Abstract
Purpose
To critically appraise, compare and summarize the measurement properties of self-report fatigue questionnaires validated in patients with multiple sclerosis (MS), Parkinson’s disease (PD) or stroke.
Methods
MEDLINE, EMBASE, PsycINFO, CINAHL and SPORTdiscus were searched. The COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) checklist was used to assess the methodological quality of studies. A qualitative data synthesis was performed to rate the measurement properties for each questionnaire.
Results
Thirty-eight studies out of 5,336 records met the inclusion criteria, evaluating 31 questionnaires. Moderate evidence was found for adequate internal consistency and structural validity of the Fatigue Scale for Motor and Cognitive functions (FSMC) and for adequate reliability and structural validity of the Unidimensional Fatigue Impact Scale (U-FIS) in MS.
Conclusions
We recommend the FSMC and U-FIS in MS. The Functional Assessment of Chronic Illness Therapy Fatigue subscale (FACIT-F) and Fatigue Severity Scale (FSS) show promise in PD, and the Profile of Mood States Fatigue subscale (POMS-F) for stroke. Future studies should focus on measurement error, responsiveness and interpretability. Studies should also put emphasis on providing input for the theoretical construct of fatigue, allowing the development of questionnaires that reflect generic and disease-specific symptoms of fatigue.
Electronic supplementary material
The online version of this article (doi:10.1007/s11136-011-0009-2) contains supplementary material, which is available to authorized users.
Keywords: Fatigue, Assessment, Psychometrics, Multiple sclerosis, Parkinson disease, Cerebrovascular disorders
Introduction
Fatigue is common in chronic neurological disorders [1]. Prevalence rates in conditions often seen in neurological rehabilitation, such as multiple sclerosis (MS), Parkinson’s disease (PD) and stroke, range from 58% [2] to 90% [3].
One of the challenges in assessing fatigue is the lack of a widely accepted definition [4] and with that, differentiating its many dimensions [2, 5]. Fatigue usually refers to the difficulty initiating or sustaining voluntary activity [6]. Its multidimensionality is believed to result from a complex interplay between the underlying disease process, peripheral control systems (i.e. muscle fatigability), central control systems (i.e. subjective sense of fatigue) and environmental factors [6]. This may reflect the large number of generic and disease-specific self-report questionnaires that are available to measure fatigue as either a multidimensional or a unidimensional assessment in patients considered for rehabilitation services. These questionnaires may measure different aspects or even different theoretical constructs of fatigue [7]. The clinician or researcher has to consider that each questionnaire is characterized by its own underlying concept, measurement properties and practical feasibility. A systematic review of the characteristics and measurement properties of self-report fatigue questionnaires can assist in selecting an appropriate questionnaire to evaluate fatigue in patients with MS, PD and stroke.
Several systematic reviews [7–13] have evaluated the measurement properties of fatigue questionnaires. Three of these reviews [7, 12, 13] focused on patients with chronic disease, including samples of patients with MS and PD. Unfortunately, no recommendations were made specifically for patients with MS or PD. One review [10] focused on patients with MS. The authors recommended the Fatigue Impact Scale (FIS) and the Modified Fatigue Impact Scale (MFIS) [10]. Another review [8] recommended the Multidimensional Fatigue Inventory (MFI) and the Fatigue Severity Scale (FSS) for patients with PD. No systematic review evaluated questionnaires validated in patients with stroke.
A limitation of the aforementioned reviews is that no uniform definitions and standards for the assessment of the methodological quality of the included studies were used. Therefore, the methodological quality of these studies was not taken into account when formulating conclusions, which makes it difficult to judge the strength of the evidence underlying the formulated recommendations. Recently, the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) checklist [14] was developed to systematically evaluate the methodological quality of studies on measurement properties. This makes it possible to appraise the methodological quality of the included studies and take this into account when formulating conclusions.
The aim of the present study was to critically appraise, compare and summarize the quality of the measurement properties of all published self-report fatigue questionnaires validated in patients with MS, PD or stroke, in order to assist clinicians and researchers in selecting a fatigue questionnaire.
Methods
Search
Five databases were searched up to November 2010 (MEDLINE (1966–2010), EMBASE (1974–2010), PsycINFO (1806–2010), CINAHL (1981–2010) and SPORTdiscus (1985–2010)). Text words and MESH terms for fatigue, MS, PD and stroke were combined with a sensitive filter (designed for PubMed) to identify studies on measurement properties of self-report questionnaires [15] (see supplementary file 1). References of the included studies were screened for additional articles.
Selection of studies
Two reviewers (RE/EvW) independently screened all titles and abstracts. The full text papers of relevant studies were obtained, and two reviewers (RE/MR) independently applied the a priori defined criteria for study selection. Studies were included if they met the following criteria: the study (1) focused on the development or evaluation of measurement properties of self-report questionnaires that assess subjective fatigue; (2) included patients with a clinical diagnosis of MS, PD or stroke and (3) included questionnaires that could be used for evaluative purposes. Studies were excluded if: the study (1) explicitly focused on the diagnostic test accuracy of the included questionnaire(s); (2) was published in a language other than Dutch, English, French or German. In case of disagreement, a third reviewer (EvW) was asked for advice to reach consensus.
Assessment of methodological quality
The methodological quality of a study was evaluated using the COSMIN checklist [14]. This checklist consists of 114 items, grouped in twelve boxes. Nine of these boxes contain standards for measurement properties (i.e. internal consistency, reliability, measurement error, content validity, structural validity, hypotheses testing, cross-cultural validity, criterion validity and responsiveness). One box contains standards for studies on interpretability, which is an important characteristic of a measurement scale [16]. In addition, two boxes contain requirements for studies in which Item Response Theory (IRT) methods are applied, and requirements for the generalizability of the results, respectively [14]. Each item was scored on a 4-point rating scale (i.e. ‘poor’, ‘fair’, ‘good’, or ‘excellent’) [17]. The methodological quality of a study was evaluated per measurement property and determined by the lowest rating of any of the items in a box. Pairs of reviewers (RE/EvW, RE/JV, RE/MR or RE/SK) independently scored the methodological quality of the included studies. Disagreement was resolved during consensus meetings.
Data extraction
A data extraction form was designed and tested before the pairs of reviewers independently extracted data on the: (1) characteristics of the study samples; (2) characteristics of the questionnaires (i.e. language version, theoretical construct of fatigue and dimensions, recall period, number of items, response options, range of scores, time to administer and ease of scoring); (3) evaluated measurement properties and (4) the interpretability and generalizability of the results.
Data synthesis
The theoretical construct of fatigue measured by a questionnaire was categorized by either ‘impact of fatigue on daily life’, ‘fatigue severity’ or ‘factors influencing fatigue’. Ease of scoring was categorized as ‘easy’ if items were simply summed, ‘moderate’ if a visual analogue scale (VAS) or simple formula was used, or ‘difficult’ if either a VAS in combination with a formula or a complex formula was used.
Measurement properties were summarized according to the COSMIN taxonomy [16]. For each study, the estimates of the investigated measurement properties were rated as ‘adequate’ (+), ‘not adequate’ (−) or ‘unclear’ (?), based on predefined criteria [18] as described below.
A qualitative data synthesis was performed to determine the overall quality of the measurement properties for each self-report questionnaire by taking into account the: (1) ratings for each measurement property; (2) consistency of results between studies; (3) methodological quality of studies and (4) the number of studies that investigated the measurement property. The possible overall quality of a measurement property was either ‘adequate’ (+), ‘not adequate’ (−), ‘conflicting’ (±) or ‘unclear’ (?). As shown in Table 1, levels of evidence were defined to express whether the strength of the evidence for the overall quality was, for example, convincing (‘strong’ level of evidence) or unconvincing (‘unknown’ level of evidence) [19].
Table 1.
Levels of evidence for the overall quality of a measurement property
| Level | Rating | Criteria |
|---|---|---|
| Strong | ‘Adequate’ or ‘Not adequate’ (+ or −) | Consistent findings in multiple studies of ‘good’ methodological quality OR in one study of ‘excellent’ methodological quality |
| Moderate | ‘Adequate’ or ‘Not adequate’ (+ or −) | Consistent findings in multiple studies of ‘fair’ methodological quality OR in one study of ‘good’ methodological quality |
| Limited | ‘Adequate’ or ‘Not adequate’ (+ or −) | One study of ‘fair’ methodological quality |
| Conflicting | ‘Conflicting’ (±) | Conflicting findings |
| Unknown | ‘Unknown’ (?) | Only studies of ‘poor’ methodological quality |
Criteria for the quality of measurement properties
Reliability
The domain reliability contains three measurement properties: internal consistency, reliability and measurement error [16].
Internal consistency is the degree of the interrelatedness among items, assuming the questionnaire to be unidimensional [16]. Cronbach’s α was considered an acceptable measure of internal consistency and scored adequate if it ranged between 0.70 and 0.95 [18]. If a questionnaire was multidimensional, internal consistency was considered per subscale.
Reliability was defined as the proportion of the total variance in the measurements which is because of ‘true’ differences between patients [16]. The intraclass correlation coefficient (ICC) and weighted kappa are acceptable measures for reliability and considered adequate if they were ≥0.70 [18]. If a Pearson or Spearman correlation coefficient (CC) was presented, which do not account for systematic differences between two tests [20], an estimate of ≥0.80 was considered adequate.
Measurement error, defined as the systematic and random error of a score that is not attributed to true changes in the construct to be measured [16], was scored adequate if the smallest detectable change (SDC) was smaller than the minimal important change (MIC), or if the MIC was outside the limits of agreement (LOA) [18].
