]
- 10.Aasland OG, Olff M, Falkum E, Schweder T, Ursin H. Health complaints and job stress in Norwegian physicians: The use of an overlapping questionnaire design. Soc Sci Med. 1997;45:1615–29. doi: 10.1016/s0277-9536(97)00093-2. [DOI] [PubMed] [Google Scholar]
- 11.Warr P, Cook J, Wall P. Scales for the measurements of some work attitudes and aspects of psychological well-being. J Occup Psychology. 1979;52:129–48. [Google Scholar]
- 12.Eysenck HJ, Eysenck SBG. Manual of the EPQ. London: Hodder & Stoughton; 1975. [Google Scholar]
- 13.Tambs K, Sundet JM, Eaves L, Solaas MH, Berg K. Pedigree analysis of Eysenck Personality Questionnaire (EPQ) scores in monozygotic (MZ) twin families. Behav Genet. 1991;21:369–82. doi: 10.1007/BF01065973. [DOI] [PubMed] [Google Scholar]
- 14.Falkum E, Førde R. Paternalism, patient autonomy, and moral deliberation in the physician–patient relationship: Attitudes among Norwegian physicians. Soc Sci Med. 2001;52:239–48. doi: 10.1016/s0277-9536(00)00224-0. [DOI] [PubMed] [Google Scholar]
- 15.Everitt BS. Cluster analysis3rd ed. London: Edward Arnold; 1993. [Google Scholar]
- 16.Ward JH. Hierarchical grouping to optimise an objective function. J Am Stat Association. 1963;58:236–44. [Google Scholar]
- 17.Efron B, Tibshirani RJ. An introduction to the bootstrap. London: Chapman & Hall; 1993. [Google Scholar]
- 18.Norrmén G, Svärdsudd K, Andersson D. Impact of physician-related factors on sickness certification in primary health care. Scand J Prim Health Care. 2006;24:104–9. doi: 10.1080/02813430500525433. [DOI] [PubMed] [Google Scholar]
- 19.Wensing M, Vedsted P, Kersnik J, Peersman W, Klingenberg A, Hearnshaw H, et al. Patient satisfaction with availability of general practice: an international comparison. Int J Qual Safe Health Care. 2002;14:111–18. doi: 10.1093/oxfordjournals.intqhc.a002597. [DOI] [PubMed] [Google Scholar]
- 20.Carlsen B, Norheim F. Introduction of the patient-list system in general practice: Changes in Norwegian physicians’ perception of their gatekeeper role. Scand J Prim Health Care. 2003;21:209–13. doi: 10.1080/02813430310004155. [DOI] [PubMed] [Google Scholar]
- 21.Weinstein MC. Should physicians be gatekeepers of medical resources? J Med Ethics. 2001;27:268–74. doi: 10.1136/jme.27.4.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Willems DL. Balancing rationalities: Gatekeeping in health care. J Med Ethics. 2001;27:25–9. doi: 10.1136/jme.27.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]