Abstract
Occupationally exposed workers, farm workers and plant protection agents in the Sahel region of Burkina Faso were interviewed to assess adverse health effects of insecticides. The subjects were also examined for changes in both hematological and biochemical parameters. The prevalence of liver and kidney dysfunction was found to be quite high among insecticide applicators, especially among plant protection agents. The prevalence of biochemical alterations seems to be correlated to the frequency of insecticide use. However, no significant differences were found between the hematological parameters among farm workers and plant protection agents. The hematological parameters of all the insecticide applicators were normal. The great majority of insecticide applicators (85%) reported symptoms related to insecticide exposure. The use of insecticides in the agriculture of Burkina Faso is threatening to human health.
Keywords: occupational exposure, insecticides, hepatotoxicity, nephrotoxicity, symptoms
Introduction
In developing countries, the losses of crops due to pests, plant diseases, and competition from weeds are great. Plant losses of the order of 40–75% have been reported, with the locust being one of the major pests responsible for losses (Clarke et al., 1997). One of the strategies to increase crop productivity is effective pest management. In tropical and developing countries like Burkina Faso, crop loss is even more severe because the prevailing high temperature and humidity are highly conductive to rapid multiplication of pests (Kannan et al., 1992). Thus, the application of a wide variety of insecticides on crop plants is necessary in the tropics to combat pests. Due to the role insecticides can play in the potentially increasing agricultural productivity, the Government of Burkina Faso regards these chemicals as a useful part of the agriculture. In the last few years, insecticides have extensively been applied and are still largely used by rural workers to combat locusts in the Sahelian region of Burkina Faso. However both a sporadic or a regular use of such chemicals could lead to significant consequences to public health (Abhilash and Singh, 2009; Prado-Lu, 2007). Some of the factors which are thought to have contributed to human poisoning include the lack of education and safety precautions among users and handlers of insecticides, factors which could minimize or prevent detrimental environmental and health effects (Clarke et al., 1997; Ouédraogo et al., 2009). Although the health hazards caused by insecticide are serious, supports from policy makers to provide for remedial measures have been lukewarm in developing countries. The resistance of policy makers is partially due to their deficient appreciation of the severity of the problem, its sources, and of suitable interventions. Their lack of knowledge is understandable, since studies of insecticide effects on health in developing countries are scarce. Moreover, neither in vitro toxicological approaches nor in vivo animal experiments are always suitable for predicting delayed adverse effects in human populations (Multinigner, 2005).
To the best of our knowledge, there is no published study about insecticide effects on exposed workers’ health in the Sahelian region of Burkina Faso, though these substances have been have used for the past two decades in agriculture. Thus, simple and effective health monitoring of those involved in insecticide application is more than essential.
The aim of this study was to assess biological signs and the prevalence of symptoms associated with insecticide exposure among insecticide applicators of the Sahelian region of Burkina Faso.
Materials and methods
Study area
The study was conducted in the Sahelian region of Burkina Faso from July to August, 2009. The target area is the most arid region located in the northern region of Burkina Faso. However, this area is frequently infested by locusts and/or grasshoppers, requiring the use of chemical insecticides.
Study population
The study was cross-sectional in design. The subjects were made up of 112 insecticide applicators, comprising 84 occasional applicators (farm workers) and 28 plant protection agents (who frequently sprayed insecticides). All subjects met the criteria of not having used insecticides in the preceding three months. A convenient series was collected based on availability of the subjects on the day of the study and on their willingness to participate.
Structured questionnaires were used to collect information on socio-demographic characteristics and life work experience of the insecticide applicators. The survey also asked farmers to report symptoms experienced after mixing and spraying insecticides.
Laboratory examinations were done for each insecticide applicator. Freshly collected blood samples from the arm vein were analyzed hematologically and biochemically.
Hematological analysis
Hematological analysis was performed using an automatic counter (ABX Diagnostics, Switzerland). Total Red Blood Cells (RBC) count (×106 mm–3), hemoglobin content (Hb) (g.dl–1), hematocrit rate (HCT) (%), total number of White Blood Cells (WBC) (×106 mm–3), total number of Platelets (×106 mm–3), Mean Corpuscular Volume (MCV) (fl), and Mean Corpuscular Hemoglobin Concentration (MCHC) (g.dl–1) were assessed.