Validity
Validity contains the measurement properties content validity, construct validity and criterion validity [16]. Content validity includes face validity and extends to the degree to which the content of a questionnaire is an adequate reflection of the construct to be measured [16]. It was rated adequate if the target population and experts considered all items in the questionnaire relevant and considered the questionnaire to be complete. Construct validity was defined as the degree to which scores of a questionnaire are consistent with hypothesis, based on the assumption that the instrument validly measures the construct to be measured [16]. Construct validity is divided into structural validity, hypothesis testing and cross-cultural validity. Structural validity, defined as the degree to which scores of a questionnaire are an adequate reflection of the dimensionality of the construct to be measured [16], was scored adequate if factor analysis showed that all factors together explained ≥50% of the total variance, or when IRT methods were applied to confirm unidimensionality. Hypothesis testing was scored adequate if the correlation with a questionnaire that assessed fatigue (convergent validity) was ≥0.50, or ≥75% of the results were in accordance with a priori defined hypotheses, and the correlations with other constructs (divergent validity) were lower than the correlations with fatigue. A score unclear was given if only the correlation with questionnaires measuring another construct than fatigue (divergent validity) was investigated. Cross-cultural validity was defined as the degree to which the performance of the items on a translated or culturally adapted health-related patient-reported outcomes (HR-PRO) instrument is an adequate reflection of the performance of the items of the original version of the HR-PRO instrument [16].
As no gold standard exits for fatigue questionnaires, criterion validity was not evaluated.
Responsiveness
Responsiveness was defined as the ability of a questionnaire to detect change over time in the construct to be measured [16]. Responsiveness refers to the validity of a change score [21] and scored adequate if the change score correlated ≥0.50 with the change score of an instrument assessing fatigue, or if ≥75% of the results were in accordance with a priori defined hypotheses, or if the area under the receiver operator characteristic curve (AUC) was ≥0.70 [18].
Interpretability
Interpretability was defined as the degree to which one can assign qualitative meaning to an instruments’ quantitative scores or change in scores. Authors should provide information about clinically relevant differences in scores between subgroups (mean or median with distribution of scores), floor and ceiling effects and the MIC [21]. A floor or ceiling effect was present if >15% of patients achieved the lowest or highest possible score on a questionnaire [18].
Results
Search
The search yielded 5,336 records, of which 56 studies were retrieved in full text for further assessment. This resulted in the exclusion of another 18 studies [10, 22–38] (see Fig. 1). Thirty-eight studies were included in the review, investigating 31 different self-report fatigue questionnaires [3, 39–75]. The FSS was most frequently investigated (n = 20) and the only questionnaire validated in patients with MS, PD and stroke. Characteristics of the included studies are presented in Table 2.
Fig. 1.
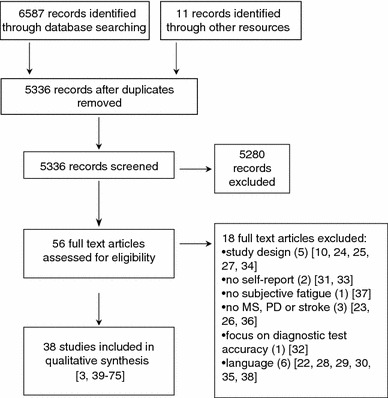
Flow diagram for study selection
Table 2.
Characteristics of included studies
| References | Patient characteristics | Questionnaire | |||||
|---|---|---|---|---|---|---|---|
| Population | N | Age Years Mean (SD) |
Disease duration Years Mean (SD) |
Disease severity EDSS/S&E/SA-SIP-30 Median (IQR) |
Investigated | Language version | |
| Armutlu [39] | MS | 72 | 38.16 (10.03) | 9.5 (6.43) |
EDSS 4.0 (1.0–9.5)a |
FSS | Turkish |
| Armutlu [40] | MS | 71 | 38.6 (9.9) | 9.42 (6.39) |
EDSS 3.94 (1.0–9.5)a |
FIS | Turkish |
| Benito-León [41] | MS | 68 | 37.0 (9.0) | 6.0 (4.0–10.0)b |
EDSS 2.5 (2.0–4.0) |
D-FIS MFI |
Spanish |
| Brown [42] | PD | 39–495c | 64.2 (9.6)–70.4 (9.5)c | 10.0 (7.6)–7.9 (6.7)c |
S&E 66.4 (23.0)–70.3 (15.5)c |
PFS-16 (2) PFS-16 (5) RFS |
English |
| Debouverie [3] | MS | 237 | 42.5 (10.9) | 9.8 (7.4) |
EDSS 3.7 (1.7)d |
EMIF-SEP FIS |
French |
| Doward [43] | MS | 9–167c | 39.0 (12.9)–54.3 (5.9)c | 8.4 (11.6)–22.7 (13.7)c | Not reported |
NHP-E U-FIS |
Canadian-English Canadian-French French German Italian Swedish US-English |
| Fisk [44] | MS | 105 | 42.5 (11.6) | Not reported | Not reported | FIS | English |
| Flachenecker [45] | MS | 151 | 39.0 (9.3) | 9.9 (6.7) |
EDSS 3.5 (0–8.5)a |
FSS MFIS MFSS |
German |
| Flachenecker [46] | MS | 67–158c | 39.2 (8.7)–39.2 (9.2)c | 9.7 (6.8)–9.9 (6.7) |
EDSS 3.5 (0–6.5)a–3.5 (0–8.5)a,c |
FSS MFIS MFSS WEIMUS |
German |
| Flachenecker [47] | MS | 25–580c | 44.1 (11.6)–47.2 (11.0)c | 11.0 (8.1)–15 (9.5)c |
EDSS 4.5 (1–8)a–5.5 (0–9)a,c |
FSS MFIS MFSS WEIMUS |
German |
| Flensner [48] | MS | 161 |
47.9 (10.1)e 48.0 (11.1)f |
Not reported | Not reported | FIS | Swedish |
| Grace [49] | PD | 50 | 71.66 (1.39) | Not reported | Not reported |
FSS PFS-16 (5) |
English |
| Hagell [50] | PD | 118 | 63.9 (9.6) | 8.4 (5.7) |
S&E 90 (80–90)g |
FACIT-F FSS NHP-E |
Swedish |
| Johansson [51] | MS | 219 | 47.0 (12.0) | 14 (10) |
EDSS 1.0–3.5: 130h 4.0–5.5: 37h 6.0–9.5: 52h |
FSS SOFI |
Swedish |
| Kim [52] | MS | 49 | 47 (25–67)i | 15.7 (1.3–48.0)i |
EDSS 3.2 (0–7)i |
FSS MFIS |
English |
| Kos [53] | MS | 51 | 51.9 (10.5) | 16.6 (8.9) |
EDSS 6.5 (3–8.5)a |
FSS MFIS |
Dutch |
| Kos [54] | MS | 30–51c | 44.6 (11.7)–52.9 (10.5)c | 11.3 (6.8)–16.6 (8.9)c |
EDSS 6 (3.5–7.5)–6.5 (3–8.5)c |
FSS MFIS |
Dutch Italian Slovenian Spanish |
| Kos [55] | MS | 62 | 52 (10.5) | Not reported |
EDSS 6.5 (3–8.5) |
FSS MFIS VAS-1 VAS-2 VAS-3 |
Dutch |
| Krupp [56] | MS | 25 | 44.8 (10) | Not reported | Not reported | FSS | English |
| Kummer [57] | PD | 87 | 56.9 (10.3) | 8.7 (4.9) |
S&E 76.7 (14.5)–86.1 (8.7)c |
PFS-16 (2) PFS-16 (5) |
Brazilian-Portuguese |
| Lerdal [58] | MS | 227–368c | 46.6 (12.4)–49.1 (11.7)c | 11.4 (8.3)–14.0 (10.4)c | Not reported |
FSS FSS-7 FSS-5 |
Norwegian Swedish |
| Losonczi [59] | MS | 111 | 43.82 (11.62) | 11.12 (8.29) |
EDSS 1.94 (1.37)d |
FIS | Hungarian |
| Marrie [60] | MS | 9324 | 52.3 (10.8) | Not reported | Not reported |
FSS MFIS PS-F |
English |
| Martínez–Martín [61] | PD | 96 | 66.7 (9.6)j | 8 (4–13)b,j |
S&E 80 (70–90)j |
D-FIS MFI |
Spanish |
| Mathiowetz [62] | MS | 54 | 50 (31–74)i | 9.5 (1–34)i | Not reported |
FIS FSS SF-36-V |
English |
| Mead [63] | Stroke | 55 | 73 (66–81)b |
23 (10–53)b,k 137 (93–217)b,l |
Not reported |
FAS MFSI-G POMS-F SF-36-V (V2.0) |
English |
| Meads [64] | MS | 15–135c | 24–77m | 0.4–59m | Not reported |
NHP-E U-FIS |
English |
| Mills [65] | MS | 416 | 45.8 (10.5) | 17.0 (9.5) |
EDSS 0.0–4.0: 143h 4.5–6.5: 126h 7.0–7.5: 81h 8.0–9.5: 58h Unknown: 8h |
FSS FSS-5 |
English |
| Mills [66] | MS | 317–318c | 46.4 (10.6)–46.8 (11.3)c | 14.2 (9.4)–16.0 (9.7)c |
EDSS 0.0–4.0: 214h 4.5–6.5: 196h 7.0–7.5: 136h 8.0–9.5: 80h Unknown: 9h |
NFI-MS | English |
| Mills [67] | MS | 415 | Not reported | Not reported | Not reported |
MFIS MFIS C-5/MFIS P-8 |
English |
| Penner [68] | MS | 309 | 43.4 (9.95) | Not reported |
EDSS 3.4 (1.63)d |
FSMC FSS MFIS |
Not reported |
| Rendas–Baum [69] | MS | 184 | 50.9 (10.5) | Not reported |
EDSS 6 (0–9)a |
FIS | Not reported |
| Reske [70] | MS | 20 | 39.1n | 9.0 (9.3) |
EDSS 3.2 (1.9)d |
FSS | German |
| Rietberg [71] | MS | 43 | 48.7 (7.0) | 14.3 (9.2) |
EDSS 3.5 (1–6.5)a |
CIS-20R FSS MFIS |
Dutch |
| Schwartz [72] | MS | 40 | Not reported | Not reported | Not reported |
FAI SF-36-V |
English |
| Smith [73] | Stroke | 80 | 74.1 (6.6) | 7.6 (5.4)o |
SA-SIP-30 72.8 (31.5)p 77.9 (26.0)q 82.1 (29.0)r 36.3 (30.6)s |
FAS | Dutch |
| Twiss [74] | MS | 911 | 36.5 (8.4) | 4.8 (5.2) |
EDSS 0.0–1.5: 400h 2.0–2.5: 262h 3.0–3.5: 135h >4: 105h Unknown: h9 |
U-FIS |
Australian-English Canadian-English Canadian-French French German Italian Spanish UK-English US-English |
| Valko [75] | MS | 188 | 45.0 (13.0) | 11.07 (9.79) |
EDSS 3.61 (2.26)d |
FSS | German |
| Stroke | 235 | 63 (14) | 1.21 (0.62) | Not reported | |||
aExpressed as median (Range)
bExpressed as median (IQR)
cRange of different (sub)samples
dExpressed as mean (SD)
eFemale
fMale
gDuring ‘off’ phase
hExpressed as numbers: EDSS categorized scores
iExpressed as mean (Range)
jBased on a total sample of N = 142
kInpatients, expressed in days
lOutpatients, expressed in days
mRange
nSD Not reported
oExpressed in months
pExpressed as percentage of total score body care and movement subscale
qExpressed as percentage of total score mobility subscale
rExpressed as percentage of total score ambulation subscale
sExpressed as percentage of total score alertness behaviour subscale
Characteristics of questionnaires
Table 3 presents the characteristics of the included self-report questionnaires. Most questionnaires aimed to assess the impact of fatigue on activities in daily life (Fatigue Impact Scale for Daily use (D-FIS), Adapted French version of Fatigue Impact Scale (EMIF-SEP), Fatigue Assessment Scale (FAS), FIS, Fatigue Severity Scale 5 item version (FSS-5), MFI, MFIS, Modified Fatigue Impact Scale Cognitive and Physical (MFIS C-5/MFIS P-8), Parkinson Fatigue Scale 2-point scale version (PFS-16 (2)), Parkinson Fatigue Scale 5-point scale version (PFS-16 (5)), Performance Scale Fatigue subscale (PS-F), Unidimensional Fatigue Impact Scale (U-FIS), Visual Analogue Scale-1, 2 or 3 (VAS-1, VAS-2, VAS-3), Würzburger Erschöpfungsinventars bei Multiple sclerosis (WEIMUS)), whereas six questionnaires focused primarily on fatigue severity (Multidimensional Fatigue Symptom Inventory general subscale (MFSI-G), Profile Of Mood States Fatigue subscale (POMS-F), Rhoten Fatigue Scale (RFS), Short-form-36 Vitality subscale (SF-36-V), Short-form-36 Vitality subscale version 2.0 (SF-36-V (V2.0)), Swedish Occupational Fatigue Inventory (SOFI)).
Table 3.
Characteristics of included questionnaires
| Questionnaire | Construct assessed | Recall period | Dimensions (number of items) | Response options (range) | Range of scores | Time to administer | Ease of scoring |
|---|---|---|---|---|---|---|---|
| CIS-20R |
Impact of fatigue Fatigue severity |
Last 2 weeks |
Subjective experience of fatigue (8) Reduction in motivation (4) Reduction in activity (3) Reduction in concentration (5) Total (20) |
7-point Likert (1–7) |
20–140 (Best–worst) |
Not reported | Easy |
| D-FIS | Impact of fatigue | Last day |
One dimension Total (8) |
5-point Likert (0–4) |
0–32 (Best–worst) |
Not reported | Easy |
| EMIF-SEP | Impact of fatigue | Last month |
Cognitive (10) Physical (13) Psychological (4) Social (13) Total (40) |
4-point Likert (1–4) |
0–100a (Best–worst) |
Not reported | Difficulta |
| FACIT-F |
Impact of fatigue Fatigue severity |
Last week |
One dimension Total (13) |
5-point Likert (0–4) |
0–52 (Worst–best) |
Not reported | Easy |
| FAI |
Impact of fatigue Fatigue severity |
Last 2 weeks |
Psychological consequencesb Severityb Situation—specificb Response to restb Total (29) |
7-point Likert (1–7) |
29–203 (Best–worst) |
Not reported | Easy |
| FAS | Impact of fatigue | Usually… |
One dimension Total (10) |
5-point Likert (1–5) |
10–50 (Best–worst) |
Not reported | Easy |
| FIS | Impact of fatigue | Last month |
Cognitive (10) Physical (10) Social (20) Total (40) |
5-point Likert (0–4) |
0–160 (Best–worst) |
Not reported | Easy |
| FSMC |
Impact of fatigue Fatigue severity Factors influencing fatigue |
In general… |
Cognitive (10) Motor (10) Total (20) |
5-point Likert (1–5) |
20–100 (Best–worst) |
Not reported | Easy |
| FSS |
Impact of fatigue Fatigue severity |
Not specified |
One dimension Total (9) |
7-point Likert (1–7) |
1–7c (Best–worst) |
Not reported | Moderatec |
| FSS-7 |
Impact of fatigue Fatigue severity |
Not specified |
One dimension Total (7) |
7-point Likert (1–7) |
1–7c (Best–worst) |
Not reported | Moderatec |
| FSS-5 | Impact of fatigue | Not specified |
One dimension Total (5) |
7-point Likert (1–7) |
0–100d (Best–worst) |
Not reported |
Moderated Easye |
| MFI | Impact of fatigue | Lately… |
General (4) Physical (4) Reduced activity (4) Reduced motivation (4) Mental (4) Total (20) |
5-point Likert (1–5) |
20–100 (Best–worst) |
Not reported | Easy |
| MFIS | Impact of fatigue | Last month |
Cognitive (10) Physical (9) Social (2) Total (21) |
5-point Likert (0–4) |
0–84 (Best–worst) |
Not reported | Easy |
| MFIS C-5/MFIS P-8 | Impact of fatigue | Last month |
Cognitive (5) Physical (8) Total (13) |
5-point Likert (0–4) |
0–52 (Best–worst) |
Not reported | Easy |
| MFSI-G | Fatigue severity | Last week |
One dimension Total (6) |
5-point Likert (0–4) |
0–24 (Best–worst) |
Not reported | Easy |
| MFSS | Factors influencing fatigue | Not specified |
One dimension Total (6) |
7-point Likert (1–7) |
1–7c (Best–worst) |
Not reported | Moderatec |
| NFI-MS |
Fatigue severity Factors influencing fatigue |
Last 2 weeks |
Abnormal nocturnal sleep (5) Cognitive (4) Physical (8) Relief by rest (6) Summary scale (10) Total (33) |
4-point Likert (0–3) |
0–99e (Best–worst) |
Not reported |
Moderated Easye |
| NHP-E |
Impact of fatigue Fatigue severity |
Not specified |
One dimensional Total (3) |
Adjectival (Weighted score per item) |
0–100 (Best–worst) |
Not reported | Easy |
| PFS-16 (2) | Impact of fatigue | Last 2 weeks |
One dimension Total (16) |
2-point Likert (0–1) |
0–16 (Best–worst) |
Not reported | Easy |
| PFS-16 (5) | Impact of fatigue | Last 2 weeks |
One dimension Total (16) |
5-point Likert (1–5) |
1–5c (Best–worst) |
Not reported | Moderatec |
| POMS-F | Fatigue severity | Last week |
One dimension Total (6) |
5-point Likert (0–4) |
0–24 (Best–worst) |
Not reported | Easy |
| PS-F | Impact of fatigue | Last month |
One dimension Total (1) |
6-point Likert (0–5) |
0–5 (Best–worst) |
Not reported | Easy |
| RFS | Fatigue severity | Last 2 weeks |
One dimension Total (1) |
11-point Likert (0–10) |
0–10 (Best–worst) |
Not reported | Easy |
| SF-36-V | Fatigue severity | Last month |
One dimension Total (4) |
6-point Likert (1–6) |
4–24 (Worst–best) |
Not reported | Easy |
| SF-36-V (V2.0) | Fatigue severity | Last month |
One dimension Total (4) |
5-point Likert (1–5) |
4–20 (Worst–best) |
Not reported | Easy |
| SOFI | Fatigue severity | Last 6 months |
Lack of energy (4) Lack of motivation (4) Physical discomfort (4) Physical exertion (4) Sleepiness (4) Total (20) |
7-point Likert (0–6) |
0–30f (Best–worst) |
Not reported | Moderatef |
| U-FIS | Impact of fatigue | Last week |
One dimension Total (22) |
4-point Likert (0–3) |
0–66 (Best–worst) |
Not reported | Easy |
| VAS-1 | Impact of fatigue | Not specified |
One dimension Total (1) |
100 mm VAS |
0–100g (Best–worst) |
Not reported | Moderateg |
| VAS-2 | Impact of fatigue | Not specified |
One dimension Total (1) |
100 mm VAS |
0–100g (Best–worst) |
Not reported | Moderateg |
| VAS-3 | Impact of fatigue | Not specified |
One dimension Total (1) |
100 mm VAS |
0–100g (Best–worst) |
Not reported | Moderateg |
| WEIMUS | Impact of fatigue | Last 2 weeks |
Cognitive (9) Physical (8) Total (17) |
5-point Likert (0–4) |
0–68 (Best–worst) |
Not reported | Easy |
aAdjusted total score on 0–100 scale
bNot reported
cAverage of total summed items
dOrdinal-interval (Rasch) transformation
eSummed raw (ordinal) score
fSummed total of averaged domain scores
gVisual analogue scale
Fifteen unidimensional (D-FIS, Functional Assessment of Chronic Illness Therapy Fatigue subscale (FACIT-F), FAS, FSS, Fatigue Severity Scale 7 item version (FSS-7), FSS-5, MFSI-G, Multiple sclerosis-specific Fatigue Severity Scale (MFSS), Nottingham Health Profile Energy subscale (NHP-E), PFS-16 (2), PFS-16 (5), POMS-F, SF-36-V, SF-36-V (2.0), U-FIS) and eleven multidimensional questionnaires (Checklist Individual Strength (CIS-20R), EMIF-SEP, Fatigue Assessment Instrument (FAI), FIS, Fatigue Scale for Motor and Cognitive functions (FSMC), MFI, MFIS, MFIS C-5/MFIS P-8, Neurological Fatigue Index MS (NFI-MS), SOFI, WEIMUS) were identified. The total number of items per questionnaire varied from 3 (NHP-E) to 40 (EMIF-SEP, FIS). Three visual analogue scales (VAS-1, VAS-2 and VAS-3) and two single-item Likert scales (PS-F, RFS) were included. Six disease-specific questionnaires were found: the MFSS, NFI-MS, PS-F and WEIMUS for patients with MS and the PFS-16 (2) and PFS-16 (5) for patients with PD.