Biochemical analysis
The serum of the blood samples was separated by centrifugation (3 000 r.p.m., for 15 min) and alanine aminotransferase (ALT), aspartate aminotransferase (AST), creatinine, and cholinesterase levels were spectrophotometrically determined using diagnostic kits (Spinreact Diagnostic Kit, Santa Coloma, Spain).
Statistical analysis
Significant differences between mean values of farm workers and plant protection agents were statistically analyzed using Mann-Whitney's test. Chi-square (Χ2) or Yates corrected Chi-square test was performed to test differences between frequencies of characteristics of the study groups. Statistical analysis was carried out using GraphPad Prism version 2.01 software (GraphPad Software Inc, USA). The criterion for statistical significance was p<0.05.
Results
Socio-demographic profile
All the respondents were male. Table 1 shows the socio-demographic characteristics of the farm workers (occasional applicators) and plant protection agents.
Table 1.
Socio-demographic characteristics (%) of farm workers (occasional applicators) and plant protection agents in the Sahelian region of Burkina Faso.
| Farm workers (n=84) No. (%) | Plants protection agents (n=28) No. (%) | Yates corrected Χ2 *p-value | |
|---|---|---|---|
| Age (years) | |||
| 18-29 | 13 (15.48) | 1 (3.57) | |
| 30-49 | 57 (67.86) | 19 (67.86) | |
| = 50 | 14 (16.66) | 8 (28.57) | 0.615 |
| Mean age ± SD | 39.36±9.21 | 41.58±10.25 | |
| Education | 0.014 | ||
| Illiterate | 55 (65.48) | 6 (21.42) | |
| Primary school | 26 (30.95) | 11 (39.29) | |
| Secondary school | 3 (3.57) | 11 (39.29) | |
| Training in the use of insecticides (Yes) | 69 (82.14) | 28 (100) | 0.002 |
p-values are based on the distribution of the data for each characteristic, by plant protection agents and farm workers (occasional applicators)
Insecticide exposure
In the Sahelian region of Burkina Faso, chemical insecticides used by insecticide applicators in the agricultural sector can be classified into 4 main types: organophosphates, pyrethroids, carbamates and phenylpyrazoles. The duration of insecticide use ranged from under 5 years to over 20 years. The mean duration of insecticide use was respectively 11.02±8.03 and 13.33±10.25 (p>0.05) in farm workers and plant protection agents. The frequency of insecticide application by plant protection agents was twice or three times a month. The farm workers used insecticides twice a year at the most. Most applications were made from June to October. Each application lasted from 30 minutes to 4 hours, and despite the high risk of exposure, farm workers did not wear proper personal protection while working with insecticides. Boots were the only protective equipment worn by the majority of farm workers (95.2%), and practically no one used aprons or gloves. Cloth face masks, which do not offer adequate coverage for some chemicals, were used by 30% of them. Improvised forms of personal protection equipment were also used, such as handkerchiefs and long sleeves. However, all the plant protection agents claimed that they used adequate personal protection equipment during insecticide application.
Laboratory examinations
No significant differences were found between hematological parameters in farm workers and plants protection agents (Table 2). Serum biochemical parameters are shown in Table 2, while Table 3 shows frequency distribution of abnormal biochemical parameters among farm workers and plant protection workers.
Table 2.