Most questionnaires were found easy to administer. One questionnaire (EMIF-SEP) uses a complex formula to calculate an adjusted total score from 0 to 100, and for two questionnaires (FSS-5, NFI-MS), a nomogram was provided [65, 66] for ordinal-interval (Rasch) transformation. None of the included studies reported on the time needed to complete the questionnaires.
Measurement properties and methodological quality
Details about the investigated measurement properties and the methodological quality of the included studies are summarized in Table 4. Most studies investigated reliability and construct validity, whereas results on measurement error and responsiveness were often not reported.
Table 4.
Methodological quality and investigated measurement properties per study
| Reference | Population | Investigated measurement properties | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Internal consistency | Reliability | Measurement error | Content validity | Structural validity | Hypothesis testing | Cross-cultural validitya | Responsiveness | ||
| Armutlu [39] | MS | Poor | Fair | Fair | Poor | ||||
| Armutlu [40] | MS | Poor | Fair | Fair | Poor | ||||
| Benito–León [41] | MS | Fair | Fair | Fair | Fair | ||||
| Brown [42] | PD | Good |
Fairb Poorc |
Fair | Good | Fair | |||
| Debouverie [3] | MS | Good | Fair | Good | Fair | ||||
| Doward [43] | MS | Goodd | Fair | Fair | Goodd | Fair | Poor | ||
| Fisk [44] | MS | Poor | Poor | Poor | |||||
| Flachenecker [45] | MS | Poor | |||||||
| Flachenecker [46] | MS |
Faire Poorf |
Poor |
Fairg Poorh |
Fair | ||||
| Flachenecker [47] | MS | Poor | Poor | ||||||
| Flensner [48] | MS | Poor | Fair | Fair | |||||
| Grace [49] | PD |
Fairb Poori |
Fair | ||||||
| Hagell [50] | PD | Fair | Fair |
Fairj Goodk |
Fair | ||||
| Johansson [51] | MS | Fair | Fair | Fair | |||||
| Kim [52] | MS | Fair | |||||||
| Kos [53] | MS | Poor | Poor | Poor | Poor | ||||
| Kos [54] | MS | Fair | Fair | Fair | Fair | Poor | |||
| Kos [55] | MS | Fair | Poor | ||||||
| Krupp [56] | MS | Poor | Poor | Poor | Poor | Poor | |||
| Kummer [57] | PD |
Fairb Poorc |
Fair | ||||||
| Lerdal [58] | MS | Good | |||||||
| Losonci [59] | MS | Poor | Poor | Poor | Poor | ||||
| Marrie [60] | MS | Fair | |||||||
| Martínez-Martín [61] | PD | Good | Poor | Fair | Fair | Poor | |||
| Mathiowetz [62] | MS | Fair | Fair | ||||||
| Mead [63] | Stroke | Fair | Fair | Fair | Fair | Fair | |||
| Meads [64] | MS | Poor | Fair | Fair | Poor | Fair | |||
| Mills [65] | MS | Good | |||||||
| Mills [66] | MS | Fair | Fair | Fair | Fair | ||||
| Mills [67] | MS | Good | |||||||
| Penner [68] | MS | Good | Fair | Fair | Good | Fair | |||
| Rendas-Baum [69] | MS | Poor | |||||||
| Reske [70] | MS | Poor | Poor | Poor | Poor | Poor | |||
| Rietberg [71] | MS | Fair | Fair | Fair | Poor | Poor | |||
| Schwartz [72] | MS | Fair | Fair | Fair | Poor | ||||
| Smith [73] | Stroke | Fair | Poor | Fair | |||||
| Twiss [74] | MS | Poor | Fair | Poor | |||||
| Valko [75] |
MS Stroke |
Poor | Poor | Poor | |||||
aOnly items for translation scored
bPFS-16 (5)
cPFS-16 (2)
dBased on Swedish subsample
eFSS, MFSS
fMFIS, WEIMUS
gFSS, MFIS, MFSS
hWEIMUS
iFSS
jCTT
kIRT
Eight out of 31 studies that investigated hypothesis testing [41, 43, 50, 51, 61, 62, 64, 66] formulated a priori hypothesis about the expected direction or magnitude of the correlation between the investigated questionnaires. Seven studies [39, 40, 54, 59, 61, 70, 75] that translated a questionnaire scored poor methodological quality because the translated questionnaires were not pre-tested in a small sample to check interpretation, cultural relevance and ease of comprehension of the translation.
All studies [53, 56, 69, 71, 74] that reported on responsiveness scored poor methodological quality.
Overall quality of measurement properties
Table 5 presents the overall quality of the measurement properties per self-report questionnaire, accompanied by the level of evidence.
Table 5.
Data synthesis, levels of evidence and overall quality of measurement properties per questionnaire
| Questionnaire | Population | Measurement properties | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Internal consistency | Reliability | Measurement error | Content validity | Structural validity | Hypothesis testing | Cross-cultural validity | Responsiveness | ||
| CIS-20R | MS |
+ Limited |
? Unknown |
− Limited |
? Unknown |
||||
| D-FIS | MS |
+ Limited |
+ Limited |
+ Limited |
− Limited |
? Unknown |
|||
| PD |
+ Moderate |
? Unknown |
+ Limited |
− Limited |
|||||
| EMIF-SEP | MS |
+ Moderate |
+ Limited |
+ Moderate |
? Unknown |
||||
| FACIT-F | PD |
+ Limited |
+ Limited |
− Moderate |
+ Limited |
||||
| FAI | MS |
+ Limited |
− Limited |
− Limited |
? Unknown |
||||
| FAS | Stroke |
± Conflicting |
+ Limited |
? Unknown |
+ Limited |
− Limited |
|||
| FIS | MS |
? Unknown |
± Conflicting |
? Unknown |
− Moderate |
? Unknown |
? Unknown |
||
| FSMC | MS |
+ Moderate |
+ Limited |
+ Limited |
+ Moderate |
+ Limited |
|||
| FSS | MS |
+ Limited |
+ Moderate |
− Strong |
± Conflicting |
? Unknown |
? Unknown |
||
| PD |
+ Limited |
− Moderate |
+ Moderate |
||||||
| Stroke |
? Unknown |
? Unknown |
? Unknown |
||||||
| FSS-7 | MS |
+ Moderate |
|||||||
| FSS-5 | MS |
± Conflicting |
|||||||
| MFI | MS |
− Limited |
|||||||
| PD |
− Limited |
||||||||
| MFIS | MS |
− Limited |
+ Moderate |
? Unknown |
± Conflicting |
+ Moderate |
? Unknown |
? Unknown |
|
| MFIS C-5/MFIS P-8 | MS |
+ Moderate |
|||||||
| MFSI-G | Stroke |
+ Limited |
+ Limited |
? Unknown |
+ Limited |
− Limited |
|||
| MFSS | MS |
− Limited |
? Unknown |
+ Limited |
− Limited |
||||
| NFI-MS | MS |
+ Limited |
+ Limited |
+ Limited |
− Limited |
||||
| NHP-E | MS |
+ Moderate |
|||||||
| PD |
+ Limited |
||||||||
| PFS-16 (2) | PD |
? Unknown |
? Unknown |
+ Limited |
? Unknown |
||||
| PFS-16 (5) | PD |
− Moderate |
− Limited |
+ Limited |
+ Moderate |
+ Moderate |
? Unknown |
||
| POMS-F | Stroke |
+ Limited |
+ Limited |
? Unknown |
+ Limited |
+ Limited |
|||
| PS-F | MS | Not applicable | Not applicable |
+ Limited |
|||||
| RFS | PD | Not applicable | Not applicable |
+ Limited |
|||||
| SOFI | MS |
− Limited |
− Limited |
− Limited |
|||||
| SF-36-V | MS |
+ Limited |
|||||||
| SF-36-V (V2.0) | Stroke |
+ Limited |
− Limited |
? Unknown |
+ Limited |
− Limited |
|||
| U-FIS | MS |
− Moderate |
+ Moderate |
+ Moderate |
+ Moderate |
+ Moderate |
? Unknown |
? Unknown |
|
| VAS-1 | MS | Not applicable |
− Limited |
Not applicable |
? Unknown |
||||
| VAS-2 | MS | Not applicable |
− Limited |
Not applicable |
? Unknown |
||||
| VAS-3 | MS | Not applicable |
− Limited |
Not applicable |
? Unknown |
||||
| WEIMUS | MS |
? Unknown |
? Unknown |
? Unknown |
− Limited |
||||
+ Adequate, − Not adequate, ± Conflicting, ? Unknown
Reliability
The EMIF-SEP and FSMC showed moderate evidence for adequate internal consistency in patients with MS (Cronbach’s α = 0.82–0.93) [3, 68] and the D-FIS in patients with PD (Cronbach’s α = 0.93) [61]. Limited evidence for adequate internal consistency was found for the D-FIS and FSS in patients with MS (Cronbach’s α = 0.91–0.93) [41, 46], the FACIT-F and FSS in patients with PD (Cronbach’s α = 0.90–0.94) [49, 50], and the MFSI-G, POMS-F and SF-36-V (V2.0) in patients with stroke (Cronbach’s α = 0.76–0.93) [63].