Hematological and biochemical parameters profile in farm workers and plant protection agents of the Sahelian region of Burkina Faso.
| Parameters | Farm workers(n=84)Mean ± SE | Plant protection agents (n=28)Mean ± SE |
|---|---|---|
| Hematological parameters | ||
| RBC (×106 mm–3) | 5.68±0.24 | 7.3±2.45 |
| Hb (g.dl–1) | 13.28±0.54 | 13.76±0.38 |
| HCT (%) | 45.86±2.72 | 45.02±1.28 |
| WBC (×106 mm–3) | 5.11±0.16 | 5.16±0.15 |
| Platelets (×106 mm–3) | 253.23±15.35 | 255.54±27.83 |
| MCV (fl) | 86.68±1.25 | 87.49±1.60 |
| MCHC (g.dl–1) | 30.61±0.90 | 30.84±0.85 |
| Biochemical parameters | ||
| ALT | 33.44±2.45* | 59.35±7.83 |
| AST | 30.67±2.57* | 45.24±4.37 |
| Creatinine (U.l–1) | 76.57±4.12* | 89.42±7.22 |
| Cholinesterase (U.l–1) | 2 862.34±144.10* | 2 665.45±214.90 |
Difference was significant (p<0.05) using Mann-Whitney's test
Table 3.
Frequency of abnormal biochemical parameters among farm workers (n=84) and plant protection agents (n=28) in the Sahelian region of Burkina Faso.
| Biochemical parameters | Farm workers (%) | Plant protection agents (%) |
|---|---|---|
| ALT | 29.17* | 63.16 |
| AST | 39.22* | 47.62 |
| Creatinine | 19.05* | 39.13 |
Difference was significant (p<0.05) using Chi-square test
Self-reported symptoms
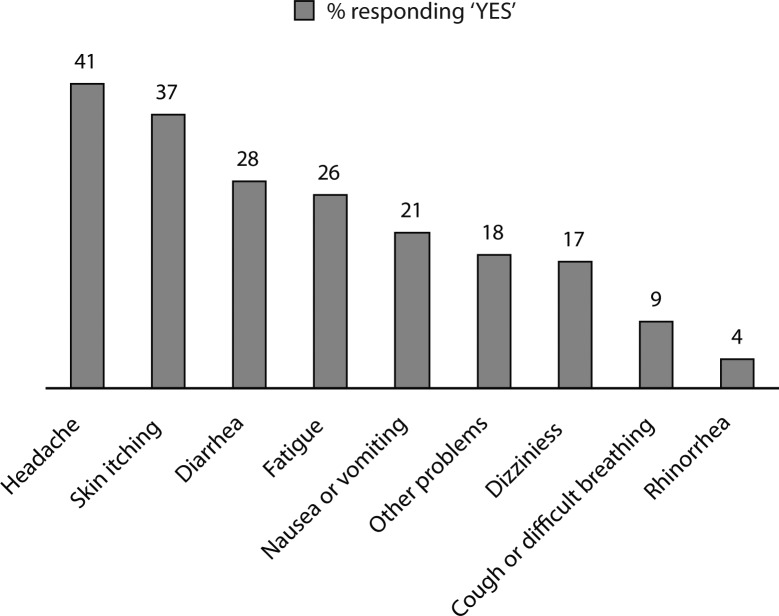
Figure 1 displays the health complaints of insecticide applicators, possibly related to insecticide exposure. Most (85%) of the surveyed insecticide applicators reported that they had multiple symptoms after using insecticides, with an average of 3 and a maximum of 6.
Figure 1.
Self-reported health impairment after using insecticides (n=112).
Discussion
Some practices predisposing to insecticide exposure and illness were identified in insecticide applicators in the Sahelian region of Burkina Faso. The mean duration of insecticide use was more than ten years (about 11 and 13 years for farm workers and plant protection agents, respectively). This is very significant, and indicates chronic exposure among these applicators. Most insecticide applicators were illiterate (Table 1) and did not wear proper personal protection. This shows the seriousness of the situation faced by the insecticide applicators. In Poland, 22 poisoning cases were seen in 2002 as a result of spraying pesticides without adequate protective equipment (Przybylska, 2004).
All the hematologic parameters of the two study groups (farm workers and plant protection agents) were normal. Similar results were reported by other authors (Lebailly et al., 2003; Pastor et al., 2002). However, many hematologic changes secondary to acute and chronic insecticide exposure were reported in both humans and animals, although there are some conflicting results (Jamil et al., 2007; Meaklim et al., 2003; Saly et al., 1995). Insecticides were shown to have hematotoxic properties and may cause aplastic anemia, agranulocytosis, neutropenia, and thrombopenia (Parent-Massin & Thouvenot, 1993). The contradictions may be attributed to the types of insecticides used and to exposure conditions.