Moderate evidence was found for adequate reliability for the FSS, MFIS and U-FIS in patients with MS (CC or ICC = 0.73–0.93) [39, 43, 52, 54, 64, 71]. Limited evidence for adequate reliability was found for the FAS, MFSI-G and POMS-F in patients with stroke (ICC = 0.74–0.77) [63] and the FACIT-F in patients with PD (ICC = 0.84–0.85) [50]. Reliability of the PFS-16 (5) was found not adequate (limited evidence, CC = 0.63) [42].
Measurement error was investigated for the CIS-20R, D-FIS, FAS, FSS, MFIS, MFSI-G, POMS-F and SF-36-V (V2.0), but only one study on the D-FIS used in patients with MS [41] reported details about the MIC. There was limited evidence for adequate measurement error of the D-FIS in patients with MS (SEM = 3.18 and MIC = 3.65) [41].
Validity
Content validity was investigated for the FAS, FIS, FSMC, MFSI-G, NFI-MS, PFS-16 (2), PFS-16 (5), POMS-F, SF-36-V (V2.0) and U-FIS. Moderate evidence was found for adequate content validity of the U-FIS in patients with MS [43, 64]. Limited evidence for adequate content validity was found for the FSMC and NFI-MS in patients with MS [66, 68], for the PFS-16 (2) and PFS-16 (5) in patients with PD [42], and for the FAS, MFSI-G, POMS-F and SF-36-V (V2.0) in patients with stroke [63].
Moderate evidence for adequate structural validity was found for the EMIF-SEP, FSMC (% total explained variance = 61.4–61.5) [3, 68] and U-FIS [43] in patients with MS and for the PFS-16 (5) in patients with PD (% total explained variance = 63.2–64.0) [42]. Four studies that applied IRT methods to assess structural validity demonstrated misfits for items in the FSS and MFIS in patients with MS [58, 65, 67] and in the FACIT-F and FSS in patients with PD [50]. Based on these analyses, new versions for the FSS (FSS-7, FSS-5) [58, 65] and for the MFIS (MFIS C-5/MFIS P-8) [67] were introduced.
Moderate evidence for convergent validity was found for the MFIS (CC = 0.54–0.89 with CIS-20R, FSMC, FSS, PS-F, WEIMUS, WEIMUS Cognitive subscale, WEIMUS Physical subscale) [46, 54, 60, 68, 71], U-FIS (CC = 0.48–0.86 with NHP-E) [43, 64] and NHP-E (CC = 0.48–0.86 with U-FIS) [43, 64] in patients with MS, and for the FSS (CC = 0.62–0.84 with FACIT-F, NHP-E, PFS-16 (5)) [49, 50] and PFS-16 (5) (CC = 0.71–0.84 with FSS, RFS) [42, 49] in patients with PD.
In 13 studies [3, 39, 40, 43, 48, 53, 54, 57, 59, 61, 70, 71, 75], questionnaires were translated. None of these studies investigated cross-cultural validity by means of confirmatory factor analysis or differential item functioning (DIF).
Responsiveness
Five studies [53, 56, 69, 71, 74] reported on responsiveness. None of these studies presented details about the correlation coefficient between change scores in the investigated questionnaires with change in an external anchor. Therefore, responsiveness was scored unknown for these questionnaires.
Interpretability
Clinically relevant differences in scores between subgroups were reported for the FIS [48], FSS [45], U-FIS [43, 64, 74] and WEIMUS [47] in patients with MS, and for the FACIT-F [50], FSS [50] and PFS-16 (5) [57] in patients with PD.
No floor or ceiling effects were found for the D-FIS [41], FSS [53], FSS-7 and FSS-5 [58], MFIS [53, 54], MFIS C-5/MFIS P-8 [67], NFI-MS [66] and U-FIS [74] in patients with MS. The SOFI showed a floor effect in patients with MS (on 12 of the 20 items, more than 25% of patients achieved the lowest possible score) [51]. The D-FIS [61], FACIT-F [50], FSS [50], PFS-16 (5) and PFS-16 (2) [57] showed no floor or ceiling effects in patients with PD.
Values for the MIC were reported for the D-FIS (MIC = 3.65) [41], FIS (MIC = 9.0–24.0) [69] and U-FIS (MIC = 2.4–7.0) [74] in patients with MS.
Discussion
To our knowledge, this review is the first that systematically appraised and summarized the evidence on the measurement properties of self-report fatigue questionnaires validated in patients with MS, PD or stroke, by taking the methodological quality of the included studies into account. Thirty-one questionnaires were evaluated. No multidimensional questionnaires were identified that were adequately validated in patients with PD or stroke. Moderate evidence was found for adequate internal consistency and structural validity of the FSMC and for adequate reliability and structural validity of the U-FIS in patients with MS. Therefore, we recommend the FSMC for the multidimensional, and the U-FIS for the unidimensional assessment of fatigue in patients with MS. The FACIT-F and FSS show promise for the assessment of fatigue in patients with PD, and the POMS-F for patients with stroke. However, reliability and validity should be confirmed in high-quality studies on the FACIT-F, FSS and POMS-F in these populations. Above recommendations should be considered with caution, given that studies investigating measurement error, responsiveness and interpretability are lacking. Second, as the level of evidence supporting the overall quality of most measurement properties was limited, future high-quality studies may change our recommendations.
Two reviews [8, 10] recommend on the use of a questionnaire. One review [10] suggested the FIS and MFIS in patients with MS. The other review [8] recommended the FSS for the unidimensional assessment of fatigue in patients with PD. Although not specifically validated in PD, the MFI was recommended for the multidimensional assessment of fatigue in patients with PD [8]. These recommendations are partially in line with our findings. However, taken the methodological quality of the studies included in our systematic review into account, most measurement properties of the FIS showed only unknown level of evidence. In addition, four studies [50, 58, 65, 67] that applied IRT methods to investigate structural validity demonstrated misfits for some items in the FSS and MFIS.
The inconsistent scores for hypothesis testing confirm that different questionnaires measure different aspects or constructs of fatigue. Unfortunately, details on the construct of fatigue measured by a questionnaire were often not reported. Furthermore, factors contributing to fatigue in patients with MS, PD or stroke are still not well known [2, 76, 77]. Translational research, bridging pre-clinical and clinical research [78], focused on physiological and clinical aspects contributing to peripheral and central fatigue [6], may provide input for more clearly defined concepts and dimensions of fatigue. As both fatigue and most clinical aspects contributing to fatigue fluctuate in time, associations between these factors may be more accurately reflected using longitudinal study designs with repeated measures in time [79]. Repeated measurement designs allow the investigation of the longitudinal construct validity of fatigue measures.
For now, we suggest that clinicians assessing fatigue carefully consider whether a questionnaire reflects the most relevant aspects of fatigue of their interest. Furthermore, a comprehensive evaluation of fatigue should be accompanied by the assessment of clinically related factors such as mood and sleep. Acknowledging that each fatigue questionnaire measures different aspects of fatigue, we recommend the simultaneous use of different questionnaires in research.
Interpretability is considered an important characteristic of a measurement scale [16], unfortunately, only a few studies reported details on clinically relevant differences in scores between subgroups [43, 45, 47, 48, 50, 57, 64, 74], floor and ceiling effects [41, 50, 51, 53, 54, 57, 58, 61, 66, 67, 74] and the MIC [41, 69, 74]. This makes it difficult to interpret scores and change scores on a fatigue questionnaire in both clinical practice and research.