The increase in the level of ALT and /or AST is a good indicator of hepatic toxicity (Dorosz, 2002; Hall, 2001). The mean levels of ALT and AST in plant protection agents were higher than the levels in farm workers (Table 2). Liver dysfunction (abnormal rise of ALT and AST) was most frequent (63.16% and 47.62%, respectively) among plant protection agents (Table 3). Abnormal levels of transaminases (ALT and AST) were found also in occupationally insecticide-exposed workers in India and Pakistan. The changes were related to the exposure of workers to insecticides (Azmi et al., 2006; Hernandez et al., 2006; Khan et al., 2008; Patil et al., 2003).
The mean level of creatinine concentration in plant protection agents was also higher than the level in farm workers (Table 2). The prevalence of abnormal levels of creatinine among plants protection agents (39.13%) was higher than the prevalence in farm workers (19.05%) (Table 3). A previous study reported subtle nephrotoxic changes in workers occupationally exposed to insecticides with high levels of creatinine (Attia, 2006).
Although organophosphate insecticides were also used by insecticide applicators, serum cholinesterase level was normal (between 1 900 and 3 800 U.l–1) (Dorosz, 2002) in all farm workers and plant protection agents. This is not surprising because serum cholinesterase indicates a significant acute organophosphate toxicity (Prado-Lu, 2007). However, the mean serum cholinesterase level of plant protection agents was lower than that of farm workers (Table 2). A screening of Hmong farmers in Thailand who used insecticides in their fields showed that 20–69% of 582 Hmong adults had risky or unsafe levels of cholinesterase (Kunstadter et al., 2001).Cholinesterase corresponds to two enzymes: acetylcholinesterase and butyrylcholinesterase. The latter is also called plasma cholinesterase (Hernandez et al., 2004). The activity of cholinesterase enzymes in blood can be utilized as a biomarker for the effect of organophosphates. An intoxicated person will show abnormally low levels of activity of cholinesterase enzymes measured in serum or in red blood cells (Kachaiyaphum et al., 2010; Tinoco-Ojanguren & Halperin, 1998).
The present study revealed that the prevalence of liver and kidney dysfunction was high among insecticide applicators in the Sahelian region of Burkina Faso and this prevalence was higher among plant protection agents. This situation could be attributed to inappropriate protection equipment of the applicators and to the frequent use of insecticides by plant protection agents.
In our study, headache was the most frequently reported symptom (40.61%), closely followed by skin itching (37%), diarrhea (28%), fatigue (26%), and nausea or vomiting (21%). Dizziness, cough or difficult breathing and rhinorrhea were also common (respectively 17%, 9%, and 4%). Such a constellation of symptoms is consistent with previous findings among farmers exposed to organophosphate insecticides (Strong et al., 2004). Our results highlight the high frequency of symptoms among insecticide applicators (85%) and confirm that they did not wear proper personal equipment while working. In northern Vietnam, Murphy et al. reported that, out of 1798 recorded pesticides spray operations 8% of the subjects involved were asymptomatic, 61% presented with vague ill-defined effects, and 31% were affected with at least one clear symptom of poisoning (Murphy et al., 2002).
The design of our survey did not allow to report on serious and long-term consequences of insecticides. Some authors observed that exposure to insecticides was increasingly linked to immune suppression, hormone disruption, diminished intelligence, reproductive abnormalities, and cancer (Undeger and Basaran, 2005; Varona et al., 2003).
Conclusion
The study demonstrated the detrimental effect of exposure to insecticides on hematologic and biochemical parameters of insecticide applicators in the Sahelian region of Burkina Faso. The laboratory examinations revealed that the prevalence of liver or kidney dysfunctions was quite high among insecticide applicators, especially among plant protection agents. The prevalence of biochemical alterations seems to be correlated to the frequent use of insecticides. No significant differences were found between hematological parameters in farm workers and plant protection agents. The great majority of insecticide applicators reported symptoms associated with insecticide exposure. More detailed studies investigating other delayed effects of insecticides on human health are critically needed in Burkina Faso. Intensive intervention efforts to reduce insecticide mortality and morbidity are required.