Although it is believed that measurement properties are sample dependent [80], no major differences in measurement properties were found for questionnaires that were evaluated in more than one population. For example, all estimates of measurement properties for the D-FIS were consistent in patients with MS and PD. The FSS showed consistent scores for most measurement properties that were evaluated in patients with MS, PD and stroke. In addition, another review [8] concluded that the items of the disease-specific PFS-16 (5) did not differ much from other generic fatigue questionnaires and that it provided no clear advantages above a generic questionnaire for use in patients with PD. Furthermore, it is not clear whether manifestations of fatigue are different between neurological disorders [8]. These results suggest that generic fatigue questionnaires presented in this review can be used interchangeably in patients with MS, PD and stroke and favour a generic approach for the assessment of fatigue. In contrast, studies using IRT methods showed misfits on the FSS for four items in patients with MS [65], and for only one item in patients with PD [50]. This difference might have been caused by a difference in statistical power between both studies [65], but it is also possible that it was related to DIF in patients with MS and PD [65]. This emphasizes the importance of disease-specific validation for fatigue questionnaires used in patients with MS, PD and stroke. Above-mentioned findings suggest that self-report fatigue questionnaires should contain a core set of items assessing generic aspects of fatigue, whereas some additional items are more disease specific. We therefore recommend the adaptation of existing questionnaires, incorporating a uniform section on general aspects of fatigue and a section with disease-specific items. Items to assess general aspects of fatigue may be derived from the recently developed Patient-Reported Outcomes Measurement Information System (PROMIS) fatigue item bank [81].
This systematic review has some limitations. First, only studies published in Dutch, English, French or German were included. This language restriction resulted in the exclusion of six articles [22, 28–30, 35, 38]; however, these studies evaluated a diversity of questionnaires and language versions, so it is not likely that this resulted in selection bias. Second, the COSMIN checklist has some items that require subjective judgment, which may lead to disagreement between raters. However, we tested the COSMIN checklist with all reviewers before assessing the methodological quality of the included studies, and one reviewer (RE) was involved in the assessment of all studies to improve consistency in rating across studies. Third, the quality criteria we applied for rating measurement properties heavily weighed on classical test theory (CTT). As a consequence, IRT methods were not considered for underpinning the structural validity of questionnaires. To overcome this incompleteness, we decided, post hoc, that any misfit in a questionnaire displayed by a study using IRT methods was judged as not adequate structural validity.
Conclusion
We recommend the FSMC and U-FIS for the assessment of fatigue in patients with MS. The FACIT-F and FSS show promise in patients with PD, and the POMS-F for patients with stroke. No multidimensional questionnaires were adequately validated in patients with PD or stroke. Future studies should focus on translational research in which assumed underlying physiological and clinical aspects contributing to fatigue are investigated longitudinally, as perceptions of fatigue often show fluctuations in time. Such studies may provide input for the development of the theoretical construct of self-report fatigue questionnaires. We suggest that existing questionnaires should be adapted to contain both a uniform section that reflects general aspects of fatigue, and a disease-specific section that contains items that are related with physiological and clinical aspects of underlying disease. Studies on responsiveness and the MIC of fatigue questionnaires in patients with MS, PD and stroke are needed, to establish whether an instrument can detect meaningful changes in clinical practice and research.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
The authors would like to thank R. Spijker (MSc), medical information specialist and Trial Search Coordinator from the Academic Medical Center and the Dutch Cochrane Centre, Amsterdam, The Netherlands for his valuable support regarding the design of the search strategy. Financial disclosures: This research project was supported by a grant from the Royal Dutch Society for Physical Therapy, Scientific College Physical Therapy, project number: BU003-2010, and the Stichting MS Research, project number 04-553 MS.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Abbreviations
- AUC
Area under the receiver operator characteristic curve
- CC
Correlation coefficient
- CIS-20R
Checklist individual strength
- CTT
Classical test theory
- COSMIN
Consensus-based standards for the selection of health measurement instruments
- D-FIS
Fatigue impact scale for daily use
- DIF
Differential item functioning
- EDSS
Expanded disability status scale
- EMIF-SEP
Adapted French version of fatigue impact scale
- FACIT-F
Functional assessment of chronic illness therapy fatigue subscale
- FAI
Fatigue assessment instrument
- FAS
Fatigue assessment scale
- FIS
Fatigue impact scale
- FSMC
Fatigue scale for motor and cognitive functions
- FSS
Fatigue severity scale
- FSS-7
Fatigue severity scale 7 item version
- FSS-5
Fatigue severity scale 5 item version
- HR-PRO
Health-related patient-reported outcomes
- ICC
Intraclass correlation coefficient
- IQR
Interquartile range
- IRT
Item response theory
- LOA
Limits of agreement
- MFI
Multidimensional fatigue inventory
- MFIS
Modified fatigue impact scale
- MFIS C-5/MFIS P-8
Modified fatigue impact scale cognitive and physical
- MFSI-G
Multidimensional fatigue symptom inventory general subscale
- MFSS
Multiple sclerosis-specific fatigue severity scale
- MIC
Minimal important change
- MS
Multiple sclerosis
- NFI-MS
Neurological fatigue index for multiple sclerosis
- NHP-E
Nottingham health profile energy subscale
- PD
Parkinson’s disease
- PFS-16 (2)
Parkinson fatigue Scale 2-point scale version
- PFS-16 (5)
Parkinson fatigue scale 5-point scale version
- POMS-F
Profile of mood states fatigue subscale
- PROMIS
Patient-reported outcomes measurement information system
- PS-F
Performance scale fatigue subscale
- RFS
Rhoten fatigue scale
- S&E
Schwab and England score
- SA-SIP-30
Stroke-adapted sickness impact profile 30 item version
- SD
Standard deviation
- SDC
Smallest detectable change
- SF-36-V
Short-form-36 vitality subscale
- SF-36-V (V2.0)
Short-form-36 vitality subscale version 2.0
- SOFI
Swedish occupational fatigue inventory
- U-FIS
Unidimensional fatigue impact scale
- VAS-1, 2 or 3
Visual analogue scale-1, 2 or 3
- WEIMUS
Würzburger Erschöpfungsinventars bei Multiple sclerosis
References
- 1.De Groot M, Phillips S, Eskes G. Fatigue associated with stroke and other neurologic conditions: Implications for stroke rehabilitation. Archives of Physical Medicine and Rehabilitation. 2003;84(11):1714–1720. doi: 10.1053/S0003-9993(03)00346-0. [DOI] [PubMed] [Google Scholar]
- 2.Friedman J, Brown R, Comella C, Garber C, Krupp L, Lou J, et al. Fatigue in Parkinson’s disease: A review. Movement Disorders. 2007;22(3):297–308. doi: 10.1002/mds.21240. [DOI] [PubMed] [Google Scholar]
- 3.Debouverie M, Pittion-Vouyovitch S, Louis S, Guillemin F. Validity of a French version of the fatigue impact scale in multiple sclerosis. Multiple Sclerosis. 2007;13(8):1026–1032. doi: 10.1177/1352458507077942. [DOI] [PubMed] [Google Scholar]
- 4.Lou J. Physical and mental fatigue in Parkinson’s disease: epidemiology, pathophysiology and treatment. Drugs and Aging. 2009;26(3):195–208. doi: 10.2165/00002512-200926030-00002. [DOI] [PubMed] [Google Scholar]
- 5.Smets E, Garssen B, Bonke B, De Haes J. The multidimensional fatigue inventory (MFI) psychometric qualities of an instrument to assess fatigue. Journal of Psychosomatic Research. 1995;39(3):315–325. doi: 10.1016/0022-3999(94)00125-O. [DOI] [PubMed] [Google Scholar]
- 6.Chaudhuri A, Behan P. Fatigue in neurological disorders. Lancet. 2004;363(9413):978–988. doi: 10.1016/S0140-6736(04)15794-2. [DOI] [PubMed] [Google Scholar]
- 7.Dittner A, Wessely S, Brown R. The assessment of fatigue: A practical guide for clinicians and researchers. Journal of Psychosomatic Research. 2004;56(2):157–170. doi: 10.1016/S0022-3999(03)00371-4. [DOI] [PubMed] [Google Scholar]
- 8.Friedman J, Alves G, Hagell P, Marinus J, Marsh L, Martínez-Martín P, et al. Fatigue rating scales critique and recommendations by the movement disorders society task force on rating scales for Parkinson’s disease. Movement Disorders. 2010;25(7):805–822. doi: 10.1002/mds.22989. [DOI] [PubMed] [Google Scholar]