Acknowledgments
The authors are grateful to DPV (Direction de la Protection des Végétaux) and PULCPA (Projet d'Urgence de Lutte Contre le Criquet Pèlerin en Afrique) for their financial and technical assistance.
REFERENCES
- Abhilash PC, Singh N. Pesticide use and application: An Indian scenario. J Hazard Mater. 2009;165:1–12. doi: 10.1016/j.jhazmat.2008.10.061. [DOI] [PubMed] [Google Scholar]
- Attia MA. Risk assessment of occupational exposure to pesticides. Earth Environ Sci. 2006;3:349–362. [Google Scholar]
- Azmi MA, Naqvi SN, Azmi MA, Aslam M. Effect of pesticide residues on health and different enzyme levels in the blood of farm workers from Gadap (rural) Karachi-Pakistan. Chemosphere. 2006;64:1739–1744. doi: 10.1016/j.chemosphere.2006.01.016. [DOI] [PubMed] [Google Scholar]
- Clarke EEK, Levy LS, Spurgeon A, Calvert IA. The problems associated with pesticide use by irrigation workers in Ghana. Occup Mod. 1997;47:301–308. doi: 10.1093/occmed/47.5.301. [DOI] [PubMed] [Google Scholar]
- Dorosz P. Guide pratique des médicaments. 22nd ed. Paris- Maloine; 2002. pp. 1686–1713. [Google Scholar]
- Hall R. Principles of Clinical Pathology for Toxicology Studies. Philadelphia: Taylor and Francis; 2001. pp. 35–37. [Google Scholar]
- Hernandez A, Gomez MA, Pena G, Gil F, Rodrigo L, Villanueva E, Pla A. Effect of long-term exposure to pesticides on plasma esterases from plastic greenhouse workers. J Toxicol Environ Health. 2004;A67:1095–1108. doi: 10.1080/15287390490452371. [DOI] [PubMed] [Google Scholar]
- Hernandez FA, Gomez MA, Perez VG, Lario VJ, Pena G, Gil F, Lopez O, Rodrigo L, Pino G, Pla A. Influence of exposure to pesticides on serum components and enzyme activities of cytotoxicity among intensive agriculture farmers. Environ Res. 2006;102:70–76. doi: 10.1016/j.envres.2006.03.002. [DOI] [PubMed] [Google Scholar]
- Jamil K, Das GP, Shaik AP, Dharmi SS, Murthy S. Epidemiological studies of pesticide exposed individuals and their clinical implications. Current Sci. 2007;92:340–345. [Google Scholar]
- Kachaiyaphum P, Howteerakul N, Sujirarat D, Siri S, Suwannapong N. Serum Cholinesterase levels of Thai chilli-farm workers exposed to chemical pesticides: Prevalence estimates and associated factors. J Occup Health. 2010;52:89–98. doi: 10.1539/joh.q9003. [DOI] [PubMed] [Google Scholar]
- Kannan K, Tanabe S, Ramesh A, Subramanian A, Tatsukawa R. Persistent orgnochlorine residues in food stuffs from India and their implications on human dietary exposure. J Agric Food Chem. 1992;40:518–524. [Google Scholar]
- Khan DA, Bhatti MM, Khan FA, Naqvi ST, Karam A. Adverse effects of pesticides residues on biochemical markers in Pakistani tobacco farmers. Int J Clin Exp Med. 2008;1:274–282. [PMC free article] [PubMed] [Google Scholar]
- Kunstadter P, Prapamontol T, Sirirojn BO, Sontirat A, Tansuhaj A, Khamboonruang C. Pesticide exposures among Hmong farmers in Thailand. Int J Occup Environ Health. 2001;7:313–325. doi: 10.1179/107735201800339227. [DOI] [PubMed] [Google Scholar]