- 9.Hewlett S, Hehir M, Kirwan J. Measuring fatigue in rheumatoid arthritis: A systematic review of scales in use. Arthritis and Rheumatism. 2007;57(3):429–439. doi: 10.1002/art.22611. [DOI] [PubMed] [Google Scholar]
- 10.Kos D, Kerckhofs E, Ketelaer P, Duportail M, Nagels G, D’hooghe M, et al. Self-report assessment of fatigue in multiple sclerosis: A critical evaluation. Occupational Therapy in Health Care. 2004;17(3–4):45–62. doi: 10.1300/J003v17n03_04. [DOI] [PubMed] [Google Scholar]
- 11.Minton O, Stone P. A systematic review of the scales used for the measurement of cancer-related fatigue (CRF) Annals of Oncology. 2009;20(1):17–25. doi: 10.1093/annonc/mdn537. [DOI] [PubMed] [Google Scholar]
- 12.Mota D, Pimenta C. Self-report instruments for fatigue assessment: A systematic review. Research and Theory for Nursing Practice. 2006;20(1):49–78. doi: 10.1891/rtnp.20.1.49. [DOI] [PubMed] [Google Scholar]
- 13.Whitehead L. The measurement of fatigue in chronic illness: A systematic review of unidimensional and multidimensional fatigue measures. Journal of Pain and Symptom Management. 2009;37(1):107–128. doi: 10.1016/j.jpainsymman.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 14.Mokkink L, Terwee C, Patrick D, Alonso J, Stratford P, Knol D, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: An international Delphi study. Quality of Life Research. 2010;19(4):539–549. doi: 10.1007/s11136-010-9606-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Terwee C, Jansma E, Riphagen I, de Vet H. Development of a methodological PubMed search filter for finding studies on measurement properties of measurement instruments. Quality of Life Research. 2009;18(8):1115–1123. doi: 10.1007/s11136-009-9528-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mokkink L, Terwee C, Patrick D, Alonso J, Stratford P, Knol D, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. Journal of Clinical Epidemiology. 2010;63(7):737–745. doi: 10.1016/j.jclinepi.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 17.Terwee, C., Mokkink, L., Knol, D., Ostelo, R., Bouter, L., & de Vet, H. (2011). Rating the methodological quality in systematic reviews of studies on measurement properties: a scoring system for the COSMIN checklist. Quality of Life Research. doi: 10.1007/s11136-011-9960-1. [DOI] [PMC free article] [PubMed]
- 18.Terwee C, Bot S, de Boer M, van der Windt D, Knol D, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology. 2007;60(1):34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 19.Van Tulder M, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the Cochrane collaboration back review group. Spine. 2003;28(12):1290–1299. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 20.Streiner D, Norman G. Health measurement scales, a practical guide to their development and use. New York: Oxford University Press; 2003. [Google Scholar]
- 21.Mokkink L, Terwee C, Knol D, Stratford P, Alonso J, Patrick D, et al. The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: A clarification of its content. BMC Medical Research Methodology. 2010;10:22. doi: 10.1186/1471-2288-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Balci K, Armutlu K, Fil A, Karabudak R. If a special scale to measure subjective fatigue in multiple sclerosis was needed? Fizyoterapi Rehabilitasyon. 2008;19(3):188. [Google Scholar]
- 23.Chang C, Cella D, Clarke S, Heinemann A, von Roenn J, Harvey R. Should symptoms be scaled for intensity, frequency, or both? Palliative & Supportive Care. 2003;1(1):51–60. doi: 10.1017/S1478951503030049. [DOI] [PubMed] [Google Scholar]
- 24.Chipchase S, Lincoln N, Radford K. Measuring fatigue in people with multiple sclerosis. Disability and Rehabilitation. 2003;25(14):778–784. doi: 10.1080/0963828031000093477. [DOI] [PubMed] [Google Scholar]
- 25.Debouverie M, Pittion-Vouyovitch S, Guillemin F. Reconsidering fatigue at the onset of multiple sclerosis. Revue Neurologique (Paris) 2009;165(Suppl 4):135–144. doi: 10.1016/S0035-3787(09)72125-3. [DOI] [PubMed] [Google Scholar]
- 26.Fisk J, Doble S. Construction and validation of a fatigue impact scale for daily administration (D-FIS) Quality of Life Research. 2002;11(3):263–272. doi: 10.1023/A:1015295106602. [DOI] [PubMed] [Google Scholar]
- 27.Graham J, Fisher N, Granger C, Tomita M. Test battery for evaluating fatigue in multiple sclerosis patients. International Journal of MS Care. 2007;9(3):118–125. doi: 10.7224/1537-2073-9.3.118. [DOI] [Google Scholar]
- 28.Gruszczak A, Bartosik-Psujek H, Pocinska K, Stelmasiak Z. Validation analysis of selected psychometric features of Polish version of modified fatigue impact scale—preliminary findings. Neurologia i Neurochirurgia Polska. 2009;43(2):148–154. [PubMed] [Google Scholar]
- 29.Haase V, Lacerda S, de Paula Lima E, de Deus Corrêa T, de Brito D, Lana-Peixoto M. Assessment of psychosocial functioning in multiple sclerosis: Psychometric characteristics of four self-report measures. Arquivos de Neuro-psiquiatria. 2004;62(2-A):282–291. [PubMed] [Google Scholar]
- 30.Iriarte J, de Castro P. Proposal of a new scale for assessing fatigue in patients with multiple sclerosis. Neurologia. 1994;9(3):96–100. [PubMed] [Google Scholar]
- 31.Iriarte J, Katsamakis G, de Castro P. The fatigue descriptive scale (FDS): A useful tool to evaluate fatigue in multiple sclerosis. Multiple Sclerosis. 1999;5(1):10–16. doi: 10.1177/135245859900500103. [DOI] [PubMed] [Google Scholar]
- 32.Jason L, Ropacki M, Santoro N, Richman J, Heatherly W, Taylor R, et al. A screening instrument for chronic fatigue syndrome: Reliability and validity. Journal of chronic fatigue syndrome. 1997;3(1):39–59. doi: 10.1300/J092v03n01_04. [DOI] [Google Scholar]
- 33.Lynch J, Mead G, Greig C, Young A, Lewis S, Sharpe M. Fatigue after stroke: The development and evaluation of a case definition. Journal of Psychosomatic Research. 2007;63(5):539–544. doi: 10.1016/j.jpsychores.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 34.Montreuil M. Analysis of subjective complaints of fatigue in patients with multiple sclerosis. Revue Neurologique (Paris) 2000;156(11):1048–1050. [PubMed] [Google Scholar]
- 35.Pavan K, Schmidt K, Marangoni B, Fernanda Mendes M, Tilbery C, Lianza S. Multiple sclerosis: cross-cultural adaptation and validation of the modified fatigue impact scale. Arquivos de Neuro-psiquiatria. 2007;65(3-A):669–673. doi: 10.1590/S0004-282X2007000400024. [DOI] [PubMed] [Google Scholar]
- 36.Taylor R, Jason L, Torres A. Fatigue rating scales: An empirical comparison. Psychological Medicine. 2000;30(4):849–856. doi: 10.1017/S0033291799002500. [DOI] [PubMed] [Google Scholar]
- 37.Tseng, B., Gajewski, B., & Kluding, P. (2010). Reliability, responsiveness, and validity of the visual analog fatigue scale to measure exertion fatigue in people with chronic stroke: a preliminary study. Stroke Research and Treatment. doi: 10.4061/2010/412964. [DOI] [PMC free article] [PubMed]
- 38.Wu C, Liu Z, Zhang Y, Li J, Wang D. Validity and reliability of Chinese version of fatigue impact scale in cerebral infarction patients. Neural Regeneration Research. 2008;3(2):177–181. [Google Scholar]
- 39.Armutlu K, Korkmaz N, Keser I, Sümbüloglu V, Akbiyik D, Güney Z, et al. The validity and reliability of the fatigue severity scale in Turkish multiple sclerosis patients. International Journal of Rehabilitation Research. 2007;30(1):81–85. doi: 10.1097/MRR.0b013e3280146ec4. [DOI] [PubMed] [Google Scholar]
- 40.Armutlu K, Keser I, Korkmaz N, Akbiyik D, Sümbüloglu V, Güney Z, et al. Psychometric study of Turkish version of fatigue impact scale in multiple sclerosis patients. Journal of the Neurological Sciences. 2007;255(1–2):64–68. doi: 10.1016/j.jns.2007.01.073. [DOI] [PubMed] [Google Scholar]
- 41.Benito-León J, Martínez-Martín P, Frades B, Martínez-Ginés M, de Andrés C, Meca-Lallana J, et al. Impact of fatigue in multiple sclerosis: The fatigue impact scale for daily use (D-FIS) Multiple Sclerosis. 2007;13(5):645–651. doi: 10.1177/1352458506073528. [DOI] [PubMed] [Google Scholar]
- 42.Brown R, Dittner A, Findley L, Wessely S. The Parkinson fatigue scale. Parkinsonism and Related Disorders. 2005;11(1):49–55. doi: 10.1016/j.parkreldis.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 43.Doward L, Meads D, Fisk J, Twiss J, Hagell P, Oprandi N, et al. International development of the unidimensional fatigue impact scale (U-FIS) Value in Health. 2010;13(4):463–468. doi: 10.1111/j.1524-4733.2010.00706.x. [DOI] [PubMed] [Google Scholar]
- 44.Fisk J, Ritvo P, Ross L, Haase D, Marrie T, Schlech W. Measuring the functional impact of fatigue: Initial validation of the fatigue impact scale. Clinical Infectious Diseases. 1994;18(Suppl 1):79–83. doi: 10.1093/clinids/18.Supplement_1.S79. [DOI] [PubMed] [Google Scholar]
- 45.Flachenecker P, Kümpfel T, Kallmann B, Gottschalk M, Grauer O, Rieckmann P, et al. Fatigue in multiple sclerosis: A comparison of different rating scales and correlation to clinical parameters. Multiple Sclerosis. 2002;8(6):523–526. doi: 10.1191/1352458502ms839oa. [DOI] [PubMed] [Google Scholar]
- 46.Flachenecker P, Müller G, König H, Meissner H, Toyka K, Rieckmann P. Fatigue in multiple sclerosis: development and validation of the Würzburger fatigue inventory for MS. Der Nervenarzt. 2006;77(2):165–174. doi: 10.1007/s00115-005-1990-x. [DOI] [PubMed] [Google Scholar]
- 47.Flachenecker P, König H, Meissner H, Müller G, Rieckmann P. Fatigue in multiple sclerosis: Validation of the WEIMUS scale (‘Würzburger erschöpfungs-inventar bei multipler sklerose’) Neurologie & Rehabilitation. 2008;14(6):299–306. [Google Scholar]
- 48.Flensner G, Ek A, Söderhamn O. Reliability and validity of the Swedish version of the fatigue impact scale (FIS) Scandinavian Journal of Occupational Therapy. 2005;12(4):170–180. doi: 10.1080/11038120510031806. [DOI] [PubMed] [Google Scholar]
- 49.Grace J, Mendelsohn A, Friedman J. A comparison of fatigue measures in Parkinson’s disease. Parkinsonism and Related Disorders. 2007;13(7):443–445. doi: 10.1016/j.parkreldis.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 50.Hagell P, Höglund A, Reimer J, Erikson B, Knutsson I, Widner H, et al. Measuring fatigue in Parkinson’s disease: A psychometric study of two brief generic fatigue questionnaires. Journal of Pain and Symptom Management. 2006;32(5):420–432. doi: 10.1016/j.jpainsymman.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 51.Johansson S, Ytterberg C, Back B, Holmqvist L, von Koch L. The Swedish occupational fatigue inventory in people with multiple sclerosis. Journal of Rehabilitation Medicine. 2008;40(9):737–743. doi: 10.2340/16501977-0236. [DOI] [PubMed] [Google Scholar]
- 52.Kim E, Lovera J, Schaben L, Melara J, Bourdette D, Whitham R. Novel method for measurement of fatigue in multiple sclerosis: Real-time digital fatigue score. Journal of Rehabilitation and Development. 2010;47(5):477–484. doi: 10.1682/JRRD.2009.09.0151. [DOI] [PubMed] [Google Scholar]
- 53.Kos D, Kerckhofs E, Nagels G, D’hooghe M, Duquet W, Duportail M, et al. Assessing fatigue in multiple sclerosis: Dutch modified fatigue impact scale. Acta Neurologica Belgica. 2003;103(4):185–191. [PubMed] [Google Scholar]
- 54.Kos D, Kerckhofs E, Carrea I, Verza R, Ramos M, Jansa J. Evaluation of the modified fatigue impact scale in four different European countries. Multiple Sclerosis. 2005;11(1):76–80. doi: 10.1191/1352458505ms1117oa. [DOI] [PubMed] [Google Scholar]
- 55.Kos D, Nagels G, D’Hooghe M, Duportail M, Kerckhofs E. A rapid screening tool for fatigue impact in multiple sclerosis. BMC Neurology. 2006;6:27. doi: 10.1186/1471-2377-6-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Krupp L, LaRocca G, Muir-Nash J, Steinberg A. The fatigue severity scale: Application to patients with multiple sclerosis and systemic lupus erythematosus. Archives of Neurology. 1989;46(10):1121–1123. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 57.Kummer, A., Scalzo, P., Cardoso, F., & Teixeira, A. (2010). Evaluation of fatigue in Parkinson’s disease using the Brazilian version of Parkinson’s fatigue scale. Acta Neurologica Scandinavica. doi: 10.1111/j.1600-0404.2010.01364.x. [DOI] [PubMed]
- 58.Lerdal A, Johansson S, Kottorp A, von Koch L. Psychometric properties of the fatigue severity scale: Rasch analyses of responses in a Norwegian and a Swedish MS cohort. Multiple Sclerosis. 2010;16(6):733–741. doi: 10.1177/1352458510370792. [DOI] [PubMed] [Google Scholar]
- 59.Losonczi E, Bencsik K, Radja C, Lencsés G, Török M, Vécsei L. Validation of the fatigue impact scale in Hungarian patients with multiple sclerosis. Quality of Life Research. 2010;20(2):301–306. doi: 10.1007/s11136-010-9749-7. [DOI] [PubMed] [Google Scholar]
- 60.Marrie R, Cutter G, Tyry T, Hadjimichael O, Campagnolo D, Vollmer T. Validation of the NARCOMS registry: Fatigue assessment. Multiple Sclerosis. 2005;11(5):583–584. doi: 10.1191/1352458505ms1216oa. [DOI] [PubMed] [Google Scholar]
- 61.Martínez-Martín P, Catalan M, Benito-León J, Ortega Moreno A, Zamarbide I, Cubo E, et al. Impact of fatigue in Parkinson’s disease: The fatigue impact scale for daily use (D-FIS) Quality of Life Research. 2006;15(4):597–606. doi: 10.1007/s11136-005-4181-0. [DOI] [PubMed] [Google Scholar]
- 62.Mathiowetz V. Test-retest reliability and convergent validity of the fatigue impact scale for persons with multiple sclerosis. The American Journal of Occupational Therapy. 2003;57(4):389–395. doi: 10.5014/ajot.57.4.389. [DOI] [PubMed] [Google Scholar]
- 63.Mead G, Lynch J, Greig C, Young A, Lewis S, Sharpe M. Evaluation of fatigue scales in stroke patients. Stroke. 2007;38(7):2090–2095. doi: 10.1161/STROKEAHA.106.478941. [DOI] [PubMed] [Google Scholar]
- 64.Meads D, Doward L, McKenna S, Fisk J, Twiss J, Eckert B. The development and validation of the unidimensional fatigue impact scale (U-FIS) Multiple Sclerosis. 2009;15(10):1228–1238. doi: 10.1177/1352458509106714. [DOI] [PubMed] [Google Scholar]
- 65.Mills R, Young C, Nicholas R, Pallant J, Tennant A. Rash analysis of the fatigue severity scale in multiple sclerosis. Multiple Sclerosis. 2009;15(1):81–87. doi: 10.1177/1352458508096215. [DOI] [PubMed] [Google Scholar]
- 66.Mills R, Young C, Pallant J, Tennant A. Development of a patient reported outcome scale for fatigue in multiple sclerosis: The neurological fatigue index (NFI-MS) Health and Quality of Life Outcomes. 2010;8:22. doi: 10.1186/1477-7525-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mills R, Young C, Pallant J, Tennant A. Rasch analysis of the modified fatigue impact scale (MFIS) in multiple sclerosis. Journal of Neurology, Neurosurgery and Psychiatry. 2010;81(9):1049–1051. doi: 10.1136/jnnp.2008.151340. [DOI] [PubMed] [Google Scholar]
- 68.Penner I, Raselli C, Stöcklin M, Opwis K, Kappos L, Calabrese P. The fatigue scale for motor and cognitive functions (FSMC): Validation of a new instrument to assess multiple sclerosis-related fatigue. Multiple Sclerosis. 2009;15(12):1509–1517. doi: 10.1177/1352458509348519. [DOI] [PubMed] [Google Scholar]
- 69.Rendas-Baum R, Yang M, Cattelin F, Wallenstein G, Fisk J. A novel approach to estimate the minimally important difference for the fatigue impact scale in multiple sclerosis patients. Quality of Life Research. 2010;19(9):1349–1358. doi: 10.1007/s11136-010-9704-7. [DOI] [PubMed] [Google Scholar]
- 70.Reske D, Pukrop R, Scheinig K, Haupt W, Petereit H. Measuring fatigue in patients with multiple sclerosis with standardized methods in German-speaking areas. Fortschritte der Neurologie, Psychiatrie. 2006;74(9):497–502. doi: 10.1055/s-2006-932189. [DOI] [PubMed] [Google Scholar]
- 71.Rietberg M, van Wegen E, Kwakkel G. Measuring fatigue in patients with multiple sclerosis: Reproducibility, responsiveness and concurrent validity of three Dutch self-report questionnaires. Disability and Rehabilitation. 2010;32(22):1870–1876. doi: 10.3109/09638281003734458. [DOI] [PubMed] [Google Scholar]
- 72.Schwartz J, Jandorf L, Krupp L. The measurement of fatigue: A new instrument. Journal of Psychosomatic Research. 1993;37(7):753–762. doi: 10.1016/0022-3999(93)90104-N. [DOI] [PubMed] [Google Scholar]
- 73.Smith O, van den Broek K, Renkens M, Denollet J. Comparison of fatigue levels in patients with stroke and patients with end-stage heart failure: Application of the fatigue assessment scale. Journal of the American Geriatrics Society. 2008;56(10):1915–1919. doi: 10.1111/j.1532-5415.2008.01925.x. [DOI] [PubMed] [Google Scholar]
- 74.Twiss J, Doward L, McKenna S, Eckert B. Interpreting scores on multiple sclerosis-specific patient reported outcome measures (the PRIMUS and U-FIS) Health and Quality of Life Outcomes. 2010;8:117. doi: 10.1186/1477-7525-8-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Valko P, Bassetti C, Bloch K, Held U, Baumann C. Validation of the fatigue severity scale in a Swiss cohort. Sleep. 2008;31(11):1601–1607. doi: 10.1093/sleep/31.11.1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kos D, Kerckhofs E, Nagels G, D’hooghe M, Ilsbroukx S. Origin of fatigue in multiple sclerosis: Review of the literature. Neurorehabilitation and Neural Repair. 2008;22(1):91–100. doi: 10.1177/1545968306298934. [DOI] [PubMed] [Google Scholar]
- 77.Tseng B, Billinger S, Gajewski B, Kluding P. Exertion fatigue and chronic fatigue are two distinct constructs in people post-stroke. Stroke. 2010;41(12):2908–2912. doi: 10.1161/STROKEAHA.110.596064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kwakkel G. Towards integrative neurorehabilitation science. Physiotherapy Research International. 2009;14(3):137–146. doi: 10.1002/pri.446. [DOI] [PubMed] [Google Scholar]
- 79.Elbers R, van Wegen E, Rochester L, Hetherington V, Nieuwboer A, Willems A, et al. Is impact of fatigue an independent factor associated with physical activity in patients with idiopathic Parkinson’s disease? Movement Disorders. 2009;24(10):1512–1518. doi: 10.1002/mds.22664. [DOI] [PubMed] [Google Scholar]
- 80.McHorney C, Ware J, Lu J, Sherbourne C. The MOS 36-item short-form health survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care. 1994;32(1):40–60. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 81.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology. 2010;63(11):1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