- Lebailly P, Devaux A, Pottie D, De Meo M, Andre V, Baldi I. Urine mutagenicity and lymphocyte DNA damage in fruit growers occupationally exposed to the fungicide captan. Occup Environ Med. 2003;60:910–917. doi: 10.1136/oem.60.12.910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meaklim J, Yang J, Drummer OH, et al. Fenitrothion: toxicokinetics and toxicologic evaluation in human volunteers. Environ Health Persp. 2003;111:305–308. doi: 10.1289/ehp.5726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Multinigner L. Delayed effects of pesticides on human health / Effets retardés des pesticides sur la santé humaine. Environ Risque Sante. 2005;4:187–194. [Google Scholar]
- Murphy HH, Hoan NP, Matteson P, Abubakar AL. Farmers’ self-surveillance of pesticide poisoning: A 12-month pilot study in Northern Vietnam. Int J Occup Env Health. 2002;8:201–211. doi: 10.1179/107735202800338894. [DOI] [PubMed] [Google Scholar]
- Ouédraogo M, Tankoano A, Ouédraogo TZ, Guissou IP. Risk factors for pesticide poisoning among users in the cotton-production region of Fada N'Gourma in Burkina Faso / Etude des facteurs de risques d'intoxications chez les utilisateurs de pesticides dans la région cotonnière de Fada N'Gourma au Burkina Faso. Environ Risque Sante. 2009;8:343–347. [Google Scholar]
- Parent-Massin D, Thouvenot D. In vitro study of pesticide hematotoxicity in human and rat progenitor. J Pharmacol Toxicol Methods. 1993;30:203–207. doi: 10.1016/1056-8719(93)90018-a. [DOI] [PubMed] [Google Scholar]
- Pastor S, Lucero L, Guitiérrez S, Durban R, Gomez C, Parron T. Follow-up study on micronucleus frequency in Spanish agricultural workers esposed to pesticides. Mutagenesis. 2002;17:79–82. doi: 10.1093/mutage/17.1.79. [DOI] [PubMed] [Google Scholar]
- Patil JA, Patil AJ, Wowindwar SP. Biochemical effects of various pesticides on sprayers of grape garden. Ind J Clin Biochem. 2003;18:16–22. doi: 10.1007/BF02867362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prado-Lu JLD. Pesticide exposure, risk factors and health problems among cutflower farmers: a cross sectional study. J Occup Med Toxicol. 2007;2:1–8. doi: 10.1186/1745-6673-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Przybylska A. Poisoning caused by chemicals for plant protection in Poland in 2002. Przegl Epidemiology. 2004;58:111–121. [PubMed] [Google Scholar]
- Saly J, Kacmar P, Neuschl J, Jantosoovic J. The effect of bentazone TP, an herbicide, on hematologic indicators in sheep during acute and subchronic poisoning. Vet Med- Praha. 1995;40:49–52. [PubMed] [Google Scholar]
- Strong LL, Thompson B, Coronado GD, Griffith WC, Vigoren EM, Islas I. Health symptoms and exposure to organophosphate pesticides in farmworkers. Am J Ind Med. 2004;46:599–606. doi: 10.1002/ajim.20095. [DOI] [PubMed] [Google Scholar]
- Tinoco-Ojanguren R, Halperin DC. Poverty, production, and health: inhibition of erythrocyte cholinesterase via occupational exposure to organophosphate insecticides in Chiapas, Mexico. Arch Environ Health. 1998;53:29–35. doi: 10.1080/00039899809605686. [DOI] [PubMed] [Google Scholar]
- Undeger U, Basaran N. Effects of pesticides on human peripheral lymphocytes in vitro: introduction of DNA damage. Arch Toxicol. 2005;79:169–176. doi: 10.1007/s00204-004-0616-6. [DOI] [PubMed] [Google Scholar]
- Varona M, Cardenas O, Crane C, Rocha S, Cuervo G, Vargas J. Cytogenic alterations in field workers routinely exposed to pesticides in Bogota farms. Biomedica. 2003;23:141–152. [PubMed] [Google Scholar]